Abstract
Shikonin was isolated from Ratanjot pigment then the obtained shikonin was well characterized. This study is aimed to optimize radiolabeling yield of shikonin with 99mTc with respect to factors that affect the reaction conditions such as shikonin amount, SnCl2·2H2O amount, reaction time and pH of the reaction mixture. In vitro stability of the radiolabeled complex was checked and it was found to be stable for up to 6 h. Biodistribution studies showed that, 99mTc–shikonin accumulate in tumor sites with higher T/NT than other currently available 99mTc(CO)3-VIP, 99mTc–nitroimidazole analogues and 99mTc–polyamine analogues indicating that shikonin deliver 99mTc to the tumor sites with a percentage sufficient for imaging and can overcome many drawbacks of other radiopharmaceuticals used for tumor imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Shikon (Lithospermum erythrorhizon Sieb. et Zucc, Chinese name: Zicao), a herbal plant, has been used in complementary and alternative medicine for thousands of years. Its dried root possesses therapeutic properties evidenced by it inhibits inflammation and enhances wound healing [1, 2]. The antitumor activity of shikon has been observed and confirmed by western science [1, 3]. Studies demonstrated that shikon arrests the cell cycle at G1/G0 and induces apoptosis in tumor cells [4].
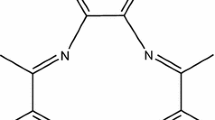
Several bioactive components in Shikon have been identified and purified including β,β-dimethylacrylalkannin, acetylshikonin, β-acetoxyisvaleryl alkannin, shikonin (SK) and β-hydroxyisovalerylalkannin [5]. In particular, SK (Fig. 1) has been characterized as a key component, and studies demonstrated that it has antiinflammatory and antitumor activities [6]. SK inhibits tumor cell proliferation in different cancer cell lines [7–9].
Decreased tissue oxygen tension (hypoxia) in tumor cells is thought to result in increased resistance of solid tumors to radiotherapy and chemotherapy.
The development of noninvasive imaging radiopharmaceutical targeted to tumor hypoxia represents a solution for the wide drawback of the invasive methods to diagnose hypoxia. In the development of hypoxia imaging agent, nitroimidazole analogues, which are enzymatically reduced and accumulated in hypoxic regions, have received great attention as hypoxia imaging agents. Several 99mTc labeled nitroimidazole analogues have been reported, however they showed some defects like, lower tumor uptakes and slow blood clearance [10–15].
Recently, 18F-Fluoromisonidazole ([18F]FMISO) [16, 17], 99mTc(CO)3-VIP and 99mTc–polyamine analogues has been used to evaluate tumor hypoxia [18]. But, the short half life and high cost of the [18F] isotope restrict the wide application of [18F]FMISO in clinical nuclear medicine while 99mTc(CO)3-VIP and 99mTc–polyamine analogues showed low percent tumor hypoxia uptake ranging from 0.5 to 1 [19, 20].
Many studies showed that shikonin exerted antitumor effects by inhibiting cancer cell growth [10], inducing apoptosis [21] and inhibiting DNA topoisomerase I/II activity, [7, 22, 23] antitelomerase activity [24] and antiangiogenesis. [25] Ratanjot pigment was used as a source for shikonin and the real source of Ratanjot was recently reported to be applied to about 15 plant species belonging mostly to family Boraginaceae including Lithospermum erythrorhizon [26]. Phytochemical investigation of authentic ratanjot hexane solubles was performed by many researchers and shikonin was reported as one of its components beside its ester derivatives [26, 27]. In this study shikonin was obtained from Ratanjot hexane extract after being subjected to alkaline hydrolysis and characterized with different analytical techniques. Shikonin was labeled with 99mTc and factors affecting the labeling yield were studied in details. 99mTc–shikonin complex was biologically investigated in mice bearing solid tumor.
Experimental
General
Melting points were determined on Branstead Google electrothermal melting point apparatus and are uncorrected. Infrared (IR) spectra were recorded on Perkin Elmer FT-IR Spectrum BX Spectrometer at cm−1 scale using KBr discs. 1H-NMR and 13C-NMR were carried out on Bruker AC 500 MHz and JEOL 300 MHz Spectrometer using TMS as internal stander and chemical shift values were recorded in ppm on δ scale. The 1HNMR data were represented as follow: chemical shifts, multiplicity (s. single, d. doublet, t. triplet, q. quartet, b. broad, m. multiplet) and number of protons. 13CNMR data were represented as chemical shifts and type of carbon. Thin layer chromatography was performed on precoated (0.75 mm) silica gel GF254 plates (E. Merck, Germany). Visualization was performed by illumination with UV light source (254 nm). Standard shikonin was purchased from Biomol (Plymouth Meeting, PA, USA).
