Abstract
Current US pregnancy-related physical activity recommendations do not provide specific guidance for vigorous intensity activity. We examined the associations between vigorous physical activity during pregnancy and length of gestation and birthweight. Methods: Women were recruited before 10 weeks gestation. At 13–16 weeks gestation, participants reported the type, frequency, and duration of their typical weekly vigorous physical activities. Activity domains included recreational, occupational, household, and child/adult care. Infant birth date was obtained from medical or vital records; if unavailable, self-report was used. Birthweight (from vital records) was studied among term births. We analyzed gestational age among 1,647 births using discrete-time survival analysis. We used logistic and linear regression to analyze preterm birth (birth at <37 weeks) and birthweight, respectively. Vigorous recreational activity was associated with longer gestation (any vs. none, hazard ratio (HR) [95% CI]: 0.85 [0.70, 1.05]) and we did not detect any dose–response association. Higher frequency of vigorous recreational activity sessions (adjusted for total volume of activity) was associated with a decreased odds of preterm birth (≥4 sessions/week vs. 0 or 1, OR [95% CI]: 0.08 (0.006, 1.0). Birthweight was not associated with physical activity measures. In summary, vigorous physical activity does not appear to be detrimental to the timing of birth or birthweight. Our data support a reduced risk of preterm birth with vigorous recreational activity, particularly with increased frequency of recreational activity sessions. Future studies should investigate the components of physical activity (i.e., intensity, duration, and frequency) in relation to birth outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the United States (US), the prevalence of preterm birth has risen over two decades to approximately 12% [1]. This increase is of pressing public health concern because preterm birth is a leading cause of morbidity and mortality in US infants [2–4]. Physical activity is one hypothesized risk factor for preterm birth or growth restriction.
Animal studies suggest decreased uterine blood flow during physical activity [5–8], but studies in women are inconclusive [9–11]. Several studies have reported an increase in fetal heart rate during maternal physical activity [12–16], although changes in fetal heart rate may occur in response to maternal epinephrine and may not reflect a decrease in oxygen [12–15]. Physical activity has been associated with decreased maternal blood glucose during [17] or after [18–21] physical activity. Physical activity during pregnancy lowers insulin levels and it is unclear how long the decrement lasts [18, 19, 21]. Relative insulin resistance is a normal adaptation of pregnancy, and is thought to increase glucose availability to the fetus [22]. Decreasing insulin resistance may leave the fetus to compete with its mother for glucose [18].
The epidemiologic literature relating physical activity to risk of preterm birth or growth restriction is growing, but inconclusive. Physical activity encompasses several types or modes including recreational, household, child care and occupational activity. These modes of physical activity may differ in their associations with preterm birth and growth restriction. The literature examining the association between physical activity and preterm birth or birthweight is limited by assessments that do not include multiple modes of physical activity [23]. Few studies have examined household and child care activities as distinct exposures in relation to preterm birth or birthweight. A large literature relates occupational physical activities to both preterm birth and birthweight (reviewed by Bonzini et al. [24]); however, the measures of occupational activity in these studies are limited. Some studies focus on specific occupational activities (e.g., lifting only or standing only); others involve environmental stressors, like chemical exposures or noise.
Recreational physical activity has been studied as a distinct exposure, but the literature is still inconclusive. A recent Cochrane review of eleven randomized trials with 472 total participants suggested that the risk of preterm birth may be higher in women who perform recreational physical activity during pregnancy, although no association was detected with gestational age [25]. They concluded that the data are insufficient to draw firm conclusions.
The physical activity literature is also limited by studies that have not measured frequency and duration of activity. This limits their ability to assess either dose–response or the independent associations of these components of activity with pregnancy outcomes. Current physical activity recommendations from the American College of Obstetricians and Gynecologists [26] and the US Department of Health and Human Services [27] do not specifically address vigorous intensity activity, suggesting that studies of the associations of vigorous activity may be informative to those who make recommendations about physical activity, as well as for women and their health care providers.
From a summary of this literature several research questions remain. First, what is the association of each mode of physical activity (recreational, household, child care, occupational) with preterm birth or birthweight? And, is there a dose–response association? Second, how are frequency and duration of physical activity related to preterm birth or birthweight? Third, what is the association between vigorous physical activity and preterm birth or birthweight? Our objective was to address these questions in a large pregnancy cohort, Right From the Start (RFTS).
Methods
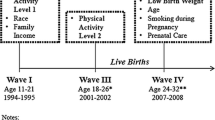
RFTS is an ongoing investigation of early pregnancy health. The study includes three waves of enrollment (RFTS1, 2 and 3). The physical activity questions differed slightly between waves 1 and 2/3, and thus only RFTS2/3 are included in this analysis. RFTS2/3 enrolled women from central North Carolina from 2004 to 2007.
RFTS invited women to participate through advertisements and community outreach. Study materials encouraged women planning a pregnancy or in early pregnancy to contact study staff through a toll free phone number. The recruitment methodology of RFTS2/3 is similar to that of RFTS1 and has been described previously [28]. The study was approved by the Institutional Review Boards of the University of North Carolina and Vanderbilt University.
