Abstract
Childhood and adolescent adversity have been shown to predict later mental and physical health outcomes. Understanding which aspects and developmental timings of adversity are important, and the mechanisms by which they have their impact may help guide intervention approaches. A large subset of adolescents (N = 457; Female 68.9 %) from the 10-year longitudinal Youth Emotion Project was examined to better understand the associations among childhood/adolescent adversity, substance use disorder, and later health quality. Adolescent (but not childhood) adversities were associated with poorer health in late adolescence/early adulthood, adolescent adversities were associated with subsequent onset of substance use disorder, and adolescent adversities continued to be associated with poorer health in late adolescence/early adulthood after accounting for the variance explained by substance use disorder onset. These associations were observed after statistically accounting for emotional disorders and socioeconomic status. Specific domains of adversity uniquely predicted substance use disorder and poorer health outcomes. In contrast with current recent research, our findings suggest the association between childhood/adolescent adversity and poorer health outcomes in late adolescence and emerging adulthood are not entirely accounted for by substance use disorder, suggesting efforts to curtail family-based adolescent adversity may have downstream health benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prior research suggests that childhood and adolescence are sensitive windows for the development of health behaviors that contribute to later health quality, and that childhood and adolescent adversities disrupt this developmental trajectory leading to poorer health in adulthood. Recent work further suggests that the development of substance use disorders may account for this. However, due to the challenges of assessing early adversity, this body of research has methodological limitations, which may hamper interpretation and cloud implications for interventions. That is, interventions might focus on bolstering family environments to reduce family-based adversity and health promotion in at-risk groups, or on curtailing adolescent substance use, or both. Thus, the current study used a longitudinal design to examine: (a) whether adversity in childhood and adolescence predicts a later measure of health quality, (b) whether adversity also predicts onsets of substance use disorders, and (c) whether adversity predicts later health quality over and above substance use disorder onsets.
Evidence that Childhood and Adolescent Adversity Influences Later Health
The harmful effects of childhood and adolescent adversity on a number of physical and emotional health-related outcomes are well-established (Putnam 2006; see Brady and Back 2012, for a review). Childhood and adolescent adversity includes difficult, stressful, or traumatic life experiences (e.g., physical, sexual, or emotional abuse) of varying frequency, severity, and duration. Such experiences appear to be associated with later poorer physical health (e.g., Flaherty et al. 2006; Goodwin and Stein 2004; Springer et al. 2007; Walker et al. 1999; Wegman and Stetler 2009), including chronic medical conditions and several leading causes of death (Felitti et al. 1998; Raposa et al. 2014). Similarly, recent longitudinal work has demonstrated associations specifically between adolescent interpersonal adversity and subsequent poorer general health (Adam et al. 2011). As we note below, despite the important advances made by these investigations, some methodological drawbacks (e.g., cross-sectional analyses, limited methods for assessing early adverse experiences) are present in the current literature due to the challenges of assessing early adversity and longitudinal outcomes.
A larger body of evidence, however, documents the association between early life adversity and later emotional health outcomes such as post-traumatic stress disorder and depression (Cougle et al. 2010; Vrshek-Schallhorn et al. 2014). But in addition, more recently, childhood adversity has also been linked to an elevated prevalence of substance use problems and substance use disorders (Anda et al. 2006; Enoch 2011; Grella et al. 2005). Of note, some studies found no significant associations between traumatic childhood and adolescent experiences and alcohol use in early adulthood (e.g., Marx and Sloan 2003) or found associations only for some subgroups (e.g., women; Myers et al. 2014).
Might Substance Use Account for the Adversity-Health Association?
Furthermore, Brady and Back (2012) suggest that the association between childhood and adolescent adversity and poor physical health outcomes may be explained by substance use disorder (see Brady and Back 2012, for discussion). Substance use disorder is associated with poor health consequences (see Schulte and Hser 2014, for review) and some studies have identified substance use as a mediator of the association between childhood adversity and a variety of physical health conditions (Chartier et al. 2007; Dong et al. 2003; Dong et al. 2004). However, these studies are limited by some of the same methodological concerns described below (e.g., cross-sectional analyses, limited methods for assessing early adverse experiences). Thus, we aimed to examine these relationships using methods that overcome many of the earlier limitations. Critically, if health outcomes are explained by substance use disorder, then substance use disorder prevention programs may also benefit future physical health outcomes. On the other hand, if childhood or adolescent adversity independently predict poor physical health outcomes after accounting for substance use disorder, then additional prevention efforts focused on reducing family-based adversity and on health promotion among those at-risk would be indicated (e.g., nutrition, exercise, and linkage to health care).
Importance of Examining Late Adolescent and Emerging Adult Trajectories
Adolescence is a key developmental period for the development of substance use disorders (Hasin et al. 2007), and substance use problems that start in adolescence have a higher likelihood of persisting well into adulthood (McGee et al. 2000). Moreover, there are hints that childhood and adolescence are sensitive windows for the development of adult health-related habits. For example, weeknight television viewing at age 5 and 15 was associated with higher cholesterol, smoking, and body mass index, and with lower frequency of exercising in 26 year olds followed longitudinally (Hancox et al. 2004). Similarly, physical fitness level assessed in the mid-teen years predicted a cardiovascular health risk profile at age 32 (Twisk et al. 2002). Thus, the current study focused on a developmentally sensitive time period for emotional health, but likely also for physical health and health-behaviors.
Limitations of Prior Research
The present research attempts to addresses several methodological limitations of prior research. First, the majority of the studies that examine the associations between childhood and adolescent adversity and substance use disorder or health outcomes are limited by cross-sectional designs. Most studies either lack dating of onset of substance use disorder or health outcomes to ensure temporal precedence of the adverse events or include periods in which the adverse events and outcomes of interest overlap temporally (e.g., Cross et al. 2015; Goodwin and Stein 2004; Grella et al. 2005; Khoury et al. 2010; Springer et al. 2007; Triffleman et al. 1995). Prospective studies are needed to strengthen our understanding of the risks conferred by childhood and adolescent adversity. This is particularly important in the case of substance use disorder given its high prevalence in adolescence (Hasin et al. 2007; Johnston et al. 2015). By contrast, the present report provides sequential and dated measures of adversity, onsets of substance use disorders, and reports of health quality.
