Abstract
Objectives
A growing body of evidence suggests an association between maternal infection and preeclampsia. To examine the strength of this association, we conducted a comprehensive review of studies published in peer-reviewed journals.
Methods
Data collection for this review involved Medline, Embase, and Cochrane data base searches of published studies since 1964 on the relationship between maternal infection and preeclampsia. Data were abstracted according to predefined inclusion and exclusion criteria. Study population included women with preeclampsia and normotensive mothers with and without bacterial or viral infections. Altogether, thirty two original studies were identified and evaluated for methodological quality, preeclampsia diagnosis and adjustment for well-known preeclampsia confounders. Pooled odds ratios and 95% confidence intervals, according to infection status, were calculated using DerSimonian-Laird random-effects models. Publication bias was assessed with a funnel plot and Egger’s regression asymmetry test.
Results
Sixteen of the 32 studies evaluated were selected for inclusion in the meta-analysis. These studies showed that women with either a bacterial or viral infection were at higher risk of developing preeclampsia, compared to women without infection. Combined results for the 16 studies yielded an OR of 2.1 (95% CI 1.6–2.7). Separate pooled estimates for prospective (OR 2.3, 95% CI 1.7–3.0), case control and retrospective studies combined (OR 2.0, 95% CI 1.4–2.9) yielded similar results. Heterogeneity was significant across overall pooled estimates, case control and retrospective studies (Qdf=20 of 45.7, P = .001; Qdf=10 of 38.7, P < .005, respectively), but not prospective studies (Qdf=9 of 6.5 P = .69).
Conclusions
In our analysis, any infection (bacterial or viral) was associated with a two-fold higher risk of preeclampsia. This association may provide a potential explanation for preeclampsia-related inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia is a multi-systemic disorder of human pregnancy complicating 2–8% of the obstetric population [1], and may result from deficient placental implantation during the first half of pregnancy [2]. Preeclampsia is characterized by new onset hypertension and proteinuria after 20th week of gestation in a previously normotensive woman, and is associated with significant maternal mortality and morbidity in the United States and world-wide [2–3]. Despite its seriousness and public health relevance, the cause of preeclampsia remains unknown. It has been hypothesized that the clinical manifestations of preeclampsia, including hypertension, oxidative stress, and proteinuria could be explained by a generalized maternal endothelium dysfunction [4]. Redman et al. extended this hypothesis further by proposing that inflammation provides the oxidative insult to the endothelium seen in preeclampsia [5]. It is unclear, however, whether inflammation occurs before development of preeclampsia or is a consequence of the disease itself. Although studies have demonstrated evidence for an inflammatory response both in normal and preeclamptic pregnancies, in preeclampsia inflammation seems excessive. For example, a number of studies have found increased levels of inflammatory cytokines, such as prostaglandin E2 (PGE2), tumor necrosis factor (TNF)-α, interleukin 1 (IL-1), interleukin 6 (IL-6), soluble phospholipase A2, activated clotting and complement pathways, as well as C-reactive protein (CRP) at higher levels in women with preeclampsia compared to normotensive pregnancies [6–13].
In the last twenty years, several epidemiological studies have assessed the association between maternal infections and preeclampsia. We conducted a comprehensive review of these studies to evaluate the evidence for this association. To our knowledge, no systematic review has been conducted before of the potential relationship between maternal infections and preeclampsia. With a meta-analysis we can pool results of a number of studies, thereby increasing statistical power. Although typically used in clinical trials, meta-analytic techniques can also be employed in observational studies [14].
Methods
Search strategy and selection criteria
We searched MEDLINE, Cochrane, and Embase databases using the following search words: “infection and preeclampsia”, “bacterial infection and preeclampsia,” “viral infection and preeclampsia,” and “periodontal disease and preeclampsia.” Publications in English, Spanish and German published between 1964 and August 2006 were considered.
Additional manual searches were conducted of reference lists obtained from these publications. All work followed guidelines proposed by the Meta-Analysis of Observational Studies in Epidemiology Group [15].
Inclusion criteria were: (1) cohort, case-control, and cross-sectional study designs, (2) study had to contain original data, (3) well-defined preeclampsia diagnosis, (4) non-hypertensive controls, (5) techniques for detecting infection, (6) ascertainment of infection throughout pregnancy, or at delivery, and (7) adjustment for well-known preeclampsia confounders (e.g. age, parity, multiple gestation pregnancies, and chronic hypertension).
We excluded case series, case reports, abstract-only studies, brief communications, commentaries, uncontrolled studies, and studies that assessed infection status after delivery. In studies with multiple publications from the same population, we only considered the most recent publication to avoid overrepresentation of the same data. We contacted authors, in instances where studies did not sufficiently report raw data to allow calculation of risk estimates. In one instance, odds ratios were recalculated to reflect the risk of testing positive for viral infection rather than the risk of testing negative [16].We did not assign quality scores to individual studies because of conflicting reports as to their utility [17–19]. We felt that our a priori defined inclusion and exclusion criteria would ensure an acceptable standard of quality.
In addition to obtaining information on the methodology used in the original studies, the following information was reviewed and abstracted by one author (LR): (1) name of author/authors and year of publication, (2) location, (3) number of case and control subjects, and (4) strength of association (odds ratios) and 95% confidence intervals. Exposure was defined as presence or absence of infection.
No institutional review board (IRB) approval was necessary, since only previously published data were used. All data were entered into Excel and later formatted as a STATA file in preparation for analysis.
Statistical analysis
Studies were grouped according to study design, and three separate meta-analyses were conducted. One meta-analysis combined results from all studies. The second and third meta-analyses pooled results of prospective, case control and retrospective studies, separately. The primary outcomes in all analyses were measures of association of bacterial or viral infections and preeclampsia. Heterogeneity was assessed with Cochran’s Q-statistics [20]. Based on a significant Q-statistic P-value less than .10, which indicated presence of heterogeneity, a random effects method of DerSimonian and Laird was used to calculate pooled odds ratios [20–21].