When women called to volunteer, study staff screened them to determine eligibility and, if eligible, collected each woman’s age and pre-pregnancy weight. Women were eligible if they were currently trying to conceive or had been pregnant less than 10 weeks based on self-report of their last menstrual period. Women also had to be at least 18 years of age, conceiving without assisted reproductive technology, willing to have a first trimester ultrasound at one of the study’s ultrasound locations, intending to remain in the area for the next 18 months, intending to carry the pregnancy to term, able to access a telephone for the first trimester interview, fluent in either English or Spanish, and able to identify a prenatal or primary care provider at the time of screening. This portion of the study included 1,861 live births beyond 20 completed weeks of gestation. We further restricted eligibility to the first pregnancy among women who participated in RFTS2/3 more than once (N = 1,735), singleton gestations (N = 1,708), and women who completed the first trimester interview (N = 1,647). Compared to women who completed the first trimester interview (N = 1,647), women who did not complete the interview (N = 61) were more likely to be under 30 years of age (67% vs. 48%), Black Non-Hispanic (30% vs. 12%), unmarried (39% vs. 6%), obese (21% vs. 16%), and have less than a college education (56% vs. 24%).
Outcomes
Multiple data sources were used to obtain and confirm infant date of birth. The hierarchy of the sources was hospital discharge summaries and prenatal care records (51%), birth and fetal death records (32%), and participant self-report (17%). Birthweight was obtained from vital record linkage for all participants. Gestational age at birth was estimated based on last menstrual period and corrected to the first trimester ultrasound estimate only if the difference between the 2 was more than 7 days. The ultrasound was performed between 6 and 12 weeks of gestation.
Physical Activity
In a telephone interview targeted for 14 weeks gestation (mean and median: 14 weeks, range: 7–20 weeks), women were asked to describe their physical activities by mode (recreational, occupational, indoor/outdoor household and child/adult care). This questionnaire was based on a modified version of a structured 7 day recall, with evidence for validity and reliability among pregnant women [29]. Women were asked to report if they do any “hard” or “very hard” recreational physical activities in a typical week. The description “hard or very hard” is a measure of vigorous intensity based on the Borg perceived exertion scale which has been found to correlate strongly with heart rate and oxygen uptake [30]. Participants were then asked to describe the type of activity and how often and for how long they performed the activity. Women who reported engaging in recreational activity but did not describe it as “hard” or “very hard” were considered to engage in non-vigorous recreational activity.
Occupational, indoor/outdoor household, and child/adult care physical activities were assessed with analogous questions and similarly coded. Occupational activities included lifting or carrying boxes and lifting and transporting patients. Examples of household activities included washing, folding, and carrying laundry, vacuuming, washing floors, and gardening. Examples of child/adult care activities included lifting and carrying children, bathing children, and lifting or transporting adults.
We summed the minutes per week of each recreational activity (i.e., jogging + swimming + walking) to obtain the total minutes per week of vigorous recreational activity. Similarly, we summed the minutes per week of each activity, within each of the other modes, to obtain the total minutes of vigorous occupational, household, and child/adult care activity, respectively. Finally, we summed over all modes to obtain the total minutes of vigorous physical activity.
Metabolic equivalent (MET) values were assigned to recreational activities only, based on the Compendium of Physical Activities [31]. The Compendium (originally published in 1993 [32], updated in 2000 [31]) was developed to compare the intensities of different physical activities across participants. We multiplied the MET value for a given activity by the minutes per week of that activity and summed across activities to obtain total MET-minutes per week. METs were assigned by the first author (AMZJ) and reviewed by the second author (KRE). MET values are a measure of absolute intensity while the participants’ categorization of an activity as “hard or very hard” is a measure of perceived or relative intensity. Thus our analysis contained two assessments of intensity. MET values have not been measured in pregnant populations and thus may not be accurate for pregnant women. Given the numerous physiologic and metabolic changes that occur during pregnancy it is possible that the woman’s characterization of the intensity of the activity is more accurate than MET values assigned to a given activity. Therefore, our presentation of results focused on perceived intensity and we present the results based on absolute intensity (MET values) only where they differed from the perceived intensity results.
The cumulative frequency of vigorous recreational activity sessions per week was calculated as the sum of the individual frequencies reported for each activity. For example, if a woman reported walking three times per week and swimming two times per week her cumulative frequency would be five sessions per week. The average duration of a recreational activity session was calculated by dividing the total reported minutes per week of vigorous recreational activity by the cumulative frequency of vigorous activity sessions. From the previous example, if she reported 60 min of walking per week and 40 min of swimming per week she would be assigned an average duration of 100/5 = 20 min/session.
Women were also asked to report if their overall current physical activity had increased, decreased or stayed the same compared with pre-pregnancy activity.
They were also asked if they changed their behaviors in preparation for becoming pregnant. If she answered affirmatively she was asked what she changed. The interviewer did not read a list of responses, but some women responded that they started exercising and these responses were coded. A woman could give multiple responses.
Covariates
The screening interview and the telephone interview collected information on important covariates including sociodemographics, reproductive history, presence of nausea and vomiting in early pregnancy, and lifestyle factors. Weight and height were measured at the first trimester ultrasound. If this measure was missing, then her self-reported weight and height from the first trimester questionnaire were used.