Second, although there are a number of studies that have significantly advanced the field in understanding the impact of child and adolescent adversity on a number of adult health outcomes, a majority of studies use early adversity assessment approaches with at least five limitations: (1) First, almost all studies depended upon recollection in middle adulthood (e.g., in participants’ 30s through 50s) of early adversities that occurred several decades earlier (see Hardt and Rutter 2004 for a review of retrospective reporting of childhood abuse). Such lengthy periods of recollection raise concerns about reliability. The present report instead used a more proximal interview measure of adversity collected when participants were between approximately 20–22 years old and covering adversity experienced between birth and age 16; (2) Second, almost all studies (with the exception of Grella et al. 2005) collapsed childhood and adolescent experiences together, despite the differential impact that adversities in these separate developmental periods may have on health-related outcomes (Goodwin and Stein 2004; Springer et al. 2007), both from environmental and neurobiological perspectives (Fox et al. 2010); (3) Third, many studies employ questionnaires rather than interviews to measure childhood adversity, with only a few exceptions in which interviews were used (Benjet et al. 2013; Khoury et al. 2010). However, there is evidence that interviews have greater validity than questionnaires (e.g., Dohrenwend 2006) and are less vulnerable to false negatives (e.g., Felitti et al. 1998); (4) Fourth, with some exceptions (Eames et al. 2014; Khoury et al. 2010; Norman et al. 2012; Triffleman et al. 1995), most studies assess only limited early adversity domains, typically measuring only sexual abuse or physical abuse, leaving other types of adversity unassessed and unaccounted for in analyses. Consistent with several other investigators (Fink et al. 1995), we conceptualize childhood and adolescent adversities more broadly, consisting of a range of difficult experiences including separation from or loss of caregivers, neglect, emotional abuse, physical abuse, and sexual abuse. Finally, (5) Finally, most studies do not attempt to account for the unique effects of different kinds of adversity by examining multiple domains simultaneously in statistical models (e.g., Batten et al. 2004).
The Present Study
To inform developmentally-minded interventions and address the above limitations, we followed a sample of adolescents into young adulthood to better understand the relationship between childhood and adolescent adversities and physical health outcomes, and in particular to determine whether substance use disorders might account for an association between adversities and poor health. The current study overcomes many of the limitations of previous work, utilizing data from the Youth Emotion Project (YEP), a 10-year longitudinal study examining common and specific risk factors for anxiety and depression. Pertinent to the current study, the participants were assessed for substance use disorders and physical health (amongst other variables; see Zinbarg et al. 2010) at baseline and then followed annually over 7–9 years, depending on cohort. Participants also completed an interview measure assessing a broad spectrum of childhood and early to mid-adolescent adversities. The primary goals of the current study were to examine whether (a) adversities in childhood and early to mid-adolescence confer risk for poor physical health (b) adversities in childhood and early to mid-adolescence confer risk for substance use disorder; and (c) the associations between childhood and early to mid-adolescent adversities and poor health are explained by the presence of substance use disorder, or adversities predict health outcomes above and beyond the variance explained by substance use disorder onset. We focused on these putative outcomes of early life adversity because they are relatively understudied compared to anxiety and depression, which have already demonstrated associations with early life adversity, including in our own work (Vrshek-Schallhorn et al. 2014), and because of the suggested link between substance use disorders and later health (e.g., Brady and Back 2012). We hypothesized that childhood and adolescent adversities would (a) be associated with poor physical health outcomes in late adolescence and early adulthood, and (b) predict onset of substance use disorder. Given the limited work in understanding the extent to which substance use disorder accounts for the association between child and adolescent adversities and later physical health, we made no hypothesis regarding the final goal of the study.
Methods
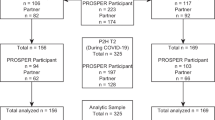
Participants
Participants enrolled in a larger two-site, 10-year longitudinal study (total N = 627) who completed an early life adversity interview (n = 457; M age = 16.57, SD = 0.37, age range = 15.68–18.28) were eligible for inclusion in the primary analyses. The larger study examined factors for psychopathology in late adolescence and early adulthood (YEP) in three consecutive cohorts of high school juniors from two demographically diverse public high schools in suburban Chicago and suburban Los Angeles. To increase the incidence of psychopathology onset during the longitudinal phase, at-risk students exhibiting high levels of neuroticism (i.e., top third) as measured by the Neuroticism subscale of the revised 23-item Eysenck Personality Questionnaire Neuroticism Scale (Eysenck and Eysenck 1975) were oversampled (Clark et al. 1994; Hayward et al. 2000). Thus, the sampling procedure was not intended to produce a nationally representative sample of adolescents, but a normal sample of adolescents in the general population, with oversampling of those high in neuroticism, to observe greater numbers of new onsets of emotion disorders, which has benefits for statistical modeling in a simulation study. See Zinbarg et al. (2010) for details regarding sampling procedures. Participants with substance use disorders at baseline were excluded from analyses. Of the participants eligible for inclusion in the primary analyses reported in the current study who completed a baseline assessment and an early life adversity interview (n = 457), 400 (87.5 %) completed the first follow-up diagnostic assessment and Life Stress Interview (LSI), 358 (78.3 %) completed the second, 379 (82.9 %) completed the third, 388 (84.9 %) completed the fourth, 402 (88.0 %) completed the fifth, 403 (88.2 %) completed the sixth, 358 (78.3 %) completed the seventh, 262 (57.3 %) completed the eighth, and 136 (29.8 %) completed the ninth. Eligibility should be noted when examining percentage of assessment completers at the two later timepoints. Specifically, the first cohort of participants was eligible to complete all ten assessments (baseline plus nine follow-up), the second cohort was eligible to complete up to nine assessments (baseline plus eight follow-up), and the third cohort completed up to eight assessments (baseline plus seven follow-up). The sample included in the current analysis was 49.0 % Caucasian, 14.2 % Hispanic, 13.6 % African-American, 4.4 % Asian, 0.7 % Native American/Pacific Islander/Alaskan Native, 12.9 % multiracial, 5.3 % who identified with another unlisted racial/ethnic group, and predominantly female (68.9 %).