We fitted random-effect meta-regression models to explore whether abstracted study variables could explain the presence of heterogeneity [22–23]. Variables included in meta-regression were, study location (US versus abroad), year of publication, study design, timing of infection ascertainment (first trimester, throughout pregnancy, at delivery), bacterial or viral infection, and adjustment for confounders. In addition, we conducted sensitivity analyses, to determine whether results of meta-analyses were influenced by individual studies. Sensitivity analyses involved dropping one study at a time from meta-analyses, to determine whether risk estimates and heterogeneity were substantially modified.
We considered the potential for publication bias by checking whether risk estimate differences between studies distorted results of the meta-analyses. This was accomplished by visually inspecting funnel plots for asymmetry and performing Egger’s regression asymmetry tests. Funnel plots graphically depict the logarithm of the study odds ratios against their standard errors [24]. The Egger’s asymmetry test plots the standardized effect estimates against precision to determine whether the intercept significantly deviates from zero. A small P-value suggests that publication bias is likely present [25].
All analyses were conducted with Stata\(\texttrademark\) 9.2 [26]. Statistical significance was set at a probability level ≤ .05.
Results
Search results
Results of the literature search are presented in Fig. 1. Initial review of the literature yielded 1,049 publications. Of these publications, 32 studies were potentially eligible for inclusion in meta-analysis. The rest were studies reporting on risk factors for preeclampsia other than maternal infections, reports on clinical management of the disease, and reviews on various aspects of preeclampsia epidemiology. Studies were published in peer-reviewed journals between 1964 and August 2006. From the 32 studies that initially met our inclusion criteria, a total of sixteen were excluded for the following reasons (Table 1): Five out of the 16 excluded studies did not include normotensive women as controls [27–31], we excluded two letters to the editor [32–33], one case report [34], one case series [35], one brief communication [36], and four abstract-only studies [37–40]. One prospective study was uncontrolled and authors did not describe how exposure was ascertained [41]. Another prospective study was excluded [42], because the sample was identical to the one used in a more recent publication [43]. Of the potentially eligible studies, we contacted authors of four studies, because they contained insufficient data to calculate risk estimates. Two authors [44–45] responded to our request and two did not [46–47]. Responses of the two authors allowed us to include their studies in analysis. We were left with 16 studies to be included in meta-analyses (Table 2).
All studies defined preeclampsia using established criteria: blood pressure > 140/90 mmHg or a rise in systolic pressure > 30 mmHg or diastolic blood pressure > 15 mmHg after 20 weeks’ gestation. Proteinuria was measured as either ≥ 1 + dipstick proteinuria on two separate occasions, ≥ 2 + dipstick proteinuria on one occasion or ≥ 300 mg proteinuria over 24 h [48].
Of the 16 studies included in this meta-analysis, two were retrospective [45, 49], eight were case controlled [44, 50–56], and another six were prospective [16, 43, 57–60]. Nine studies were conducted abroad [16, 44–45, 52–53, 55, 57, 59–60], and seven in the US [43, 49–51, 54, 56, 58]. Four of the studies examined multiple infectious agents [16, 44, 53, 57]. Data from these publications were considered as individual studies in analysis (Table 2). Eleven studies explored whether maternal exposure to bacterial infections were associated with preeclampsia [16, 43–44, 49–52, 54–55, 57–58, 60], five studies examined this association with viral infections [16, 45, 53, 56, 59], and two studies examined both [16, 53]. The total combined population across the 16 published studies was 3,204 women with preeclampsia and 17,382 normal pregnancies.
Review of studies included in meta-analysis
Characteristics of studies included in this review are detailed in Table 2. Hsu et al. [49] in a retrospective study of 13,852 pregnant women found that patients with preeclampsia experienced significantly more urinary tract infections than did non-hypertensive patients (χ2 = 64.2, P < .001). Authors reported an increased risk of preeclampsia among women who developed urinary tract infections during pregnancy (OR 4.2, 95% CI 1.1–5.1), after controlling for gestational age, method of delivery, use of oxytocin to induce labor, and premature rupture of membranes. However, information on catheter use, a potential cause of urinary tract infection, was not adjusted for in regression analysis.
These findings were replicated in two prospective investigations: Gilbert et al. [57] followed a total of 123 pregnant women attending prenatal care clinics to term, and determined the rate of bacteriuria (U. urealyticum and G. vaginalis) in women with preeclampsia and women with healthy pregnancies. Authors found that preeclampsia was three times more common (P = .02) in women who had Ureaplasma bacteriuria at the first prenatal visit. Of the 51 patients diagnosed with preeclampsia, 10 (20%) were positive for bacteriuria, compared to 6 of 72 (8%) healthy pregnancies. Authors cautioned that since Ureaplasma bacteriuria is more common among young primigravid women, higher rates of Ureaplasma bacteriuria in these women may be due to chance.
This study was followed by Hill et al. [58] who determined whether asymptomatic bacteriuria (> 100,000 colonies /ml of urine) were more common among women with preeclampsia. In this study, the rate of asymptomatic bacteriuria in 100 primigravidas with preeclampsia was compared to that of 100 normotensive primigravidas undergoing primary cesarean section. The results indicate that asymptomatic bacteriuria were more common among women with preeclampsia (19%) compared to normal pregnancies (3–6%). Authors suggested that the observed increased incidence of bacteriuria in preeclamptic women delivering by cesarean section could in part be due to increased severity of disease in this subgroup, as well as increased susceptibility to infection caused by preeclampsia-associated hypoproteinemia.
