Abstract
Bombesin is a tetradecapeptide that binds specifically to gastrin releasing peptide receptors in humans. Several forms of cancer, including lung, prostate, breast, and colon express receptors for bombesin-like peptides. Radiolabeled bombesin analogs with a high affinity for these receptors might therefore be used for scintigraphic imaging of these tumor types. A truncated bombesin derivative (HYNIC-βAla-Bombesin(7–14)) was radiolabeled with technetium-99m using EDDA and tricine as coligands. In vitro stability was evaluated in presence of plasma and excess of cysteine. The receptor-binding affinity assays was evaluated in MDA-MB-231 cancer cell line. In addition, in vivo biodistribution was performed in nude mice bearing breast tumor. In vitro assay showed a good affinity for the MDA-MB-231 cell line, showing 20.0 % of internalization at 4 h post-administration. 99mTc-HYNIC-βAla-Bombesin(7–14) biodistribution revealed a rapid clearance and a significant renal excretion. In addition, tumor uptake was higher than non-excretory organs, such as the spleen, the liver, and muscles. Tumor-to-muscle and tumor-to-blood ratios for 99mTc-HYNIC-βAla-Bombesin(7–14) showed high values at 4 h post-injection (5.34 and 4.55, respectively). Furthermore, blocked studies using cold bombesin peptide were performed, which demonstrated an important decrease in tumor uptake, indicating a tumor specificity for 99mTc-HYNIC-βAla-Bombesin(7–14). The 99mTc-HYNIC-βAla-Bombesin(7–14) displayed suitable radiochemical characteristics, and adequate affinity to breast tumor cells (MDA-MB-231). Therefore, this analog can be considered as a candidate for the identification of bombesin-positive tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer is among the most common causes of death throughout the world. In 2008, approximately 13 million new cancer cases and 7.6 million cancer deaths are estimated to have occurred worldwide [1]. Cancer imaging techniques using radiotracers targeted to specific receptors have yielded successful results, demonstrating the utility of such approaches for developing specific radiopharmaceuticals [2–7]. Molecular imaging of tumor metabolism, proliferation, and other-specific targets is a powerful tool in the diagnosis, staging, restaging, response evaluation and guiding surgery, radiotherapy, and systemic treatment [8, 9].
Regulatory peptide receptors are over-expressed in numerous human cancer cells. These receptors have been used as molecular targets for radiolabeled peptides to locate tumors. In recent years, many studies have been performed to identify peptide analogs able to target these tumors, such as gastrin-releasing peptides, somatostatin, neurotensin, and vasoactive intestinal peptides [10–15].
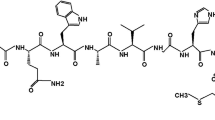
Bombesin (BBN), a tetradecapeptide, was first isolated by Anastasi et al. [16] from the skin of European Bombina bombina frog. The mammalian counterpart is the 27 amino acid gastrin-releasing peptide (GRP). BBN and GRP differ by only 1 of 10 carboxy-terminal residues, which explains the similar biological activity of the two peptides [17–19]. The bombesin receptor family is comprised of four receptor subtypes: (1) neuromedin B receptor (BBN1); (2) gastrin-releasing peptide receptor (BBN2); (3) the orphan receptor subtype (BBN3); and (4) the bombesin receptor subtype (BBN4) [20–22]. A variety of tumors have been found to express receptors for these peptides, such as lung, prostate, breast, pancreas, and colon [23]. Radiolabeled BBN analogs with a high affinity for these receptors might therefore be used for scintigraphic imaging of these tumor types [24–26]. Several of these analogs bind selectively and avidly to GRP receptors on cancer cells when the truncated amino acid sequence (BBN(7–14)NH2) is used. Prior studies have been reported that the C-terminal amino acid sequence is necessary to retain receptor binding affinity. Thus, the N-terminal region of the peptide can be used for radiolabeling [10, 27–31].
