Abstract
Background
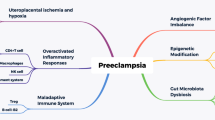
Preeclampsia (PE) is one of the major causes of maternal and perinatal morbidity and mortality, especially in low- and middle-income countries. In recent years, a growing body of literatures suggests that infections by bacteria, viruses, and parasites and their related inflammations play an important role in the pathogenesis of PE.
Methods
We searched PubMed, Google scholar, and Cochrane databases using the following search words: “infection and preeclampsia,” “bacterial infection and preeclampsia,” “viral infection and preeclampsia” and “parasitic infection and preeclampsia.”
Results
The literature review revealed that many bacteria including Helicobacter pylori, Chlamydia pneumonia, and those are involved in periodontal disease or urinary tract infections (UTIs) and some viral agents such as Cytomegalovirus, herpes simplex virus type-2, human immunodeficiency virus, and some parasites especially Plasmodium spp. and Toxoplasma gondii can be effective in development of PE. Inflammation responses against infections has major role in the inducement of PE. The shift of immunological cytokine profile of Th2 toward Th1 and high levels of pro-inflammatory cytokines (TNF-ɑ, IL-12, IFN-γ, etc.), increase of oxidative stress, increase of anti-angiogenic proteins, increase of vascular endothelial growth factor receptor 1 (sVEGFR1), and complement C5a are the main potential mechanisms related to infections and enhanced development of PE.
Conclusion
Thus, early diagnosis and treatment of bacterial, viral, and parasitic infections could be an effective strategy to reduce the incidence of PE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preeclampsia (PE), a multisystem vascular syndrome, is characterized by the gestational onset of hypertension and proteinuria and generally occurred after 20 weeks’ of gestation [1]. PE is one of the major causes of maternal and perinatal morbidity and mortality, especially in low- and middle-income countries [2, 3]. It affects approximately 5–8% of all pregnancies around the world [4], and is responsible for almost 350,000 maternal deaths [3, 5], six million perinatal deaths [6], eight million preterm births [7], and approximately 20 million low-birth-weight newborns in developing countries [8]. Moreover, it is demonstrated that PE is associated with higher risks of chronic noncommunicable diseases in later life of affected women [9]. Despite several researches to identification of the major risk factors and potential mechanisms and much advance in our knowledge, the PE’s etiology remains elusive. However, it is hypothesized that PE’s etiology is multifactorial, involving both maternal and placental contributions [10].
The maternal infections, especially those that are transmissible in utero, are responsible for several incidences of morbidity and mortality during pregnancy [11]. TORCH complex, comprise toxoplasmosis, other (syphilis, varicella-zoster, parvovirus B19, Hepatitis B), Rubella, Cytomegalovirus (CMV), and Herpes infections, hepatitis infections, human immunodeficiency virus (HIV) are the most common transplacentally acquired infections by the fetus [11, 12]. These infections are responsible for several congenital anomalies like still birth, abortion, intrauterine fetal deaths, congenital malformations, and other congenital failures [11, 13,14,15]. Zika virus infection is considered as the newest TORCH complex that is associated with several complications such as intrauterine fetal infection, microcephaly, neurological abnormalities, and Guillain–Barré syndrome [16,17,18]. Moreover, coinfection with the above mentioned microorganisms can lead to more adverse effect on mother and fetus and also can lead to difficulties in actual diagnosis [19, 20].
In recent years, a growing body of literatures suggests that infections by bacteria, viruses, and parasites and their related inflammations play an important role in the pathogenesis of PE [21, 22]. Several maternal infectious agents including HIV, malaria, different bacteria, and periodontal disease or urinary tract infections (UTIs) have been suggested to increase the risk of PE [21, 22]. This narrative review will discuss the role the infectious agents in development of PE and possible mechanisms related to these infections that are involved in PE. For this purpose, we searched PubMed, Google scholar, and Cochrane databases using the following search words: “infection and preeclampsia,” “bacterial infection and preeclampsia,” “viral infection and preeclampsia,” and “parasitic infection and preeclampsia.” Publications in English language were considered, but we did not impose any study design or geographic limitations. Review was conducted on more than 38 potentially relevant articles published between 2009 and 2017.
Bacterial infection
In the last three decades, several epidemiological and casual studies have evaluated the possible relationship between maternal bacterial and viral infections and PE. Many of these studies indicated a positive association between bacterial and viral infections and PE [23,24,25,26,27,28]. Moreover, intrauterine infections and their resulting inflammatory responses are responsible for early preterm births and labor in pregnant women [29,30,31]. Rustveld et al. [21] in a meta-analysis study have demonstrated that women with either a bacterial or viral infection had twofold higher risk to develop PE compared with women without infection (OR 2.1; 95% CI 1.6–2.7).
Several retrospective and prospective studies demonstrated potential risk of UTIs by bacteria to induce PE [32,33,34,35]. Several pathogenic bacteria are responsible for UTIs including Escherichia coli, responsible for 70–80% of all UTIs in pregnancy; Gram-negative bacteria include Klebsiella, Enterobacter, Proteus, Pseudomonas, Citrobacter, and Gram-positive bacteria, for example, group B Streptococci [36]. Moreover, other bacteria, including Ureaplasma parvum, Gardnerella vaginalis, Mycoplasma hominis, lactobacilli, and Chlamydia trachomatis, have also been reported to induce UTIs [33, 37,38,39]. It is demonstrated that the early diagnosis and treatment of UTI decreased the incidence of PE by 64% [40]. Hsu et al. in a retrospective study on 13,852 pregnant women reported that risk of PE was significantly more (OR 4.2; 95% CI 1.1–5.1) among women who developed UTIs during pregnancy [32]. Conde-Agudelo et al. [22] in a comprehensive meta-analysis study have shown that that risk of PE was increased in pregnant women with UTIs (OR 1.57; 95% CI 1.45–1.70).
