Abstract
A preparation of 125I-celecoxib is carried out via an electrophilic substitution reaction. The reaction parameters studied were celecoxib concentration, reaction temperature, pH of the reaction mixture and kinds of oxidizing agents in order to obtain a high radiochemical yield of the 125I-celecoxib. Using 3.7 MBq of Na125I, 150 μg (3.9 mM (mmol/L)) of celecoxib, and 1.6 mM (mmol/L) of chloramine-T (CAT) as oxidant at pH 4 and 60 °C for 15 min a maximum radiochemical yield of 125I-celecoxib (65%) was obtained. The labeled compound was separated and purified by means of high pressure liquid chromatography (HPLC). The biological distribution in infected mice indicates the suitability of radioiodinated celecoxib as imaging of tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celecoxib (CEL), a cyclooxygenase-2 (COX-2) selective inhibitor is a non-steroid anti-inflammatory drug (NSAID) approved for the treatment of rheumatic pain and osteoarthritis [1]. This approval is based on its improved side effects profile in comparison to that observed for NSAIDs, especially during chronic use [2]. Available experimental and clinical data show improved gastric tolerance as compared to conventional, non-selective NSAIDs [3, 4]. Selective inhibition of COX-2, the main isoenzyme expressed during inflammation by CEL, is the main specification which reduces the serious side effects of NSAIDs associated with the inhibition of COX-1 seen with non-selective COX inhibitors [5].
Celecoxib has demonstrated potent anti-cancer activity in various animal tumor models in the laboratory [6]. Despite these promising results, however, the underlying molecular mechanisms by which celecoxib exerts its anti-tumor potential are not completely understood. Particularly intriguing are a number of reports describing potent anti-proliferative and pro-apoptotic effects of this drug in the absence of any apparent involvement of COX-2 [7]. The anti-tumor effects of celecoxib are studied in cell culture in vitro, concentrations in the range of 30–100 μM are generally required in order to achieve substantial growth inhibition or induction of apoptosis in tumor cells. On occasion, lower concentration of the drug might be effective as well, although in those cases reduced serum concentrations in the cell culture growth medium or longer incubation times seem to be required [8–11].
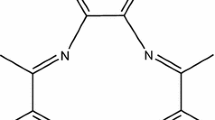
The COX-2, 5-(4-iodophenyl)-1-[4-(methylsulfonyl)phenyl]-3-trifluoromethyl-1H-pyrazole (IMTP) was labeled by iodine-125 and was assessed by comparison with the 125I-celecoxib analogue with a sulfonamide moiety (125I-IATP) [12].
The iodine-125 has been used in the labeling process for several reasons like its half-life is relatively long (T 1/2 = 59.4 days), it decays by electron capture (EC) with a probability of 10%, and then decays further by internal conversion (IC) with a probability of 93% to the stable tellurium-125. It is known as a very effective Auger electrons emitter, due to its specific decay characteristic. Thus, two successive Auger cascades occur per each decay of iodine-125, and consequently it emits 21 Auger electrons in condensed matters per decay. The energies of Auger electrons are between 10 eV and 34 keV. [13]. It is also interesting to note that the ranges of Auger electrons emitted by an iodine-125 atom can be reached up to about 40–45 nm [14], so if the iodine-125 reaches the infected cell nucleus for the treatment of proliferative tumor and apoptotic effects, it has no damage effect on the normal cell.
The present work concerns the labeling of celecoxib by iodine-125 depending on the significance of the celecoxib as chemotherapy beside its expected significance for the 125I-celecoxib (125I-Cel) as radiotherapy. So, the factors which affect the radiochemical yield of 125I-celecoxib such as celecoxib concentration, temperature, pH and oxidizing agent have been studied, and then the labeled compound (125I-Cel) has been purified by using HPLC for studying the biodistribution in infected mice.
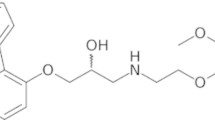
The presumable structure for 125I-Cel via reaction of celecoxib with Na125I in the presence of CAT as oxidizing agent is shown in Eq. 1; where 125I in the aromatic ring is in ortho position to the methyl group. 
