Abstract
To assess the association between a child’s and their parent’s public health insurance status during a time when children had access to coverage independent of policies that impacted adults’ access. Secondary data from the Oregon Health Plan (OHP) [Oregon’s Medicaid and Children’s Health Insurance Programs] for families with at least one parent and one child with OHP coverage at any time during the study period (2002–2010). We linked children to their parents in the OHP data set and examined longitudinal associations between the coverage patterns for children and their parents, controlling for several demographic and economic confounders. We tested for differences in the strength of associations in monthly coverage status in five time periods throughout the nine-year study period. The odds of a child being insured by the OHP in months in which at least one parent had OHP coverage were significantly higher than among children whose parents were not enrolled at that time. Children with at least one parent who maintained or gained OHP coverage in a given month had a much higher probability of being enrolled in the OHP in that month, compared to children who had no covered parents in the given month or the month prior. Despite implementation of policies that differentially affected eligibility requirements for children and adults, strong associations persisted between coverage continuity for parents and children enrolled in Oregon public health insurance programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with continuous health insurance have higher rates of preventive health care and improved health outcomes, compared to children with unstable coverage [1, 2]. Historically, children in the United States were covered by the same health insurance program as their parent(s)—an employer-sponsored plan or a public insurance program [3]. This tradition of a ‘family health insurance plan’ likely contributed to past reports of a strong association between coverage for children and parents [4–6]. More recently, programs target parents and children separately, and fewer families have just one plan covering all family members. For example, the Children’s Health Insurance Program (CHIP) ‘decouples’ family insurance by providing access to coverage for children independent of policies that impact adults’ access [7], and many states’ Medicaid programs have different eligibility requirements for adults and children [8].
As children have had increased opportunities for coverage, we assessed whether coverage status changes for parents are still affecting their children’s coverage [9–11]. This relationship is poorly understood. Most previous studies that reported associations between the insurance status of parents and children used cross-sectional or survey data limiting their ability to assess longitudinal associations between parent and child coverage continuity, or the odds of a child having coverage during a time period when a parent gains or loses coverage [6, 12–15].
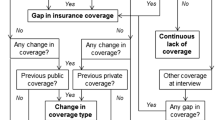
We hypothesized that, as a result of CHIP policies, a child’s public health insurance status may become less strongly associated with their parent’s status. To test this, we linked children and their parents using Oregon Health Plan (OHP) [Oregon’s Medicaid and CHIP programs] administrative data, and assessed the longitudinal association between children’s odds of being covered and their parents’ maintenance, gain, or loss of public coverage. We compared the strength of this association during five time periods over 9 years that incorporated three major policy changes (see Fig. 1 and descriptions below), and examined whether these changes were associated with significant differences in the percentage of children in the sample covered by the OHP.
Five time periods that span before and after three major policy changes of the Oregon Health Plan (OHP) between 2002 and 2010. Oregon Health Plan (OHP): Oregon’s Medicaid and Children’s Health Insurance Programs (CHIP). source OHP administrative data, 2002–2010. For more information: Oregon Health Plan (OHP) An Historical Overview. 2006. http://www.oregon.gov/oha/healthplan/DataReportsDocs/OregonHealthPlan-Anhistoricaloverview.pdf. The time periods were delineated before and after each policy change in order to see if differences existed with each change. a The OHP expansion population included adults with income <100 % FPL who were not categorically eligible for Medicaid (described in detail elsewhere); [16, 17] the expansion population was enrolled in a newly created OHP Standard program that instituted copayments, reduced benefits and required timely payment of premiums to stay enrolled [19, 50]. b Expansion of Oregon’s CHIP. Family income determines whether the child qualifies for no-cost, low-cost or full-cost health insurance options. Note The three policy change points of interest (noted in boxes below the timeline) coincided with five time periods (noted above the timeline) in which trends in children’s coverage rates differed significantly (P values <0.001), as identified by joinpoint regression analyses
The Policy Changes
Policy Change One
In 2003, Oregon expanded CHIP eligibility from 133 to 185 % of the Federal Poverty Level (FPL). Concurrently, due to declining state revenues, the OHP split into two programs for adults: OHP Plus for those eligible to receive coverage based on Federal rules (e.g., pregnant women, the disabled) and OHP Standard for non-disabled adults making less than 100 % FPL (described elsewhere) [16, 17]. OHP Standard required an adult to be uninsured for 6 months before they could be considered for coverage, reduced adults’ benefits, increased copayments, and introduced premiums. OHP Standard then closed to new applicants from mid-2004 to 2008. Over 50,000 adults covered by OHP Standard lost coverage [18, 19]. Oregon’s decision to cut adults from the OHP was made with the explicit goal of keeping children covered by expanding children’s eligibility. We looked at this policy change to investigate what happened to children when their parents lost public coverage.