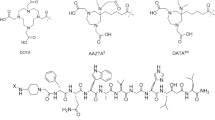
Technetium-99m (99mTc) has mostly been used to label radiopharmaceuticals, due to its suitable physical and chemical characteristics and inexpensive isotope cost [32, 33]. 2-Hydrazinonicotinamide (HYNIC) is an attractive bifunctional chelating ligand used to prepare 99mTc-labeled peptides [34], as it shows a high labeling efficiency and its usage with various co-ligands (e.g., ethylendiaminediacetic acid (EDDA), tricine and glucoheptonate) allows for the control of hydrofobicity and pharmacokinetics of the small 99mTc-labeled peptides [35].
Radiolabeling and biodistribution studies of 99mTc-HYNIC-βAla-Bombesina(7–14) can be found in prior studies carried out by the present research group [2], the results of which showed that the complex was able to identify Erhlich tumors, a form of murine breast cancer. Therefore, the purpose of the present study was to demonstrate the ability of 99mTc-HYNIC-βAla-Bombesina(7–14) to identify human breast tumors (MDA-MB-231 cell line) in athymic nu/nu mice. To achieve this, in vitro assays, biodistribution studies were performed, and scintigraphic images were acquired.
Materials and methods
Materials
The peptide HYNIC-βAla-Bombesin(7–14) was purchased from GL Biochem (Shanghai, China). Technetium-99m was obtained from an alumina-based 99Mo/99mTc generator. All solvents (HPLC analytical grade) and other reagents, including tricine, ethylenediamine-N,N′-diacetic acid (EDDA), and SnCl2·2H2O, were purchased from Sigma-Aldrich (São Paulo, Brazil). The subcutaneous tumor model was established in a 6–8 week-old female athymic nu/nu mice purchased from CEMIB (Campinas, Brazil). All animal studies were approved by the local Ethics Committee for Animal Experiments (CETEA).
Radiolabeling
To a sealed vial containing 20 mg tricine and 5 mg of EDDA was added 0.5 ml of 0.9 % NaCl. Next, ten micrograms of HYNIC-βAla-Bombesin(7–14), and 10 μl of 4.5 mM SnCl2·2H2O solution in 0.1 N HCl were added. The pH was adjusted to 7 with 10 μl of NaOH (1 mol/l). Next, an aliquot of 0.5 ml of Na99mTcO4 (37 MBq) was added. The solution was heated for 15 min in a water bath at 100 °C and cooled in water.
Radiochemical purity
Radiochemical purity analyses were performed by instant thin layer chromatography on silica gel (ITLC-SG, Merck) and reverse phase high-performance liquid chromatography (HPLC).
ITLC-SG analysis was accomplished using two different mobile phases: Methylethylketone to determine the amount of free 99mTcO4 − and a solution of acetonitrile:water (1:1) to identify the 99mTcO2. The HPLC analysis was performed using a Waters 717 with a radioactivity detector. HPLC solvents consisted of H2O, containing 0.1 % trifluoroacetic acid (solvent A) and acetonitrile containing 0.1 % trifluoroacetic acid (solvent B). A Symmetry C-18 column (5.0 μm, 4.6 × 150 mm) was used at a rate of 1.0 ml/min. The HPLC gradient system began with a solvent composition of 95 % A and 5 % B, and followed a linear gradient of 30 % A and 70 % B for 10 min and 5 % A: 95 % B from 10 to 15 min. In this system, retention times for free 99mTcO4 − and 99mTc-HYNIC-βAla-Bombesin(7–14) were 2–3 and 5–6 min, respectively.
Partition coefficient
Aliquots of 0.1 ml of the 99mTc-HYNIC-βAla-Bombesin(7–14) (0.37 MBq) were added to tubes containing 2.0 ml of n-octanol/water (1:1). The tubes were vigorously stirred for 3 min. After phase separation, aliquots of 0.5 ml from each phase were collected. Partition coefficient was determined using radioactivity measured in each aliquot by an automatic scintillation apparatus.
Plasma stability
ITLC-SG were used to estimate the plasma stability of 99mTc-HYNIC-βAla-Bombesin(7–14). A volume of 90 μl of labeled peptide solution was incubated, under agitation, at 37 °C with 1.0 ml of fresh mice plasma. Radiochemical stability was determined from samples taken at 1, 2, 4, 6, and 24 h after incubation.