Covariates for these analyses were chosen if they were considered to be potential confounders based on directed acyclic graphs [33] constructed for each outcome. In all models, we considered adjustment for maternal age, race/ethnicity, education, income, marital status, alcohol consumption, body mass index, cigarette smoking, illicit drug use, history of miscarriage, history of preterm birth, parity, vaginal bleeding, nausea/vomiting, and history of any type of diabetes. These variables were included in the models if their removal changed the estimates by more than 10% for the preterm birth and 20% for birthweight.
Behavioral characteristics were reported in the first trimester questionnaire. Current smokers include women who were smoking at the time of interview and who reported quitting in the previous 4 months. Former smokers were women who reported quitting at least 4 months prior to the questionnaire. Alcohol use was categorized into women who have never used alcohol, current users, those who stopped drinking within 4 months of interview and those who stopped drinking more than 4 months from the interview.
Statistical Analysis
Analyses were performed with SAS software, version 9.1. We used a standard multivariable logistic regression to examine the association between physical activity and preterm birth as a dichotomous variable (<37 completed weeks of gestation). For comparison with previous studies we also evaluated the association between physical activity and length of gestation using a discrete time survival model [34]. We examined time-varying associations (i.e., those interacting with gestational age) in the full model but none were significant (group P > 0.1).
Among term births, we used a linear regression model to examine physical activity and birthweight, adjusted for gestational week at birth. Birthweight in preterm infants can reflect either their prematurity or growth restriction or both. Because the outcome is heterogeneous in preterm infants, we limited our analysis of birthweight to term infants. To improve the precision of our birthweight model, we included two strong predictors, maternal height and infant gender. The other outcomes were not modeled with linear regression, and thus adjustment for non-confounders is not warranted [35].
Continuous variables, including our exposures of interest, were finely categorized and examined with each outcome variable in an unadjusted analysis. The shape of the crude association of each variable with each outcome was visually inspected to determine the appropriate structure (linear, quadratic, categorical) and, if categorical, the number and location of cutpoints. More parsimonious models with fewer parameters were compared to the full model containing the highly categorized variables. Fewer parameters were used if information was not lost when compared to the highly parameterized model (likelihood ratio test P value >0.05). For each mode of vigorous physical activity (recreational, occupational, household and child/adult care) the minutes of activity were categorized into tertiles, resulting in five categories: no activity, non-vigorous activity, and tertiles of the minutes of vigorous activity. The total minutes of vigorous physical activity was divided into five categories: no physical activity reported or only non-vigorous activity reported, and four categories of the total minutes of vigorous activity. We combined the “none” and “non-vigorous” categories because the number of women who reported no physical activity in any mode was small (2%).
For vigorous recreational physical activity only, we conducted separate multivariable analyses for perceived intensity (minutes per week) and absolute intensity (MET-minutes per week), duration of vigorous recreational activity session, and frequency of vigorous recreational activity sessions. Duration and frequency were modeled separately and both were adjusted for the total minutes of recreational activity (as recommended by Lee and Skerret [36]), the previously described covariates, and the other modes of physical activity (household, occupational, child/adult care). Women who performed 0 min of recreational activity also had a frequency of zero recreational activity sessions per week. To avoid collinearity, women with a frequency of zero or one were combined to form the lowest frequency category. A similar strategy was employed with duration of recreational activity.
Results
Of the 1,647 live births, 108 (7%) were born preterm. The majority of this cohort was 25–34 years of age (71%), white non-Hispanic (78%), college graduates (76%), married (94%), non-smokers (76%), and non-drug users (97%) (Table 1).
Vigorous physical activity typically corresponds to a MET value of at least six [27]. The median MET value assigned to the recreational activities using absolute intensity measures from the compendium [31] was 5.5 (interquartile range (IQR): 3.3, 7), suggesting that the median perceived intensity of the activities was higher than the corresponding median MET value of the activity.
Only 35% of the women in this cohort performed first-trimester vigorous physical activity. The average total vigorous activity reported was 76 min/week (Table 1). Recreational activity was the most common mode of physical activity accounting for 38% of the total minutes of vigorous activity in the cohort, followed by child/adult care activity (29%).
Length of Gestation
Preterm births were more frequent among black, non-Hispanic women (15%) compared with white non-Hispanic women (6%), Hispanic women (7%) and women grouped in “Other” racial groups (1%). Women who performed first-trimester vigorous recreational activity tended to have lower odds of preterm birth (Table 2). This was also true when considering absolute intensity (MET-minutes per week) (data not shown). The results of the survival analysis were similar; the hazard ratio for any vigorous recreational activity compared with none was 0.85 (95% confidence interval (CI) 0.70, 1.05) (data not shown). We did not find any dose–response association (Appendix 1). The odds of preterm birth were also lower with increasing frequency of first-trimester vigorous recreational activity sessions. This association persisted despite adjustment for total volume of recreational activity (Table 2). None of the other modes of first-trimester physical activity (occupational, household, child/adult care), nor total first-trimester physical activity were associated with length of gestation or preterm birth.