In a large nested case control study involving 386 women with preeclampsia and 2,355 normotensive women, Mittendorf et al. [50] demonstrated that primigravidas who developed any urinary tract infection were five time more likely to develop preeclampsia (OR 5.5, 95% CI 2.9–9.7). Authors suggested that antibiotic treatment of primigravid women with a history of urinary tract infections might reduce the risk of preeclampsia.
In 2002, Carreiras et al. [59] showed that women with a genetic predisposition, as well as reactivation of Human Cytomegalovirus (HCMV) were at greater risk for developing preeclampsia. In this study 104 DNA samples from mothers with preeclampsia and normotensive mothers were tested by polymerase chain reaction (PCR) for presence of HCMV sequences. HLA-G polymorphism in connection with HCMV infection conferred a significant risk for preeclampsia. Twelve of 29 (41.3%) normotensive mothers and 14 of 26 (54%) preeclamptic mothers showed HCMV positivity. Moreover, 11 of 14 (79%) infected preeclamptic mothers were DRB1*07 or *06 as compared with 1 of 12 (18%) HCMV+ control mothers carrying the same DRB1 alleles (RR = 8.5, P = .003). Fetal inheritance of maternal G*0104 was also found to be a risk factor for preeclampsia. In another molecular study [56], the rates of Adeno-Associated Virus-2 (AAV) placental infection were compared between 40 cases of severe preeclampsia and 27 normotensive controls. AAV DNA was found in 22 of 40 placentas from women with severe preeclampsia and 5 of 27 normotensive placentas (P = .002). Trophoblast cells from multiparous patients with preeclampsia were six times more likely to be infected with AAV than that of healthy pregnancies (OR 6.0, P = .04), whereas increased rate of AAV infection in placentas from nulliparous patients was not statistically significant. Authors suggested that AAV infections may impair or destroy extravillous trophoblast cells resulting in abnormal invasion of maternal spiral arteries [56].
In a Norwegian study, Trogstad LIS et al. [16] showed an increased risk of preeclampsia among women who were seronegative for, and therefore at risk of acquiring HSV-2 (OR 1.7, 95% CI .7–4.2), CMV (OR 1.6, 95% CI .8–3.2) and EBV (OR 3.5, 95% CI 1.1–10.6) infections. No association was found between Toxoplasma gondii (T. gondii) and preeclampsia (OR 1.0, 95% CI .3–3.5). Although, well-conducted, this study was insufficiently powered to make a definitive conclusion about the relationship between maternal infection and preeclampsia. Todros et al. [55] also studied the relationship between T. gondiiand preeclampsia in a cohort of 417 women with primary T. gondiiinfection treated with spiramycin. In this study, the odds of developing preeclampsia in the treated group were .3 (95% CI .1–1.7). This study is one of the first studies to examine the effect of treatment of infection on the development of preeclampsia. However, controls did not represent the exposure patterns in the population from which the cases originated. Cases were obtained from two tertiary care hospitals and controls from an outpatient clinic. Therefore, possibility for selection bias and lack of generalizability is of concern. For example, the likelihood of detecting T. gondii and preeclampsia in a tertiary care high risk group may be greater, compared to the low-risk pregnancy group.
In a case control study conducted by Heine et al. [51] serum samples were taken from 37 pregnant women with preeclampsia and 37 women with normal pregnancies at admission for labor and delivery. Adjustments were made for maternal age, race, current smoking, and gestational age at delivery. In this study, women with elevated titers of IgG to C. pneumoniae were found to have a three-fold increased risk of preeclampsia (OR 3.1, 95% CI 1.2–7.9). Authors concluded that rather than acute infection or reinfection with C. pneumoniae, persistent or chronic infection may be related to preeclampsia. Similarly, in a nested case control study of prospectively collected serum, von Dadelszen et al. [53] found that women with early onset preeclampsia had higher levels of IgG to C. pneumoniae(.354, 95% CI .067–.659) as compared to normotensives (.207, 95% CI .105–.359). Authors also demonstrated higher IgG levels to CMV (79, 95% CI 49–179) among preeclamptics compared to women with normal pregnancies (49, 95% CI 45–70). However, because cases were obtained from a tertiary referral center, referral patterns may predispose to a concentration of high risk populations, thereby potentially overestimating associations.
Investigation of the relationship between C. pneumoniaeand preeclampsia was extended further in a prospective study by Goulis et al. [60] In this study, serum levels of IgG, IgA and IgM antibodies to C. pneumoniae were measured in 32 women with a previous history of preeclampsia. In contrast to previous studies, no association was found between C. pneumoniae and preeclampsia among primiparous women. However, in subgroup analysis of parous women, levels of all classes of C. pneumoniae antibodies were significantly higher in women with a history of preeclampsia than parous women with normal pregnancies (P≤ .003). Authors suggested that chronic C. pneumoniae infection at conception may confer greater risk of preeclampsia than viral reactivation in later pregnancy.
Raynor et al. [54] in a hospital-based case control study of 287 singleton pregnancies, found no significant difference in the rate of C. pneumoniae seropositivity between preeclampsia and normal pregnancy. Forty-nine percent of normotensives were seropositive for C. pneumoniae, compared to 38.3% of women with preeclampsia (OR 1.6, 95% CI 1.0–2.6, P = .1). This study included women with pre-gestational and gestational diabetes, as well as women with chronic hypertension. No adjustments were made for these confounders in regression analysis. Authors suggested that pre-gestational and gestational diabetes, as well as pre-existing hypertension would not impact on C. pneumoniae positive results. However, inclusion of women with underlying maternal disease may significantly increase the risk of preeclampsia. In these women, infection is less likely to be the cause of preeclampsia.
Frank et al. [45] evaluated the relationship between HIV infection and preeclampsia in a retrospective study of 2,600 women attending prenatal care clinics in Soweto, South Africa who underwent HIV testing. They were unable to report a significant association between HIV infection and the risk of developing preeclampsia (OR 1.1, 95% CI .7–1.6). This lack of association persisted after adjusting for maternal age, gestational age, parity, and maternal weight.