Cysteine challenge
A fresh cysteine solution was prepared and diluted in different concentrations. Next, 0.9 ml of each cysteine solution was mixed with 0.1 ml of the labeled peptide solution. The molar ratios of cysteine to peptide were 1:1, 10:1, and 100:1. Each tube test was incubated at 37 °C, and the radiochemical purity was analyzed by ITLC at 1, 2, 4, 6, and 24 h post-incubation.
Blood clearance
The 99mTc-HYNIC-βAla-Bombesin(7–14) complex was administrated to each mouse (n = 3) through a tail vein, and blood samples (approximately 50 μl each) were collected at 1, 3, 5, 10, 15, 30, 45, 60, 90, and 120 min after administration. A small incision was made in the distal tail to facilitate rapid and reliable blood collection. Each sample was weighed, and the associated radioactivity was determined in an automatic scintillation apparatus. The percentage injected dose per gram (%ID/g) and its mean ± SD in each sample were determined, and the data were plotted as a function of time. Blood clearance analysis was performed using RSTRIP II (Micromath, Salt Lake City, UT, USA).
Cell culture
MDA-MB-231 cells were grown in Dulbecco’s modified Eagle’s medium (D-MEM, Gibco, USA), supplemented by 10 % (v/v) fetal bovine serum, penicillin (100 IU/ml), gentamicin (60 μg/ml), amphotericin B (0.25 μg/l), and streptomycin (100 μg/ml). Cells were kept in humidified air containing 5 % CO2 at 37 °C. The cells were grown to confluence and later harvested by trypsinization. After centrifugation (5 min at 330×g), cells were re-suspended in PBS for inoculation into the athymic nu/nu mice.
Tumor cell inoculation
Aliquots (100 μl) with 1 × 107 MDA-MB-231 cells were subcutaneously injected into the right thigh of female athymic nu/nu mice (17–23 g). Tumor cells were allowed to grow in vivo for 3 to 4 weeks post-inoculation, thus forming tumors with a diameter of no more than 10 mm. Breast tumor-bearing athymic nu/nu mice were used for biodistribution studies and scintigraphic images.
Cell binding, internalization assay, and non-specific binding
MDA-MB-231 cells supplied in D-MEM medium were diluted to 1 × 106 cells/tube and incubated with 99mTc-HYNIC-βAla-Bombesina(7–14) (0.3 nmol total peptide) in triplicate at 37 °C for 1 h and 4 h. The tubes were centrifuged (10 min, 3,000×g) and washed with 0.9 % NaCl. The activity of the cell pellet was determined in an automatic scintillation apparatus. Radioactivity in the cell pellet represents both externalized peptide and internalized peptide. An aliquot with the initial activity was taken as 100 %, and the cell uptake activity was then calculated.
To determine the percentage of internalization, the cell surface-bound radioligand (externalized peptide) was removed using an acid wash buffer (1 ml of 0.2 M acetic acid/0.5 M NaCl; pH 2.8) at room temperature for 5 min. The test tubes were centrifuged, washed with 0.9 % NaCl, and re-centrifuged. Pellet activity represented internalization. Non-specific binding was performed in parallel using the same aforementioned protocol; however, 40 μl (10 μM) of the cold HYNIC-βAla-Bombesin(7–14) were used to block GRP receptors.
Biodistribution studies
Aliquots of 3.7 MBq of the 99mTc-HYNIC-βAla-Bombesin(7–14) were injected intravenously into tumor bearing-athymic nu/nu mice (n = 5). After 1 h and 4 h, mice were anesthetized with a mixture of xylazine (15 mg/kg) and ketamine (80 mg/kg). Whole liver, spleen, kidney, stomach, heart, lungs, blood, muscle, thyroid, intestines, pancreas, and tumor were all removed, washed with distilled water, dried on filter paper, and placed in pre-weighed plastic test tubes. The radioactivity was measured using an automatic scintillation apparatus. A standard dosage containing the same injected amount was counted simultaneously in a separate tube, which was defined as 100 % radioactivity. The results were expressed as the percentage of injected dose/g of tissue (%ID/g). Receptor blocking studies were also carried out by the administration of 40 μg of cold bombesin together with the 99mTc-HYNIC-βAla-Bombesin(7–14).