Birthweight
Birthweight was obtained from vital records and examined among term births (N = 1,539). A confirmed match could not be found for 23% of these births. Compared with women who had birthweight information (N = 1,184), women missing birthweight (N = 355) were more likely to be Hispanic (11% vs. 4%), to report an income ≤$40,000 (29% vs. 21%), to report never using alcohol (21% vs. 13%), and to report their physical activity stayed the same (37% vs. 32%) or increased (5% vs. 3%) relative to pre-pregnancy. Women missing birthweight information did not differ by any first-trimester physical activity measures.
Of the 1,184 term births with birthweight information, 14 (1%) were low birthweight (<2,500 g). White non-Hispanic women had the heaviest infants (mean birthweight = 3,549 g) followed by Hispanic women, 3,488 g, and other race women, 3,387 g. Black non-Hispanic women gave birth to the lightest infants, 3,310 g. Women who performed first-trimester vigorous recreational activity tended to have lighter babies, but this was not statistically significant (P = 0.08) (Table 3). We did not see a dose–response association (Appendix 2). None of the other first-trimester physical activity measures were associated with birthweight (Table 3).
Sensitivity Analyses
A woman’s physical activity in the first pregnancy may have influenced her first pregnancy outcome. If the woman tended to perform the same physical activities across pregnancies, controlling for previous pregnancy outcome would, in effect, be controlling for the exposure. To address this, we examined our multivariable results without pregnancy history variables (history of miscarriage or preterm birth and parity). When we did this, child and adult care activity estimates were generally strengthened possibly because care activity was confounded by parity. Because none of the other estimates meaningfully changed when pregnancy history variables were excluded, we retained them in the final models which were presented in Tables 2 and 3. Similarly, we examined our results without controlling for nausea/vomiting and vaginal bleeding; estimates were unchanged and these variables were retained.
Women could have reported their physical activities in an unexpected category (i.e., a woman reported laundry as a recreational activity instead of a household activity). If this is the case, controlling for other modes of physical activity (i.e., controlling household activity for recreational activity) may be an over-adjustment. We examined each mode of activity without controlling for the other modes and results did not meaningfully change.
Discussion
We found no evidence that first-trimester vigorous recreational physical activity was associated with adverse changes in length of gestation. Previous studies suggest that recreational physical activity is either not associated [37–50] or associated with lower risk of preterm birth [51–57]. When limited to studies that have measured frequency, intensity, duration, and type of activity the results suggest reduced risk of preterm birth [50, 53, 54, 56–61]. Of these studies, the most precise estimate was from a survival analysis (hazard ratio: 0.82 [95% CI: 0.76, 0.88] for any exercise vs. none) and the authors found no dose–response association [60]. Our survival analysis results were nearly identical (0.85 [0.70, 1.05]).
We found that frequency of first-trimester recreational activity sessions was associated with reduced risk of preterm birth. We did not find any studies that examined the associations between components of recreational activity (duration and frequency) with preterm birth while controlling for total volume of recreational activity, as we have done.
Recreational activity may benefit pregnancy through placental development. Continuing to exercise during pregnancy has been associated with greater placental villous vascular volume and a higher proliferation index [62]. Moreover, intermittent changes in oxygen or nutrient delivery to the placenta may stimulate placental growth [63]. A recreational activity session could be associated with a decrease in nutrient delivery to the placenta, which would be followed by an increase as the woman recovers. The more frequent recreational activity sessions are, the more fluctuation there will be in nutrient delivery to the placenta, which may stimulate placental growth. This is intriguing given that frequency of vigorous activity sessions was associated with lower odds of preterm birth in our analysis.
Women who performed recreational activity tended to have lighter babies. Several previous studies reported no association [38, 39, 42, 46, 47, 64] or an increase in birthweight with recreational activity [41, 65]; however, these studies did not account for gestational age. We restricted our analysis of birthweight to term infants and also adjusted for gestational week. Of the earlier studies that adjusted for gestational age, three reported higher birthweight for babies of mothers who perform recreational activity [43, 55, 66], four others reported a decrease [67–70] and three reported no association [71–73]. These studies include mostly recreational activities, although some have combined recreational with occupational, child care, or housework activities [47, 55, 69, 73]. A recent randomized trial found that women who participated in a stationary cycling program from 20 weeks of gestation to delivery gave birth to babies that were lighter (about 140 g) than babies of control women [50].
We did not find convincing associations of vigorous first-trimester occupational, household, or child/adult care activities with any of the birth outcomes. These modes of physical activity could differ from recreational activity because they may not be volitional. One study examined household or child/adult care activities as separate exposures and suggested no association with preterm birth [52]. A recent Brazilian study suggested a reduced risk of preterm birth with increasing hours per day of domestic activity [61]. Odds ratio estimates from studies of occupational physical activity and preterm birth range from 0.7 to 4, with most less than 2 [24]. Two of five occupational activity studies suggest increased risk of small-for-gestational age birth [55, 74–77]. These studies vary widely in terms of their occupational activity measures and do not usually include detailed assessments of intensity, frequency, and duration of physical activity.