A handful of studies have begun to explore the relationship between periodontal disease and preeclampsia. Canakci et al. [52] studied the association between periodontal disease and preeclampsia in 41 women with preeclampsia and 41 normotensive pregnancies matched on age, gravidity, parity, smoking and prenatal care. Periodontal disease was found in 46.3% of women with preeclampsia and 21.9% of normotensive patients. Multiple conditional logistic regression showed that women with preeclampsia were 3.5 times more likely to have periodontal disease compared to women with healthy pregnancies (OR 3.5, 95% CI 1.1–9.3), after adjusting for maternal body weight, serum triglyceride and serum cholesterol.
In a recent case control study of 130 women with preeclampsia and 243 normotensive controls between 26 and 36 weeks of gestation, Contreras et al. [44], found that chronic periodontitis was more prevalent in women with preeclampsia by almost 64% compared to normotensive women. More specifically, authors found that chronic periodontal disease and the presence of microorganisms, including Porphyromonas gingivalis (P. gingivalis) (OR 1.8, 95% CI 1.1–2.8), Tannerella forsythia (T. forsythia) (OR 1.8, 95% CI 1.1–3.0), and Eikenella corrodens (E. corrodens) (OR 1.8, 95% CI 1.1–2.8) were significantly associated with preeclampsia.
In a prospective investigation by Bogess et al. [43] periodontal examinations were performed on 763 case control subjects to determine whether mild, severe or progressive periodontal disease were associated with preeclampsia. The results indicated that women with severe periodontal disease at delivery or women who developed periodontal disease during pregnancy were twice as likely to have preeclampsia (OR 2.4, 95% CI 1.1–5.3; OR 2.1, 95% CI 1.0–4.4).
Meta-analysis
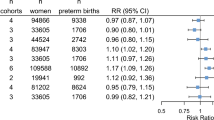
Figures 2–4 show forest plots comparing odds of preeclampsia among women with either bacterial or viral infections. A forest plot illustrates the contribution of each study to the meta-analysis (its weight) and is represented by the area of a box whose center represents the size of effect estimated from that study (point estimate) [25]. Overall pooled estimates indicate a statistically significant association of maternal infections with preeclampsia (OR 2.1, 95% CI 1.6–2.7), with significant heterogeneity (Qdf=20 test of 45.7, P = .001) (Fig 2). Subset meta-analyses based on type of study design revealed significant associations between maternal infections and preeclampsia for prospective (Fig 3), (OR 2.3, 95% CI 1.7–3.0), as well as case control and retrospective studies (Fig 4), (OR 2.0, 95% CI 1.4–2.9). Significant heterogeneity was found in pooled estimates, for case control and retrospective studies (Qdf=10 of 38.7, P < .005), but not for prospective studies (Qdf=9 of 6.5, P = .69).
Association between bacterial and viral infections and preeclampsia. Black squares and horizontal lines denote odds ratios and 95% confidence intervals for each study. The size of the black square reflects the weight of each study. The diamond shape denotes pooled odds ratio and 95% confidence interval. Heterogeneity Q = 45.7, df = 20, P = 0.001
Association between bacterial and viral infections and preeclampsia. Black squares and horizontal lines denote odds ratios and 95% confidence intervals for each study. The size of the black square reflects the weight of each study. The diamond shape denotes pooled odds ratio and 95% confidence interval. Heterogeneity Q = 6.5, df = 9, P = 0.69
Association between bacterial and viral infections and preeclampsia. Black squares and horizontal lines denote odds ratios and 95% confidence intervals for each study. The size of the black square reflects the weight of each study. The diamond shape denotes pooled odds ratio and 95% confidence interval. Asterisks indicate retrospective studies. Heterogeneity Q = 38.7, df = 10, P < 0.005
Meta-regression and sensitivity analysis
Results from the meta-regression analysis are given in Table 3. Meta-regression showed that neither year of publication, timing of infection, type of infection (bacterial or viral), adjustment for confounders (maternal age, gestational age, parity, chronic hypertension, diabetes mellitus), nor study location explained the observed heterogeneity in meta-analyses. However, sensitivity analysis showed a significant reduction in heterogeneity upon exclusion of one case control study [54]. Combined odds ratio, after exclusion, was (OR 2.2, 95% CI 1.8–2.7; Qdf=19, P = .13).
Publication bias
Funnel plots in Figs 5–7 show symmetrical patterns, indicating no evidence of publication bias, and Egger’s Test was non-significant for all three meta-analyses (overall P = .65, 95% CI .9–1.5; prospective P = .57, 95% CI 1.7–2.9; case control and retrospective P = .31, 95% CI 2.3–2.4).
Discussion
Despite variation in exposure ascertainment and study population, relevant epidemiologic data revealed a two-fold increased risk of preeclampsia associated with bacterial and viral infections in all three meta-analyses. These findings are consistent with most results obtained from individual studies, with the exception of two studies [45, 54]. Limitations of meta-analytic reviews should be considered when interpreting results. These limitations generally fall into two categories: (1) limitations carried over from when studies were originally conducted, and (2) those related to the conduct of the meta-analysis.
