Abstract
Parent’s insurance coverage is associated with children’s insurance status, but little is known about whether a parent’s coverage continuity affects a child’s coverage. This study assesses the association between an adult’s insurance continuity and the coverage status of their children. We used data from a subgroup of participants in the Oregon Health Care Survey, a three-wave, 30-month prospective cohort study (n = 559). We examined the relationship between the length of time an adult had health insurance coverage and whether or not all children in the same household were insured at the end of the study. We used a series of univariate and multivariate logistic regression models to identify significant associations and the rho correlation coefficient to assess collinearity. A dose response relationship was observed between continuity of adult coverage and the odds that all children in the household were insured. Among adults with continuous coverage, 91.4% reported that all children were insured at the end of the study period, compared to 83.7% of adults insured for 19–27 months, 74.3% of adults insured for 10–18 months, and 70.8% of adults insured for fewer than 9 months. This stepwise pattern persisted in logistic regression models: adults with the fewest months of coverage, as compared to those continuously insured, reported the highest odds of having uninsured children (adjusted odds ratio 7.26, 95% confidence interval 2.75, 19.17). Parental health insurance continuity is integral to maintaining children’s insurance coverage. Policies to promote continuous coverage for adults will indirectly benefit children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Uninsured children in the United States have higher odds of having an unmet medical need compared to children with insurance [1, 2]. Recent policy and reform efforts have focused on expanding health insurance coverage for children. Yet, despite efforts to provide health insurance to more children, many children who qualify for public health insurance remain uninsured [3]. One study estimated that almost 11% of children in Oregon presumed eligible for public health insurance were uninsured [3]. Further, the ability of a child to obtain and maintain health insurance coverage is influenced by the relationship between parental and child health insurance status [4]. Maternal health insurance coverage is associated with a decreased likelihood of children losing coverage [5]. In Massachusetts, children experienced a 14% increase in public health insurance coverage prevalence after the State expanded coverage to parents [6]. In Oregon, children with uninsured parents are more likely to be uninsured than children with insured parents [7]. Insuring both parents and children is also associated with children having continuous coverage and regular physician visits. [2, 8] In addition to health insurance status, other parental characteristics, such as race and ethnicity, primary language, and income level, have been found to be associated with whether or not a child is insured [1, 9–16].
Previous research has confirmed associations between parents’ health insurance status, household characteristics, and the insurance status of their children. However, less is known about the relationship between continuity of adult coverage and children’s health insurance status. Thus, we sought to assess the specific association between the continuity of an adult’s health insurance coverage over time and the coverage status of children in the same household, among a low-income population in Oregon.
Methods
Data Source
We conducted secondary analyses of data from the Oregon Health Care Survey (OHCS), a three-wave, 30-month prospective panel study conducted between 2003 and 2006 to assess policy changes that affected adults enrolled in the Oregon Health Plan (OHP), Oregon’s public health insurance program [17]. The OHCS study selected a panel of OHP adults to be included in a prospective cohort study, shortly after policy changes were implemented to increase cost sharing and reduce benefits for adult OHP enrollees. Specifically, a stratified random sample of potential participants was selected from OHP Medicaid eligibility files. The sample included 10,600 adults aged 19–64 years that qualified for OHP at least 30 days before February 15, 2003, when administrative and cost-sharing changes were put into effect for OHP Standard. African American, Native American and Spanish-speaking populations were over-sampled to ensure adequate representation, with 500 people randomly selected from each of these racial and ethnic groups. Of the original 10,600 people selected, 8,260 were found to be eligible [18].
Surveys were mailed to the panel at 6, 18, and 30 months after policy changes were implemented. If a response was not received within 4 months, two additional surveys were mailed at one-month intervals. Between each survey mailing, reminder postcards were sent and telephone reminder calls were made. Surveys were conducted in both English and Spanish. Spanish language surveys were translated and then independently back translated. Several widely accepted data collection tools were used to devise the OHCS, which assessed respondents’ health insurance continuity, access to health care, health care utilization, and financial and health outcomes [19, 20]. Cognitive testing of the survey instrument was conducted with a pilot sample of OHP members to ensure validity of the instrument. The panel study had a recruitment rate of 34% (n = 2783), and subsequently a 66% (n = 1837) response rate (56% of the panel recruited responded to all three surveys). Additional information including results of the original survey can be found elsewhere. [4, 17, 18, 21, 22].