Periodontal disease (PD) is another most prevalent human infection disease that has been reported as potential risk factor for the development of PE. Several genera of bacteria include Treponema, Bacteroides, Porphyromonas, Prevotella, Capnocytophaga, Peptostreptococcus, Fusobacterium, Actinobacillus, Tannerella, and Eikenella, and their related species are involved in PD [41]. In a case–control study, Contreras et al. have found that the presence of microorganisms related in PDs such as Porphyromonas gingivalis (OR 1.8; 95% CI 1.1–2.8), Tannerella forsythia (OR 1.8; 95% CI 1.1–3.0), and Eikenella corrodens (OR 1.8; 95% CI 1.1–2.8) were significantly associated with the development of PE in pregnant women [42]. Conde-Agudelo et al. in their meta-analysis reported significant relationship between the presence of PD and the induction of PE (OR 1.76; 95% CI 1.43–2.18) [22]. Similar finding (OR 2.79; 95% CI 2.01–3.01) was achieved in a recent meta-analysis study by Wei et al. [43]. Two comprehensive studies by Rustveld et al. and Conde-Agudelo et al. have been published in 2008; we summarized recently conducted studies (2009–2016) regarding the association between UTIs and PD [2, 34, 35, 44,45,46,47,48,49,50,51] with development of PE in Table 1.
Chlamydia pneumonia, Ureaplasma urealyticum, and Helicobacter pylori are other bacterial organisms that were reported as potential risk factors for the development of PE [52, 53]. Heine et al. using a case–control study demonstrated that women with elevated titers of IgG to C. pneumoniae have a threefold increased risk of PE (OR 3.1, 95% CI 1.2–7.9) compared with healthy controls [23]. Although in other studies, no significant correlation was observed between C. pneumoniae and PE [54,55,56], Dadelszen et al. in a prospective cohort study reported that women with early-onset PE had significantly higher levels of IgG to Chlamydophila pneumonia compared with normotensive pregnant women [24].
The significant relationship between H. pylori infection and PE was described for the first time by Ponzetto et al. [57]. They reported that seropositive women for H. pylori had almost threefold higher risk to develop PE [57]. Subsequent studies reported also a significantly higher H. pylori seropositivity rate in preeclamptic women compared with controls [25, 26, 58,59,60,61, 65, 66]. Moreover, recent studies described that infection with Cytotoxin-associated antigen A (CagA)- and Vacuolating cytotoxin A (VacA)-positive H. pylori-strains is significantly related with PE and, especially with “placental PE” [58]. This could be explained by the fact that CagA- and VacA-positive H. pylori strains are generally associated to higher levels of inflammatory mediators compared with negative strains [62]. Recently conducted studies (2009-2017) regarding the associations between C. pneumonia, C. trachomatis, and H. pylori infections and PE [25, 26, 39, 52, 58,59,60,61, 63,64,65,66] are summarized in Table 2.
Viral infection
Among the viral pathogens, Cytomegalovirus (CMV), Adeno-Associated Virus-2 (AAV-2), herpes simplex virus type-2 (HSV2), Epstein-Barr virus (EBV), and human immunodeficiency virus (HIV) have been more studied and found to have more likelihood to be effective in PE. Dadelszen et al. through a nested case–control study indicated that women with early-onset PE had higher anti-CMV levels than women with late-onset PE and normotensive women (P < 0.05) [24]. Similar results were obtained by Xie et al. in two subsequent studies [28, 67]. Moreover, their results showed that women with PE have upregulated TLR-2/-4 mRNA expression, increased levels of serum IL-6 and TNF-α, and reduced IL-10 compared with matched normal and nonpregnancy controls [67]. Arechavaleta-Velasco et al. [68] in a molecular study reported that rates of AAV-2 placental infection were significantly higher among women with severe PE compared with women having normotensive placentas (P = 0.002). In a subsequent study, same team reported that the first-trimester maternal IgM seropositivity for AAV-2 was 5.6 times more prevalent among PE (P = 0.0004) than in healthy controls [69]. Rustveld et al. have found that seroconversion for HSV 1/2 or CMV was associated with a fivefold increased risk for developing PE (OR 5.4; 95% CI 1.0–29.0) after adjusting for education, income, smoking, years of cohabitation, medical insurance, and type of birth control [70]. In another study, Trogstad et al. reported an increased risk of PE among women who were seronegative for, and therefore at the risk of acquiring EBV (OR 3.5; 95% CI 1.1–10.6), CMV (OR 1.6; 95% CI 0.8–3.2), and HSV-2 (OR 1.7; 95% CI 0.7–4.2) infections [71]. Moreover, there are several studies regarding the effect of HIV on hypertensive disorders of pregnancy [72,73,74,75,76]. Based on data from a comprehensive meta-analysis study [77], however, no evidence was found regarding the relationship between HIV infection and PE (OR 1.04; 95% CI 0.60–1.79), but significant associations were observed regarding HIV infection with hypertension (OR 1.46; 95% CI 1.03–2.05) and eclampsia (OR 2.56; 95% CI 0.15–44.11) among pregnant women. Recent studies (2009–2017) regarding the associations between viral infections and PE [28, 39, 64, 67, 78,79,80,81,82,83,84] are summarized in Table 3.
Mechanisms for bacterial and viral infections
Inflammation responses against infections play important roles in the initiation and enhancement of acute uteroplacental atherosis or destruction of trophoblast cells, major risks known to induce PE [68]. Moreover, clinical and epidemiologic data indicated that acute atherosis is directly associated with PE [70, 85]. The increase of monocytes circulation resulting from infections and establishment of macrophage foam cells in the arterial intima could be the key factors to induce early lesion in atherosclerosis [70, 86,87,88]. Moreover, several studies have demonstrated that inflammatory responses are excessive in preeclamptic pregnancies compared with normal pregnancies [89,90,91,92,93]. Bacterial and viral infections during pregnancy could stimulate release of high level of pro-inflammatory cytokines (TNF-ɑ, IL-12, IFN-γ, etc.) and also increase of oxidative stress and endothelial cell dysfunction, all of which could lead to initiation of hypertension disorders including PE [70]. Increased levels of oxidative stress induced by Chronic or acute infections could impair the production and bioactivity of nitric oxide (NO) that can lead to endothelial dysfunction, a crucial event to induce the PE. In agreement with this statement, PE-like manifestations were observed in experimental models by blocking endothelial production of NO [94,95,96,97].
