Abstract
Celecoxib was labelled effectively with 99mTc. The labeling yield was found to be influenced by the amount of celecoxib, the amount of stannous chloride dihydrate, the reaction time, the temperature and the pH of the reaction mixture. The importance of stannous chloride dihydrate arises from its function as a reducing agent for pertechnetate to form complex celecoxib. The suitable amount required to produce high labeling yield of 99mTc-celecoxib was 500 μg SnCl2·2H2O. The pH of the reaction medium was found to play a significant role in this labeling process. The labeling reaction was performed at a neutral medium (pH 7). The labeling reaction proceeds well at room temperature (25 ± 1 °C) and the complex decomposes by heat. The labeled celecoxib (99mTc-celecoxib) showed a good localization in inflamed foci and a good imaging must be taken 4 h post injection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional imaging with radiotracers has been found to detect inflammatory processes with high sensitivity. This technique is also of great importance in monitoring response to therapy [1, 2]. Both specific and nonspecific radiopharmaceuticals have been tested to image inflammations as the result of infectious and noninfectious causes. The nonspecific mechanisms of tracer accumulation include enhanced blood flow, increased vascular permeability and possibly other factors. Specific accumulation of radiolabeled compounds in inflammatory lesions results from binding to activated endothelium (e.g. radiolabeled anti-E-selectin) [3], the enhanced influx of leukocytes (e.g. radiolabeled autologous leukocytes, anti-granulocyte antibodies or cytokines), the enhanced glucose-uptake by activated leukocytes (18F-fluorodeoxyglucose) [4] or by direct binding to micro-organisms (e.g. radiolabeled ciprofloxacin [5, 6], pefloxacin [7] and levofloxacin [8] or antimicrobial peptides). Although a multitude of agents have been tested and used for imaging infections and inflammations, gallium-67 (67Ga citrate) [9], labeled leukocytes with technetium-99m (99mTc) or indium-111 (111In) [1], and 18F-fluorodeoxyglucose (FDG) [4] have gained a wide acceptance for routine use. The ideal characteristics of an effective radiolabeled imaging agent in this setting include high sensitivity and specificity, ease of preparation, minimal toxicity and radiation dose and low cost in addition to rapid localization and good retention at site of infection and uptake in infection not in sterile inflammation in case of imaging infectious inflammation [10]. During the past decade, the focus in the development of new radiopharmaceuticals has greatly increased and studies are continuing to improve their effectiveness for diagnostic imaging in the future.
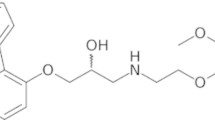
Celecoxib; 4-[5-(4-methylphenyl)-3-(trifluoromethyl)pyrazol-1-yl] benzene sulfonamide; (Fig. 1) is a nonsteroidal anti-inflammatory drug that exhibits anti-inflammatory, analgesic, and antipyretic activities [11]. It is used in the treatment of osteoarthritis, rheumatoid arthritis, acute pain, painful menstruation and menstrual symptoms [12]. It’s mechanism of action is believed to be due to inhibition of prostaglandin synthesis, primarily via inhibition of cyclooxygenase-2 (COX-2), and at therapeutic concentrations in humans, it does not inhibit the cyclooxygenase-1 (COX-1) isoenzyme. In animal colon tumor models, celecoxib reduced the incidence and multiplicity of tumors [13].
In this work, celecoxib was labelled with 99mTc. The reaction parameters were investigated and the labelled compound was examined as a possible diagnostic agent for inflammation imaging.
Experimental
Materials
All chemicals and laboratory reagents used in this work were of the highest purity grade. In all cases, double distilled water was used. Celecoxib, 4-[5-(4-methylphenyl)-3-(trifluoromethyl) pyrazol-1-yl] benzene sulfonamide, MF (C17H14F3N3O2S), MW 381.38 was obtained as a gift from Amoun Pharmaceutical Co. Cairo, Egypt. Stannous chloride dihydrate (SnCl2·2H2O), MW 225.6, was purchased from Sigma-Aldrich, Germany. Pertechnetate-99 m solution was obtained by elution from the sterile 99Mo/99mTc generator (Elutic, Brussels, Belgium). All other chemicals and reagents used were of analytical grade (AR). White Albino mice were used for biodistribution studies.