Limitations and Strengths
This study recruited women early in pregnancy and prospectively ascertained their pregnancy outcomes. The participants were volunteers planning a pregnancy and our results may not be generalizable to other populations. Birthweight was obtained from a vital records match, which lead to a substantial proportion of missing data (23%); however, missing birthweight data was not associated with physical activity, reducing the likelihood of bias. Physical activity was assessed through self-report early in pregnancy. Women were asked several detailed questions to describe their vigorous physical activities which should have reduced exposure misclassification. The physical activity questionnaire we used in modified form had moderate to almost perfect evidence for test–retest reliability and moderate to substantial evidence for validity when compared to a structured diary among a sample of pregnant women [29]. However, like many other self-report questionnaires on physical activity, the correlations between the accelerometer and questionnaire were only fair for most assessments. Moderate intensity activities, which are recommended during pregnancy [26, 27], were not measured in detail. Because the physical activity questions were asked early in pregnancy (around 14 weeks gestation) they may not reflect the appropriate exposure window in pregnancy for effects on timing of birth or birthweight. However, the responses at this point in pregnancy would not have been affected by the manifestation of some conditions that commonly lead to medically indicated preterm birth (pre-eclampsia, hypertension). Thus, our exposure measurement is less susceptible to reverse causality.
The detailed exposure measurements allowed us to examine the modes of vigorous physical activity as well as frequency and duration of vigorous recreational activities as separate exposures, which has not been reported previously in the literature. The physical activity recommendations from the American College of Obstetricians and Gynecologists [26] and the US Department of Health and Human Services [27] do not currently specify safe amounts of vigorous activity.
Conclusion
In summary, first-trimester vigorous physical activity does not appear to be detrimental to the timing of birth or birthweight. Our data support a reduced risk of preterm birth with first-trimester vigorous recreational activity, particularly with increased frequency of vigorous recreational activity sessions. Further investigation of the modes of physical activity will clarify if recreational activity differs from other activity types. Additionally, future studies should investigate intensity, duration, and frequency of physical activity sessions, controlling for total volume of physical activity.
References
Martin, J. A., Hamilton, B. E., Sutton, P. D., Ventura, S. J., Menacker, F., Kirmeyer, S., et al. (2009). Births: Final data for 2006. Natational Vital Statics Report, 57(7). Accessed at http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_07.pdf.
Shapiro-Mendoza, C. K., Tomashek, K. M., Kotelchuck, M., Barfield, W., Nannini, A., Weiss, J., et al. (2008). Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics, 121(2), e223–e232.
Tomashek, K. M., Shapiro-Mendoza, C. K., Davidoff, M. J., & Petrini, J. R. (2007). Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. Journal of Pediatrics, 151(5), 450–456.
Underwood, M. A., Danielsen, B., & Gilbert, W. M. (2007). Cost, causes and rates of rehospitalization of preterm infants. Journal of Perinatology, 27(10), 614–619.
Hohimer, A. R., Bissonnette, J. M., Metcalfe, J., & McKean, T. A. (1984). Effect of exercise on uterine blood flow in the pregnant Pygmy goat. American Journal of Physiology, 246(2 Pt 2), H207–H212.
Lotgering, F. K., Gilbert, R. D., & Longo, L. D. (1983). Exercise responses in pregnant sheep: Oxygen consumption, uterine blood flow, and blood volume. Journal of Applied Physiology, 55(3), 834–841.
Nesbitt, A. E., Murphy, R. J., & O’Hagan, K. P. (2005). Effect of gestational stage on uterine artery blood flow during exercise in rabbits. Journal of Applied Physiology, 99(6), 2159–2165.
O’Hagan, K. P., & Alberts, J. A. (2003). Uterine artery blood flow and renal sympathetic nerve activity during exercise in rabbit pregnancy. American Journal of Physiology: Regulatory, Integrative and Comparative Physiology, 285(5), R1135–R1144.
Baumann, H., Huch, A., & Huch, R. (1989). Doppler sonographic evaluation of exercise-induced blood flow velocity and waveform changes in fetal, uteroplacental and large maternal vessels in pregnant women. Journal of Perinatal Medicine, 17(4), 279–287.
Erkkola, R. U., Pirhonen, J. P., & Kivijarvi, A. K. (1992). Flow velocity waveforms in uterine and umbilical arteries during submaximal bicycle exercise in normal pregnancy. Obstetrics and Gynecology, 79(4), 611–615.
Rauramo, I., & Forss, M. (1988). Effect of exercise on maternal hemodynamics and placental blood flow in healthy women. Acta Obstetrics and Gynecology Scandinavian, 67(1), 21–25.
Brenner, I. K., Wolfe, L. A., Monga, M., & McGrath, M. J. (1999). Physical conditioning effects on fetal heart rate responses to graded maternal exercise. Medicine and Science in Sports and Exercise, 31(6), 792–799.
Kennelly, M. M., Geary, M., McCaffrey, N., McLoughlin, P., Staines, A., & McKenna, P. (2002). Exercise-related changes in umbilical and uterine artery waveforms as assessed by Doppler ultrasound scans. American Journal of Obstetrics and Gynecology, 187(3), 661–666.