In addition to the above mentioned mechanisms, some antigenic factors of microorganisms like Cytotoxin-associated antigen A (CagA) may be directly related PE [98]. Recent studies showed that anti-CagA antibodies are able to cross-react with antigens (β-actin proteins) of endothelial cells and cytotrophoblast cells of placenta that can lead to negative effects on its invasiveness ability [99, 100]. Moreover, it is reported that anti-CagA antibodies are able to inhibit the activation of mediator factors that are important during trophoblast proliferation, such as ERK and Nuclear Factor-kB [99].
Parasitic infections
Among the parasite diseases, infections with protozoa such as Plasmodium spp., Toxoplasma gondii, Trichomonas vaginalis, and Trypanosoma cruzi could be potential risk factors for PE, mainly regarding vertical transmission, placental infection, and the host immune response to them. Infection with these protozoa during the pregnancy could result to low birth weight, still birth, spontaneous abortion, growth restriction, intrauterine fetal death, and fetal abnormalities [101]. There are no study exploring role of the trypanosomiasis in development of PE, although some evidences are available regarding parasite invasion to the placenta and inhibit the implantation and cell division [101]. Toxoplasmosis is one of the most prevalent infection disease with worldwide distribution [102]. It is the cause of many adverse complications in immunocompromised patients and pregnant women [103, 104]. Todros et al. [105] in a cohort study indicated that pregnant women treated with spiramycin have shown lower pregnancy-induced hypertension (OR 0.092; 95% CI 0.021–0.399) compared with women who did not take any antibiotic during pregnancy. Although in a recently conducted study in Mexico, it was reported that chronic toxoplasmosis is not associated with hypertensive disorders in pregnant women [106].
Although, there is any study indicating the role of T. vaginalis in PE, but secretion of galectin family (galectin-1 and galectin-3) by cervical and vaginal epithelial cells upon T. vaginalis infection could be possible mechanism to induce PE, as these galectins modulate the inflammatory responses [107]. Than et al. [108] have demonstrated that placental expression of galectin-1 was significantly higher in patients with severe PE than in normal controls, and these increases may represent a fetal response to an exaggerated systemic maternal inflammation. Moreover, T. vaginalis lipophosphoglycan motivates species-specific inflammatory response and selective chemokine (IL-8 and macrophage inflammatory protein-3ɑ) upregulation by human cervical and vaginal epithelial cells [107, 109].
Malaria especially induced by P. falciparum has been the most-described parasitic mechanism to cause PE. Annually, 125 million pregnant women are at risk of malarial infection in malarious areas, and the excess risk of infection varies with gravidity [110, 111]. There are several epidemiological overlaps between malaria infection and PE [112]. Both malaria and PE have markedly higher risk in young and primigravidae women and also similar seasonal distribution [112,113,114,115,116]. In addition, some observational studies reported placental malaria as a potential risk factor for developing increased maternal hypertension and related disorders, including PE [117,118,119,120,121]. Sartelet et al. [117] in 1996 reported that placental malaria was significantly related with PE in Senegalian pregnant women (OR 3.0; 95% CI 1.3–6.9). Muehlenbachs et al. in Tanzania indicated that malaria was associated with the increased risk of hypertension in young (18–20 years old) first-time mothers (OR 3.1; 95% CI 1.1–9.0) [115]. In a recent case–control study in Sudan, placental malaria (OR 2.3; 95% CI 1.0–5.2) was significantly associated with PE [120].
There are several evidences to multiple mechanisms contributing to PE associated with malaria in pregnant women including anemia, alternation in immunological milieu, and increase of anti-angiogenic proteins that contribute to the pathogenesis of PE such as sFlt-1 and endoglin [115, 116, 122, 123]. Moreover, Muehlenbachs et al. [115] reported that soluble vascular endothelial growth factor receptor 1 (sVEGFR1), a preeclampsia biomarker, was significantly increased in first-time mothers with both malaria infection and hypertension. Complement C5a, which plays an important role in induction of inflammation and initiation of acquired immune response, is another factor that is elevated in malarial infection and has significant role in the induction of PE [122, 124,125,126]. The shift of immunological cytokine profile of Th2, typical immune profile associated with pregnancy, to Th1 includes TNF-ɑ, IL-12, and IFN-γ. immune profile more suited to parasite killing is another important possible mechanism by malarial infection to induce preeclampsia [15, 127] [110, 111].
Conclusion
PE is the major public health problem in both developed and developing countries. However, etiology of PE is multifactorial, but infections and their related inflammations have important roles in the development of PE. Pro-inflammatory cytokines and other cellular mediators induced by periodontal, vaginal, or urinary infections cause endothelial dysfunction that is essential alteration in the pathophysiology of PE. Early diagnosis and treatment of bacterial, viral, and parasitic infections could be an effective strategy to reduce the incidence of PE. In order to achieve significant decreases in maternal and perinatal mortality rates resulting from PE, it is crucial that the screening and treatment of common maternal infections be incorporated into the prenatal care programs.
References
American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013;122:1122.
Bilano VL, Ota E, Ganchimeg T, Mori R, Souza JP. Risk factors of pre-eclampsia/eclampsia and its adverse outcomes in low-and middle-income countries: a WHO secondary analysis. PLoS One. 2014;9:e91198.
Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367:1066–74.
ACOG Committee on Obstetric Practice. Diagnosis and management of preeclampsia and eclampsia. Int J Gynecol Obstet. 2002;77:67–75.