Measures
Substance Use Disorder Assessment
The Structured Clinical Interview for the Diagnostic and Statistical Manual—IV (DSM-IV), non-patient edition (SCID-I/NP; First et al. 1995) was administered to assess for DSM-IV disorders. A lifetime SCID version was given to participants at baseline to assess for the presence of current and previous psychopathology. Following baseline, participants were administered the SCID on an annual basis to evaluate diagnostic symptomatology since the prior interview (see Zinbarg et al. 2010, for details). During each interview, screening questions were used to identify which diagnostic sections required further inquiry and administration. After screening, interviewers administered endorsed diagnostic sections and rated the clinical severity of each current diagnosis using the 0–8 Clinical Severity Rating Scale (Di Nardo and Barlow 1988). Using this scale, a score of 4 or higher is indicative of symptoms that were clinically severe, distressing or impairing within the past month. When the diagnostic criteria were met for a disorder during the follow-up period but not within the past month at the time of the interview, we coded these as “past diagnoses” that were considered either clinically significant (coded as 4), a “possible case” (coded as 3), or “no case” (coded as 0). Thus, all participants received a Clinical Severity Rating from 0–8 for all possible substance use disorder diagnoses across time points. Inter-rater reliability for the SCID diagnoses was κ = .82 across time-points and raters across sites. Individuals meeting the DSM-IV-TR criteria for any substance use disorder (including alcohol and all non-alcohol substances of dependence) with a Clinical Severity Rating rating of 4 or higher were considered to have met substance use disorder criteria. Because the baseline assessment was a lifetime interview, those meeting diagnostic criteria at baseline for a substance use disorder (n = 9; 2 % of the sample) were excluded from analyses as a conservative measure to ensure that onsets did not occur prior to any of the child or adolescent adversities assessed (see below). For our secondary dimensional analyses of substance use severity, we used the highest Clinical Severity Rating obtained at any time point across the study, with the exception of baseline, in which those with a clinically significant substance use disorders were excluded for the reasons described above.
Childhood and Adolescent Adversity
The semi-structured Childhood Trauma Interview (CTI; Fink et al. 1995) was administered for the retrospective assessment of childhood and early to mid-adolescent adversity. Individuals conducting interviews were trained extensively on administration and scoring protocol. Participants (who completed the CTI at ages 20–23) were queried regarding six domains of adversity from birth to the age of 16; (1) separation from or loss of caregiver, (2) neglect by caregiver, (3) emotional abuse, (4) physical abuse, (5) witnessing violence, and (6) sexual abuse and assault. Severity ratings were assigned to each adversity by the interviewer using a scale ranging from 1 (minimal to mild) to 6 (very extreme, sadistic) (see Vrshek-Schallhorn et al. 2014, for details). Adversities occurring from 0–9 years of age were considered childhood adversities, while adversities occurring from 9–16 were separately considered as pre to mid-adolescent (which we refer to as adolescent hereafter) adversities. If a particular adversity spanned both childhood and adolescence, it was counted in both developmental periods. Because participants could endorse multiple adverse experiences in each domain, we calculated summary scores of adversity within each domain. Severity scores for all adversities within the same domain were added together to compute an overall sum of severity scores for each domain. Our primary dependent variables were the separate sums of severity scores that were calculated for adversities experienced during childhood and adolescence. In addition to domain-specific summary scores, we calculated cross-domain summary scores, to provide a global index of early adversity burden and for use in omnibus statistical testing to reduce family-wise error ahead of follow-up testing using the individual domains. Sums of severity scores across all domains were calculated for childhood adversities and adolescence separately. We previously showed that this scoring approach predicts first onsets of anxiety disorders and major depression (see Vrshek-Schallhorn et al. 2014, for details).
Physical health
Annual evaluation of physical health was assessed via the UCLA Life Stress Interview (Hammen et al. 1987; Hammen et al. 1985), a semi-structured interview of ongoing, objective stress in various life domains (LSI; see Vrshek-Schallhorn et al. 2015 for details). All LSI administrations assessed physical health in the past year (baseline and all follow-up assessments). As with all domains of the LSI, physical health was rated by trained interviewers on objective circumstances, represented on a behaviorally anchored scale ranging from 1 to 5, using half-point increments (exceptionally good health to severe or life threatening disease or condition). Raters were trained to consider scores of 1 and 5 to be rare and relatively extreme cases. The health domain includes illness (acute or chronic), medical care and utilization, injury, exercise, nutrition, weight, smoking behavior, and (briefly) drinking behavior. Raters consider the severity of health problems alongside objective indices of impairment and negative life impact (e.g., time spent in medical care, social, occupational, and financial impact of medical conditions). The mean within-site intraclass correlation across all time points was .72. The mean cross-site intraclass correlation across all time points was .61. If changes in physical health occurred during the interview interval, each distinct period was rated separately then prorated for duration for final summary score calculation. An average physical health score (across all time points including baseline, none of which overlapped with time periods assessed in the CTI) was generated by calculating the mean physical health score of completed interview time-points across all available follow-up assessments for each participant. Physical health assessed via the LSI has previously demonstrated concurrent validity in a large sample of adolescents with a validated self-reported measure of overall perception of personal health (Short Form Health Survey, General Health Perceptions Subscale (SF-36); Ware and Sherbourne 1992), where measures were found to significantly correlate with one another, r = .41, p < .05 (Keenan-Miller et al. 2007).
Covariates
The following variables are associated with early life adversity, substance use disorders, and health outcomes, and were thus included as covariates in order to statistically account for the variance explained by these correlates of substance use disorder and health in the models.
Socioeconomic Status (SES)
SES was entered as a covariate in the primary analyses. SES was measured at baseline using Hollingshead’s Index (Hollingshead 1975).
Emotional Disorders
DSM-IV-TR anxiety and unipolar mood disorder diagnoses (herein referred to as emotional disorders) were assigned from the SCID in the same way as substance use disorder diagnoses (described above). Given that anxiety and unipolar mood disorders frequently co-occur with substance use disorder and have been found to negatively impact physical health, the presence of such disorders at any time during the study was entered as a covariate (Grant et al. 2004; Kiecolt-Glaser and Glaser 2002; Shen et al. 2011). This ensured that any variance in the dependent variables explained by emotional disorders was accounted for in the statistical models. Anxiety disorders included panic disorder with or without agoraphobia, agoraphobia without panic, social anxiety disorder, specific phobia, generalized anxiety disorder, posttraumatic stress disorder, and obsessive compulsive disorder. Unipolar mood disorders included major depressive episode, dysthymia, depressive disorder not otherwise specified, and adjustment disorder with depressed mood.