Policy Change Two
In 2008, OHP Standard re-opened enrollment for a limited number of new applications from low-income adults who did not qualify for categorical Medicaid. Because demand far exceeded availability, the Centers for Medicare and Medicaid Services permitted a randomized selection process for enrollment of new members. By February 2008, nearly 100,000 uninsured, low-income adults in Oregon placed their names on an OHP ‘reservation list,’ in hopes of being randomly selected to apply for OHP coverage. Starting in March, a series of eight random drawings were conducted; approximately 10,000 individuals with incomes at or below 100 % FPL eventually received coverage after applying [20–22]. We looked at this policy change to investigate the likelihood of a child gaining coverage when a parent gained coverage.
Policy Change Three
The OHP random selection process was repeated in 2010. Concurrently, Oregon expanded CHIP to include children with family incomes up to 200 % FPL and launched the Healthy Kids Connect program, which offered insurance premium subsidies for children of families earning between 200 and 300 % FPL. Although an estimated 90,000 children gained coverage through these programs [23], many eligible children remained uninsured [24, 25]. We looked at this policy change to investigate what happened to children when parents gained coverage.
Methods
Data Sources
We used OHP administrative data, which included enrollment details for all children who received Medicaid or CHIP coverage at any point between January 1, 2002 and December 31, 2010. This longitudinal dataset contained each child’s age, race, sex and zip code, individual identification (ID) number, household case ID number, and dates enrolled in coverage. This dataset also included similar information for all individuals who shared a household case ID number with these children. Data on county Rural–Urban Continuum Code (RUCA), yearly estimates of the percent of the county population participating in the Supplemental Nutrition Assistance Program (SNAP), and the percent of unemployed county labor force were obtained from the United States Department of Agriculture (USDA) [26–28]. Monthly data on unemployment rates in the state of Oregon were obtained from the Bureau of Labor Statistics local area unemployment statistics [29]. Families were linked to county level economic indicators through their zip code.
Study Population
We began with 889,452 household case IDs from the OHP administrative data. Because child-parent pairs were not explicitly identified within the household, we created an algorithm to select a cohort of children with parent(s) who were also enrolled in the OHP at some point during the study period (detailed algorithm can be found elsewhere) [30]. Briefly, we included any OHP-enrolled household with two or more individuals, with at least one individual younger than 19 years of age and at least one possible parent older than 19 at any point during the study period. An adult was considered a possible parent if he or she was 12–55 years older than the child. Children could only have one possible parent of the same sex.
Family coverage data were limited to months in which the child was over 2 and <18. The earliest possible month a family was included was when the child turned 2, or when anyone in the family first appeared in the OHP data, whichever came last. The last possible month was when the child turned 18 or the month the entire family was gone from the OHP data set for a year, whichever came first. We chose 1 year because the mean length of a gap in coverage in our dataset was 12 months. The data were restricted to months when the child was aged 2–18 to increase generalizability; some states have covered children up to age 2 with the same eligibility rules as those aged 0–1 [8, 31]. Child-months in which insurance eligibility codes indicated that coverage for the mother or child was based on pregnancy were also excluded from the analysis.
Because the within family intra-class correlation (ICC) was close to one, we limited our analysis population to a single child per family. To avoid bias due to differences in the probability of selection among families of different sizes, we utilized the youngest child in each household that met study inclusion criteria. Child’s age was included in the analysis to control for any bias introduced by selection of the youngest child. As a sensitivity analysis, we tested our results in age stratified models. Our final cohort consisted of 138,651 household case IDs; including 133,045 mothers and 48,911 fathers.