Limitations of studies
We addressed the first limitation, by defining a priori, inclusion and exclusion criteria. An important inclusion criterion required that a uniform preeclampsia diagnosis was implemented in all studies included in all three meta-analyses. By doing so, we were reasonably certain that preeclampsia was defined consistently, which made it possible to make comparisons between studies. In the past, lack of consistency in defining preeclampsia often resulted in the erroneous inclusion of women with superimposed preeclampsia or women with underlying maternal disease such as, chronic hypertension and diabetes mellitus. Available epidemiologic evidence suggests that these women are more likely to develop preeclampsia, consequently infection is less likely to be the cause of preeclampsia in these women. For example, one study [54] reported a lack of association between C. pneumoniae and preeclampsia but did not adjust for pre-existing hypertension and diabetes in regression analysis. However, when terms for chronic hypertension and diabetes (both coded as “originally adjusted for” (yes/no)) were entered into meta-regression analysis, we found that they did not exert any significant influence on pooled estimates. However, upon removal of this study in sensitivity analysis, heterogeneity was substantially reduced. This was probably the result of very few studies reporting a negative association between maternal infection and preeclampsia.
Descriptive observational studies, although useful in generating hypotheses, do not sufficiently adjust for major confounding factors, because the outcome of interest (preeclampsia) and predictors (maternal infections) are measured at the same time. For example, in studies where timing of blood collection coincided with preeclampsia diagnosis, we cannot be certain that maternal infections increased the risk of preeclampsia or whether preeclampsia increased the risk of maternal infections.
Misclassification of infection status is also a concern, since ascertainment of maternal exposure to infectious agents is highly dependent on laboratory diagnostic techniques, which can vary significantly between laboratories. Although most studies included in this review used established laboratory methods to measure maternal infection (PCR, glycoprotein gG enzyme-linked immunosorbent assays (ELISA), and micro-immunofluorescence), in some patients, antibody titers may fluctuate significantly. Other patients may not develop significant antibodies at all. In these patients, misclassification of serostatus may be unavoidable. Also, diagnosis of chronic infection is hindered by current limitations in serological methods. For example, identification of patients with chronic C. pneumoniae infection using IgG and IgA antibody levels is complicated by a lack of reference test for validating chronic infection [61]. Consequently, it is not clear what antibody titer levels correspond with chronic infection. Additionally, two [51, 53] of the four studies exploring the association between C. pneumoniae and preeclampsia used different cutoff levels for seropositivity, and two studies [54, 60] did not specify cutoffs.
The second limitation includes bias stemming from the conduct of a meta-analysis, such as publication bias, and heterogeneity. Publication bias is the tendency on the parts of investigators, reviewers, and editors to submit or accept manuscripts for publication based on the direction or strength of the study findings [62]. Typically this involves a higher acceptance rate of studies showing statistically significant results. In a meta-analysis, this type of bias can have the effect of skewing meta-analytic reviews toward a positive result. Inspection of the funnel plots in Figs 5–7 show symmetrical distributions of study results (shown in Figs. 5–7 as log odds ratios). We therefore do not believe publication bias was a limitation in this review. There was, however, evidence of statistically significant heterogeneity between studies: overall pooled analysis (P = .001), case control studies and retrospective studies (P < .005).
We explored the following variables as potential sources of heterogeneity; study design, year of publication, study location, type of infectious agent, timing of infection, and whether or not studies adjusted for major preeclampsia confounders, but none of these factors emerged as significant contributors to combined risk estimates. Even so, it is possible that other factors, whose effects are unable to be evaluated in meta-analysis, may have contributed significantly to heterogeneity. If potential confounders were not adequately addressed when studies were originally carried out, combined results will inevitably reflect these limitations. For example, we cannot discount the possibility that unmeasured infection-related risk factors may have confounded the relationship between infection and preeclampsia in some studies. These may include: behavioral and clinical factors (smoking, alcohol consumption, length of cohabitation, sexual, contraceptive, and history of STDs and other infections). Most of the studies reviewed in the three meta-analyses evaluated some but not all of these potential confounding factors. Additionally, several studies did not adjust for maternal age. Maternal age is associated with both infection and preeclampsia.
Also, measurement of periodontal disease varied between studies that explored the association between periodontal disease and preeclampsia. Lack of universal agreement on definition and classification of periodontal disease may have significantly increased the likelihood of case misclassification, and may have led to varying measures of association between exposure and disease across studies. Although periodontal disease is commonly associated with oral pathogens, definitions tend to be based on clinical measures of periodontal disease, without direct assessment of infection status. For example, only one [44] study obtained either bacterial counts or antibody levels of oral pathogens.
Potential mechanisms
It has been postulated that infection may be important in the pathogenesis of preeclampsia, either through initiation (by increasing the risk of acute uteroplacental atherosis) and/or its enhancement (by magnifying the maternal systemic inflammatory response), [53] or through direct effect on trophoblast cells (by destruction or impairment of trophoblast cells, resulting in shallow invasion of maternal spiral arteries) [56].These hypotheses are supported by key clinical and epidemiologic data. First, preeclampsia is associated with a distinct pathologic lesion of the decidual arterioles known as acute atherosis, which closely resembles atherosclerotic lesions of coronary arteries [63]. One of the main features of early lesion development in atherosclerosis is formation of macrophage foam cells in the arterial intima [64–66]. Infectious agents can exert direct effects on atherogenesis by residing in the vascular wall, after being delivered to the vessel wall by circulating monocytes [67].
Second, preeclampsia and atherosclerosis share many other characteristics and risk factors, including dyslipidemia, insulin resistance, obesity, hypertension [68], and endothelial dysfunction, all of which involve inflammation. Although studies have demonstrated evidence for an inflammatory response both in normal and preeclamptic pregnancies, in preeclampsia inflammation seems excessive [7–11]. Maternal infections may trigger release of pro-inflammatory cytokines into maternal circulation, which may further enhance the already heightened level of inflammation observed in women with preeclampsia, resulting in endothelial cell dysfunction and oxidative stress [5–6, 12, 69].
Similarly, in periodontal disease, monocyte-derived cytokines such as tumor necrosis factor-alpha (TNF-α), and interleukins (IL-1, IL-6 and IL-8) may be released in response to infection with oral pathogens [70], resulting in major vascular responses, including an inflammatory cell infiltrate in the vessel walls, vascular smooth muscle proliferation, vascular fatty degeneration, and intravascular coagulation [71, 72].