Procedures
Participants completed SCID, CTI, and LSI interviews over the phone or in-person. After baseline, participants were assessed annually for seven to nine additional years, depending on enrollment cohort. Participants completed the SCID and LSI at each annual assessment. They completed the CTI once, mid-way through the study (around years 6–7 of the 10-year study). Enrolled participants were contacted annually regardless of previous interview completion status. Participants completing at least the baseline SCID, LSI, and CTI assessments were considered for analysis (N = 457). Participants with a baseline substance use disorder (n = 9) were excluded from analyses, resulting in N = 448. An additional nine participants were missing SES data, resulting in a final sample size of N = 439. Importantly, although the CTI was administered retrospectively (albeit shortly after mid-adolescence), the period of time assessed in the CTI occurred prior to the baseline SCID and LSI assessments. Thus, none of the adversities assessed in the CTI overlapped with any of the health or symptom measures. As described above, we conservatively eliminated those with substance use disorder at the baseline SCID interview in order to further ensure no overlap.
Results
The primary analyses were conducted using a series of linear regressions in SPSS 22.0. Parallel sets of models were analyzed with each dependent variable, substance use disorder onset and health score. In the first block of each analysis, we entered our covariates. In the second block, we included the sum of CTI severity scores across domains during childhood and the sum of CTI severity scores across domains during adolescence. When the overall childhood or adolescent sum of severity scores variable significantly predicted the dependent variable of interest, we conducted follow-up tests that included the sum of severity scores for each of the six domains of adversity for that developmental period in one model to examine whether specific types of adversity uniquely contributed to the model. We used this approach of conducting follow-up tests only when the omnibus test was significant in order to control for inflated type I error that may have otherwise accrued with multiple tests examining the specific domains of adversity, as well as to preserve power by only including the several variables tapping into the different domains of adversity into models when an omnibus test indicated these follow-up tests may be warranted.
Next, we examined whether childhood and adolescent adversity predicted poor health above and beyond the effects of substance use disorder by including substance use disorder onset as a covariate alongside the other covariates in predicting poor health. For this set of analyses, in order to account for the potential overlap in the substance use disorder onset variable and the LSI health variable, in which one of many items that factors into the score is drinking frequency, we created an of adversity in lieu of the categorical diagnostic substance use disorder variable to assess whether similar patterns of findings emerged when we utilized a ross timepoints. Average drinking frequency was operationalized as the average number of drinks per month. This variable was additionally included in the models as a covariate to account for the potential small overlap between the substance use disorder predictor variable and the LSI health dependent variable. Finally, we conducted a secondary analysis using the highest substance use disorder Clinical Severity Rating from the first follow-up period through the end of the study in lieu of the categorical diagnostic substance use disorder variable to assess whether similar patterns of findings emerged when we utilized a dimensional measure of substance use severity. All covariates, including the “average drinking frequency” variable, were included in these secondary analyses.
Sample Descriptive Statistics on Predictor and Outcome Measures
Table 1 presents descriptive data for the childhood and adolescent adversity variables. Table 2 reports the zero-order correlations among variables included in the models. The mean score on the LSI health module across all assessment periods across participants who completed the CTI (N = 457) was 2.15 (SD = 0.27) on the 1 (“exceptionally good health”) to 5 (“severe or life threatening disease or condition”) interviewer-rated scale, indicating generally good health, which is expected for the sample’s developmental stage. Specifically, a score of a 2 indicates “typical problems but overall healthy.” Within the sample, 36.8 % of individuals had a mean health score ≤ 2 across all LSI assessments, and 62.3 % of the sample had a mean health score between 2 and 3 across all assessments. Only 0.8 % of the sample had a mean health score > 3.2. Two percent of the sample included in these analyses (i.e., those who completed the CTI) met the diagnostic criteria for substance use disorder at baseline (n = 9) and were thus excluded from analyses predicting substance use disorder onset. 17.3 % of the sample (n = 79) went on to develop substance use disorders over the 7–9 year follow-up period.
Childhood and Adolescent Adversity as Predictors of Poor Health
In the first model, after covarying for SES and the presence of any emotional disorder in the first block, the sum of the severity scores of childhood adversities (across all domains of adversity) did not significantly predict subsequent health scores (p = .94) when also accounting for the variance explained by the sum of severity scores of adolescent adversities, which did significantly predict subsequent health scores in the model, β = 0.24, t (437) = 3.82, p < .001, such that greater severity of adolescent adversity was associated with poorer health scores. In order to further explore this significant association, a linear regression including the sum of severity scores for each domain of adolescent adversity as predictors was conducted (also covarying for SES and emotional disorders in the first block of the regression) (see Table 3). When including each domain of adolescent adversity in the model, the sum of severity ratings for sexual abuse [β = 0.21, t (437) = 4.23, p < .001], separation/loss [β = 0.13, t (437) = 2.71, p < .01], and neglect [β = 0.11, t (437) = 2.35, p < .05] each uniquely contributed to the model (see Table 3). None of the other domains of adolescent adversity significantly contributed to the model predicting health scores (all ps > .30).
Child and Adolescent Adversities as Predictors of Substance Use Disorders
A set of logistic regression models were conducted with a clinically significant substance use disorder as the dependent variable. When both childhood and adolescent adversities were entered as predictors in the model, and after covarying for SES and emotional disorders, the overall sum of severity scores for childhood adversities did not predict subsequent onset of substance use disorders (p > .53). In contrast, the overall sum of severity scores for adolescent adversities significantly predicted substance use disorders across the follow-up period, OR = 1.02, 95 % CIs = 1.00–1.05, p = .05. A follow-up test examining the unique contributions of each type of adolescent adversity together in a logistic regression model (shown in Table 4) indicated that the sum of severity scores in the emotional abuse domain uniquely contributed to the model in predicting substance use disorder onset, OR = 1.09, 95 % CIs = 1.01–1.17, p < .05. None of the other domains of adversity predicted substance use disorder onset (all ps > .49).
Our secondary analyses using the dimensional substance use severity score as the dependent variable in lieu of the categorical, diagnostic substance use disorder variable, yielded a virtually identical set of findings: Adolescent [β = 0.20, t (445) = 3.20, p = .001], but not childhood (p = .68) adversity significantly predicted greater substance use severity. The follow-up test including all domains of adolescent adversity in one model indicated that only emotional abuse significantly and uniquely contributed to the model, β = 0.15, t (445) = 2.19, p = .01, with all other ps > .06.