Extraction and hydrolysis of shikonin ester derivatives
Ratanjot powder was purchased from Canadian store cranberry lane (0.5 kg) and was extracted with n-hexane using soxhlet until no more pigment was removed. The extract was evaporated to give red viscous oil (6 g). The pigment (0.5 g) was shaken with aqueous 2 N-sodium hydroxide at RT for one hour. The blue solution was filtered, cooled in ice, and acidified with dilute acetic acid. The red suspension was extracted with chloroform (3 × 150 ml). The phenolic hydrolysis product was obtained as a red solid by evaporation of the chloroform solution. Repeated crystallization from ether-petroleum yielded shikonin as red prisms (100 mg), m.p. 147–148° (lit., 147°), R f 0.44 (n-hexane/ethyl acetate 80:20 v/v) identical with authentic sample of shikonin.
Shikonin: red prisms; R f 0.44 (n-hexane/ethylacetae 80:20 v/v); 1H-NMR (CDCl3, 500 MHz) δ 1.68 (3 H, s, CH3-5′), 1.78 (3 H, s, CH3-6′), 2.38, 2.66 (2 H, m, H-2′), 4.93 (1 H, dd, J = 4.5, 3 Hz, H-1′), 5.23 (1 H, m, H-3′), 7.18 (1 H, s, H-3), 7.20 (2 H, s, H-6, 7), 12.45 (1 H, s, OH-5), 12.60 (1 H, s, OH-8); 13C-NMR (CDCl3, 500 MHz) δ 18.1 (C-5′), 26.0 (C-6′), 35.7 (C-2′), 68.3 (C-1′), 111.5 (C-10), 112.0 (C-9), 118.5 (C-3′), 131.7 (C-3), 132.3 (C-7), 132.4 (C-6), 137.4 (C-4′), 151.5 (C-2), 164.9 (C-8), 165.5 (C-5), 179.8 (C-4), 180.6 (C-1); IR νmax (cm−1): 3436 (OH), 1696 (C=O),1610 (C=O), 1452 (C=C). Comparison of NMR and IR data with that of an authentic sample of shikonin showed the two to be indistiguishable.
Labeling procedure
Exactly 600 μg of shikonin, dissolved in 1 ml N2-purged distilled water, were separately transferred to evacuated penicillin vials. Exactly 50 μg of SnCl2·2H2O was added to each vial along with different amounts of 0.1 N NaOH or 0.1 N HCl to adjust pH in a range of 1–7. Then, 1 ml of freshly eluted 99mTcO4 − (400 MBq) was added to each vial. The reaction mixtures were left at room temperature for 30 min. The same procedure was repeated with varying SnCl2·2H2O amounts (10–70 μg), varying shikonin amounts (500–750 mg), and different reaction times (5–450 min).
Radiochemical purity of 99mTc–shikonin complex
The percent labeling yield of the labeled 99mTc–shikonin complex was determined by using ascending paper chromatographic technique. Strips of Whatman No. 1 paper chromatography of 13 cm long and 0.5 cm wide were marked at a distance of 2 cm from the lower end and lined into sections 1 cm each up to 10 cm. A spot from 99mTc–shikonin complex solution was applied using hypodermic syringe, and then the strip was developed in an ascending manner in a closed jar filled with N2 gas to prevent oxidation of the labeled shikonin spot. The developing solvents were acetone for developing one paper and saline (0.9 % NaCl) for developing another one. After complete development, the strips were dried and cut into fragments 1 cm each. Then the sections were counted in a NaI(Tl) γ-ray scintillation counter.