Third, as suggested by Arechevaleta-Velasco and Fisher et al. [56], maternal infection may either destroy cytotrophoblast cells or impair their function, resulting in shallow invasion of uterine spiral arteries.
Conclusion
Individual retrospective, case control and prospective studies have reported on the relationship between both bacterial and viral pathogens in association with preeclampsia. Our combined results confirm these study findings. Endothelial dysfunction and excessive inflammation are consistent characteristics of preeclampsia. The exact cause of inflammation is not completely understood. However, infection is known to stimulate the immune system and may provide a biologically plausible explanation for preeclampsia-related inflammation. The concept that infection may trigger preeclampsia would provide insight into the pathophysiology of this maternal syndrome. Furthermore, it would suggest public health measures that might reduce the incidence of a disease that causes major maternal morbidity and perinatal mortality.
References
WHO international collaborative study of hypertensive disorders of pregnancy (1988). Geographic variation in the incidence of hypertension in pregnancy. American Journal of Obstetrics and Gynecology, 158, 80–83.
Roberts, J. M., & Redman, C. W. (1993). Preeclampsia: more than pregnancy-induced hypertension. Lancet, 342, 619.
Saftlas, A. F., Olson, D. R., Franks, A. L., Atrash, H. K., & Pokras, R. (1990). Epidemiology of preeclampsia and eclampsia in the United States, 1979–1986. American Journal of Obstetrics and Gynecology, 163(2), 460–465.
Roberts, J. M., Taylor, R. N., Musci, T. J., Rodgers, G. M., Hubel, C. A., & McLaughlin, M. K. (1989). Preeclampsia: an endothelial cell disorder. American Journal of Obstetrics and Gynecology, 161, 1200–1204.
Redman, C. W. G., Sacks, G. P., & Sargent, I. L. (1999). Preeclampsia: An excessive maternal inflammatory response to pregnancy. American Journal of Obstetrics and Gynecology, 180, 499–506.
Sacks, G. P., Studena, K., Sargent, I. L., & Redman, C. W. G. (1998). Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. American Journal of Obstetrics and Gynecology, 197, 80–86.
Rinehart, B. K., Terrone, D. A., Lagoo-Deenadayalan, S., Barber, W. H., Hale, E. A., Martin, J. N. Jr, & Benett, W. A. (1999). Expression of the placental cytokines tumor necrosis factor-α, interleukin 1-ß, and interleukin 10 is increased in preeclampsia. American Journal of Obstetrics and Gynecology, 181(4), 915–920.
Visser, W., & Wallenburg, H. C. (1999). Prediction and prevention of pregnancy-induced hypertensive disorders. Baillière’s Best Practice & Research. Clinical Obstetrics & Gynaecology, 13, 131–156.
Sanchez, S. E., Zhang, C., Williams, M. A., Ware-Jauregui, S., Larrabare, G., Bazul, V., & Farrand, A. (2000). Tumor necrosis factor-α soluble p55(sTNFp55) and risk of preeclampsia in Peruvian women. Journal of Reproductive Immunology, 47, 49–63.
Amory, J. H., Hitti, J., Lawler, R., & Eschenbach, D. A. (2001). Increased tumor necrosis factor-α production after lipopolysaccharide stimulation of whole blood in patients with previous preterm delivery complicated by intraamniotic infection or inflammation. American Journal of Obstetrics and Gynecology, 185, 1064–1067.
Benyo, D. F., Smarason, A., Redman, C. W. G., Sims, C., & Conrad, K. P. (2001). Expression of inflammatory cytokines in placentas from women with preeclampsia. The Journal of clinical endocrinology and metabolism, 86, 2505–2512.
Luppi, P., Haluszczak, C., Betters, D., Richard, C. A. H., Trucco, M., & DeLoia, J. A. (2002). Monocytes are progressively activated in the circulation of pregnant women. The Journal of clinical endocrinology and metabolism, 72, 874–884.
Paternoster, D. M., Fantinato, S., Stella, A., Nanhorngue, K. N., Milani, M., Plebani, M., Nicolini, U., & Girolami, A. (2006). C-reactive protein in hypertensive disorders in pregnancy. Clinical & Applies Thrombosis/Hemostasis, 12, 330–337.
Gordis, L. (1996). Meta-analysis. In: L. McGrew (Ed.), Epidemiology. (p. 253). Philadelphia: WB Saunders Company.
Stroup, D. F., Berlin, J. A., Morton, S. C., & et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting – Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA, 283, 2008–2012.
Trogstad, L. I., Eskild, A., Bruu, A. L., Jeansson, S., & Jenum, P. A. (2001). Is preeclampsia an infectious disease? Acta Obstetricia et Gynecologica , 80, 1036–1038.
Jüni, P., Witschi, A., Bloch, R., & Matthias, E. (1999). The hazards of scoring the quality of clinical trials for meta-analysis. JAMA, 282, 1054–1060.
Greenland, S., & O’Rourke, K. (2001). On the bias produced by quality scores in meta-analysis, and a hierarchical review of proposed solutions. Biostatistics, 2, 463–471.
Whiting, P., Harbord, R., & Kleijnen, J. (2005). No role for quality scores in systematic reviews of diagnostic accuracy studies. BMC Medical Research Methodology, 5, 19.
Laird, N. M., & Mosteller, F. (1990). Some statistical methods for combining experimental results. International Journal of Technology Assessment in Health Care, 6, 5–30.
DerSimonian, R., & Laird, N. (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7, 177–188.
Higgins, J. P. T., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21, 1539–1558.
Berkey, C. S., Hoaglin, D. C., Mosteller, F., & Colditz, G. A. (1995). A random-effects regression model for meta-analysis. Statistics in Medicine, 14, 395–411.