Childhood and Adolescent Adversities as Predictors of Poorer Health after Accounting for the Variance Explained by Substance Use Disorder Onset
To understand whether the association between childhood and adolescent adversities and poorer health outcomes were explained by substance use disorder, we conducted a linear regression predicting poorer health with the covariates in the first block, substance use disorder onset and the drinking frequency covariate extracted from the LSI in the second block and childhood and adversity variables in the third block. The final model was statistically significant, Adjusted R 2 = .12, R2Δ = .05, F (2, 430) = 11.37, p < .001. substance use disorder onset, β = 0.12, t (437) = 2.38, p < .05, anxiety disorders, β = 0.10, t (437) = 2.05, p < .05, and unipolar mood disorders, β = 0.11, t (437) = 2.32, p < .05, were significantly associated with poor health. Childhood adversity was not a significant predictor of poor health (p = .78) but adolescent adversity remained a significant predictor of poor health, β = 0.21, t (437) = 3.47, p = .001 above and beyond the variance accounted for by substance use disorder onset, drinking frequency, childhood adversity, SES, and emotional disorders. A model examining each of the six domains of adolescent adversity as separate predictors in the model (see Table 5) indicated that sexual abuse [β = 0.21, t (437) = 4.38, p < .001], separation/loss [β = 0.13, t (437) = 2.75, p < .01], and neglect [β = 0.11, t (437) = 2.23, p < .05] each continued to uniquely contribute to the model in predicting poor health after accounting for the significant variance accounted for by substance use disorder onset and the other covariates. None of the other types of adolescent adversity significantly contributed to the model (all ps > .48). The secondary analyses using the dimensional substance use severity score yielded an identical pattern of findings and significance.
Discussion
The primary aim of the current study was to better understand the predictive associations between child and adolescent adversities and two health-related consequences in late adolescence and early adulthood: substance use disorder and health outcomes. Identifying these consequences of early life adversity at a developmentally sensitive time for the onset of substance use problems and solidification of health behaviors advances the field’s understanding of these risk factors for health outcomes. Importantly, we also examined whether associations between child and adolescent adversity and poorer health outcomes were accounted for by the onset of substance use disorders during late adolescence and early adulthood. These findings have the potential to preliminarily identify key mechanisms or pathways to poorer health that can inform prevention interventions.
In this investigation of adolescents followed into early adulthood, adolescent (but not childhood) adversities were significantly associated with poorer health in late adolescence/early adulthood and onset of substance use disorder. Moreover, adolescent adversities were associated with health outcomes in late adolescence/early adulthood after accounting for the variance shared with substance use disorder onset. Our models included childhood and adolescent adversities simultaneously, indicating that when accounting for the variance explained by adolescent adversities, childhood adversities (i.e., more distally occurring) were not significantly associated with substance use disorder and health outcomes in this sample. Critically, these associations with adolescent adversity and substance use disorder and health outcomes were observed after accounting for the presence of any emotional disorders at any time during the study, as well as baseline SES. In other words, these associations were not better accounted for by emotional disorders or environmental factors which are also linked to substance use disorders (Wolitzky-Taylor et al. 2012) and poor health (Härter et al. 2003; Moldin et al. 1993; Wickrama et al. 2015).
Our first aim was to examine the relationships between early life adversity and physical health outcomes. The large effects of adolescent adversities on the average rating of health over the longitudinal follow-up are consistent with prior research (e.g., Chartier et al. 2007; Felitti et al. 1998; Walker et al. 1999). Sexual abuse, separation, and neglect experiences in pre to mid adolescence also had a negative association with the physical health outcomes. In contrast to the abundance of investigations of the impact of sexual abuse (e.g., Irish et al. 2009), surprisingly little attention has been paid to the impact of neglect and separation from caregivers in adolescence. One possible explanation for the observed relationships is that early neglect and separation from caregivers leads to poor health care and poor nutrition, which lead to long-lasting health consequences (Lissau and Sorensen 1994; Norman et al. 2012). Furthermore, poor health care and nutrition in childhood may deleteriously act upon neurodevelopmental pathways [e.g., prefrontal cortex or hypothalamic–pituitary–adrenal (HPA) axis] implicated in adverse outcomes (Sheridan and McLaughlin 2014). For example, increased HPA axis reactivity and dysfunction has been found following broad childhood adversity (see Heim et al. 2008 for a review). HPA axis dysfunction has been posited to play a role in substance abuse and addiction (Koob and Le Moal 2001). Although speculative, further investigation of these putative pathways, particularly including specific domains of adversity such as neglect and separation, may elucidate these associations.
Our second aim was to examine the relationships between childhood and adolescent adversities and substance use disorder onset. As with our analyses predicting poorer health outcomes, adolescent but not childhood adversities predicted substance use disorder onset. Importantly, these findings were identical when using a dimensional index of substance use disorder symptom severity as the dependent variable. Prior findings in this limited area of research have been inconsistent (e.g., Anda et al. 2006; Marx and Sloan 2003), possibly due to differences in operationalization of substance use, type of adversities examined, and developmental periods. That is, several but not all studies have found childhood adversity to be associated with substance use outcomes (and physical health outcomes), whereas we did not observe an association between childhood adversities and these outcomes in our sample. In contrast to our study, prior reports of significant associations between childhood adversity and substance use disorders combined childhood and adolescent development periods in the measurement of “childhood adversity.” Thus, prior findings may have been driven by adolescent adversities. Our inclusion of both childhood and adolescent adversities into the same model allowed us to identify specific effects when accounting for the variance explained by adversities within each developmental period. As a consequence, this approach may elucidate the developmental period (in this case, pre-adolescence to mid-adolescence) that confers greater risk for adversities having an impact on health and substance use disorder outcomes (compared to earlier childhood adversities). Also, relatively low base rates of childhood adversities (compared to adolescent adversities) may have resulted in insufficient power to detect effects in the present study (see Wolitzky-Taylor et al. 2014 and Vrshek-Schallhorn et al. 2014, for details).
There are several benefits to separating these developmental periods, and our data may elucidate the nuances of this association that prior studies have not disentangled. Specifically, in line with prior work (Technow et al. 2015; Vrshek-Schallhorn et al. 2014), our findings support a stress continuation model suggesting more recent stressors elicit negative outcomes. That is, ongoing stress that continues to occur more proximally to the poor health outcome may be more potent than earlier periods of stress that subside. Thus, collapsing developmental periods, as done in much of the literature examining the effects of early life adversity, may mask these distinctions. Possibly, individuals who experience childhood adversity may experience intervening protective variables that occur after a childhood adversity (i.e., resilience factors), which, in the absence of stress continuation into adolescence, may prevent the development of substance use disorders (and poorer health) by late adolescence and early adulthood, a time of high risk for the onset of substance use disorders (Hasin et al. 2007). Future investigations that identify resilience factors that occur after risk factors emerge can help us develop more targeted prevention interventions that aim to replicate or augment these resilience factors.