Scintigraphic images
Aliquots of 18 MBq of the 99mTc-HYNIC-βAla-Bombesin(7–14) were injected intravenously into tumor bearing-athymic nu/nu mice (n = 5). Anesthetized mice were horizontally placed under the collimator of a gamma camera (Mediso, Hungary) employing a low-energy high-resolution collimator. Images were acquired at 1 and 4 h post-injection using a 256 × 256 × 16 matrix size with a 20 % energy window set at 140 keV for a period of 300 s.
Statistical analysis
All data are expressed as mean ± SD. Means between the various groups were compared for differences with analysis of variance. In case of multiple comparisons, a post hoc Bonferroni correction was applied. A P value <0.05 was considered to indicate a statistically significant difference. All data were analyzed by GraphPad PRISM version 5.00 software.
Results and discussion
Radiochemical purity and partition coefficient
The ITLC and HPLC were used for radiochemical analyses to predict the radiochemical purity of the 99mTc-HYNIC-βAla-Bombesina(7–14) complex, as previously described [2]. The results obtained by ITLC analyses showed a mean radiochemical purity for 99mTc-HYNIC-βAla-Bombesina(7–14) of 97.8 ± 0.9 % (n > 15), which remains stable after 24 h without post-labeling purification. HPLC analysis showed similar results, the 99mTc-HYNIC-βAla-Bombesina(7–14) complex presented a retention time of 5.26 min, and the lower peak, in a retention time of 2.41 min, was considered to be pertechnetate (Fig. 1, black line). The area for both peaks were calculated, and the 99mTc-HYNIC-βAla-Bombesina(7–14) complex showed a radiochemical purity equal to 96.2 %. In addition, HPLC analysis of the 99mTc-HYNIC-βAla-Bombesina(7–14) complex revealed high stability, since the complex showed the same retention time (Fig. 1, gray line) after 24 h post-labeling. The difference of intensity between the post-labeling line (black line) and the 24 h post-labeling line was attributed to the decay of technetium-99m. The presence of radiochemical impurities proved to be a drawback in nuclear medicine, yielding images with poor quality. Thus, it can be concluded that radiopharmaceuticals should contain high radiochemical purity (above 90 %). Therefore, the 99mTc-HYNIC-βAla-Bombesina(7–14) complex presented good chemical characteristics, since it presented a high radiochemical purity (>95 %).
Partition coefficient of the radiolabeled peptide was determined by the ratio between n-octanol and water. log P of 99mTc-HYNIC-βAla-Bombesina(7–14) could be observed within the hydrophilic range (log P = −1.78).
Plasma stability and cysteine challenge
Radiochemical stability was evaluated for the 99mTc-HYNIC-βAla-Bombesina(7–14) radiopharmaceutical at 1, 2, 4, 6, and 24 h in mice plasma. An excellent stability, even over long periods of time (>90 %), could be observed. The radiopharmaceutical was also evaluated by transchelation toward cysteine. After incubation with 1:1, 10:1 and 100:1 molar ratios of cysteine to peptide, ITLC revealed that the radioactivity dissociated from 99mTc-HYNIC-βAla-Bombesina(7–14) was less than 10 % (Table 1). These data indicated a high stability in all assays.
Blood clearance
Blood clearance for 99mTc-HYNIC-βAla-Bombesina(7–14) was rapid (Fig. 2), showing a biphasic profile with α half-life of 12.9 min and β half-life of 3.2 min. This data supported early imaging, since the background radiation will not contribute to a decrease in imaging quality [36].
Cell binding and internalization assay
The binding affinity of 99mTc-HYNIC-βAla-Bombesina(7–14) for GRP receptors was evaluated for MDA-MB-231 cells. The in vitro results showed an important uptake, which was significantly inhibited by the co-incubation of cold HYNIC-βAla-Bombesina(7–14) during all assayed times (Fig. 3). This data confirmed the in vitro specificity of 99mTc-HYNIC-βAla-Bombesina(7–14) for GRP receptors presented on cell membranes of the breast tumor.