Methods
Preparation of stannous chloride dihydrate
The solution was prepared by dissolving 100 mg of the crystalline salt in 0.5 mL of conc. HCl with heating, and then the volume was completed to 10 mL using nitrogen purged double distilled water. One mL was again diluted to 10 mL with the same water. The solution was dispensed in 10 mL clean penicillin vials (0.5 mL each) and stored at 25 ± 1 °C.
99mTc-celecoxib preparation
Stannous chloride dihydrate solution (500 μL) was added to a solution of celecoxib in ethanol (0.5 mg/0.05 mL) in a clean sterile penicillin vial under positive nitrogen pressure. Pertechnetate solution (0.5 mL, ~750 MBq) was added and the reaction mixture was left for 30 min at 25 ± 1 °C.
Determination of the radiochemical purity of 99mTc-celecoxib
-
(a)
The percentages of colloids were determined by filtration of the reaction mixture through 0.22 μm Millipore filter [14] according to the following equation:
-
(b)
Instant thin layer chromatography-silica gel/methyl ethyl ketone (ITLC-SG/MEK) system was used to determine free pertechnetate and the labelled celecoxib in the filtrate. Free 99mTcO4 − moves with the solvent front (Rf = 1), while 99mTc-celecoxib complex remains at the starting line (Rf = 0). The labeling yield percent was calculated as follows:
Biodistribution studies
Sterile inflammation was induced by injecting sterile turpentine oil (200 μL), intramuscularly [15] (IM), into the right thigh muscle [16], while infectious (septic) inflammation was induced by IM injection of E. coli suspension [17]. When swelling of the muscle was apparent, 99mTc-celecoxib was injected intravenously (i.v.). Groups of three mice were used for each experiment. The mice were sacrificed by decapitation under chloroform anesthesia at 0.5, 1 and 4 h post injection, respectively. Blood samples were collected at the time of decapitation. Both thighs (right thigh muscle as target, left thigh muscle as control) and organs were dissected, weighed and their radioactivity measured using a well-type NaI scintillation detector. The activity distribution was determined in weighed fractions of blood, bone, and muscle and then calculated by using the following assumptions; blood represents 7%, bones represent 10% and muscles represent 40% of the body weight of the mouse [18].
Results and discussion
Factors affecting the labeling yield % of 99mTc-celecoxib:
Effect of stannous chloride dehydrate amount
The amount of tin (II) required to reduce pertechnetate from its heptavalent state to the reactive reduced state must be adjusted to prevent the formation of undesirable radiochemical species; such as colloids and free pertechnetate 99mTcO4 − especially in alkaline pH medium. To study the effect of stannous chloride dihydrate content on the formation of 99mTc-celecoxib complex, different amounts of stannous chloride dihydrate were ranged from 25 to 1,000 μg. The results obtained from the analysis of the reaction mixture after 30 min reaction time at room temperature (25 ± 1 °C) are shown in Fig. (2). As indicated in the figure, at low amounts of stannous chloride dihydrate (25 and 50 μg), the radiochemical yields of 99mTc-celecoxib are 52 and 58%, respectively indicating that the amount of the reducing agent was not sufficient to reduce all the pertechnetate present in the reaction medium. By increasing the amount of SnCl2·2H2O to 500 μg, the radiochemical yield of 99mTc-celecoxib increased to 99.67%. On the other hand, above 500 μg SnCl2·2H2O, colloidal solution was obtained and this may be due to the formation of Sn(OH)2 which is insoluble in the reaction medium.
Effect of celecoxib amount
The effect of the amount of celecoxib on the radiochemical yield % of 99mTc-celecoxib complex was studied and the results are shown in Fig. (3). The data indicate that at 500 μg of celecoxib, the radiochemical yield is 99.7%. No significant change in the radiochemical yield of 99mTc-celecoxib was observed in the range of 500–1,000 μg celecoxib. At low amounts of celecoxib (50 and 100 μg), the radiochemical yields of 99mTc-celecoxib were 85 and 90% indicating the insufficiency of celecoxib to complex all the reduced 99mTc ions.