Sterne J. A. C., & Egger, M. (2001). Funnel plots for detecting bias in meta-analysis: Guidelines on choice of axis. Journal of Clinical Epidemiology, 54, 1046–1055.
Egger, M., Smith, G. D., & Phillips, A. N. (1997). Meta-analysis: principles and procedures. BMJ, 315, 1533–1537.
Stata\({\texttrademark}\) 9.2 Stata Corporation, 4905 Lakeway Drive, College Station, Texas 77845 USA.
Stuart, K. L., Cummins, G. T. M., & Chin, W. A. (1965). Bacteriuria, prematurity, and the hypertensive disorders of pregnancy. British Medical Journal, 5434, 554–556.
Kincaid-Smith, P., & Bullen, M. (1965). Bacteriuria in pregnancy. Lancet, 191, 7382–7399.
Tarjan, G. (1967). Frequency of bacteriuria in women with late toxemias of pregnancy. Zentralblatt für Gynäkologie, 89, 646–646 (Article in German).
Wimalasundera, R. C., Larbalestier, N., Smith, J. H., de Ruiter A., McG Thom, S. A., Hughes, A. D., Poulter, N., Regan, L., & Taylor, G. P. (2002). Preeclampsia, antiretroviral therapy, and immune reconstitution. Lancet, 360, 1152–1154.
Castaldi, J. L., Bertin, M. S., Gimenez, F., & Lede, R. (2006). Periodontal disease: is it a risk factor for premature labor, low birth weight or preeclampsia? Rev Panam Salud Publica, 19, 253–258 (Article in Spanish).
Sartelet, H., Rogier, C., Milko, S.I., Angel, G., & Michel, G. (1996). Malaria associated preeclampsia in Senegal. Lancet, 347, 1121.
Teran, E., & Escudero, C. (2003). Seroprevalence of antibodies to Chlamydia pneumoniae in women with preeclampsia. Obstetrics and Gynecology, 102, 198–199.
Mattar, R., Amed, A. M., Lindsey, P. C., Sass, N., & Daher, S. (2004). Preeclampsia and HIV infection. Obstetrics and Gynecology, 117, 240–241.
Oettinger-Barak, O., barak Shlomi, Ohel, G., Oettinger, M., Kreutzer, H., Peled, M., & machtei, E. E. (2005). Severe pregnancy complication (preeclampsia) is associated with greater periodontal destruction. Journal of Periodontology, 76, 134–137.
Aral, M., Guven, M. A., & Kocturk, S. A. (2005). Chlamydia pneumoniae seropositivity in women with preeclampsia. International Journal of Gynaecology and Obstetrics, 92, 77–78.
Belfort, M., Cortes, J., Bowles, N., Saade, G., Dorman, K., Abadajos, P., & Towbin J. (1998). Placental Cytomegalovirus infection and preeclampsia: Are they related? Journal of the Society for Gynecologic Investigation, 5, 136A–T403.
Rustveld, L., Ness, R., Costantino, J., & Roberts, J. (2003). Serological association between primary infections with Herpes Simplex Virus Types 1 and 2 (HSV-1 and HSV-2), Cytomegalovirus (CMV) and Epstein Barr Virus (EBV) and the risk of preeclampsia. American Journal of Epidemiology, 157(suppl), 296-S.
Blaauw, J., Kunnen, A., Van Pampus, M. G., Van Doormaal, J. J., Van Winkelhoff, A. J., Abbas, F., & Aarnoudse, J. G. (2005). Periodontal disease in recently preeclamptic women. American Journal of Obstetrics and Gynecology, 193, S69.
Chang, E., Armstrong, M. D., Ebeling, M., Hulsey, T., & Newman R. (2006). Urinary tract infections are associated with an increased risk of preeclampsia. American Journal of Obstetrics and Gynecology, 193(suppl), S71–214.
Herrera, J. A., Chaudhuri, G., & Lopez-Jaramillo, P. (2001). Is infection a major risk factor for preeclampsia. Medical Hypotheses, 57, 393–397.
Riche, E. L., Boggess, K. A., Lieff, S., Murtha, A. P., Beck, J. D., & Offenbacher, S. (2002). Periodontal disease increases the risk of preterm delivery among preeclamptic women. Annals of Periodontology, 7, 95–101.
Bogess, K. A., Lieff, S., Murtha, A., Moss, K., Beck, J., & Offenbacher, S. (2003). Maternal periodontal disease is associated with an increased risk for preeclampsia. Obstetrics and Gynecology, 101, 227–231.
Contreras, A., Herrera, J. A., Soto, J. E., Arce, R. M., Jaramillo, A., & Botero, J. E. (2006). Periodontitis is associated with preeclampsia in pregnant women. Journal of Periodontology, 77, 182–188.
Frank, K. A., Buchmann, E. J., & Schackis, R. C. (2004). Does Human Immunodeficiency Virus infection protect against preeclampsia-eclampsia? Obstet Gynecol, 104, 238–242.
Suy, A., Martinez, E., Coll, O., Lonca, M., Palacio, M., de Lazzari, E., Larrousse, M., Milinkovic, A., Hernandez, S., Blanco, J. L., Mallolas, J., Leon, A., Vanrell, J. A., & Gatell, J. M. (2006). Increased risk of preeclampsia and fetal death in HIV-infected pregnant women receiving highly active antiretroviral therapy. AIDS, 20, 59–66.
Wimalasundera, R. C., Larbalestier, N., Smith, J. H., de Ruiter A., Thom, SA. MCG., Hughes, A .D., Poulter N., Regan L., & Taylor, G. P. (2002). Preeclampsia, antiretroviral therapy, and immune reconstitution. Lancet, 360, 1152–1154.
American College of Obstetrics and Gynecologist (ACOG) (2002) Hypertension in pregnancy. ACOG Educational Bulletin 33.