When examining by domain of adversity, only emotional abuse uniquely predicted substance use disorder onset. Emotional abuse has been observed as a correlate of drug use in a meta-analysis (Norman et al. 2012) and uniquely predicted first onsets of anxiety disorders and major depressive disorders in a prior paper using some of the data examined in the current investigation (Vrshek-Schallhorn et al. 2014). Consequently, emotional abuse may be a robust risk factor for a variety of mental disorders. Importantly, the association between adolescent emotional abuse and later substance use disorder onset in this investigation was significant after covarying for childhood adversities, SES, and emotional disorders, suggesting that the effect of emotional abuse on substance use disorders (and symptom severity) is not better accounted for by the variance shared with emotional disorders and other correlates of emotional disorders and substance use disorders.
Our final aim was to understand whether the association between early life adversity and poor health outcomes was better accounted for by substance use disorder onset, which is associated with poor physical health (Schulte and Hser 2014). Adolescent adversities remained significantly associated with poorer health outcomes after covarying for substance use disorder onset. These data suggest that the association between early life adversity and negative health consequences is not better accounted for by the potential health consequences of having a substance use disorder. Thus, it appears that other mechanisms are likely to account for a substantial proportion of the variance that explains the association between early life adversity and poorer health in young adulthood. Future research should aim to identify these other mechanisms, which are likely to be comprised of complex pathways leading to poor health. For example, it is plausible that certain types of adversity (e.g., neglect) may lead to poor health behaviors (e.g., poor diet, low physical activity), which then may lead to physiological changes that confer risk for poor health outcomes. Alternatively, direct effects of adversity on and resulting long-term changes in biological stress pathways such as HPA axis activity could play a role (Heim et al. 2008).
Overall, our findings support the hypothesis that the associations between early life adversity and poorer health outcomes in young adulthood are not entirely accounted for by substance use disorders. This finding at first appears to contrast with cross-sectional studies that have identified risky substance use as a mediator of the association between childhood adversity and health conditions (e.g., Chartier et al. 2009). However, these prior (and limited) mediational studies found that risky substance use partially and modestly mediated the relationship between childhood adversity and health outcomes (e.g., Chartier et al. 2009), consistent with our finding that there is still significant variance in health outcomes not explained by substance use disorders. This underscores the importance of not only providing drug and alcohol prevention programs for youth who have experienced adversity, but also addressing potential health consequences through prevention programs that may include interventions for emotional stress as well as health education, nutrition and exercise components, and medical screenings for early symptoms or physiological risk factors for physical health conditions. In addition, these findings call for additional investigations to identify other factors that may account for the association between early life adversity and physical health consequences.
Despite the several methodological strengths of our study, there are some limitations worth noting. First, we lacked measures of health during the developmental period in which adversities were measured (i.e., ages 0–16). Consequently, because poor health may have preceded childhood adversities for some participants, firm causal inferences cannot be drawn from the observed relationships. Second, assessment of health included a rating of drinking frequency. Although drinking frequency is one of many factors that contribute to the overall health score (and is arguably an important health behavior to assess), it nonetheless overlaps with items in the SCID for alcohol use disorder. This may have led to inflated correlations between substance use disorder and the health outcome variable. However, our analyses accounted for this overlap by covarying for drinking frequency, data which we extracted from the LSI health domain. These findings suggest then that the inclusion of a question about drinking frequency in the LSI health domain did not appear to drive the association between substance use disorder onset and LSI health scores. Third, although participants completed the CTI relatively soon after their childhood and adolescence, it was nonetheless administered retrospectively. Thus, responses may have been biased. In particular, participants who had an onset of an emotional disorder or substance use disorder prior to administration of the CTI (i.e., in the first 5 years of the study) may be biased in their reporting of retrospective, autobiographical memories (see Griffith et al. 2012, for a review). Finally, as expected with a longitudinal study spanning ten years, there was attrition over the follow-up period. We do not know whether individuals who dropped had clinical characteristics that differed from those who completed the annual assessments. Still, this investigation is the first to our knowledge that examined these temporal pathways using a prospective design over a decade of assessment and thus advances our understanding of the ways in which early life adversity, substance use disorder, and health are longitudinally related.
Conclusions
This investigation significantly extended prior work examining the associations between child and adolescent adversities and both substance use disorders or problems and other health outcomes. Our use of interview measures and ten years of longitudinally assessing participants from late adolescence to early adulthood allowed us to improve upon prior methodologies in examining childhood and adolescent adversities as predictors of later substance use disorders (and substance use severity) and general health outcomes. In sum, we observed a pattern in which adolescent, but not childhood, adversities conferred risk for substance use disorders and poorer health. Moreover, the association between adolescent adversities and poorer health remained significant after accounting for the significant association between substance use disorder onset and poorer physical health. Particularly if future research replicates these findings, these results suggest that prevention interventions aimed at improving health-related behaviors as well as prevention interventions to reduce substance use are both warranted in this high-risk group of adolescents.
References
Adam, E. K., Chyu, L., Hoyt, L. T., Doane, L. D., Boisjoly, J., & Duncan, G. J., et al. (2011). Adverse adolescent relationship histories and young adult health: cumulative effects of loneliness, low parental support, relationship instability, intimate partner violence, and loss. Journal of Adolescent Health, 49(3), 278–286.
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., & Perry, B. D., et al. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186.
Batten, S. V., Aslan, M., Maciejewski, P. K., & Mazure, C. M. (2004). Childhood maltreatment as a risk factor for adult cardiovascular disease and depression. Journal of Clinical Psychiatry, 65(2), 249–254.
Benjet, C., Borges, G., Medina-Mora, M. E., & Méndez, E. (2013). Chronic childhood adversity and stages of substance use involvement in adolescents. Drug and Alcohol Dependence, 131(1), 85–91.
Brady, K. T., & Back, S. E. (2012). Childhood trauma, posttraumatic stress disorder, and alcohol dependence. Alcohol Research: Current Reviews, 34(4), 408–413.