Kennelly, M. M., McCaffrey, N., McLoughlin, P., Lyons, S., & McKenna, P. (2002). Fetal heart rate response to strenuous maternal exercise: Not a predictor of fetal distress. American Journal of Obstetrics and Gynecology, 187(3), 811–816.
McMurray, R. G., Katz, V. L., Poe, M. P., & Hackney, A. C. (1995). Maternal and fetal responses to low-impact aerobic dance. American Journal of Perinatology, 12(4), 282–285.
Morrow, R. J., Ritchie, J. W., & Bull, S. B. (1989). Fetal and maternal hemodynamic responses to exercise in pregnancy assessed by Doppler ultrasonography. American Journal of Obstetrics and Gynecology, 160(1), 138–140.
Lindqvist, P. G., Marsal, K., Merlo, J., & Pirhonen, J. P. (2003). Thermal response to submaximal exercise before, during and after pregnancy: A longitudinal study. The Journal of Matern-Fetal Neonatal Medicine, 13(3), 152–156.
Bonen, A., Campagna, P., Gilchrist, L., Young, D. C., & Beresford, P. (1992). Substrate and endocrine responses during exercise at selected stages of pregnancy. Journal of Applied Physiology, 73(1), 134–142.
Bonen, A., Campagna, P. D., Gilchrist, L., & Beresford, P. (1995). Substrate and hormonal responses during exercise classes at selected stages of pregnancy. Canadian Journal of Applied Physiology, 20(4), 440–451.
Clapp, J. F., I I I, Wesley, M., & Sleamaker, R. H. (1987). Thermoregulatory and metabolic responses to jogging prior to and during pregnancy. Medicine and Science in Sports and Exercise, 19(2), 124–130.
McMurray, R. G., Hackney, A. C., Guion, W. K., & Katz, V. L. (1996). Metabolic and hormonal responses to low-impact aerobic dance during pregnancy. Medicine and Science in Sports and Exercise, 28(1), 41–46.
Cunningham, F. G., Gilstrap, L. C., I. I. I., Gant, N. F., Hauth, J. C., Wenstrom, K. D., & Leveno, K. J. (2001). Williams obstetrics (21st ed.). New York: McGraw-Hill, Medical Publishing Division.
Chasan-Taber, L., Evenson, K. R., Sternfeld, B., & Kengeri, S. (2007). Assessment of recreational physical activity during pregnancy in epidemiologic studies of birthweight and length of gestation: Methodologic aspects. Women and Health, 45(4), 85–107.
Bonzini, M., Coggon, D., & Palmer, K. T. (2007). Risk of prematurity, low birthweight and pre-eclampsia in relation to working hours and physical activities: A systematic review. Occupational and Environmental Medicine, 64(4), 228–243.
Kramer, M. S., & McDonald, S. W. (2006). Aerobic exercise for women during pregnancy. The Cochrane Database of Systematic Reviews, 3, CD000180.
ACOG Committee Opinion. (2002). Number 267, January 2002: Exercise during pregnancy and the postpartum period. Obstetrics and Gynecology, 99(1), 171–173.
US Department of Health and Human Services. (2008). 2008 Physical activity guidelines for Americans. In Department of Health and Human Services, p. 61.
Promislow, J. H., Makarushka, C. M., Gorman, J. R., Howards, P. P., Savitz, D. A., & Hartmann, K. E. (2004). Recruitment for a community-based study of early pregnancy: The Right from the Start Study. Pediatric and Perinatal Epidemiology, 18(2), 143–152.
Evenson, K., & Wen, F. (2010). Measuring physical activity among pregnant women using a structured one-week recall questionnaire: Evidence for validity and reliability. International Journal of Behavioral Nutrition Physical Activity, 7(1), 21.
Borg, G. A. (1982). Psychophysical bases of perceived exertion. Medicine and Science in Sports and Exercise, 14(5), 377–381.
Ainsworth, B. E., Haskell, W. L., Whitt, M. C., Irwin, M. L., Swartz, A. M., Strath, S. J., et al. (2000). Compendium of physical activities: An update of activity codes and MET intensities. Medicine and Science in Sports and Exercise, 32(9 Suppl), S498–S504.
Ainsworth, B. E., Haskell, W. L., Leon, A. S., Jacobs, D. R., Jr., Montoye, H. J., Sallis, J. F., et al. (1993). Compendium of physical activities: Classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise, 25(1), 71–80.
Greenland, S., Pearl, J., & Robins, J. M. (1999). Causal diagrams for epidemiologic research. Epidemiology, 10(1), 37–48.
Cole, S. R., & Ananth, C. V. (2001). Regression models for unconstrained, partially or fully constrained continuation odds ratios. International Journal of Epidemiology, 30(6), 1379–1382.
Robinson, L. D., & Jewell, N. P. (1991). Some surprising results about covariate adjustment in logistic-regression models. International Statistical Review, 59(2), 227–240.
Lee, I. M., & Skerrett, P. J. (2001). Physical activity and all-cause mortality: What is the dose-response relation? Medicine and Science in Sports and Exercise, 33(6 Suppl), S459–S71; discussion S493–S494.
Alderman, B. W., Zhao, H., Holt, V. L., Watts, D. H., & Beresford, S. A. (1998). Maternal physical activity in pregnancy and infant size for gestational age. Annals of Epidemiology, 8(8), 513–519.