It was further confirmed by a Shimadzu HPLC system, which consists of pumps LC-9A, Rheodyne injector and UV spectrophotometer detector (SPD-6A) operated at a wavelength of 520 nm. Chromatographic analysis was performed by injection of 10 μl from the reaction mixture of 99mTc–shikonin into a reversed-phase column (Lichrosorb RP18, 4 mm × 250 mm; 5 μm). The isocratic solvent system used was CH3CN: H2O: CH3COOH:Et3N (630: 370: 3: 3, v/v). Chromatography was performed at a flow rate of 0.5 ml/min, injection volume of 10 μl, pressure of 140 bar, and a column temperature of 23 °C. Fractions of 0.5 ml were collected separately using a fraction collector up to 12 ml and counted in a well-type γ-scintillation counter.
In vitro stability of 99mTc–shikonin complex
The in vitro stability of 99mTc–shikonin complex was investigated as a function of time up to 8 h post labeling.
Induction of tumor in mice
The parent tumor line (Ehrlich Ascites Carcinoma) was withdrawn from 7 days old donor female Swiss Albino mice and diluted with sterile physiological saline solution to give 12.5 × 106 cells/ml. Exactly 0.2 ml solution was then injected intramuscularly in the right thigh to produce a solid tumor. The animals were maintained till the tumor development was apparent (10–15 day) [28].
Biodistribution study
The study was approved by the animal ethics committee, Labeled Compound Department, and was in accordance with the guidelines set out by the Egyptian Atomic Energy Authority. Biodistribution of 99mTc–shikonin was carried out in a group of male Albino Swiss mice weighted 20–25 g. Each animal was injected in the tail vein with 0.2 ml solution containing 100 KBq of 99mTc–shikonin. The animals were sacrificed by cardiac puncture post anesthesia at 0.25, 1, 4 and 6 h post-injection (p.i.).
Various organs, tissue and tumors were excised following sacrifice, washed with normal saline, dried and the radioactivity associated with each organ and tissue was determined using a flat type NaI(Tl) counter. The weights of each organ and tumor were also determined by using an analytical balance. The percent injected dose (%ID) in various organs, tissue and tumor were calculated from the above data and expressed as %ID per gram (%ID/g) of organ/tissue. The total uptake in blood, bone and muscles were calculated by assuming that 7, 10 and 40 % of the body weight are constituted by this organs/tissue, respectively [29, 30]. Differences in the data were evaluated with the Student t test. Results for P using the two-tailed test are reported and all results are given as mean ± SEM. The level of significance was set at P < 0.05.
Results and discussion
Radiolabeling of 99mTc–shikonin complex
Using ascending paper chromatographic technique, The radiochemical purity of the formed 99mTc–shikonin complex was checked by using acetone as a developing solvent where free 99mTcO4 − was moved with the solvent front (R f = 1) while other species (reduced hydrolyzed 99mTc colloid and 99mTc–shikonin complex) remained at the point of spotting. The percentage of the reduced hydrolyzed-99mTc was calculated using saline as developing solvent where reduced hydrolyzed-99mTc colloid remained at the origin (R f = 0) while free 99mTcO4 − and 99mTc–shikonin complex migrate to the top of the paper. The percent of 99mTc–shikonin complex were determined as follows:
An HPLC radiochromatogram (Fig. 2) showed two peaks, one at fraction number 2, which corresponds to 99mTcO4 − whereas the second peak was collected at fraction number 10, which corresponds to 99mTc–shikonin complex, which was found to coincide with the UV signal. Nearly, 98 % of the injected activity in the HPLC was recovered as collected activity.
Effect of shikonin concentration
As shown in Fig. 3, at low shikonin concentration (500 μg) the yield was small and equal to 85.3 ± 0.9 %. These low labeling yields were due to the shikonin concentrations being insufficient to form complex with all of the reduced technetium so, the remaining reduced 99mTc was converted to reduced hydrolyzed technetium colloid (13.5 ± 2.1 %). Increasing the shikonin concentration lead to higher labeling yield and the maximum yield of 96.5 ± 4.75 % was achieved at 600 μg. Increasing the shikonin concentration over the optimum values, nearly did not affect on the labeling yield.