Lozano R, Wang H, Foreman KJ, Rajaratnam JK, Naghavi M, Marcus JR, Dwyer-Lindgren L, Lofgren KT, Phillips D, Atkinson C. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet. 2011;378:1139–65.
Ahman E, Zupan J. Neonatal and perinatal mortality: country, regional and global estimates 2004. OMS. 2007;9241596147.
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, Rubens C, Menon R, Van Look PF. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31–8.
Wardlaw TM. Low birthweight: country, regional and global estimates. Geneva: World Health Organization, UNICEF; 2004.
Bygbjerg I. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337:1499–501.
Trogstad L, Magnus P, Stoltenberg C. Pre-eclampsia: risk factors and causal models. Best Pract Res Clin Obstet Gynaecol. 2011;25:329–42.
Neu N, Duchon J, Zachariah P. TORCH infections. Clin Perinatol. 2015;42:77–103.
Yadav RK, Maity S, Saha S. A review on TORCH: groups of congenital infection during pregnancy. J Sci In Res. 2014;3(2):258–64.
De Francesco M, Corbellini S, Piccinelli G, Benini A, Ravizzola G, Gargiulo F, Caccuri F, Caruso A. A cluster of invasive listeriosis in Brescia, Italy. Infection. 2015;43:379.
Sen M, Shukla B, Tuhina B. Prevalence of serum antibodies to TORCH infection in and around Varanasi, Northern India. J Clin Diagn Res. 2012;6:1483.
Waldorf KMA, McAdams RM. Influence of infection during pregnancy on fetal development. Reproduction. 2013;146:151–62.
Duijster JW, Goorhuis A, van Genderen PJ, Visser LG, Koopmans MP, Reimerink JH, Grobusch MP, van der Eijk AA, van den Kerkhof JHCT, Reusken CB, Hahné SJM. Zika virus infection in 18 travellers returning from Surinam and the Dominican Republic, The Netherlands, November 2015–March 2016. Infection. 2016;44:797–802.
Nourollahpour Shiadeh M, Rostami A, Danesh M, Sajedi AA. Zika virus as new emerging global health threat for pregnancy and child birth. J Matern Fetal Neonatal Med. 2017;30:562.
Coyne CB, Lazear HM. Zika virus—reigniting the TORCH. Nat Rev Microbiol. 2016;14:707–15.
Boos V, Feiterna-Sperling C, Sarpong A, Garten L, Cremer M, von Weizsäcker K, Bührer C, Dame C. The rationale for third trimester testing of vertical HIV transmission in neonates with CMV infection. Infection. 2016;44(4):555–7.
Baroncelli S, Pirillo M, Amici R, Tamburrini E, Genovese O, Ravizza M, Maccabruni A, Masuelli G, Guaraldi G, Liuzzi G, Pinnetti C, Giacomet V, Degli Antoni A, Vimercati A, Dalzero S, Sacchi V, Floridia M. HCV–HIV coinfected pregnant women: data from a multicentre study in Italy. Infection. 2016;44:235–42.
Rustveld LO, Kelsey SF, Sharma R. Association between maternal infections and preeclampsia: a systematic review of epidemiologic studies. Matern Child Health J. 2008;12:223–42.
Conde-Agudelo A, Villar J, Lindheimer M. Maternal infection and risk of preeclampsia: systematic review and metaanalysis. Am J Obstet Gynecol. 2008;198:7–22.
Heine RP, Ness RB, Roberts JM. Seroprevalence of antibodies to Chlamydia pneumoniae in women with preeclampsia. Obstet Gynecol. 2003;101:221–6.
Dadelszen P, Magee LA, Krajden M, Alasaly K, Popovska V, Devarakonda RM, Money DM, Patrick DM, Brunham RC. Levels of antibodies against cytomegalovirus and Chlamydophila pneumoniae are increased in early onset pre-eclampsia. BJOG Int J Obstet Gynaecol. 2003;110:725–30.
ÜstÜn Y, Engin-ÜstÜn Y, Özkaplan E, Otlu B, Sait TekerekoĞlu M. Association of Helicobacter pylori infection with systemic inflammation in preeclampsia. J Matern Fetal Neonatal Med. 2010;23:311–4.
Aksoy H, Ozkan A, Aktas F, Borekci B. Helicobacter pylori seropositivity and its relationship with serum malondialdehyde and lipid profile in preeclampsia. J Clin Lab Anal. 2009;23:219–22.
Pugliese A, Beltramo T, Todros T, Cardaropoli S, Ponzetto A. Interleukin-18 and gestosis: correlation with Helicobacter pylori seropositivity. Cell Biochem Funct. 2008;26:817–9.
Xie F, Hu Y, Magee LA, Money DM, Patrick DM, Krajden M, Thomas E, Von Dadelszen P, Group TS. An association between cytomegalovirus infection and pre-eclampsia: a case–control study and data synthesis. Acta Obstet Gynecol Scand. 2010;89:1162–7.
DiGiulio DB, Romero R, Amogan HP, Kusanovic JP, Bik EM, Gotsch F, Kim CJ, Erez O, Edwin S, Relman DA. Microbial prevalence, diversity and abundance in amniotic fluid during preterm labor: a molecular and culture-based investigation. PLoS One. 2008;3:e3056.
Fredricks DN, Fiedler TL, Marrazzo JM. Molecular identification of bacteria associated with bacterial vaginosis. N Engl J Med. 2005;353:1899–911.
Menard JP, Mazouni C, Salem-Cherif I, Fenollar F, Raoult D, Boubli L, Gamerre M, Bretelle F. High vaginal concentrations of Atopobium vaginae and Gardnerella vaginalis in women undergoing preterm labor. Obstet Gynecol. 2010;115:134–40.
Hsu C, Witter F. Urogenital infection in preeclampsia. Int J Gynecol Obstet. 1995;49:271–5.