Hsu, C. D., & Witter, F. R. (1995). Urogenital infection in preeclampsia. Journal of Obstetrics and Gynaecology, 49, 271–275.
Mittendorf, R., Lain, K. Y., Williams, M. A., & Walker, C. K. (1996). Preeclampsia: A nested, case control study for risk factors and their interactions. The Journal of Reproductive Medicine, 41, 491–496.
Heine, R. P., Ness, R. B., & Roberts, J. M. (2003). Seroprevalence of antibodies to Chlamydia pneumoniae in women with preeclampsia. Obstetrics and Gynecology, 101, 221–226.
Canakci, V., Canakci, C. F., Canakci, H., Canakci, E., Cicek, Y., Ingec, M., Ozgoz, M., Demir, T., Dilsiz, A., Yagiz, H. (2004). Periodontal disease as a risk factor for preeclampsia: A case contol study. Australian and New Zealand Journal of Obstetrics and Gynaecology, 44, 568–573.
Von Dadelszen, P., & Magee, L. A. (2002). Could an infectious tiger explain the differential maternal response to the shared placental pathology of preeclampsia and normotensive intrauterine growth restriction? Acta Obstetricia et Gynecologica Scandinavica, 81, 642–648.
Raynor, D. B., Bonney, E. A., Jang, K. T., Coto, W., & Garcia, M. S. (2004). Preeclampsia and Chlamydia pneumoniae: Is there a link? Hypertension in Pregnancy, 23, 129–133.
Todros, T., Verdiglione, P., Ogge, G., Paladini, D., Vergani, P., Cardaropoli, S. (2006). Low incidence of hypertensive disorders of pregnancy in women treated with spiramycin for toxoplasma infection. British Journal of Clinical Pharmacology, 61(3), 336–340.
Arechavaleta-Velasco, F., Ma, Y., Zhang, J., McGrath, C. M., & Parry, S. (2006). Adeno-Associated Virus-2 (AAV-2) causes trophoblast dysfunction, and placental AAV-2 infection is associated with preeclampsia. The American Journal of Pathology , 168, 1951–1959.
Gilbert, G. L., Garland, S. M., Fairley, K. F., & McDowall, D. M. (1986). Bacteriuria due to ureaplasmas and other fastidious organisms during pregnancy: prevalence and significance. Pediatric Infectious Disease, 5(6Suppl), S239–243.
Hill, J. A., Devoe, L. D., & Bryans, C. I. Jr (1986). Frequency of asymptomatic bacteriuria in preeclampsia. Obstetrics and Gynecology, 67, 529–532.
Carreiras, M., Montagnani, S., & Layrisse, Z. (2002). Preeclampsia: A multifactorial disease resulting from the interaction of the feto-maternal HLA genotype and HCMV infection. AJRI, 48, 176–183.
Goulis, D. G., Chappell, L., Gibbs, R. G. J., Williams, D., Dave, J. R., Taylor, P., de Swiet, M., Poston, L., & Williamson, C. (2005). Association of raised titres of antibodies to Chlamydia pneumoniae with a history of pre-eclampsia. BJOG : An International Journal of Obstetrics and Gynaecology, 112, 299–305.
Dowell, S. F., Peeling, R. W., Boman, J., Carlone, G. M., Fields, B. S., Guarner, J., Hammerschlag, M. R., Jackson, L. A., Kuo, C. C., Maass M., Messmer T. O., Talkington D. F., Tondella M. L., & Zaki S. R. (2001). Standardizing Chlamydia pneumoniae Assays: Recommendations from the Centers for Disease Control and Prevention (USA) and the Laboratory Centre for Disease Control (Canada). Clinical Infectious Diseases, 33, 492–503.
Dickersin, K. (1990). The existence of publication bias and risk factors for its occurrence. JAMA, 263, 1385–1389.
Hubel, C. A. (1999). Oxidative stress in the pathogenesis of preeclampsia. Proceedings of the Society for Experimental Biology and Medicine, 222, 222–234.
Kalayoglu, M. V., & Byrne, G. I. (1998). Induction of macrophage foam cell formation by Chlamydia pneumoniae. The Journal of Infectious Diseases , 177, 725–729.
Ross, R. (1999). Atherosclerosis: an inflammatory disease. The New England Journal of Medicine, 340, 115–226.
Brown, M., & Goldstein, J. (1983). Lipoprotein metabolism in the macrophage. Annual Review of Biochemistry, 52, 223–261.
Lindberg, G., Rastam, L., Lundblad, A., & et al. (1997). ARIC Study Investigators. The association between serum sialic acid and asymptomatic carotic atherosclerosis is not related to antibodies to Herpes type viruses of Chlamydia pneumoniae. International Journal of Epidemiology, 26, 1386–1391.
Sibai, B., Dekker, G., & Kupferminc, M. (2005). Preeclampsia. Lancet, 365, 785–799.
Sacks, G., Sargent, I., & Redman, C. W. G. (1999). An innate view of human pregnancy. Immunology Today, 20, 114–118.
Genco, R., Offenbacher, S., & Beck, J. (2002). Periodontal disease and cardiovascular disease: Epidemiology and possible mechanisms. JADA, 133, 14S–22S.
Mattila, K. J., Nieminen, M. S., & Valtonen, V. V. (1989). Association between dental health and acute myocardial infarction. BMJ, 298, 779–781.
Marcus, A. J., & Hajjar, D. P. (1993). Vascular transcellular signaling. Journal of Lipid Research, 34, 2017–2031.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rustveld, L.O., Kelsey, S.F. & Sharma, R. Association Between Maternal Infections and Preeclampsia: A Systematic Review of Epidemiologic Studies. Matern Child Health J 12, 223–242 (2008). https://doi.org/10.1007/s10995-007-0224-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-007-0224-1