Internalization analysis showed moderate values for 99mTc-HYNIC-βAla-Bombesina(7–14), presenting 16.8 and 20.0 % internalized activity after 1 and 4 h post-injection, respectively. The values increased proportionally with the time of incubation, illustrating that internalization was time-dependent. These results were higher than values reported for other BBN analogs [13], which confirmed that this analog presents a sufficient affinity for GRP receptor-expressing tumors.
Biodistribution studies and scintigraphic images
Results obtained from in vitro studies suggested that the BBN derivative can be used as a radiotracer. However, these tests are not a dependable index of clinical usefulness. Therefore, it is only possible to predict the real feasibility of 99mTc-HYNIC-βAla-Bombesina(7–14) after having performed biodistribution studies [37].
99mTc-HYNIC-βAla-Bombesina(7–14) biodistribution is shown in Table 2. Maximum uptake could be observed in the kidneys, indicating a main renal excretion; however, hepatobiliary clearance is also present. These data corroborate with partition coefficient results, since hydrophilic molecules are preferably eliminated through renal excretion [38]. The radiotracer revealed rapid blood clearance, with only 0.45 %ID/g at 1 h, followed by a further decrease at 4 h. This result coincides with data shown in the blood clearance assay, which is important to allow for early imaging [36].
The pancreas is typically used as an indicator of GRP receptor specificity for BBN derivatives [37, 39]. In the present study, the pancreas presented a higher uptake, when compared with the non-excretory organs, such as the spleen, the liver, and muscles due to its GRPR expression, indicating that BBN acts as a targeting vector. Moreover, in blocked studies, pancreas uptake at 1 and 4 h post-injection was reduced, from unblocked biodistribution, by 56 and 87 %, respectively (Table 2).
This finding suggests specificity for GRP receptors.
Tumors showed a moderate uptake, the highest of which was recorded at 4 h, indicating the trapping of 99mTc-HYNIC-βAla-Bombesin(7–14) in the tumor site, due to the fact that GRP receptors are present on the surface of MDA-MB-231 cell line [10, 12, 40]. Higher tumor uptakes have been reported in other studies [41–43]; however, this can be explained due to the fact that different cell lines were evaluated (e.g., PC-3), which express higher GRP receptor densities when compared to the cell lines analyzed in this work (MDA-MB-231) [13, 44]. Nevertheless, tumor-to-muscle and tumor-to-blood ratios for 99mTc-HYNIC-βAla-Bombesin(7–14) presented high values at 4 h (6.00 and 4.69, respectively). It has been considered in the literature [45] that radiotracers showing target/non-target ratios of greater than 1.5 (50 % higher uptake in the target tissue) may be considered potential diagnostic agents. Furthermore, when cold HYNIC-βAla-Bombesin(7–14) was co-administrated, the results showed a significant reduction in tumor-to-muscle ratios of 50.0 % at 1 h and 65.2 % at 4 h post-injection, as observed in Fig. 4. Therefore, there is strong evidence pointing to the 99mTc-HYNIC-βAla-Bombesin(7–14) specificity for GRP receptors.
Scintigraphic studies performed in breast tumor-bearing athymic nu/nu mice revealed similar excretion profiles. Although tumor uptake was lower than those observed in other studies [41–43], strong signals in the tumor area could be observed in the scintigraphic images, most likely due to the rapid clearance presented for 99mTc-HYNIC-βAla-Bombesin(7–14) (Fig. 5). The quantitative analyses of scintigraphic images showed tumor-to-muscle ratios for 99mTc-HYNIC-βAla-Bombesina(7–14) of 3.56 at 1 h and 5.15 at 4 h, demonstrating no statistical difference between biodistribution and scintigraphic studies. These results showed a tropism of the 99mTc-HYNIC-βAla-Bombesin(7–14) to the tumor during the entire experiment.