Experimental
Materials
All chemicals used in the present work were of analytical grade. Celecoxib (4-[5-(4-methyl phenyl)-3-(trifluoromethyl)-1H-pyrazol-1-yl] benzene sulfonamide was presented by Amoun Pharmaceutical Company, Egypt. Absolute ethanol and dimethyl formamide (DMF) were used as a solvent without further purification. Double distilled water was used for all experiments. Chloramine-T [N-chloro-p-toluene sulfonamide salt (CAT)], N-Bromosuccinimide (NBS) were purchased from Aldrich. Thin layer chromatography (TLC) aluminum sheets (20 × 25 cm) SG-60 F254 (Merck). Na125I (185 MBq/50 μL) in diluted NaOH, pH 7–11 was purchased from Institute of Isotopes, Budapest, Hungary.
Equipment
Radioactivity was measured by means of a gamma counter (Nucleus Model 2010) connected with a well type NaI (Tl) crystal. HPLC [Merck-Hitachi Model], L-6000 pump, equipped with a Rheodyne injector (Syringe Loading Sample Injector-7125), L-4000 UV Spectrophotometric Detector Merck, D-2500 Chromat-Integrator and stationary phase comprising a reversed phase nucleosil phenyl column (250 mm × 4.6 mm, 5 μm).
Radioiodination procedure of celecoxib
All experiments were carried out in a convenient round bottom flask (5 mL) with two necks. The flask was fitted with a reflux condenser on one neck and the other neck was fitted with rubber stopper for withdrawing samples. The flask was immersed in a thermostatically controlled water bath. 10 μL Na125I (3.7 MBq) was added in the bottom of the flask and they were dried by a vacuum line, then the desired concentration of oxidizing agent, and the desired concentration of the substrate in a suitable medium were added. The reaction mixture was stirred with a magnetic stirrer and heated to the specific temperature for the suitable time. The different parameters which affect the radiochemical yield of 125I-celecoxib such as celecoxib concentration [50–200 μg (1.3–5.2 mM (mmol/L))], reaction temperature (25–80 °C), type of oxidizing agent (CAT, NBS) and pH of the reaction mixture (4–11) in ethanol as organic reaction medium were studied.
Radiochemical yield and purity
The radiochemical yield and purity of the product were determined by TLC and HPLC.
TLC analysis
TLC technique was used to estimate the labeling yield, where a thin layer of silica gel coated on aluminum sheet (20 cm × 20 cm) was cut into strips. On TLC strip (1 cm width, 13 cm length), 5 μL sodium metabisulfite (10% NaHSO3) was firstly spotted to quench the reaction, and then 1–2 μL of the reaction mixture was placed 2 cm above the edge and allowed to evaporate spontaneously. For development a fresh mixture of methylene chloride:ethyl acetate (2:1 v/v) was used. Radioiodide 125I remained near the origin (Rf = 0–0.1), while the iodo-compound (125I-celecoxib) moved with the solvent front (Rf = 0.8–1). The percentage radiochemical yield of the 125I-celecoxib was estimated as the ratio of the radioactivity of 125I-celecoxib to the total activity, multiplied by 100. The radiochemical yield of 125I-celecoxib is the mean value of two experiments.
HPLC analysis
The mobile phase used in chromatographic separations consists of a binary mixture of solvents acetonitrile (A), and water in 0.1% acetic acid, pH 3.16 (B), at a flow rate of 1 mL/min at wavelength 254 nm. 10 μL of the reaction mixture was injected into the reversed phase nucleosil phenyl column (250 mm × 4.5 mm, 5 μm). The separation was carried out by the gradient elution mode, where the radioiodide was firstly eluted by using 15:85 (A:B, v/v) for 7 min, where its retention time was 3.9 min, then the 125I-celecoxib was eluted by using the 90:10 (A:B, v/v) for 25 min, where its retention time was 23 min as shown in Fig. 5.
Tumor transplantation in mice
The parent tumor line (Ehrlich Ascites Carcinoma) was withdrawn from 7 days old downer female Swiss albino mice and diluted with sterile physiological saline solution to give 12.5 × 106 cells/mL. 0.2 mL solution was then injected in mice intraperitoneally to produce ascites, or intramuscularly in the right thigh to produce solid tumor. The animals were maintained till the tumor development was apparent during 15 days [15].
Results and discussion
Celecoxib concentration
The labeling efficiency was affected by changing the celecoxib concentration from 50 to 200 μg (from 1.3 to 5.2 mM) (Fig. 1). In each case of a celecoxib concentration, the labeling yield increased by increasing the reaction time up to 30 min the results indicate that the radiochemical yield of 125I-celecoxib reached the maximum value (65%) by using 150 μg (3.9 mM) celecoxib and 1.6 mM CAT as oxidizing agent at 60 °C within 30 min. The radiochemical yield is not affected by the amount of celecoxib higher than 150 μg (3.9 mM). This may be attributed to the fact that 150 μg (3.9 mM) of celecoxib is enough to capture the entire generated iodonium ions as a result of the oxidation of the radioactive iodide (125I−) at 1.6 mM CAT [16].