Study Variables
The primary dependent variable for the regression analyses was whether or not a child was enrolled in the OHP at any time during a given month. We included two primary independent variables: (1) the policy change and (2) parental OHP coverage during the month of interest and the prior month. Additionally, an interaction term for these two variables was included to examine the strength of the child-parent coverage association over time. Age of child, child’s race and sex, number of children in the family, and RUCA were included as potential confounders of the association between the primary independent and dependent variables, as they have been shown to influence coverage [1, 6, 24, 32, 33]. Based on exploratory analysis of one-year age periods, children were categorized into four-year age blocks. To control for potential confounding related to income, which is associated with coverage [34], and the overall strength of the economy at the time of the assessment, variables were included for: yearly percent of Oregon children with private insurance, monthly percent of county participating in SNAP, yearly percent of county unemployment, and monthly Oregon unemployment (not adjusted for seasonal work).
Analyses
We calculated monthly coverage rates for children and their parents between 2002 and 2010. The analysis assessed the association between OHP insurance continuity for parents and their children over five time periods: (1) Before 2003 adult cost containment; (2) After 2003 adult cost containment to 2005; (3) From 2005 to the first OHP random selection for adults in 2008; (4) Between the first OHP random selection for adults and the Healthy Kids/CHIP expansions in 2010; and (5) Post 2010 Healthy Kids/CHIP expansions. As shown in Fig. 1 (above), the three policy changes were used to define the boundaries of time periods in which the association of children’s coverage with their parent’s coverage could significantly differ.
To examine the association between a child’s coverage status and parental coverage, we used a generalized estimating equation (GEE) model with a logit link to account for the correlation of repeated measures over time. We used a sandwich estimator for the GEE and specified an independent correlation structure for the model of repeated measures, an approach shown to be more robust than misspecification when the structure is unknown [35].
We used joinpoint regression to identify significant changes in the trend of children’s coverage rates over the study period. Joinpoint is a data-driven method that determines significant time trend changes, using a Monte Carlo permutation method and applying Bonferroni corrections to maintain type I error. (Joinpoint Regression Software Version 4.0.1, Statistical Research and Applications Branch, National Cancer Institute) [36].
All analyses, except joinpoint regression, were conducted using SAS software, version 9.3 (SAS Institute, Inc.). A P value of <0.05 was considered statistically significant for all analyses. This study was approved by the Institutional Review Board at our academic institution.
Results
Time Periods of Most Significant Change in Children’s Coverage Rates
Figure 2 demonstrates monthly coverage rates for children in the study sample (enrolled in the OHP at some point between 2002 and 2010 with parent(s) also covered by the OHP at some point during this time period), and coverage rates of their linked parent(s). The five time periods included in the longitudinal analysis are delineated by vertical lines. Intervals with significant changes in the linear trend in children’s coverage levels are identified by solid lines. Although a higher percentage of children than parents were covered each month, children’s public coverage patterns closely mirrored parents’ coverage patterns. Notably, we observe a significant drop in children’s coverage following 2003 adult cost containment, which coincided with a policy to expand CHIP eligibility. During the third time period, joinpoints two and three likely correspond to changes in children’s enrollment policies at the time including: reenrollment changing from 6 to 12 months and the implementation of proof of citizenship [37]. Coverage rates for both children and parents increased after the OHP random selection, which were implemented in five waves from February to October 2008. The joinpoint analysis confirmed a significant increase in children’s coverage following random selection. Coverage rates for children and parents increased more steeply in 2010 after the implementation of Healthy Kids and the 2nd round of OHP random selection for adults.
Figure 3 demonstrates how year-end coverage rates changed for children in the study population before and after major policy changes of interest. Coverage rates fell significantly from December 2002 to December 2003 (before vs. after OHP adult cost containment). Rates increased between December 2007 and December 2008 (before vs. after the first OHP random selection). Rates increased further when comparing December 2009–December 2010 (before vs. after the second round of OHP random selection and major CHIP expansions).