Effect of SnCl2·2H2O concentration
For contributing most of 99mTc to increase the labeling yield of shikonin, SnCl2·2H2O is the best reducing agent for reduction of 99mTc from (VII) to lower valence state, which facilitates its chelation by shikonin. The effect of the amount of stannous chloride was summarized in Fig. 4. At 10 μg SnCl2·2H2O, the labeling yield of 99mTc–shikonin was low (12.6 ± 0.3 %) due to SnCl2·2H2O concentration was insufficient to reduce all pertechnetate so the percentage of 99mTcO4 − was high (84.6 ± 2.2 %). The labeling yield was significantly increased by increasing the amount of SnCl2·2H2O from 10 to 50 μg, at which maximum labeling yield of 96.5 ± 4.75 % was obtained. By increasing the amount of SnCl2·2H2O above the optimum concentration value, the labeling yield decreased again. This may be due to the fact that most of the ligand molecules were consumed in the formation of complexes, so the pertechnetate is reduced to insoluble technetium (IV) TcO2·xH2O in the absence of ligand [31] or due to the fact that the excess amount of stannous chloride leads to the formation of stannous hydroxide colloid Sn(OH)3 (41.5 ± 1.1 % at 70 μg SnCl2·2H2O) in basic medium [32, 33].
Effect of pH of the reaction mixture
Figure 5 clearly shows that, the labeling yield of 99mTc–shikonin complex was increased with increasing the pH of the reaction mixture where at pH 1 the labeling yield was 68.3 ± 1.8 % and at pH value equal to 5, the maximum labeling yield (96.5 ± 4.75 %) was obtained where at this pH value shikonin combined all the reduced 99mTc. When the pH value was increased towards the neutral pH, the percent labeling yield was decreased again which reached to 87.4 ± 1.5 % at pH 7.
Effect of reaction time and stability
Figure 6 describes the labeling yield of 99mTc–shikonin complex at different reaction times.
The labeling yield of 99mTc–shikonin complex increased with time till reaching 96.5 ± 4.75 % at 30 min reaction time. It remained constant (~96 %) even when the reaction time was extended to 6 h.
Biodistribution
Biodistribution of 99mTc–shikonin in solid tumor bearing mice was found to be greatest in blood, heart and lung (16.8 ± 0.2, 6.0 ± 0.1 and 4.1 ± 0.2 %, respectively) at 15 min post injection and lowest in left leg and Stomach (1.06 ± 0.03 and 0.1 ± 0.0, respectively) (Table 1). Most of radioactivity was excreted through the urinary pathway where the activity in urine reached to 42.8 ± 2.2 % at 6 h post injection. The activity uptake of 99mTc–shikonin in the right thigh (inoculated) was greater than that of left one at all time intervals. The maximum T/NT for 99mTc–shikonin (T/NT = 8.63) was significantly higher than that of the currently available 99mTc(CO)3-VIP, nitroimidazole analogues and 99mTc–polyamine analogues (T/NT = 0.5–1) indicating that shikonin deliver 99mTc to the tumor sites with a percentage sufficient for imaging and can overcome all drawbacks of other radiopharmaceuticals for tumor imaging.
Conclusion
In this study shikonin was isolated from Ratanjot pigment and then well characterized using different analytical techniques. Shikonin was labeled with 99mTc using simple and instantaneous method. The labeling of shikonin with 99mTc was optional in the following reaction mixture: 600 μg shikonin, 50 μg SnCl2·2H2O, pH 5 and 30 min reaction time. The formed complex was stable for time up to 6 h. 99mTc–shikonin was found to be highly localized in tumor sites (T/NT = 8.63) where shikonin was considered an ideal victor to carry 99mTc to the tumor cells. In conclusion, 99mTc–shikonin could be used as a new non nitroimidazole hypoxic imaging agent in the future and this study demonstrates a hopeful approach for cancer imaging.