Gilbert GL, Garland SM, Fairley KF, Mcdowall RD. Bacteriuria due to ureaplasmas and other fastidious organisms during pregnancy: prevalence and significance. Pediatr Infect Dis J. 1986;5:239–43.
Minassian C, Thomas SL, Williams DJ, Campbell O, Smeeth L. Acute maternal infection and risk of pre-eclampsia: a population-based case–control study. PLoS One. 2013;8:e73047.
Easter SR, Cantonwine DE, Zera CA, Lim K-H, Parry SI, McElrath TF. Urinary tract infection during pregnancy, angiogenic factor profiles, and risk of preeclampsia. Am J Obstet Gynecol. 2016;214:381–7.
Glaser AP, Schaeffer AJ. Urinary tract infection and bacteriuria in pregnancy. Urol Clin North Am. 2015;42:547–60.
Agger WA, Siddiqui D, Lovrich SD, Callister SM, Borgert AJ, Merkitch KW, Mason TC, Baumgardner DJ, Burmester JK, Shukla SK. Epidemiologic factors and urogenital infections associated with preterm birth in a midwestern US population. Obstet Gynecol. 2014;124:969–77.
Cohen I, Veille J-C, Calkins BM. Improved pregnancy outcome following successful treatment of chlamydial infection. JAMA. 1990;263:3160–3.
Haggerty CL, Klebanoff MA, Panum I, Uldum SA, Bass DC, Olsen J, Roberts JM, Ness RB. Prenatal Chlamydia trachomatis infection increases the risk of preeclampsia. Pregnancy Hypertens. 2013;3:151–4.
Herrera J, Chaudhuri G, López-Jaramillo P. Is infection a major risk factor for preeclampsia? Med Hypotheses. 2001;57:393–7.
Guthmiller J, Novak K. Chapter 8, Periodontal diseases. In: Brogden KA, Guthmiller JM, editors. Polymicrobial diseases. Washington (DC): ASM Press; 2002.
Contreras A, Herrera J, Soto J, Arce R, Jaramillo A, Botero J. Periodontitis is associated with preeclampsia in pregnant women. J Periodontol. 2006;77:182–8.
Wei B-J, Chen Y-J, Yu L, Wu B. Periodontal disease and risk of preeclampsia: a meta-analysis of observational studies. PLoS One. 2013;8:e70901.
Mazor-Dray E, Levy A, Schlaeffer F, Sheiner E. Maternal urinary tract infection: is it independently associated with adverse pregnancy outcome? J Matern Fetal Neonatal Med. 2009;22:124–8.
Shamsi U, Hatcher J, Shamsi A, Zuberi N, Qadri Z, Saleem S. A multicentre matched case control study of risk factors for preeclampsia in healthy women in Pakistan. BMC Women Health. 2010;10:14.
Lohsoonthorn V, Kungsadalpipob K, Chanchareonsook P, Limpongsanurak S, Vanichjakvong O, Sutdhibhisal S, Sookprome C, Wongkittikraiwan N, Kamolpornwijit W, Jantarasaengaram S. Maternal periodontal disease and risk of preeclampsia: a case–control study. Am J Hypertens. 2009;22:457–63.
Shetty M, Shetty PK, Ramesh A, Thomas B, Prabhu S, Rao A. Periodontal disease in pregnancy is a risk factor for preeclampsia. Acta Obstet Gynecol Scand. 2010;89:718–21.
Politano G, Passini R, Nomura M, Velloso L, Morari J, Couto E. Correlation between periodontal disease, inflammatory alterations and pre-eclampsia. J Periodontal Res. 2011;46:505–11.
Moura da Silva G, Coutinho SB, Piscoya MDB, Ximenes RA, Jamelli SR. Periodontitis as a risk factor for preeclampsia. J Periodontol. 2012;83:1388–96.
Taghzouti N, Xiong X, Gornitsky M, Chandad F, Voyer R, Gagnon G, Leduc L, Xu H, Tulandi T, Wei B. Periodontal disease is not associated with preeclampsia in Canadian pregnant women. J Periodontol. 2012;83:871–7.
Kumar A, Basra M, Begum N, Rani V, Prasad S, Lamba AK, Verma M, Agarwal S, Sharma S. Association of maternal periodontal health with adverse pregnancy outcome. J Obstet Gynaecol Res. 2013;39:40–5.
Xie F, Hu Y, Magee LA, Money DM, Patrick DM, Brunham RM, Thomas E, von Dadelszen P. Chlamydia pneumoniae infection in preeclampsia. Hypertens Pregnancy. 2010;29:468–77.
Karinen L, Leinonen M, Bloigu A, Paldanius M, Koskela P, Saikku P, Hartikainen A-L, Järvelin M-R, Pouta A. Maternal serum Chlamydia pneumoniae antibodies and CRP levels in women with preeclampsia and gestational hypertension. Hypertens Pregnancy. 2008;27:143–58.
Raynor BD, Bonney EA, Jang KT, Coto W, Garcia MS. Preeclampsia and Chlamydia pneumoniae: is there a link? Hypertens Pregnancy. 2004;23:129–34.
Goulis DG, Chappell L, Gibbs RG, Williams D, Dave JR, Taylor P, De Swiet M, Poston L, Williamson C. Association of raised titres of antibodies to Chlamydia pneumoniae with a history of pre-eclampsia. BJOG Int J Obstet Gynaecol. 2005;112:299–305.
Chrisoulidou A, Goulis DG, Iliadou PK, Dave JR, Bili H, Simms C, Redman CW, Williamson C. Acute and chronic Chlamydia pneumoniae infection in pregnancy complicated with preeclampsia. Hypertens Pregnancy. 2011;30:164–8.
Ponzetto A, Cardaropoli S, Piccoli E, Rolfo A, Gennero L, Kanduc D, Todros T. Pre-eclampsia is associated with Helicobacter pylori seropositivity in Italy. J Hypertens. 2006;24:2445–9.