Chartier, M., Walker, J., & Naimark, B. (2007). Childhood abuse, adult health, and health care utilization: results from a representative community sample. American Journal of Epidemiology, 165(9), 1031–1038.
Chartier, M., Walker, J., & Naimark, B. (2009). Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. American Journal of Public Health, 99(5), 847–854.
Clark, L. A., Watson, D., & Mineka, S. (1994). Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology, 103(1), 103.
Cougle, J. R., Timpano, K. R., Sachs-Ericsson, N., Keough, M. E., & Riccardi, C. J. (2010). Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey-Replication. Psychiatry Research, 177(1), 150–155.
Cross, D., Crow, T., Powers, A., & Bradley, B. (2015). Childhood trauma, PTSD, and problematic alcohol and substance use in low-income, African-American men and women. Child Abuse & Neglect, 44, 26–35.
Di Nardo, P., & Barlow, D. (1988). Anxiety disorders interview schedule for DSM-III-R (ADIS-R). Albany, NY: Graywind.
Dohrenwend, B. P. (2006). Inventorying stressful life events as risk factors for psychopathology: Toward resolution of the problem of intracategory variability. Psychological Bulletin, 132(3), 477.
Dong, M., Dube, S. R., Felitti, V. J., Giles, W. H., & Anda, R. F. (2003). Adverse childhood experiences and self-reported liver disease: new insights into the causal pathway. Archives of Internal Medicine, 163(16), 1949–1956.
Dong, M., Giles, W. H., Felitti, V. J., Dube, S. R., Williams, J. E., & Chapman, D. P., et al. (2004). Insights into causal pathways for ischemic heart disease adverse childhood experiences study. Circulation, 110(13), 1761–1766.
Eames, S. F., Businelle, M. S., Suris, A., Walker, R., Rao, U., & North, C. S., et al. (2014). Stress moderates the effect of childhood trauma and adversity on recent drinking in treatment-seeking alcohol-dependent men. Journal of Consulting and Clinical Psychology, 82(3), 441.
Enoch, M. A. (2011). The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology, 214(1), 17–31.
Eysenck, H. J., & Eysenck, S. B. G. (1975). Manual of the eysenck personality questionnaire (junior and adult). Kent, UK: Hodder & Stoughton.
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., & Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258.
Fink, L. A., Bernstein, D., Handelsman, L., Foote, J., & Lovejoy, M. (1995). Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. American Journal of Psychiatry, 152(9), 1329–1335. doi:10.1176/ajp.152.9.1329
First, M., Spitzer, R., Williams, J., & Gibbon, M. (1995). Structured clinical interview for DSM-IV-non-patient edition (SCID-NP, Version 1.0). Washington, DC: American Psychiatric.
Flaherty, E. G., Thompson, R., Litrownik, A. J., Theodore, A., English, D. J., & Black, M. M., et al. (2006). Effect of early childhood adversity on child health. Archives of Pediatrics & Adolescent Medicine, 160(12), 1232–1238.
Fox, S. E., Levitt, P., & Nelson III, C. A. (2010). How the timing and quality of early experiences influence the development of brain architecture. Child development, 81(1), 28–40.
Goodwin, R. D., & Stein, M. B. (2004). Association between childhood trauma and physical disorders among adults in the United States. Psychological Medicine, 34(03), 509–520.
Grant, B. F., Stinson, F. S., Dawson, D. A., Chou, S. P., Dufour, M. C., & Compton, W., et al. (2004). Prevalence and co-occurrence of substance use disorders and independentmood and anxiety disorders: results from the national epidemiologic survey on alcohol and relatedconditions. Archives of General Psychiatry, 61(8), 807–816.
Grella, C. E., Stein, J. A., & Greenwell, L. (2005). Associations among childhood trauma, adolescent problem behaviors, and adverse adult outcomes in substance-abusing women offenders. Psychology of Addictive Behaviors, 19(1), 43.
Griffith, J. W., Sumner, J. A., Raes, F., Barnhofer, T., Debeer, E., & Hermans, D. (2012). Current psychometric and methodological issues in the measurement of overgeneral autobiographical memory. Journal of Behavior Therapy and Experimental Psychiatry, 43, S21–S31.
Hammen, C., Adrian, C., Gordon, D., Burge, D., Jaenicke, C., & Hiroto, D. (1987). Children of depressed mothers: maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology, 96(3), 190.
Hammen, C., Marks, T., Mayol, A., & DeMayo, R. (1985). Depressive self-schemas, life stress, and vulnerability to depression. Journal of Abnormal Psychology, 94(3), 308.
Hancox, R. J., Milne, B. J., & Poulton, R. (2004). Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. The Lancet, 364(9430), 257–262.
Hardt, J., & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273.
Härter, M. C., Conway, K. P., & Merikangas, K. R. (2003). Associations between anxiety disorders and physical illness. European Archives of Psychiatry and Clinical Neuroscience, 253(6), 313–320.
Hasin, D. S., Stinson, F. S., Ogburn, E., & Grant, B. F. (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64(7), 830–842.
Hayward, C., Killen, J. D., Kraemer, H. C., & Taylor, C. B. (2000). Predictors of panic attacks in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 39(2), 207–214.
Heim, C., Newport, D. J., Mletzko, T., Miller, A. H., & Nemeroff, C. B. (2008). The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology, 33(6), 693–710.
Hollingshead, A. (1975). Four factor index of social status. New Haven, CT: Yale University. Unpublished manuscript.
Irish, L., Kobayashi, I., & Delahanty, D. L. (2009). Long-term physical health consequences of childhood sexual abuse: a meta-analytic review. Journal of Pediatric Psychology, jsp118.
Johnston, L. D., O’Malley, P. M., Miech, R. A., Bachman, J. G., & Schulenberg, J. E. (2015). Monitoring the Future national survey results on drug use: 1975–2014: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan.
Keenan-Miller, D., Hammen, C. L., & Brennan, P. A. (2007). Health outcomes related to early adolescent depression. Journal of Adolescent Health, 41(3), 256–262.
Khoury, L., Tang, Y. L., Bradley, B., Cubells, J. F., & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety, 27(12), 1077–1086.
Kiecolt-Glaser, J. K., & Glaser, R. (2002). Depression and immune function: central pathways to morbidity and mortality. Journal of Psychosomatic Research, 53(4), 873–876.