References
Jiangsu XYXY (1986) Dictionary of Chinese Materia Medica. Shanghai Press of Science and Technology, Shanghai
Bown D (1995) Encyclopaedia of herbs and their uses. Dorling Kindersley, London
Lee H, Lin JY (1988) Mutat Res 204:229–234
Wang GL, Chen CB, Gao JM, Ni H, Wang TS, Chen L (2005) Zhongguo Zhong Yao Za Zhi 30:50–54
Chen X, Yang L, Oppenheim JJ, Howard MZ (2002) Phytother Res 16:199–209
Chen X, Yang L, Zhang N, Turpin JA, Buckheit RW, Osterling C, Oppenheim JJ, Howard OM (2003) Antimicrob Agents Chemother 47:2810–2816
Yoon Y, Kim YO, Lim NY, Jeon WK, Sung HJ (1999) Planta Medica 65:532–535
Singh F, Gao D, Lebwohl MG, Wei H (2003) Cancer Lett 200:115–121
Hsu PC, Huang YT, Tsai ML, Wang YJ, Lin JK, Pan MH (2004) J Agric Food Chem 52:6330–6337
Chu TW, Li RJ, Hu SW, Liu XQ, Wang XY (2004) Nucl Med Biol 31:199–203
Kong DJ, Lu J, Ye SZ, Wang XB (2007) J Label Compd Radiopharm. 50:1137
Mallia MB, Mathur A, Subramanian S, Banerjee S, Sarma HD, Venkatesh M (2005) Bioorg Med Chem Lett 15:3398
Mallia MB, Subramanian S, Banerjee S, Sarma HD, Venkatesh M (2006) Bioorg Med Chem 14:7666
Mallia MB, Subramanian S, Mathur A, Sarma HD, Venkatesh M, Banerjee S (2008) Bioorg Med Chem Lett 18:5233
Zhang Y, Chu TW, Gao XG, Liu XQ, Yang Z, Guo ZQ, Wang XY (2006) Bioorg Med Chem Lett 16:1831–1835
Yang DJ, Wallace S, Cherif A, Li C, Gretzer MB, Kim EE, Podoloff DA (1995) Radiology 194:795
Zhang J, Qian Y, Huo J, Pang Y, Yang S, He Y, Tang T, Yang C, Wang X (2010) J Radioanal Nucl Chem 283:481–487
Kanchan K, Sudhanand P, Aruna K, Archana M, Archana M, Manu J, Meera V, Ambikalmajan MRP, Rama M, Natesan R (2007) Appl Radiat Isot 65:382–386
Chiara DP, Alan CP, Sotiris M (2009) Nucl Med Biol 36:703–707
Wei-Xing W, Min Y, Shang-Ren P, Chun-Jing Y, Na-Jing W (2008) Drug Dev Res 69:520–526
Guo XP, Zhang XY, Zhang SD (1991) Zhong Xi Yi Jie He Za Zhi 11:598–599
Ahn BZ, Baik KU, Kweon GR, Lim K, Hwang BD (1995) J Med Chem 38:1044–1047
Plyta ZF, Li T, Papageorgiou VP, Mellidis AS, Assimopoulou AN, Pitsinos EN, Couladouros EA (1998) Bioorg Med Chem Lett 8:3385–3390
Fujii N, Yamashita Y, Arima Y, Nagashima M, Nakano H (1992) Antimicrob Agents Chemother 36:2589–2594
Lu Q, Liu W, Ding J, Cai J, Duan W (2002) Bioorg Med Chem Lett 12:1375–1378
Hisa T, Kimura Y, Takada K, Suzuki F, Takigawa M (1998) Anticancer Res 18:783–789
Arora A, Gulrajani ML, Gupta D (2009) Nat Prod Radiance 8:142–145
Srivastava A, Shukla YN, Sushil K (1999) J Med Aromat Plant Sci 12:1131–1138
Korde A, Venkatesh M (1998) International symposium on modem trends in radiopharmaceuticals for diagnosis and therapy, Lisbon, Portugal, vol 30, 3 April 1998, IAEA, SM-355/13
Awasthi V, Meinken G, Springer K, Srivastava SC, Freimuth P (2004) J Virol 78:6431–6438
Das T, Chakraborty S, Sarma HD, Tandon P, Banerjee S, Venkatesh M, Pillai MRA (2009) Nucl Med Biol 36:561–568
Srivastava SC, Richards P (1983) Technetium-labeled compounds. In: Rayudu GVS (ed) Radiotracers for medical applications, CRC series in radiotracers in biology and medicine. CRC Press, Boca Raton, pp 107–185
Wardell JL (1994) Tin: inorganic chemistry. In: King RB (ed) Encyclopedia of inorganic chemistry, vol 8. Wiley, New York, pp 4159–4197
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Motaleb, M.A., Al-Musayeib, N.M., Zaghary, W.A. et al. Synthesis and preclinical pharmacological evaluation of a novel 99mTc–shikonin as a potential tumor imaging agent. J Radioanal Nucl Chem 293, 391–396 (2012). https://doi.org/10.1007/s10967-012-1701-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-012-1701-6