Cardaropoli S, Rolfo A, Piazzese A, Ponzetto A, Todros T. Helicobacter pylori’s virulence and infection persistence define pre-eclampsia complicated by fetal growth retardation. World J Gastroenterol. 2011;17:5156–65.
Mosbah A, Nabiel Y. Helicobacter pylori, Chlamydiae pneumoniae and trachomatis as probable etiological agents of preeclampsia. J Matern Fetal Neonatal Med. 2016;29:1607–12.
Rădulescu C, Bacârea A, Huţanu A, Şincu N, Băţagă S. Helicobacter pylori infection and pre-eclampsia in a Romanian study group. Int J Gynecol Obstet. 2016;135:328–9.
Di Simone N, Tersigni C, Cardaropoli S, Franceschi F, Di Nicuolo F, Castellani R, Bugli F, Waure C, Cavaliere AF, Gasbarrini A. Helicobacter pylori infection contributes to placental impairment in preeclampsia: basic and clinical evidences. Helicobacter. 2017;22:2. doi:10.1111/hel.12347.
Graham DY, Yamaoka Y. Disease-specific helicobacter pylori virulence factors: the unfulfilled promise. Helicobacter. 2000;5:3–9.
Gomez LM, Parry S. Trophoblast infection with Chlamydia pneumoniae and adverse pregnancy outcomes associated with placental dysfunction. Am J Obstet Gynecol. 2009;200:521–6.
Haggerty CL, Panum I, Uldum SA, Bass DC, Olsen J, Darville T, Eastman JM, Simhan HN, Roberts JM, Ness RB. Chlamydia trachomatis infection may increase the risk of preeclampsia. Pregnancy Hypertens. 2013;3:28–33.
Hollander WJ, Schalekamp-Timmermans S, Holster IL, Jaddoe VW, Hofman A, Moll HA, Perez-Perez GI, Blaser MJ, Steegers EA, Kuipers EJ. Helicobacter pylori colonization and pregnancies complicated by preeclampsia, spontaneous prematurity, and small for gestational age birth. Helicobacter. 2017;22:2. doi:10.1111/hel.12364.
Elkhouly NI, Elkelani OA, Elhalaby AF, Shabana AA. Relation between Helicobacter pylori infection and severe pre-eclampsia complicated by intrauterine growth restriction in a rural area in Egypt. J Obstet Gynaecol. 2016;36:1046–9.
Xie F, Dadelszen P, Nadeau J. CMV infection, TLR-2 and-4 expression, and cytokine profiles in early-onset preeclampsia with HELLP syndrome. Am J Reprod Immunol. 2014;71:379–86.
Arechavaleta-Velasco F, Ma Y, Zhang J, McGrath CM, Parry S. Adeno-associated virus-2 (AAV-2) causes trophoblast dysfunction, and placental AAV-2 infection is associated with preeclampsia. Am J Pathol. 2006;168:1951–9.
Arechavaleta-Velasco F, Gomez L, Ma Y, Zhao J, McGrath C, Sammel M, Nelson D, Parry S. Adverse reproductive outcomes in urban women with adeno-associated virus-2 infections in early pregnancy. Hum Reprod. 2008;23:29–36.
Rustveld L, Ness R, Costantino J, Roberts J. Serological association between primary infections with herpes simplex virus types 1 and 2 (HSV-1 and HSV-2), cytomegalovirus (CMV) and Epstein Barr virus (EBV) and the risk of preeclampsia. Am J Epidemiol. 2003;157:S74.
Trogstad LI, Eskild A, Bruu AL, Jeansson S, Jenum PA. Is preeclampsia an infectious disease? Acta Obstet Gynecol Scand. 2001;80:1036–8.
Suy A, Martínez E, Coll O, Lonca M, Palacio M, de Lazzari E, Larrousse M, Milinkovic A, Hernández S, Blanco JL. Increased risk of pre-eclampsia and fetal death in HIV-infected pregnant women receiving highly active antiretroviral therapy. AIDS. 2006;20:59–66.
Wimalasundera R, Larbalestier N, Smith J, De Ruiter A, Thom SM, Hughes A, Poulter N, Regan L, Taylor G. Pre-eclampsia, antiretroviral therapy, and immune reconstitution. Lancet. 2002;360:1152–4.
Boer K, Nellen J, Patel D, Timmermans S, Tempelman C, Wibaut M, Sluman M, Van Der Ende M, Godfried M. The AmRo study: pregnancy outcome in HIV-1-infected women under effective highly active antiretroviral therapy and a policy of vaginal delivery. BJOG Int J Obstet Gynaecol. 2007;114:148–55.
De Groot M, Corporaal L, Cronje H, Joubert G. HIV infection in critically ill obstetrical patients. Int J Obstet Gynaecol. 2003;81:9–16.
Frank KA, Buchmann EJ, Schackis RC. Does human immunodeficiency virus infection protect against preeclampsia-eclampsia? Obstetr Gynecol. 2004;104:238–42.
Calvert C, Ronsmans C. HIV and the risk of direct obstetric complications: a systematic review and meta-analysis. PLoS One. 2013;8:e74848.
Strand K, Odland M, Iversen AC, Nordbø S, Vik T, Austgulen R. Cytomegalovirus antibody status at 17–18 weeks of gestation and pre-eclampsia: a case–control study of pregnant women in Norway. BJOG Int J Obstet Gynaecol. 2012;119:1316–23.
Haeri S, Shauer M, Dale M, Leslie J, Baker AM, Saddlemire S, Boggess K. Obstetric and newborn infant outcomes in human immunodeficiency virus–infected women who receive highly active antiretroviral therapy. Am J Obstet Gynecol. 2009;201:311–5.
Boyajian T, Shah PS, Murphy KE. Risk of preeclampsia in HIV-positive pregnant women receiving HAART: a matched cohort study. J Obstet Gynaecol Can. 2012;34:136–41.