Effect of temperature
The variation of the radiochemical yield of 125I-celecoxib as a function of reaction time at different reaction temperatures (25–80 °C) in the presence of 1.6 mM CAT was studied. The results are shown in Fig. 2. The reaction temperature is a vital factor which affects the radiochemical yield of 125I-celecoxib. The labeling efficiency increased by raising the temperature up to 60 °C, where the radiochemical yield of 125I-celecoxib reached the equilibrium 35, 50 and 65% within 30 min at 25, 40 and 60 °C, respectively. At 80 °C, the labeling yield reached 48% after 5 min reaction time, but more than 5 min, it decreased to about 15% within 30 min. This may be attributed to the thermal decomposition of the labeled compound or degradation of the oxidizing agent [17].
Effect of pH
The influence of acidity of the reaction medium on the labeling yield is shown in Fig. 3. The labeling yield increased about 10–13% in pH 4 in comparison with pH 7 after 10 min of the reaction time, but further increase of pH towards the alkaline medium (pH 11) leads to decreasing the radiochemical yield of 125I-celecoxib to 30%. This effect has been observed earlier in studies concerning the radiohalogenation using CAT as an oxidiant [18–20]. Our results agree with that of Petzold and Coenen [20]. The effect can be explained by the generation of ClO− in high concentration of hydroxyl ions that will continue to oxidize iodide to hypoiodite, which is not able to participate in electrophilic substitution reactions. The labeling yield reached the maximum values 65, 52 and 30 at pH 4, 7 and 11 within 15 min.
Effect of oxidizing agents
The influence of CAT (0.8–2.4 mM) and NBS (0.8–3 mM) on the labeling efficiency of celecoxib is shown in Fig. 4. Radioiodination of organic molecules has been performed by using a mild oxidizing agent such as CAT, which decomposes to hypochlorite anion that acts as an oxidizing agent, transforming iodine from I− to oxidative state I+. The influence of CAT concentration on the radiochemical yield of 125I-celecoxib was firstly studied at pH 4 and 60 °C for 15 min to show that the labeling yield increased from 55 to 65% by increasing the concentration of CAT from 0.8 to 1.6 mM. Increasing the CAT concentration above 1.6 mM leads to a decrease in the radiochemical yield of 125I-celecoxib due to the formation of undesirable oxidative side reactions like chlorination [20, 21], polymerization and denaturation of substrate [22]. While, NBS is a source of free-radical or positive bromine, used primarily in the bromination of organic substrates, a major use is in the bromination of allylic or benzylic positions in the substrate. Other potential uses are bromination of activated benzene rings, cleavage of benzyl ethers and esters, conversion of alcohols to alkyl bromides, and oxidation of certain reactive substrates. The results indicate that the labeling efficiency increased gradually from 15 to 35% by increasing the concentration of NBS from 0.8 to 3 mM. The results clarifies that CAT is a more effective oxidant than NBS. The low radiochemical yield of 125I-celecoxib in case of NBS may be attributed to the bromination of celecoxib.
Purification of 125I-celecoxib
125I-celecoxib was separated by means of HPLC as shown in Fig. 5. 125I-celecoxib was completely separated from celecoxib, where the retention times are 23 and 19.5 min, respectively, while the radioiodide was separated at retention time about 4 min. The fractions were collected and evaporated under reduced pressure, dissolved in saline solution and sterilized by Millipore filter (0.22 μm) under aseptic conditions [23] to be ready for injection.
In vitro stability of 125I-celecoxib
The stability of 125I-celecoxib was studied in order to determine the suitable time for injection to avoid the formation of the undesired products which result from the decomposition of the labeled compound. These undesired radioactive products may be accumulated in non- target organs. Table 1 shows the stability of 125I-celecoxib. The results indicate that 125I-Celecoxib is stable up to 24 h at room temperature.