Children’s Oregon Health Plan (OHP) coverage rates before and after three policy changes, among linked children and parent(s) in OHP data. Oregon Health Plan (OHP): Oregon’s Medicaid and Children’s Health Insurance Programs (CHIP) source OHP administrative data, 2002–2010 Pre-policy to post-policy change comparisons are significant at P < 0.0001 for time periods shown
Table 1 presents the results of longitudinal GEE logistic regression models that assessed associations between monthly coverage for each child and coverage status of their linked parent(s) during the five time periods (before and after the three policy change points). Although the probability that a child would be covered if their parent was not covered increased between the first and last time period in the study, children with at least one parent who maintained (yes/yes) or gained OHP coverage (no/yes) in a given month had a much higher probability of being enrolled in the OHP in that month, compared to children who had no covered parents in the given month or the month prior (no/no) in all study time periods. (The adjusted probabilities of a child being covered if their parent was not insured in the current month ranged from 0.28 to 0.57, while the probability that a child with an insured parent was insured ranged from 0.89 to 0.95). The odds ratios (OR) for children’s insurance with insured compared to uninsured parents were higher in the earlier time periods, and attenuated in time periods 4 and 5, but remained significant throughout the study (adjusted OR for children’s coverage ranged from 17.5 to 22.7 in time periods 1 through 3, dropping to between 6.1 and 13.9 in periods 4 and 5). In four of the five time periods, children with a parent who lost public coverage (yes/no) had significantly lower probability of being enrolled in the OHP than children whose parents had no coverage in the given month or the prior month (no/no). Notably, in the time period immediately following the implementation of policies aimed at restricting coverage for adults, children whose parents lost public coverage (yes/no) had slightly higher odds of being enrolled in the OHP, compared with children whose parents had no coverage in the given month or the prior month (no/no) (adjusted OR 1.34, 95 % CI 1.31–1.36); however, their probability of coverage was still significantly lower than children whose parents were insured in that month.
Discussion
In this population of children and parents reliant on the OHP for health insurance, the overall patterns of coverage for children mirrored that of parents, suggesting that children’s public coverage was affected by policies intended for adults only (Fig. 2). The adjusted odds of being covered in a given month were significantly higher if a parent gained or maintained coverage, compared to if the parent had no coverage (Table 1). This association decreased in later time periods, but remained strong throughout the entire study. Even after CHIP expansions in 2010, children with a parent who lost public coverage had significantly lower odds of being enrolled in OHP, compared with children whose parents had no coverage. In other words, the historic association between coverage for children and their parents persisted, even when public coverage was expanded for children. Our results suggest that children whose parents were covered by public insurance had similar patterns of coverage to their parents, even though policies diverged for children and adults. Child-only expansions in public coverage were associated with increases in children’s health insurance coverage rates overall, yet children’s coverage remained strongly associated with parental coverage patterns [7, 38].
Several possible explanations exist for the enduring association of child-parent coverage congruity reported here. During periods when OHP coverage was not accessible to many adults, parents may not have realized that these eligibility restrictions did not apply to children, or may have mistakenly thought that a loss of adult coverage equated to a loss for the entire family. This phenomenon has been shown in qualitative studies. Interviewees reported they discovered their children qualified for OHP only after they put their name on the 2008 OHP ‘reservation list’ [39, 40], likely explaining the higher rates of coverage in 2009, compared to 2008 (Fig. 3).
Child-parent pairs in our cohort could have dis-enrolled from OHP after entire families gained access to private coverage. However, rates of employer-sponsored coverage have declined for American families in the past decade [41, 42] and the percentage of US employers offering health insurance to families decreased from 66 % in 1999 to 59 % in 2009; for families still able to obtain employer-sponsored coverage, premium costs increased 97 % since 2002 [43, 44]. We included the percentage of privately insured children, county and state unemployment levels and county SNAP participation rates in our model to account for possible economic changes. While these variables were significantly associated with the probability of a child being insured, they did not alter the strength of the association of child-parent insurance status.
Another possible explanation for why a child and parent could have concurrently lost OHP coverage could be that the family moved out of state. To account for families who may have moved, we only kept individuals from a household in the analysis for 1 year after coverage ended if there was no further record of anyone in the household obtaining OHP coverage. Also notable was that children whose parents lost public coverage had lower odds of being insured as compared to children whose parents never had coverage in a given period. This phenomenon could be due to the known confusion about a child’s eligibility for continued coverage at the time an adult lost public coverage.