For our secondary analysis of the OHCS data, we developed several additional criteria for inclusion. First, we included only those who provided information about the length of their own insurance coverage, and lastly, we included only those who reported whether all children (under 19 years) in the same household had health insurance at the end of the study period (30 months after policy changes), for a final sample of 559 adults. To account for oversampling by race and ethnicity, base weights represented the probability of selection. Iterative post-stratification ‘raking’ was then used to adjust for each wave of data collection’s non-response and differences between our study population as compared to the overall population, with information such as demographics, health care utilization and health status [17]. Composite survey weights were calculated in excel for each respondent in our study population (the base weight and non-response weight were multiplied together), and these pre-calculated weights were used in all analyses.
Variables and Analyses
Study Variables
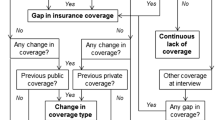
The primary dependent variable was children’s health insurance status at the end of the study period (30 months after baseline). The survey assessed coverage status for each child, which we collapsed into a dichotomous variable: (1) all children (under 19 years) insured or (2) at least one child (under 19 years) not insured. The primary independent variable was the total length of parents’ health insurance coverage during the study period, collapsed into four categories: 0–9, 10–18, 19–27 or 28–30 months. Because coverage was measured in 3-month intervals, the insurance length interval of 28–30 months was considered to be continuous health insurance coverage. All adults that responded to the survey were insured by the OHP at the beginning of the study period, so any coverage gap reflected a disenrollment from OHP at some point during the study period.
We selected all available independent variables that might potentially influence the dependent variable of interest (whether or not all children in the household were covered at the end of the study period). These covariates included information reported by the adult responding to the survey, including: (1) age at study start, (2) race/ethnicity, (3) primary language, (4) household income, (5) employment stability, (6) educational attainment, (7) OHP member type at start of the survey, and whether or not the individual reported having (8) medical debt and (9) financial strain. Race/ethnicity was defined as White/non-White, and primary language was defined as English/non-English. Health related financial strain was coded ‘yes’ if the participant answered yes to a series of questions about financial problems they have encountered in the last 6 months because of health care expenses. OHP member type was determined by those who were categorically eligible for Medicaid based on federal guidelines (in the OHP “Plus” program) and those who were in the OHP expansion population of adults who did not meet federal guidelines for Medicaid (in the OHP “Standard” program).
Statistical Analysis
We first conducted a series of univariate analyses to compare characteristics of adult respondents as associated with different lengths of insurance coverage. We then determined univariate associations between the primary independent variable (adult coverage lengths) and our dependent variable. We used simple logistic regression models to assess significant univariate associations between all 8 independent covariables and the dependent variable of interest (p < 0.05). We then assessed collinearity between covariables using the rho correlation coefficient. Although only length of adult coverage, race and primary language were significant (p < 0.05), we moved forward with all variables in the model because they were all conceptually relevant. We then assessed for collinearity between variables. Income, education and employment were highly collinear, so we included only education in the final model. Medical debt and financial strain were also found to be collinear, so we included only medical debt in the final model. Thus, the following variables were included in the multivariate analysis: adult insurance coverage length (primary independent variable), age at study start, race/ethnicity, primary language, education, OHP member type, and medical debt. Using goodness-of-fit testing techniques, we determined that this final model fit well because there was not a significant difference between the observed and expected values [23]. All data were analyzed using STATA Version 10 (STATA Corporation). The study was approved by the Institutional Review Board at Oregon Health & Science University.
Results
There were differences with regard to OHP member type and length of coverage; among those with OHP Plus, 66.3% were continuously insured versus only 2.9% with only 0–9 months of coverage. In contrast, among those with OHP Standard, 37.8% reported continuous coverage versus 18.7% with 0–9 months of coverage. Among those who did not have any medical debt at 30 months, 60.2% were continuously insured, as compared to 18.7% with 19–27 months of coverage, 12.0% with 10–18 months of coverage, and only 9.2% with 0–9 months of coverage. Of note, only 38.6% of those with greater than $500 in medical debt reported continuous coverage (Table 1).