Koob, G. F., & Le Moal, M. (2001). Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology, 24(2), 97–129.
Lissau, I., & Sorensen, T. I. (1994). Parental neglect during childhood and increased risk of obesity in young adulthood. The Lancet, 343(8893), 324–327.
Marx, B. P., & Sloan, D. M. (2003). The effects of trauma history, gender, and race on alcohol use and posttraumatic stress symptoms in a college student sample. Addictive Behaviors, 28(9), 1631–1647.
McGee, R., Williams, S., Poulton, R., & Moffitt, T. (2000). A longitudinal study of cannabis use and mental health from adolescence to early adulthood. Addiction, 95(4), 491–503.
Moldin, S. O., Scheftner, W. A., Rice, J. P., Nelson, E., Knesevich, M., & Akiskal, H. (1993). Association between major depressive disorder and physical illness. Psychological Medicine, 23(3), 755–761.
Myers, B., McLaughlin, K. A., Wang, S., Blanco, C., & Stein, D. J. (2014). Associations between childhood adversity, adult stressful life events, and past-year drug use disorders in the National Epidemiological Study of Alcohol and Related Conditions (NESARC). Psychology of Addictive Behaviors, 28(4), 1117.
Norman, R. E., Byambaa, M., De, R., Butchart, A., Scott, J., & Vos, T. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Medicine, 9(11), e1001349.
Putnam, F. W. (2006). The impact of trauma on child development. Juvenile and Family Court Journal, 57(1), 1–11.
Raposa, E. B., Hammen, C. L., Brennan, P. A., O’Callaghan, F., & Najman, J. M. (2014). Early adversity and health outcomes in young adulthood: The role of ongoing stress. Health Psychology, 33(5), 410.
Schulte, M. T., & Hser, Y. (2014). Substance use and associated health conditions throughout the lifespan. Public Health Reviews, 35(2), 1–27.
Shen, B. -J., Eisenberg, S. A., Maeda, U., Farrell, K. A., Schwarz, E. R., & Penedo, F. J., et al. (2011). Depression and anxiety predict decline in physical health functioning in patients with heart failure. Annals of Behavioral Medicine, 41(3), 373–382.
Sheridan, M. A., & McLaughlin, K. A. (2014). Dimensions of early experience and neural development: deprivation and threat. Trends in Cognitive Sciences, 18(11), 580–585.
Springer, K. W., Sheridan, J., Kuo, D., & Carnes, M. (2007). Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect, 31(5), 517–530.
Technow, J. R., Hazel, N. A., Abela, J. R., & Hankin, B. L. (2015). Stress sensitivity interacts with depression history to predict depressive symptoms among youth: prospective changes following first depression onset. Journal of Abnormal Child Psychology, 43(3), 489–501.
Triffleman, E. G., Marmar, C. R., Delucchi, K. L., & Ronfeldt, H. (1995). Childhood trauma and posttraumatic stress disorder in substance abuse inpatients. The Journal of Nervous and Mental Disease, 183(3), 172–176.
Twisk, J., Kemper, H., & Van Mechelen, W. (2002). The relationship between physical fitness and physical activity during adolescence and cardiovascular disease risk factors at adult age. The Amsterdam Growth and Health Longitudinal Study. International Journal of Sports Medicine, 23(S1), 8–14.
Vrshek-Schallhorn, S., Stroud, C. B., Mineka, S., Hammen, C., Zinbarg, R. E., & Wolitzky-Taylor, K., et al. (2015). Chronic and episodic interpersonal stress as statistically unique predictors of depression in two samples of emerging adults. Journal of Abnormal Psychology, 124(4), 918.
Vrshek-Schallhorn, S., Wolitzky-Taylor, K., Doane, L. D., Epstein, A., Sumner, J. A., & Mineka, S., et al. (2014). Validating new summary indices for the Childhood Trauma Interview: Associations with first onsets of major depressive disorder and anxiety disorders. Psychological Assessment, 26(3), 730.
Walker, E. A., Gelfand, A., Katon, W. J., Koss, M. P., Von Korff, M., & Bernstein, D., et al. (1999). Adult health status of women with histories of childhood abuse and neglect. The American Journal of Medicine, 107(4), 332–339.
Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care, 473-483.
Wegman, H. L., & Stetler, C. (2009). A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine, 71(8), 805–812.
Wickrama, K. K., Lee, T. K., O’Neal, C. W., & Kwon, J. A. (2015). Stress and resource pathways connecting early socioeconomic adversity to young adults’ physical health risk. Journal of Youth and Adolescence, 44(5), 1109–1124.
Wolitzky-Taylor, K., Bobova, L., Zinbarg, R. E., Mineka, S., & Craske, M. G. (2012). Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addictive Behaviors, 37(8), 982–985.
Wolitzky-Taylor, K., Vrshek-Schallhorn, S., Waters, A. M., Mineka, S., Zinbarg, R. E., & Ornitz, E. M., et al. (2014). Adversity in early and midadolescence is associated with elevated startle responses to safety cues in late adolescence. Clinical Psychological Science, 2(2), 202–213.
Zinbarg, R. E., Mineka, S., Craske, M. G., Griffith, J. W., Sutton, J., & Rose, R. D., et al. (2010). The Northwestern-UCLA youth emotion project: associations of cognitive vulnerabilities, neuroticism and gender with past diagnoses of emotional disorders in adolescents. Behaviour Research and Therapy, 48(5), 347–358.
Authors’ Contributions
K.W. and A.R.S. developed the research questions, conducted data analysis, and prepared the manuscript. S.V. assisted with manuscript preparation and data analysis. L.B. assisted with data management and manuscript editing. E.K.A. and C.H. provided manuscript feedback and revisions. R.E.Z., S.M., and M.G.C. developed the research design of the YEP and provided manuscript editing and feedback. All authors were involved in either the design of the project or data collection, and all approved the final version of the manuscript.
Funding
The research reported and the preparation of this article was supported by National Institute of Mental Health Grants R01 MH65651 and R01 MH65652 to Michelle G. Craske, Susan Mineka, and Richard E. Zinbarg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wolitzky-Taylor, K., Sewart, A., Vrshek-Schallhorn, S. et al. The Effects of Childhood and Adolescent Adversity on Substance Use Disorders and Poor Health in Early Adulthood. J Youth Adolescence 46, 15–27 (2017). https://doi.org/10.1007/s10964-016-0566-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10964-016-0566-3