Scintigraphic images of breast tumor-bearing athymic nu/nu mice at 1 h (a) and 4 h (b) after radiopharmaceutical administration. While under ketamine/xylazine anesthesia, 18 MBq of 99mTc-HYNIC-βAla-Bombesina(7–14) were injected into the tail vein. The length of scan was 300 s. The arrows show tumor area
Conclusions
The peptide HYNIC-βAla-Bombesin(7–14) was successfully labeled with technetium and demonstrated a high level of stability. In vitro assays confirmed the affinity of 99mTc- HYNIC-βAla-Bombesin(7–14) to MDA-MB-231 cells. Biodistribution and scintigraphic studies showed adequate tumor-to-muscle ratios in breast tumor-bearing athymic nu/nu mice. In summary, these results showed the feasibility of 99mTc- HYNIC-βAla-Bombesin(7–14) as a functional agent in tumor diagnoses.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
de Barros ALB, Mota LG, Ferreira CA, Oliveira MC, Góes AM, Cardoso VN (2010) Bombesin derivative radiolabeled with technetium-99m as agent for tumor identification. Bioorg Med Chem Lett 10:6182–6184
Dijkgraaf I, Rijnders AY, Soede A, Dechesne AC, van Esse GW, Brouwer AJ, Corstens FHM, Boerman OC, Rijkers DTS, Liskamp RMJ (2007) Synthesis of DOTA-conjugated multivalent cyclic-RGD peptide dendrimers via 1,3-dipolar cycloaddition and their biological evaluation: implications for tumor targeting and tumor imaging purposes. Org Biomol Chem 5:935–944
Froidevaux S, Eberle AN, Christe M, Sumanovski L, Heppeler A, Schmitt JS, Eisenwiener K, Beglinger C, Macke HR (2002) Neuroendocrine tumor targeting: study of novel gallium-labeled somatostatin radiopeptides in a rat pancreatic tumor model. Int J Cancer 98:930–937
Froidevaux S, Heppeler A, Eberle AN, Meier A, Hausler M, Beglinger C, Béthé M, Powell P, Macke HR (2000) Preclinical comparison in AR4-2J tumor-bearing mice of four radiolabeled 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-somatostatin analogs for tumor diagnosis and internal radiotherapy. Endocrinology 141:3304–3312
Henze M, Schuhmacher J, Hipp P, Kowalski J, Becker DW, Doll J, Macke HR, Hofman M, Debus J, Haberkorn U (2001) PET imaging of somatostatin receptors using [68Ga]DOTA-D-Phe1-Tyr3-Octreotide: first results in patients with meningiomas. J Nucl Med 42:1053–1056
Zhang H, Chen J, Waldherr C, Hinni K, Waser B, Reubi JC, Maecke HR (2004) Synthesis and evaluation of bombesin derivatives on the basis of pan-bombesin peptides labeled with Indium-111, Lutetium-177, and Yttrium-90 for targeting bombesin receptor-expressing tumors. Cancer Res 64:6707–6715
Munnink THO, Nagengast WB, Brouwers AH, Schroder CP, Hospers GA, Lub-de Hooge MN, Van der Wall E, Van Diest PJ, Vries EGE (2009) Molecular imaging of breast cancer. Breast J S3:S66–S73
Schottelius M, Wester H (2009) Molecular imaging targeting peptide receptors. Methods 48:161–177
Faintuch BL, Teodoro R, Duatti A, Muramoto E, Faintuch S, Smith CJ (2008) Radiolabeled bombesin analogs for prostate cancer diagnosis: preclinical studies. Nucl Med Biol 35:401–411
Koopmans KP, Neels ON, Kema IP, Elsinga PH, Links TP, Vries EGE, Jager PL (2009) Molecular imaging in neuroendocrine tumors: molecular uptake mechanisms and clinical results. Crit Rev Oncol Hematol 71:199–213
Okarvi SM, Al-Jammaz I (2003) Synthesis, radiolabelling and biological characteristics of a bombesin peptide analog as a tumor imaging agent. Anticancer Res 23:2745–2750
Santos-Cuevas CL, Ferro-Flores G, Merphy CA, Ramírez FM, Luna-Gutiérrez MA, Pedraza-Lopez M, Gárcia-Becera R, Ordaz-Rosado D (2009) Design, preparation, in vitro and in vivo evaluation of 99mTc-N2S2-Tat(49–57)-bombesin: a target-specific hybrid radiopharmaceutical. Int J Pharm 375:75–83