We found a dose response relationship between insurance continuity among adults and the likelihood that their children were insured at the end of the study period, as shown in Table 2. For example, among adults who were insured for 28–30 months, 91.4% reported that all children in the household were insured at 30 months, compared to 83.7% among adults insured for 19–27 months, 74.3% among adults insured for 10–18 months, and 70.8% among adults insured for fewer than 9 months.
This pattern was also clearly visualized in the unadjusted logistic regression models presented in Table 3. Adults with less coverage continuity were more likely to report at least one uninsured child in the household at the end of the study. Those with the fewest months of coverage reported the highest odds of having uninsured children in the household (Odds ratio [OR] 4.41, 95% Confidence interval [CI] 2.04, 9.53). We also found relationships between adult race/ethnicity and language and children’s coverage. Non-White adults had higher odds of having at least one uninsured child in the household at 30 months, as compared with White adults (OR 2.22, 95% CI 1.28, 3.86) and non-English speaking adults had higher odds than English speaking adults to report uninsured children (OR 4.72, 95% CI 2.24, 9.92).
When controlling for statistically and conceptually significant covariates in a multivariate model, as shown in Table 4, the significant associations between adults with fewer months of health insurance coverage and higher odds of having uninsured children remained. Adults with the shortest insurance coverage continuity (0–9 months) had the highest odds of having at least one uninsured child in the household at the end of the study period (adjusted OR 7.26, 95% CI 2.75, 19.17). In addition to adult insurance continuity, there was a significant multivariate association between an adult in the household with a primary language other than English and having at least one uninsured child at 30 months (adjusted OR 4.12, 95% CI 1.38, 12.32).
Discussion
We found a significant association between parents’ health insurance continuity and the odds of all children in the household being insured at the end of the study. Beyond past studies which confirmed a significant association between parental and child health insurance coverage status [2, 6–8, 13, 24–26], our analysis also suggests a dose response relationship between the continuity of an adult’s health insurance coverage and the odds of all children in the household being insured. This new finding has significant policy relevance regarding the critical importance of insurance coverage continuity for adults as a way to increase uptake of public insurance by eligible low-income children in the United States.
Previous research has shown that race and ethnicity are significantly associated with whether children have insurance [1, 9, 25], and that Hispanic children are more likely to be uninsured compared to non-Hispanic children. [9, 27, 28] Additionally, Hispanic children have significantly higher odds of having parents with shorter lengths of insurance coverage [25]. Although our study did not specifically examine ethnicity, we did find a lower percentage of non-White adults with continuous coverage. Further, in multivariate analyses, non-White adults had significantly higher odds of having at least one child uninsured in household at the end of the study period. Non-English speakers also had higher odds of having at least one uninsured child, and language remained a significant covariate in the adjusted models. Speaking a language other than English has been shown in prior research to be a barrier to enrolling Medicaid-eligible children in public health insurance [29, 30]. Therefore, interventions to help non-English speakers and racial and ethnic minority groups obtain and maintain public health insurance may also help to increase the prevalence of insurance coverage among some of the nation’s most vulnerable children.
Previously published analyses from the OHCS have shown that the 2003 Oregon Health Plan policy changes negatively impacted adult enrollment in the OHP [17, 21, 22]. Even though these policy changes did not affect children’s public insurance eligibility or enrollment criteria, our study suggests that children’s insurance coverage was impacted. One possible explanation is that low-income adults may not have distinguished between their own eligibility for public coverage and that of their children. Efforts to increase or expand children’s insurance coverage may have greater impact if eligibility requirements were better communicated and understood. Additionally, if policies were to focus on ensuring continuous health insurance coverage for parents, or covering both parents and children simultaneously, the outcome will likely be better coverage for children.
Limitations
This study had several potential limitations. First, selection bias may have occurred with the study population. Previously published OHCS data studies, however, report participants who responded to the survey were demographically similar to those who did not participate [22]. Second, this study included Oregon residents; thus, our findings may not be applicable to health policy changes for children living in other regions [28]. Third, the survey was subject to potential recall bias because of the self-reported methodology. To minimize this bias, multiple questions were used to assess survey issues, the survey was validated, and extensive cognitive testing was used in the development of the survey [17, 19, 20]. Fourth, there was no baseline health insurance information for children in this study; health coverage information was only collected for children during the final survey (at 30 months). Therefore, the timing of when children attained and lost health insurance coverage was not known. A causal association, therefore, cannot be determined between child(ren) and an adult in the same household attaining or losing health insurance. There is also a possibility that other differences between the adult length of insurance coverage groups may have caused children to lack insurance at 30 months. Finally, several important child characteristics could not be studied including child’s health, race, ethnicity, and age, which have been previously shown to have significant associations with child insurance status and health care access [31–33].