Botkin, C., & Driscoll, C. E. (1991). Maternal aerobic exercise: Newborn effects. The Family Practice Research Journal, 11(4), 387–393.
Duncombe, D., Skouteris, H., Wertheim, E. H., Kelly, L., Fraser, V., & Paxton, S. J. (2006). Vigorous exercise and birth outcomes in a sample of recreational exercisers: A prospective study across pregnancy. The Australian & New Zealand Journal of Obstetrics & Gynaecology, 46(4), 288–292.
Haas, J. S., Fuentes-Afflick, E., Stewart, A. L., Jackson, R. A., Dean, M. L., Brawarsky, P., et al. (2005). Prepregnancy health status and the risk of preterm delivery. Archives of Pediatrics and Adolescent Medicine, 159(1), 58–63.
Hall, D. C., & Kaufmann, D. A. (1987). Effects of aerobic and strength conditioning on pregnancy outcomes. American Journal of Obstetrics and Gynecology, 157(5), 1199–1203.
Horns, P. N., Ratcliffe, L. P., Leggett, J. C., & Swanson, M. S. (1996). Pregnancy outcomes among active and sedentary primiparous women. Journal of Obstetrics, Gynecology and Neonatal Nursing, 25(1), 49–54.
Leiferman, J. A., & Evenson, K. R. (2003). The effect of regular leisure physical activity on birth outcomes. Matern and Child Health Journal, 7(1), 59–64.
Lokey, E. A., Tran, Z. V., Wells, C. L., Myers, B. C., & Tran, A. C. (1991). Effects of physical exercise on pregnancy outcomes: A meta-analytic review. Medicine and Science in Sports and Exercise, 23(11), 1234–1239.
Orr, S. T., James, S. A., Garry, J., Prince, C. B., & Newton, E. R. (2006). Exercise and pregnancy outcome among urban, low-income, black women. Ethnicity and Disease, 16(4), 933–937.
Rice, P. L., & Fort, I. L. (1991). The relationship of maternal exercise on labor, delivery and health of the newborn. The Journal of Sports Medicine and Physical Fitness, 31(1), 95–99.
Rose, N. C., Haddow, J. E., Palomaki, G. E., & Knight, G. J. (1991). Self-rated physical activity level during the second trimester and pregnancy outcome. Obstetrics and Gynecology, 78(6), 1078–1080.
Sternfeld, B., Quesenberry, C. P., Jr., Eskenazi, B., & Newman, L. A. (1995). Exercise during pregnancy and pregnancy outcome. Medicine and Science in Sports and Exercise, 27(5), 634–640.
Both, M. I., Overvest, M. A., Wildhagen, M. F., Golding, J., & Wildschut, H. I. (2010). The association of daily physical activity and birth outcome: A population-based cohort study. European Journal of Epidemiology, 25(6), 421–429.
Hopkins, S. A., Baldi, J. C., Cutfield, W. S., McCowan, L., & Hofman, P. L. (2010). Exercise training in pregnancy reduces offspring size without changes in maternal insulin sensitivity. The Journal of Clinical Endocrinology and Metabolism, 95(5), 2080–2088.
Badr, L. K., Abdallah, B., & Mahmoud, A. (2005). Precursors of preterm birth: Comparison of three ethnic groups in the middle East and the United States. Journal of Obstetrics, Gynecology and Neonatal Nursing, 34(4), 444–452.
Berkowitz, G. S., Kelsey, J. L., Holford, T. R., & Berkowitz, R. L. (1983). Physical activity and the risk of spontaneous preterm delivery. The Journal of Reproductive Medicine, 28(9), 581–588.
Evenson, K. R., Siega-Riz, A. M., Savitz, D. A., Leiferman, J. A., & Thorp, J. M., Jr. (2002). Vigorous leisure activity and pregnancy outcome. Epidemiology, 13(6), 653–659.
Hatch, M., Levin, B., Shu, X. O., & Susser, M. (1998). Maternal leisure-time exercise and timely delivery. American Journal of Public Health, 88(10), 1528–1533.
Magann, E. F., Evans, S. F., & Newnham, J. P. (1996). Employment, exertion, and pregnancy outcome: Assessment by kilocalories expended each day. American Journal of Obstetrics and Gynecology, 175(1), 182–187.
Misra, D. P., Strobino, D. M., Stashinko, E. E., Nagey, D. A., & Nanda, J. (1998). Effects of physical activity on preterm birth. American Journal of Epidemiology, 147(7), 628–635.
Juhl, M., Kogevinas, M., Andersen, P. K., Andersen, A. M., & Olsen, J. (2010). Is swimming during pregnancy a safe exercise? Epidemiology, 21(2), 253–258.
Domingues, M. R., Barros, A. J., & Matijasevich, A. (2008). Leisure time physical activity during pregnancy and preterm birth in Brazil. International Journal of Gynaecology and Obstetrics, 103(1), 9–15.
Hegaard, H. K., Hedegaard, M., Damm, P., Ottesen, B., Petersson, K., & Henriksen, T. B. (2008). Leisure time physical activity is associated with a reduced risk of preterm delivery. American Journal of Obstetrics and Gynecology, 198(2), 180e1–180e5.