Biodistribution of 125I-celecoxib in ascites bearing mice
The experiment was carried out by injecting 3.7 MBq of 125I-celecoxib into the tail vein of the infected albino mice. At each time point (0.5, 1 and 24 h), three mice were sacrificed to calculate standard deviation as shown in Table 2. The results clarify that the uptake of 125I-celecoxib after 0.5 h post injection in the kidneys, blood stomach and liver is shown in Table 2. By increasing the time post injection from 1 to 24 h, the 125I-celecoxib uptake in ascitic fluid increased significantly from 32.6 to 55.2% of the total activity, while its uptake in other organs (kidneys, blood stomach and liver) decreased gradually. The results of bio-distribution study of 125I-celecoxib in ascites bearing mice revealed that ascites is the highest site of uptake of 125I-celecoxib within 1 h post injection which suggests the use of 123I-celecoxib as a tumor imaging agent. The high uptake of 125I-celecoxib in kidney may reflect its excretion as a drug via urine. Also, the lower radioactivity in thyroid compared with the other organs indicates that the 125I-celecoxib is free from radioiodide which is easily captured in the thyroid.
Conclusion
The preparation of 125I-celecoxib was carried out by electrophilic substitution reaction via iodine-125—hydrogen exchange in the presence of CAT (1.6 mM) as oxidizing agent at 60 °C within 15 min to obtain the labeling yield about 65%. The radioiodinated celecoxib was purified by using HPLC for biodistribution study in the infected mice, which clarifies its importance as a tumor imaging in case of using iodine-123, while it may be used as tumor radiotherapy in case of using iodine-125. Where, the biodistribution confirms the importance of 123I-celecoxib as a tumor imaging agent from 1 to 24 h post-injection, while, this study represent a preliminary study for 125I-celecoxib as a tumor therapy, so a more biological study would be needed to ensure the efficiency of the 125I-celecoxib for this purpose.
References
Lane NE (1997) J Rheumatol 24(Suppl 49):20
Mandell BF (1999) Clevel Clin J Med 65:285
Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, Makuch R, Eisen G, Agrawal NM, Stenson WF, Burr AM, Zhao WW, Kent JD, Lefkowith JB, Verburg KM, Geis GS (2000) J Am Med Assoc 284:1247
Goldstein JL, Correa P, Zhao WW, Burr AM, Hubbard RC, Verburg KM, Geis GS (2001) Am J Gastroenterol 96:1019
Geis GS (1999) J Rheumatol 26:31
Koki AT, Masferrer JL (2002) Cancer Control 9:28
Grösch S, Maier TJ, Schiffmann S, Geisslinger G (2006) J Natl Cancer Inst 98:736
Hsu AL, Ching TT, Wang DS, Song X, Rangnekar VM, Chen CS (2000) J Biol Chem 275:11397
Kucab JE, Lee C, Chen CS, Zhu J, Gilks CB, Cheang M et al (2005) Breast Cancer Res 7:R796
Patel MI, Subbaramaiah K, Du B, Chang M, Yang P, Newman RA et al (2005) Clin Cancer Res 11:1999
Zhu J, Song X, Lin HP, Young DC, Yan S, Marquez VE et al (2002) J Natl Cancer Inst 94:1745
Kuge Y, Katada Y, Shimonaka S, Temma T, Kimura H, Kiyono Y, Yokota C, Minematsu K, Seki K, Tamaki N, Ohkura K, Saji H (2006) Nucl Med Biol 33:21
Charlton DE, Booz J (1981) Radiat Res 87:10
Unak P (2002) Braz Arch Biol Technol 45:97
Abu-Zeid M, Hori H, Nagasawa H, Uto Y, Inayama S (2000) Biol Pharm Bull 2:195
El-Azony KM, El-Mohty AA, Killa HM, Seddik U, Khater SI (2009) J Label Compd Radiopharm 52:1
El-Azony KM (2004) Arab J Nucl Sci Appl 37:81
Tolmachev V, Bruskin A, Sivaev I, Lundqvist H, Sjöberg S (2002) Radiochem Acta 90:229
Orlova A, Tolmachev V, Lundqvist H (2000) Eur J Nucl Med 27:1210
Petzold G, Coenen HH (1981) J Label Compd Radiopharm 18:139
Knust EJ, Dutschka K, Machulla HJ (1990) J Radioanal Nucl Chem Lett 144:107
Saccavini JC, Bruneau C (1984) IAEA CN 4519:153
Verbruggen RF (1986) Int J Appl Radiat Isot 37:1249
Acknowledgments
The author wishes to thank the editor and the referees of the JRANC for their cooperation, valuable comments, and revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Azony, K.M. Preparation of 125I-celecoxib with high purity as a possible tumor agent. J Radioanal Nucl Chem 285, 315–320 (2010). https://doi.org/10.1007/s10967-010-0583-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-010-0583-8