Kalumba V, Moodley J, Naidoo T. Is the prevalence of pre-eclampsia affected by HIV/AIDS? A retrospective case-control study: cardiovascular topics. Cardiovasc J Afr. 2013;24:24–7.
Hall D, Gebhardt S, Theron G, Grové D. Pre-eclampsia and gestational hypertension are less common in HIV infected women. Pregnancy Hypertens. 2014;4:91–6.
Landi B, Bezzeccheri V, Guerra B, Piemontese M, Cervi F, Cecchi L, Margarito E, Giannubilo SR, Ciavattini A, Tranquilli AL. HIV infection in pregnancy and the risk of gestational hypertension and preeclampsia. World J Cardiovasc Dis. 2014;4:257–67.
Sansone M, Sarno L, Saccone G, Berghella V, Maruotti GM, Migliucci A, Capone A, Martinelli P. Risk of preeclampsia in human immunodeficiency virus-infected pregnant women. Obstet Gynecol. 2016;127:1027–32.
Roberts J, Cooper D. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001;357:53–6.
Kalayoglu MV, Byrne GI. Induction of macrophage foam cell formation by Chlamydia pneumoniae. J Infect Dis. 1998;177:725–9.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95.
Ross R. Atherosclerosis—an inflammatory disease. New Engl J Med. 1999;340:115–26.
Rinehart BK, Terrone DA, Lagoo-Deenadayalan S, Barber WH, Martin JN, Bennett WA. Expression of the placental cytokines tumor necrosis factor α, interleukin 1β, and interleukin 10 is increased in preeclampsia. Am J Obstet Gynecol. 1999;181:915–20.
Amory JH, Hitti J, Lawler R, Eschenbach DA. Increased tumor necrosis factor-α production after lipopolysaccharide stimulation of whole blood in patients with previous preterm delivery complicated by intra-amniotic infection or inflammation. Am J Obstet Gynecol. 2001;185:1064–7.
Benyo DF, Smarason A, Redman CW, Sims C, Conrad KP. Expression of inflammatory cytokines in placentas from women with preeclampsia 1. J Clin Endocrinol Metabol. 2001;86:2505–12.
Teran E, Escudero C, Moya W, Flores M, Vallance P, Lopez-Jaramillo P. Elevated C-reactive protein and pro-inflammatory cytokines in Andean women with pre-eclampsia. Int J Gynecol Obstet. 2001;75:243–9.
LaMarca BD, Ryan MJ, Gilbert JS, Murphy SR, Granger JP. Inflammatory cytokines in the pathophysiology of hypertension during preeclampsia. Curr Hypertens Rep. 2007;9:480–5.
López-Jaramillo P, Casas J, Serrano N. Preeclampsia: from epidemiological observations to molecular mechanisms. Braz J Med Biol Res. 2001;34:1227–35.
Davidge ST. Oxidative stress and altered endothelial cell function in preeclampsia. Seminars in reproductive endocrinology. Stuttgart: Thieme Medical Publishers Inc; 1998. p. 65–73.
Belayet HM, Kanayama N, Khatun S, El Maradny E, Masui M, Tokunaga N, Sumimoto K, Kobayashi T, Terao T. Decreased renal and hepatic blood flow with preeclampsia-like histologic changes was obtained by stimulation of the celiac ganglion with LPS. Am J Perinatol. 1998;15:109–14.
López-Jaramillo P, Herrera JA, Arenas-Mantilla M, Jáuregui IE, Mendoza MA. Subclinical infection as a cause of inflammation in preeclampsia. Am J Ther. 2008;15:373–6.
Cardaropoli S, Rolfo A, Todros T. Helicobacter pylori and pregnancy-related disorders. World J Gastroenterol. 2014;20:654.
Franceschi F, Di Simone N, D’ippolito S, Castellani R, Di Nicuolo F, Gasbarrini G, Yamaoka Y, Todros T, Scambia G, Gasbarrini A. Antibodies Anti-Caga Cross-React with Trophoblast Cells: A Risk Factor for Pre-Eclampsia? Helicobacter. 2012;17(6):426–34.
Franceschi F, Niccoli G, Ferrante G, Gasbarrini A, Baldi A, Candelli M, Feroce F, Saulnier N, Conte M, Roccarina D, Lanza GA, Gasbarrini G, Gentiloni SN, Crea F. CagA antigen of Helicobacter pylori and coronary instability: insight from a clinico-pathological study and a meta-analysis of 4241 cases. Atherosclerosis. 2009;202:535–42.
Shiadeh Nourollahpour. Niyyati M, Fallahi S, Rostami A. Human parasitic protozoan infection to infertility: a systematic review. Parasitol Res. 2016;115:469–77.
Rostami A, Seyyedtabaei SJ, Aghamolaie S, Behniafar H, Lasjerdi Z, Abdolrasouli A, Mehravar S, Alvarado-Esquivel C. Seroprevalence and risk factors associated with Toxoplasma gondii infection among rural communities in Northern IRAN. Rev Inst Med Trop Sao Paulo. 2016;58:70.
Nourollahpour Shiadeh M, Rostami A, Pearce B, Gholipourmalekabadi M, Newport D, Danesh M, et al. The correlation between Toxoplasma gondii infection and prenatal depression in pregnant women. Eur J Clin Microbiol Infect Dis. 2016;35:1829–35.
Rostami A, Keshavarz H, Shojaee S, Mohebali M, Meamar AR. Frequency of Toxoplasma gondii in HIV Positive Patients from West of Iran by ELISA and PCR. Iran J Parasitol. 2014;9(4):474–81.
Todros T, Verdiglione P, Oggè G, Paladini D, Vergani P, Cardaropoli S. Low incidence of hypertensive disorders of pregnancy in women treated with spiramycin for Toxoplasma infection. Br J Clin Pharmacol. 2006;61:336–40.