Juhl, M., Andersen, P. K., Olsen, J., Madsen, M., Jorgensen, T., Nohr, E. A., et al. (2008). Physical exercise during pregnancy and the risk of preterm birth: A study within the Danish National Birth Cohort. American Journal of Epidemiology, 167(7), 859–866.
Takito, M. Y., & Benicio, M. H. (2010). Physical activity during pregnancy and fetal outcomes: A case-control study. Revista de Saude Publica, 44(1), 90–101.
Bergmann, A., Zygmunt, M., & Clapp, J. F., I. I. I. (2004). Running throughout pregnancy: Effect on placental villous vascular volume and cell proliferation. Placenta, 25(8–9), 694–698.
Clapp, J. F. (2006). Influence of endurance exercise and diet on human placental development and fetal growth. Placenta, 27(6–7), 527–534.
Nieuwenhuijsen, M. J., Northstone, K., & Golding, J. (2002). Swimming and birth weight. Epidemiology, 13(6), 725–728.
Collings, C. A., Curet, L. B., & Mullin, J. P. (1983). Maternal and fetal responses to a maternal aerobic exercise program. American Journal of Obstetrics and Gynecology, 145(6), 702–707.
Hatch, M. C., Shu, X. O., McLean, D. E., Levin, B., Begg, M., Reuss, L., et al. (1993). Maternal exercise during pregnancy, physical fitness, and fetal growth. American Journal of Epidemiology, 137(10), 1105–1114.
Campbell, M. K., & Mottola, M. F. (2001). Recreational exercise and occupational activity during pregnancy and birth weight: A case-control study. American Journal of Obstetrics and Gynecology, 184(3), 403–408.
Clapp, J. F., I. I. I., & Capeless, E. L. (1990). Neonatal morphometrics after endurance exercise during pregnancy. American Journal of Obstetrics and Gynecology, 163(6 Pt 1), 1805–1811.
Perkins, C. C., Pivarnik, J. M., Paneth, N., & Stein, A. D. (2007). Physical activity and fetal growth during pregnancy. Obstetrics and Gynecology, 109(1), 81–87.
Juhl, M., Olsen, J., Andersen, P. K., Nohr, E. A., & Andersen, A. M. (2010). Physical exercise during pregnancy and fetal growth measures: A study within the Danish National Birth Cohort. American Journal of Obstetrics and Gynecology, 202(1), 63e1–63e8.
Hegaard, H. K., Petersson, K., Hedegaard, M., Ottesen, B., Dykes, A. K., Henriksen, T. B., et al. (2009). Sports and leisure-time physical activity in pregnancy and birth weight: A population-based study. Scandinavian Journal of Medicine and Science in Sports, 20(1), e96–e102.
Kardel, K. R., & Kase, T. (1998). Training in pregnant women: Effects on fetal development and birth. American Journal of Obstetrics and Gynecology, 178(2), 280–286.
Klebanoff, M. A., Shiono, P. H., & Carey, J. C. (1990). The effect of physical activity during pregnancy on preterm delivery and birth weight. American Journal of Obstetrics and Gynecology, 163(5 Pt 1), 1450–1456.
Fortier, I., Marcoux, S., & Brisson, J. (1995). Maternal work during pregnancy and the risks of delivering a small-for-gestational-age or preterm infant. Scandinavian Journal of Work, Environment & Health, 21(6), 412–418.
Launer, L. J., Villar, J., Kestler, E., & de Onis, M. (1990). The effect of maternal work on fetal growth and duration of pregnancy: A prospective study. British Journal of Obstetrics Gynaecology, 97(1), 62–70.
Nurminen, T., Lusa, S., Ilmarinen, J., & Kurppa, K. (1989). Physical work load, fetal development and course of pregnancy. Scandinavian Journal of Work, Environment & Health, 15(6), 404–414.
Tuntiseranee, P., Geater, A., Chongsuvivatwong, V., & Kor-anantakul, O. (1998). The effect of heavy maternal workload on fetal growth retardation and preterm delivery. A study among southern Thai women. J Occupational and Environmental Medicine, 40(11), 1013–1021.
Acknowledgments
This research was supported, in part, by the Intramural Research Program of the National Institute of Health (NIH), National Institute of Environmental Health Sciences (NIEHS). The related components of the parent study, Right From the Start, were funded by NIH, National Institute of Child Health and Development RO1HD043883 and RO1HD049675. This work was also supported in part by NIH/NIEHS T32ES007018 and NIH/NIEHS P30ES10126. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We would like to thank Dr. Olga Basso and Dr. Shannon Laughlin for their insightful comments.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
See Table 4.
Appendix 2
See Table 5.
Rights and permissions
About this article
Cite this article
Jukic, A.M.Z., Evenson, K.R., Daniels, J.L. et al. A Prospective Study of the Association Between Vigorous Physical Activity During Pregnancy and Length of Gestation and Birthweight. Matern Child Health J 16, 1031–1044 (2012). https://doi.org/10.1007/s10995-011-0831-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-011-0831-8