Policy Implications
The Affordable Care Act (ACA) has provisions to expand public coverage options for adults, which may lead directly to improved coverage continuity for many parents. Due to the continued association between child and parent coverage, improved continuity for parents could indirectly impact coverage continuity for their children [45]. This could happen through a ‘welcome mat’ effect, which happens when parents obtain coverage and discover that their children are also eligible [46]. It remains unclear how many low- and middle-income parents will gain coverage once the ACA is implemented, as state Medicaid expansions are optional [47]. Some may gain coverage under the ACA mechanism that gives people earning up to 400 % FPL subsidies for purchasing health insurance through state exchanges. However, these policies are being challenged in court and may not be available in every state. There is also concern about a ‘family glitch’ that will not provide subsidies adequate enough for parents to buy coverage for their children [48]. Further, many families experience frequent income fluctuations, which could result in parents ‘churning’ on and off different insurance programs. A recent study estimates that 35 % of adults will experience a change in eligibility and 24 % will experience at least two eligibility changes within a year of ACA implementation [49]. As demonstrated here, high parental churn will be detrimental to kids’ coverage. When parents lose public coverage, their children have much higher odds of losing public coverage.
Limitations
Our analyses were limited by the data available. We had information about public coverage in one state only; associations may differ among families with different types of coverage, or in states with different eligibility and/or enrollment policies. This research was not designed to provide a causal link between parent and child coverage congruity. Because the study focus was the association of children’s coverage with their parents’ coverage, our analysis excluded children whose parents were never covered by the OHP. As CHIP policies were changed to promote enrollment of additional children, we were concerned that the proportion of children with parents also covered by OHP might drop over the study period, compared to the total number of children with OHP coverage. However, when we looked at the percentage of children in our study population, compared to the total number of children enrolled in the OHP each year, we found the percentage remained consistent (approximately 35 % each year). We investigated the difference in results if we excluded parents whose Medicaid eligibility codes indicated disabled status (n = 8,030 children) and found predicted probabilities were virtually unchanged. We dropped children/parents from the population after a period of 1 year with no family member enrolled in the OHP, which may have underestimated rates of uninsurance. Since we included children aged 2–18, generalizability of our results is limited to children in this age range. We included only the youngest child in the family to avoid GEE model instability from low cluster sizes within families. The ICC findings; however, indicated that the use of only the youngest child from each family did not unduly bias our results. Finally, to test the effect of additional smoothing of coverage, we conducted analyses without counting those with a 1 month gap as uncovered (n = 12,451 children) and found minimal variance in results.
Conclusions
This study highlights a consistent association between patterns of public coverage for children and parents during a time in which public coverage eligibility was closed or very limited for most parents, but was consistently open and expanded for children. Findings show that when parents lose health insurance coverage, children also risk losing coverage. Therefore, keeping parents insured is important to keeping children insured.
References
DeVoe, J. E., et al. (2008). “Mind the gap” in children’s health insurance coverage: Does the length of a child’s coverage gap matter? Ambulatory Pediatrics, 8(2), 129–134.
Cassedy, A., et al. (2008). The impact of insurance instability on children’s access, utilization, and satisfaction with health care. Ambulatory Pediatrics, 8(5), 321–328.
Ziegenfuss, J. Y., & Davern, M. E. (2010). Twenty years of coverage: An enhanced current population survey-1989–2008. Health Services Research, 46(1 Pt 1), 199–209.
DeVoe, J. E., Tillotson, C. J., & Wallace, L. S. (2009). Children’s receipt of health care services and family health insurance patterns. Annals of Family Medicine, 7(5), 406–413.
Wisk, L. E., & Witt, W. P. (2012). Predictors of delayed or forgone needed health care for families with children. Pediatrics, 130(6), 1027–1037.
Yamauchi, M., et al. (2013). Does health insurance continuity among low-income adults impact their children’s insurance coverage? Maternal and Child Health Journal, 17(2), 248–255.
Dubay, L., & Kenney, G. (2009). The impact of CHIP on children’s insurance coverage: An analysis using the national survey of America’s families. Health Services Research, 44(6), 2040–2059.
Kaiser Commission on Medicaid and the Uninsured (2008). Health coverage for children and families in medicaid and SCHIP: State efforts face new hurdles, in A 50-state update on eligibility rules, enrollment and renewal procedures, and cost-sharing practices in medicaid and SCHIP in 2008. Washington, DC.