Conclusions
This study showed that continuity of health insurance coverage for adults was significantly associated with the insurance status of children in the same household. Therefore, it is likely that policies which optimize parental insurance coverage continuity will result in higher rates of children’s health insurance coverage.
References
Hoilette, L. K., Clark, S. J., Gebremariam, A., & Davis, M. M. (2009). Usual source of care and unmet need among vulnerable children: 1998–2006. Pediatrics, 123(2), e214–e219.
Guendelman, S., & Pearl, M. (2004). Children’s ability to access and use health care. Health Affairs, 23(2), 235–244.
DeVoe, J. E., Krois, L., Edlund, C., Smith, J., & Carlson, N. E. (2008). Uninsured but eligible children: Are their parents insured? recent findings from oregon. Medical Care, 46(1), 3.
Carlson, M. J., DeVoe, J. E., & Wright, B. (2006). Short-term impacts of coverage loss in a medicaid population: Early results from a prospective cohort study of the Oregon health plan. Annals of Family Medicine, 4(5), 391–398.
Sommers, B. D. (2006). Insuring children or insuring families: Do parental and sibling coverage lead to improved retention of children in Medicaid and CHIP? Journal of Health Economics, 25(6), 1154–1169.
Dubay, L., & Kenney, G. (2003). Expanding public health insurance to parents: Effects on children’s coverage under medicaid. Health Services Research, 38(5), 1283–1302.
DeVoe, J., Lisa, K., Tina, E., Jeanene, S., & Nichole, E. C. (2008). Uninsurance among children whose parents are losing medicaid coverage: Results from a statewide survey of Oregon families. Health Services Research, 43(1p2), 401–418.
Davidoff, A., Dubay, L., Kenney, G., & Yemane, A. (2003). The effect of parents’ insurance coverage on access to care for low-income children. Inquiry, 40(3), 254–268.
Pylypchuk, Y., & Selden, T. M. (2008). A discrete choice decomposition analysis of racial and ethnic differences in children’s health insurance coverage. Journal of Health Economics, 27(4), 1109–1128.
Federico, S., Tjoeng, H., & Berman, S. (2007). State strategies to reduce the number of uninsured children. The Journal of Pediatrics, 151(5, S1), S28–S31.
Chung, E. K., Mathew, L., McCollum, K. F., Elo, I. T., & Culhane, J. F. (2008). Continuous source of care among young underserved children: Associated characteristics and use of recommended parenting practices. Ambulatory Pediatrics, 8(1), 36–42.
Van Wie, A., Ziegenfuss, J., Blewett, L. A., & Davern, M. (2008). Persistent disparities in health insurance coverage: Hispanic children, 1996 to 2005. Journal of Health Care for the Poor and Underserved, 14(4), 1181–1191.
DeVoe, J. E., Tillotson, C., & Wallace, L. S. (2008). Uninsured children and adolescents with insured parents. The Journal of the American Medical Association, 300(16), 1904–1913.
DeVoe, J., Graham, A., Angier, H., Baez, A., & Krois, L. (2008). Obtaining healthcare services for low-income children: A hierarchy of needs. Journal of Healthcare for the Poor and Underserved, 19(4), 1192–1211.
Cassedy, A., Fairbrother, G., & Newacheck, P. W. (2008). The impact of insurance instability on children’s access, utilization, and satisfaction with health care. Ambulatory Pediatrics, 8(5), 321–328.
Minkovitz, C. S., O’Campo, P. J., Chen, Y., & Grason, H. A. (2002). Associations between maternal and child health status and patterns of medical care use. Ambulatory Pediatrics, 2(2), 85–92.
Carlson, M. J., & Wright, B. J. (2005). The impact of program changes on enrollment, access, and utilization in the Oregon health plan standard population. Portland, OR: The Office for Oregon Health Policy and Research.