Effect of pH of the reaction medium
The effect of pH of the reaction mixture on the radiochemical yield % of 99mTc-celecoxib was studied. The reaction was carried out at pH values ranging from 4 to 11. Labeling at pH 4 led to the formation of 99mTc-celecoxib complex with a radiochemical yield of 90%, while the radiochemical yield increased at pH 5, 7 and 9 to 98, 99.67 and 97.84%, respectively as shown in Fig. (4). At pH 10 and 11, the radiochemical yields decreased to 82 and 20%, respectively which is due to the formation of undesired radiochemical species as colloids.
Effect of reaction time
The effect of reaction time on the radiochemical yield % of 99mTc-celecoxib was investigated. The results are presented in Fig. (5). A gradual increase of the labeling yield with time was clearly observed. At 5 min reaction time, the radiochemical yield of 99mTc- celecoxib was 83.7%, while by increasing the reaction time to 15 min the radiochemical yield increased to 97%. The results also indicate also that, the highest labeling yield (99.67% of 99mTc-celecoxib) was achieved after 30 min at room temperature. Hence, 30 min would be enough for complete complex formation of 99mTc-celecoxib. Upon increasing the reaction time to 60 and 120 min, no significant change in the radiochemical yield was observed.
Effect of reaction temperature
The labeling of celecoxib with 99mTc was performed at 25 ± 1, 50 ± 1, 75 ± 1 and 100 ± 1 °C for 30 min. The results showed that the complexation between 99mTc and celecoxib was completely done at room temperature after 30 min with a high radiochemical yield of 99.67%. 99mTc-celecoxib complex was decomposed gradually by heating the reaction mixture in a water bath. The rate of decomposition increased as the reaction temperature increased. At 50 ± 1 and 75 ± 1 °C, 99mTc-celecoxib complex decomposed by 11.5 and 13.2%, respectively, while it decomposed by ~30% in a boiling water bath.
In vitro stability of 99mTc-celecoxib
The stability of 99mTc-celecoxib was studied in order to determine the suitable time for injection to avoid the formation of undesired products that result from the radiolysis of labeled compound. These undesired radioactive products may accumulate in non-target organs. The results of the in vitro stability of 99mTc-celecoxib are presented in Table (1). The data clearly show that 99mTc-celecoxib complex is stable for up to 24 h which is suitable for nuclear medicine applications.
Our results are in good agreement with previous confirmatory studies where H. Thakkar et al., who reported that celecoxib and albumin microspheres were labeled with 99mTc by direct labeling method. Also the labeling efficiency of celecoxib reached 98% at pH 6.5 [19].
Biodistribution of 99mTc-celecoxib in normal mice
The results of the in vivo biodistribution studies carried out in normal Albino Swiss mice at different time intervals after injection of 99mTc-celecoxib are shown in Table (2). The blood uptake was 27.9% at 15 min post injection and decreased to 13.0% at 4 h, indicating that the labelled compound cleared from the systemic circulation within 4 h post injection. The liver uptake decreased by time from 23.6 to 20.6 and 15.0% after 15 min, 1 and 4 h post injection, respectively. Kidneys showed high uptake indicating that the excretion was done through the kidneys to urine. Heart and lung uptake was not high as observed from the Table. The majority of organs showed significant decrease in uptake of 99mTc-celecoxib.
Detection of infections and sterile inflammatory foci in mice
Table 3 shows the biodistribution data of 99mTc-labeled celecoxib in sterile inflamed mice. The mice were injected with 0.2 mL of sterile turpentine oil (for sterile inflammation induction). It was observed that biodistribution of 99mTc-celecoxib nearly looks like that in normal mice. Inflamed muscle receives 99mTc-celecoxib more than normal muscle. The difference in uptake between inflamed and non inflamed muscle may be due to high vascularities to inflamed area so blood supply deliver more 99mTc-celecoxib to the inflamed muscle. The target/non target ratios for sterile inflamed mice were equal to 3.5/2.1, 4.8/2.3 and 4.7/1.9 at 15 min, 1 h and 4 h post injection, respectively. This means that this 99mTc labeled compound is able to localize in sterile inflammation and can be used as an inflammatory imaging agent.