DeVoe, J., et al. (2008). Uninsurance among children whose parents are losing Medicaid coverage: Results from a statewide survey of Oregon families. Health Service Research, 43(1 Part II), 401–418.
Ku, L., (2007). Collateral damage: Children lose coverage when their parents lose health insurance. Center on Budget and Policy Priorities: Washington, DC.
DeVoe, J. E., et al. (2014). Recent health insurance trends for US families: Children gain while parents lose. Maternal and Child Health Journal, 18(4), 1007–1016.
Guendelman, S., et al. (2006). The effects of child-only insurance coverage and family coverage on health care access and use: Recent findings among low-income children in California. Health Services Research, 41(1), 125–147.
Davidoff, A., et al. (2003). The effect of parents’ insurance coverage on access to care for low-income children. Inquiry, 40(3), 254–268.
Gifford, E., Weech-Maldonado, R., & Short, P. (2005). Low-income children’s preventive services use: Implications of parents’ medicaid status. Health Care Financing Review, 26(4), 81–94.
Sommers, B. D. (2006). Insuring children or insuring families: Do parental and sibling coverage lead to improved retention of children in Medicaid and CHIP? Journal of Health Economics, 25(6), 1154–1169.
Bodenheimer, T. (1997). The Oregon health plan: Lessons for the nation: First of two parts. New England Journal of Medicine, 337(9), 651–656.
Bodenheimer, T. (1997). The Oregon health plan: Lessons for the nation: Second of two parts. New England Journal of Medicine, 337(10), 720–723.
Oberlander, J. (2007). Health reform interrupted: The unraveling of the Oregon health plan. Health Affairs (Millwood), 26(1), w96–w105.
Carlson, M., DeVoe, J., & Wright, B. (2006). Short-term impacts of coverage loss in a Medicaid population: Early results from a prospective cohort study of the Oregon health plan (OHP). The Annals of Family Medicine, 4(4), 391–398.
Oregon Division of Medical Assistance Programs (2008). OHP Standard Reservation List Final Report. [cited 2013 May 31]; Available from: http://www.oregon.gov/oha/healthplan/DataReportsDocs/OHP%20Standard%20Reservation%20List%20Final%20Report.pdf.
Allen, H., et al. (2010). What the Oregon health study can tell us about expanding Medicaid. Health Affairs (Millwood), 29(8), 1498–1506.
Baicker, K., et al. (2013). The Oregon experiment–effects of Medicaid on clinical outcomes. New England Journal of Medicine, 368(18), 1713–1722.
Oregon Health Authority (2011). Oregon Health Insurance Survey Initial Results. 2011 [cited 2013 May 31]; Available from: http://www.oregon.gov/oha/OHPR/RSCH/docs/uninsured/2011_ohis_initial_results.pdf.
DeVoe, J. E., et al. (2007). Uninsured but eligible children: Are their parents insured? Recent findings from Oregon. Medical Care, 46(1), 3–8.
Crocetti, M., et al. (2012). Characteristics of children eligible for public health insurance but uninsured: Data from the 2007 national survey of children’s health. Maternal and Child Health Journal, 16(Suppl 1), S61–S69.
United States Department of Agriculture (2013). Rural-Urban Continuum Codes. [cited 2013 August 22]; Available from: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/.aspx.
United States Department of Agriculture (2013). Supplemental Nutrition Assistance Program (SNAP) Data System. [cited 2013 August 22]; Available from: http://www.ers.usda.gov/data-products/supplemental-nutrition-assistance-program-(snap)-data-system.aspx.
United States Department of Agriculture (2013). Unemployment and median household income for the US and counties, 2000–2011. [cited 2013 August 22]; Available from: http://www.ers.usda.gov/data-products/county-level-data-sets/download-data.aspx.
Bureau of Labor Statistics (2013). Local Area Unemployment Statistics. [cited 2013 August 22]; Available from: http://www.bls.gov/lau/.
Angier, H., et al. (2014). Linkage methods for connecting children with parents in electronic health record and state public health insurance data. Maternal and Child Health Journal, 18(9), 2025–2033.