Solotaroff, R., DeVoe, J. E., Wright, B., Smith, J., Boone, J., Edlund, T., et al. (2005). Medicaid programme changes and the chronically ill: Early results from a prospective cohort study of the Oregon Health Plan. Chronic Illness, 1, 191–205.
Agency for Healthcare Research and Quality. (2002). CAHPS 2.0 survey and reporting kit. Silver Springs, MD: Agency for Healthcare Research and Quality.
Center for Studying Health System Change. (2004). Community Tracking study, Household survey instrument 2000–2001, Round three. Technical Publication #54. Washington, DC: Center for Studying Health System Change.
Wright, B. J., Carlson, M. J., Allen, H., Holmgren, A. L., & Rustvold, D. L. (2010). Raising premiums and other costs for Oregon Health Plan enrollees drove many to drop out. Health Affairs, 29(12), 2311–2316.
Wright, B. J., Carlson, M. J., Edlund, T., DeVoe, J. E., Gallia, C., & Smith, J. (2005). The impact of increased cost sharing on medicaid enrollees. Health Affairs, 24(4), 1106–1116.
Archer, K. J., & Lemeshow, S. (2006). Goodness-of-fit test for a logical regression model fitted using survey sample data. The Stata Journal, 6(1), 97–105.
Sommers, B. (2007). Why millions of children eligible for Medicaid and SCHIP are uninsured: Poor retention versus poor take-up. Health Affairs, 26(5), w560–w567.
DeVoe, J. E., Tillotson, C. J., & Wallace, L. S. (2009). Children’s receipt of health care services and family health insurance patterns. Annals of Family Medicine, 7(5), 406–413.
Sarnoff, R., & Hughes, D. (2005). Increasing health insurance coverage in the first year of life. Maternal and Child Health Journal, 9(4), 343–350.
DeVoe, J. E., Graham, A., Krois, L., Smith, J., & Fairbrother, G. L. (2008). “Mind the gap” in children’s health insurance coverage: Does the length of a child’s coverage gap matter? Ambulatory Pediatrics, 8(2), 129–134.
Olson, L. M., Tang, S. F., & Newacheck, P. W. (2005). Children in the United States with discontinuous health insurance coverage. New England Journal of Medicine, 353(4), 382–391.
Feinberg, E., Swartz, K., Zaslavsky, A. M., Gardner, J., Gardner, J., & Klein Walker, D. (2002). Language proficiency and the enrollment of medicaid-eligible children in publicly funded health insurance programs. Maternal and Child Health Journal, 6(1), 5–18.
DeCamp, L. R., & Bundy, D. G. (2011). Generational status, health insurance, and public benefit participation among low-income Latino children. Maternal & Child Health Journal. doi:10.1007/s10995-011-0779-8
Currie, J., Decker, S., & Lin, W. (2008). Has public health insurance for older children reduced disparities in access to care and health outcomes? Journal of Health Economics, 27(6), 1567–1581.
Voelker, R. (2009). Reforms Needed in Adolescent Health Care. The Journal of the American Medical Association, 301(4), 368.
Committee on Adolescence and Committee on Child Health Financing. (2009). Underinsurance of Adolescents: Recommendations for Improved Coverage of Preventive, Reproductive, and Behavioral Health Care Services. Pediatrics, 123(1), 191–196.
U.S. Department of Health and Human Services. (2003). HHS poverty guidelines. Federal Register, 68(7), 6456–6458.
Acknowledgments
This study was financially supported by an Robert Wood Johnson Foundation State Coverage Initiatives in Health Care Reform (0403017), the Commonwealth Fund (20040741), the Agency for Healthcare Research and Quality (R03 HS016119) (1 K08 HS16181) (1 R01 HS018569), the Oregon Health & Science University Department of Family Medicine, and the Oregon Office of Medical Assistance Programs. These funding agencies had no involvement in the design and conduct of the study; analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The authors also gratefully acknowledge the Oregon Health Research and Evaluation Collaborative, Dr. Charles Gallia, from the Division of Medical Assistance Programs, and the Office for Oregon Health Policy and Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamauchi, M., Carlson, M.J., Wright, B.J. et al. Does Health Insurance Continuity Among Low-income Adults Impact Their Children’s Insurance Coverage?. Matern Child Health J 17, 248–255 (2013). https://doi.org/10.1007/s10995-012-0968-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-012-0968-0