The biodistribution of radioiodinated celecoxib confirmed its importance as a tumor imaging agent [20].
Conclusion
Conventional imaging typically provides information on only one part of the body and detects disturbance to the normal anatomy. In contrast, nuclear medicine can scan the whole body and localize occult disease processes. Nuclear medicine is very important in the diagnosis and localizing of the inflammations when conventional imaging is unsuccessful. The preliminary studies of a newly developed radiopharmaceutical, 99mTc-celecoxib; have proven its effectiveness as inflammation detecting agent. The product appeared to be safe, stable, and reproducible. High labeling efficiency of 99.67% could be achieved using 500 μg of the substrate and 500 μg stannous chloride dihydrate in a neutral medium of pH 7. Labeling reaction was simple and accomplished after 30 min at 25 ± 1 °C.
References
Basu S, Zhuang H, Torigian DA, Rosenbaum J, Chen W, Alavi A (2009) Sem Nucl Med 39(2):124
Laverman P, Corstens FH, Boerman OC, Oyen WJ (2008) Curr Radiopharm 1:42
Everts M, Koning GA, Kok RJ, Asgeirsdóttir SA, Vestweber D, Meijer DK, Storm G, Molema G (2003) Pharm Res 20(1):64
Harari OA, Al-Nahhas A, Jawad A (2008) Nucl Med Commun 29(9):838
Zhang J, Guo H, Zhang S, Lin Y, Wang X (2008) Bioorg Med Chem Lett 1(18):5168
Sierra JM, Rodriguez-Puig D, Soriano A, Mensa J, Piera C, Vila J (2008) Antimicrob Agents Chemother 52(7):2691
El-Ghany EA, Amin AM, El-Sayed AS, El-Kolaly MT, Abdel-Gelil F (2005) J Radioanal Nucl Chem 266(1):131
El-Ghany EA, Amin AM, El-Kawy OA, Amin M (2007) J Label Compd Radiopharm 50(1):25
Becker W, Meller J (2001) Lancet infect dis 1:326
Gemmel F, Dumarey N, Welling M (2009) Sem Nucl Med 39(1):11
Goodman AG, Gilman LS (2008). Analgesic-antipyretic and anti-inflammatory agents. Brunton LL, Parker KL (eds). McGraw-Hill, New York
Malhotra S, Shafiq N, Pandhi P (2004) Medscape Gen Med 6(1):6
Schiffmann S, Maier TJ, Wobst I, Janssen A, Wilhelm HC, Angioni C, Geisslinger G, Grösch S (2008) Biochem Pharmacol 76(2):179
Celerier C, Robert N, Bertrand-Barat J, Ducassou D (1997) Medecine Nucleaire Imagerie Fonctionnelle et Metabolique 21(6):373
Asikoglu M, Yurt F, Cagliyan O, Unak P, Ozkilic H (2000) Appl Radiat Isot 53:411
Oyen WJG, Boerman OC, Corstens FHM (2001) J Microbiol Methods 47:151
Vander Laken CJ, Boerman OC, Oyen WJG, Vande Ven MTP, Van der Meer JWM, Corstens FHM (2000) J Nucl Med 41:463
El-Kolaly MT, El-Wetery AS (1990) J Label Compd Radiopharm 28:329
Thakkar H, Sharma RK, Mishra AK, Chuttani K, Murthy RR (2005) AAPS PharmSciTech 6(1):E65–E73
El-Azony KM (2010) J Radioanal Nucl Chem 285:315–320
Acknowledgments
The authors wish to thank Prof. K. Farah and Prof. N. L. Mehany for their efforts in reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farouk, N., El-Tawoosy, M., Ayoub, S. et al. Optimization of the reaction conditions for the preparation of 99mTc-celecoxib and its biological evaluation. J Radioanal Nucl Chem 290, 685–690 (2011). https://doi.org/10.1007/s10967-011-1364-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-011-1364-8