Virgolini IJ, Gabriel M, Guggenberg EV, Putzer D, Kendler D, Decristoforo C (2009) Role of radiopharmaceutical in the diagnosis and treatment of neuroendocrine tumours. Eur J Cancer 45:274–291
Zhang K, Aruva MR, Shanthly N, Cardi CA, Patel CA, Rattan S, Cesarone G, Wickstrom E, Thakur ML (2007) Vasoactive intestinal peptide (VIP) and pituitary adenylate cyclase activating peptide (PACAP) receptor specific peptide analogues for PET imaging of breast cancer: in vitro/in vivo evaluation. Regul Pept 144:91–100
Anastasi A, Erspamer V, Bucci M (1971) Isolation and structure of bombesin and alytesin, 2 analogous active peptides from the skin of the European amphibians Bombina and Alytes. Experientia 27:166–167
Reubi JC (2003) Peptide receptors as molecular targets for cancer diagnosis and therapy. Endocr Rev 24:389–427
Jensen RT, Battley JF, Spindel ER, Benya RV (2008) Mammalian bombesin receptors: nomenclature, distribution, pharmacology, signaling, and functions in normal and disease states. Pharmacol Rev 60:1–42
Gonzalez N, Moody TW, Igarashi H, Ito T, Jensen RT (2008) Bombesin-related peptides and their receptors: recent advances in their role in physiology and disease states. Curr Opin Endocrinol Diabetes Obes 15:58–64
Smith CJ, Volkert WA, Hoffman TJ (2005) Radiolabeled peptide conjugates for targeting of the bombesin receptor superfamily subtypes. Nucl Med Biol 32:733–740
Schulz S, Rocken C, Schulz S (2006) Immunohistochemical detection of bombesin receptor subtypes GRP-R and BRS-3 in human tumors using novel antipeptide antibodies. Virchows Arch 449:421–427
Weber HC (2009) Regulatory and signaling of human bombesin receptor and their biological effects. Curr Opin Endocrinol Diabetes Obes 16:66–71
Langer M, Beck-Sickinger AG (2010) Peptides as carrier for tumor diagnosis and treatment. Curr Med Chem Anticancer Agents 1:71–93
Schuhmacher J, Zhang H, Doll J, Macke HR, Matys R, Hauser H, Henze M, Haberkorn U, Eisenhut M (2005) GRP receptor-targeted PET of a rat pancreas carcinoma xenograft in nude mice with a 68 Ga-labeled bombesin(6–14) analog. J Nucl Med 46:691–699
Scopinaro F, de Vincentis AD, Varvarigou AD (2005) Use of radiolabeled bombesin in humans. J Clin Oncol 23:3170–3171
van de Wiele C, Phonteyne P, Pauwels P, Goethals I, Van den Broecke R, Cocquyt V, Dierckx RA (2008) Gastrin-releasing peptide receptor imaging in human breast carcinoma versus immunohistochemistry. J Nucl Med 49:260–264
Hoffman TJ, Quinn TP, Volkert WA (2001) Radiometalled receptor-avid peptide conjugates for specific in vivo targeting of cancer cells. Nucl Med Biol 28:527–539
Hoffman TJ, Gali H, Smith CJ, Sieckman GL, Hayes DL, Owen NK, Volkert WA (2003) Novel series of 111In-labeled bombesin analogs as potential radiopharmaceuticals for specific targeting of gastrin-releasing peptide receptors expressed on human prostate cancer cells. J Nucl Med 44:823–831
Kunstler JU, Veerendra B, Figueroa SD, Sieckman GL, Rold TL, Hoffman TJ, Smith CJ, Pietzsch HJ (2007) Organometallic 99mTc(III) ‘4 + 1’ bombesin(7–14) conjugates: syntesis, radiolabeling, and in vitro/in vivo studies. Bioconjug Chem 18:1651–1661
Liu Z, Li ZB, Cao Q, Liu S, Wang F, Chen X (2009) Small-animal PET of tumors with 64Cu-labeled RGD-bombesin heterodimer. J Nucl Med 50:1168–1177
Zhang X, Cai W, Cao F, Schreibmann E, Wu Y, Wu JC, Xing L, Chen X (2006) 18F-labeled bombesin analogs for targeting GRP receptor-expressing prostate cancer. J Nucl Med 47:492–501