Kaiser Commission on Medicaid and the Uninsured (2011). Holding steady, looking ahead, in annual findings of A 50-state survey of eligibility rules, enrollment and renewal procedures, and cost-sharing practices in Medicaid and CHIP, 2010–2011. Washington, DC.
Fairbrother, G., et al. (2011). Reporting on continuity of coverage for children in Medicaid and CHIP: What states can learn from monitoring continuity and duration of coverage. Academic Pediatrics, 11(4), 318–325.
DeVoe, J. E., Tillotson, C. J., & Wallace, L. S. (2011). Insurance coverage gaps among US children with insured parents: Are middle income children more likely to have longer gaps? Maternal and Child Health Journal, 15(3), 342–351.
Hill, H. D., & Shaefer, H. L. (2011). Covered today, sick tomorrow? Trends and correlates of children’s health insurance instability. Medical Care Research and Review, 68(5), 523–536.
Pepe, M., & Anderson, G. (1994). A cautionary note on inference for marginal regression models with longitudinal data and general correlated response data. Communications in Statistics: Simulation and Computation, 23(4), 939–951.
Kim, H. J., et al. (2000). Permutation tests for joinpoint regression with applications to cancer rates. Statistics in Medicine, 19, 335–351.
Medical Assistance Programs, (2012) Event narrative, In DHS|OHA Forecasting. Salem, OR.
Hudson, J. L., & Selden, T. M. (2007). Children’s eligibility and coverage: Recent trends and a look ahead. Health Affairs, 26(5), w618–w629.
DeVoe, J. E., Ray, M., & Graham, A. (2011). Public health insurance in Oregon: Underenrollment of eligible children and parental confusion about children’s enrollment status. American Journal of Public Health, 101(5), 891–898.
DeVoe, J. E., et al. (2012). Why do some eligible families forego public insurance for their children? A qualitative analysis. Family Medicine, 44(1), 39–46.
Chernew, M., Cutler, D. M., & Keenan, P. S. (2005). Increasing health insurance costs and the decline in insurance coverage. Health Services Research, 40(4), 1021–1039.
Gould, E. (2010). Employer-sponsored health insurance erosion continues in 2008 and is expected to worsen. International Journal of Health Services, 40(4), 743–776.
Kaiser Family Foundation and the Health Research and Education Trust (2011). Employer Health Benefits: 2011 Annual Survey. Available from: http://ehbs.kff.org/pdf/2011/8225.pdf.
Vistnes, J.P., et al., (2012). Declines in employer-sponsored insurance coverage between 2000 and 2008: Examining the components of coverage by firm size. Health Services Research, 47(3 Pt 1), 919–938.
111th Congress (2010). Compilation of Patient Protection and Affordable Care Act. [cited 2011 December 16]; Available from: http://docs.house.gov/energycommerce/ppacacon.pdf.
Sonier, J., Boudreaux, M. H., & Blewett, L. A. (2013). Medicaid ‘welcome-mat’ effect of affordable care act implementation could be substantial. Health Affairs, 32(7), 1319–1325.
Kenney, G., et al. (2012). Making the medicaid expansion an ACA option: how many low-income americans could remain uninsured. Health Policy Center June 29 [cited 2013 May 31]. Available from: http://www.urban.org/publications/412606.html.
The Henry J. Kaiser Family Foundation, (2014). Children’s health coverage: Medicaid, CHIP and the ACA, in issue Brief, Kaiser Commission on Medicaid and the Uninsured, Editor. Washington, DC.
Sommers, B. D., & Rosenbaum, S. (2011). Issues in health reform: How changes in eligibility may move millions back and forth between medicaid and insurance exchanges. Health Affairs, 30(2), 228–236.
Wright, B., et al. (2005). The impact of increased cost sharing on Medicaid enrollees. Health Affairs, 24(4), 1106–1116.
Acknowledgments
This work was financially supported by the Agency for Healthcare Research and Quality (AHRQ) Grant Number (1 R01 HS018569), the Patient-Centered Outcomes Research Institute (PCORI), and the Oregon Health & Science University Department of Family Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeVoe, J.E., Crawford, C., Angier, H. et al. The Association Between Medicaid Coverage for Children and Parents Persists: 2002–2010. Matern Child Health J 19, 1766–1774 (2015). https://doi.org/10.1007/s10995-015-1690-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-015-1690-5