Alvarado-Esquivel C, Vázquez-Alaníz F, Sandoval-Carrillo AA, Salas-Pacheco JM, Hernández-Tinoco J, Sánchez-Anguiano LF, Liesenfeld O. Lack of association between Toxoplasma gondii infection and hypertensive disorders in pregnancy: a case–control study in a Northern Mexican population. Parasites Vectors. 2014;7:1.
Fichorova RN. Impact of T. vaginalis infection on innate immune responses and reproductive outcome. J Reprod Immunol. 2009;2009(83):185–9.
Than NG, Erez O, Wildman DE, Tarca AL, Edwin SS, Abbas A, Hotra J, Kusanovic JP, Gotsch F, Hassan SS. Severe preeclampsia is characterized by increased placental expression of galectin-1. J Matern Fetal Neonat Med. 2008;21:429–42.
Fichorova RN, Trifonova RT, Gilbert RO, Costello CE, Hayes GR, Lucas JJ, Singh BN. Trichomonas vaginalis lipophosphoglycan triggers a selective upregulation of cytokines by human female reproductive tract epithelial cells. Infect Immun. 2006;74:5773–9.
Dellicour S, Tatem AJ, Guerra CA, Snow RW, ter Kuile FO. Quantifying the number of pregnancies at risk of malaria in 2007: a demographic study. PLoS Med. 2010;7:e1000221.
van Eijk AM, Hill J, Noor AM, Snow RW, ter Kuile FO. Prevalence of malaria infection in pregnant women compared with children for tracking malaria transmission in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2015;3:617–28.
Brabin BJ, Johnson PM. Placental malaria and pre-eclampsia through the looking glass backwards? J Reprod Immunol. 2005;65:1–15.
Etard J-F, Kodio B, Ronsmans C. Seasonal variation in direct obstetric mortality in rural Senegal: role of malaria? Am J Trop Med Hyg. 2003;68:503–4.
Anya SE. Seasonal variation in the risk and causes of maternal death in the Gambia: malaria appears to be an important factor. Am J Trop Med Hyg. 2004;70:510–3.
Muehlenbachs A, Mutabingwa TK, Edmonds S, Fried M, Duffy PE. Hypertension and maternal–fetal conflict during placental malaria. PLoS Med. 2006;3:e446.
Hlimi T. Association of anemia, pre-eclampsia and eclampsia with seasonality: a realist systematic review. Health Place. 2015;31:180–92.
Sartelet H, Rogier C, Milko-Sartelet I, Angel G, Michel G. Malaria associated pre-eclampsia in Senegal. Lancet. 1996;347:1121.
Ekeleme Uzochukwu G, Kama Ugochukwu H, Otutu Elijah A, Ajunwa Kelechi V, Oha Ndubuisi OC, Ndimele Eugene C. Studies on the infections of Malaria, Human Immunodeficiency Virus and Hepatitis B Virus among Secondary School Students in Enugu West. Int J Sci Res Publ. 2016;6:36–43.
Ndao CT, Dumont A, Fievet N, Doucouré S, Gaye A, Lehesran J-Y. Placental malarial infection as a risk factor for hypertensive disorders during pregnancy in Africa: a case-control study in an urban area of Senegal, West Africa. Am J Epidemiol. 2009;170:847–53.
Adam I, Elhassan EM, Mohmmed AA, Salih MM, Elbashir MI. Malaria and pre-eclampsia in an area with unstable malaria transmission in Central Sudan. Malar J. 2011;10:1.
Dorman E, Shulman C, Kingdom J, Bulmer J, Mwendwa J, Peshu N, Marsh K. Impaired uteroplacental blood flow in pregnancies complicated by falciparum malaria. Ultrasound Obstet Gynecol. 2002;19:165–70.
Conroy AL, Silver KL, Zhong K, Rennie M, Ward P, Sarma JV, Molyneux ME, Sled J, Fletcher JF, Rogerson S. Complement activation and the resulting placental vascular insufficiency drives fetal growth restriction associated with placental malaria. Cell Host Microbe. 2013;13:215–26.
Muehlenbachs A, Fried M, Lachowitzer J, Mutabingwa TK, Duffy PE. Natural selection of FLT1 alleles and their association with malaria resistance in utero. Proc Natl Acad Sci. 2008;105:14488–91.
Conroy A, Serghides L, Finney C, Owino SO, Kumar S, Gowda DC, Liles WC, Moore JM, Kain KC. C5a enhances dysregulated inflammatory and angiogenic responses to malaria in vitro: potential implications for placental malaria. PLoS One. 2009;4:e4953.
Muehlenbachs A, Fried M, Lachowitzer J, Mutabingwa TK, Duffy PE. Genome-wide expression analysis of placental malaria reveals features of lymphoid neogenesis during chronic infection. J Immunol. 2007;179:557–65.
Soto E, Romero R, Richani K, Espinoza J, Chaiworapongsa T, Nien JK, Edwin SS, Kim YM, Hong JS, Goncalves LF. Preeclampsia and pregnancies with small-for-gestational age neonates have different profiles of complement split products. J Matern Fetal Neonatal Med. 2010;23:646–57.
Saito S, Shiozaki A, Nakashima A, Sakai M, Sasaki Y. The role of the immune system in preeclampsia. Mol Asp Med. 2007;28:192–209.
Acknowledgements
The authors would like to thank Dr. Hamed Behniafar, for his assistance in the preparation of this manuscript.
Funding
There are no funding sources for this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Ethical approval
This study received the approval from the Shahid Beheshti University of Medical Science Ethical Committee.
Rights and permissions
About this article
Cite this article
Nourollahpour Shiadeh, M., Behboodi Moghadam, Z., Adam, I. et al. Human infectious diseases and risk of preeclampsia: an updated review of the literature. Infection 45, 589–600 (2017). https://doi.org/10.1007/s15010-017-1031-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-017-1031-2