de Barros ALB, Cardoso VN, Mota LG, Alves RJ (2010) Synthesis and biodistribution studies of carbohydrate derivative radiolabeled with technetium-99m. Bioorg Med Chem Lett 20:315–317
Yang DJ, Kim C, Schechter NR, Azhdarinia A, Yu D, Oh C, Bryant JL, Won J, Kim EE, Podoloff DA (2003) Imaging with 99mTc-ECDG targeted at the multifunctional glucose system: feasibility studies with rodents. Radiology 226:465–473
Surfraz MB, King R, Mather SJ, Biagini SCG, Blower PJ (2007) Trifluoroacetyl-HYNIC peptide: synthesis and 99mTc radiolabeling. J Med Chem 50:1418–1422
Miranda-Olvera AD, Ferro-Flores G, Pedraza-López M, Murphy CA, León-Rodríguez LM (2007) Synthesis of oxytocin HYNIC derivative as potent diagnostic agent for breast cancer. Bioconjug Chem 18:1560–1567
Zhang K, Aruva MR, Shanthly N, Cardi CA, Rattan S, Patel C, Kim C, McCue PA, Wickstrom E, Thakur ML (2008) PET imaging of VPAC1 expression in experimental and spontaneous prostate cancer. J Nucl Med 49:112–121
Smith CJ, Gali H, Sieckman GL, Higginbotham C, Volkert WA, Hoffman TJ (2003) Radiochemical investigation of 99mTc-N3S-X-BBN[7–14]NH2: an in vitro/in vivo structure-activity relationship study where X = 0-, 3-, 5-, 8- and 11-carbon tethering moieties. Bioconjug Chem 14:93–102
Kim I, Kim TH, Ma K, Park ES, Oh KT, Lee ES, Lee KC, Youn YS (2011) A 4-arm polyethylene glycol derivative conjugated with exendin-4 peptide and palmitylamine having dual-function of size-increase and albumin-binding for long hypoglycemic action. Regul Pept 167:239–245
Nock B, Nikolopoupou A, Chiotellis E, Loudos G, Maintas D, Reubi JC, Maina T (2003) [99mTc]Domobesin 1, a novel potent bombesin analogue for GRP receptor-targeted tumour imaging. Eur J Nucl Med Mol Imaging 30:247–258
Chao C, Ives K, Hellmich HL, Townsend CM, Hellmich MR (2009) Gastrin-releasing peptide receptor in breast cancer mediates cellular migration and interleukin-8 expression. J Surg Res 156:26–31
Cescato R, Maina T, Nock B, Nikolopoulou A, Charalambidis D, Piccand V, Reubi JC (2008) Bombesin receptor antagonists may be preferable to agonists for tumor targeting. J Nucl Med 49:318–326
Maina T, Nock BA, Zhang H, Nikolopoulou A, Waser B, Reubi J, Maecke HR (2005) Species differences of bombesin analog interactions with GRP-R define the choice of animal models in the development of GRP-R-targeting drugs. J Nucl Med 46:823–830
Mansi R, Wang X, Forrer F, Waser B, Cescato R, Graham K, Borkowski S, Reubi JC, Maecke HR (2011) Development of a potent DOTA-conjugated bombesin antagonist for targeting GRPr-positive tumours. Eur J Nucl Med Mol Imaging 38:97–107
Halmos G, Wittliff JL, Schally AV (1995) Characterization of bombesin/gastrin-releasing peptide receptors in human breast cancer and their relationship to steroid receptor expression. Cancer Res 55:280–287
Phillips WT (1999) Delivery of gamma-imaging agents by liposomes. Adv Drug Deliv Rev 37:13–32
Acknowledgments
We wish to thank Pro-Reitoria de Pesquisa (UFMG), Comissão Nacional de Energia Nuclear (CNEN-Brazil), and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG-Brazil) for their financial support and fellowships.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Barros, A.L.B., das Graças Mota, L., de Aguiar Ferreira, C. et al. 99mTc-labeled bombesin analog for breast cancer identification. J Radioanal Nucl Chem 295, 2083–2090 (2013). https://doi.org/10.1007/s10967-012-2331-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-012-2331-8