Abstract
Background
Few studies have examined the prospective influences of depression and anxiety on physical health functioning in heart failure (HF) patients. Prior studies were also limited by employing psychological measures containing somatic items confounded with HF symptoms.
Purpose
This study examined whether depression, anxiety, social support, and their changes predicted the decline of physical functioning in HF patients over 6 months.
Methods
Participants were 238 HF patients among whom 164 provided follow-up data. The depression and anxiety measures did not contain somatic items.
Results
After controlling for baseline physical functioning and demographic and medical covariates, baseline depression and its increase, as well as baseline anxiety and its increase, independently predicted greater decline in physical functioning at 6 months. Social support and its change were not associated with either concurrent or follow-up physical functioning.
Conclusions
Depression, anxiety, and their changes independently predicted the decline of physical health functioning over 6 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the extraordinary medical advances in recent years, heart failure (HF) remains a devastating disease with a poor prognosis. It is estimated that five million people have HF in the USA, with approximately 550,000 new cases diagnosed annually. Heart failure is also a direct or contributing cause of death for more than 287,000 Americans every year [1].
In addition to the severe physical impairments, many HF patients also face harsh emotional challenges, particularly depression and anxiety. Research has indicated that at least one in five HF patients present clinically significant depressive symptoms [2], and the prevalence of anxiety has been reported in the range of 18% to 63% [3–5].
Research has just begun to investigate the adverse effects of depression and anxiety on the clinical outcomes in HF patients. Both depression [4, 6–11] and anxiety [4, 10] have been linked to higher mortality, although the predictive ability of anxiety appeared to diminish after adjusting for demographic and clinical covariates. In addition, elevated depression [9, 12] and anxiety [13] have also contributed to greater likelihood and frequency of hospitalization even after controlling for other demographic and medical factors.
As improved treatment continues to extend patients' lives, more research has started exploring the relevance of emotional and psychosocial factors that may facilitate or hinder their everyday physical health functioning and quality of life. Most existing studies have observed that depression is cross-sectionally associated with poor physical functioning in HF patients [14–17]. Few prospective studies have investigated the influence of depression on health functioning over time and have primarily focused on the general ability to perform daily living tasks such as grooming, dressing, and bathing oneself. Two studies observed that depression independently predicted the decline in activities of daily living over 6 months to a year [18, 19]. One study demonstrated a significant association between depressive symptoms and decline in activities of daily living among HF patients at 6 month follow-up after adjusting for baseline activities of daily living, sociodemographic background, ejection fraction, blood pressure, dyspnea-related physical limitation, HF-related hospitalizations, and history of myocardial infarction and diabetes [18]. Another study identified depressed mood as a significant predictor of severe limitations in activities of daily living at 1 year in HF patients after adjusting for age, ejection fraction, New York Heart Association (NYHA) class, HF diagnosis, risk status, medical comorbidities, and clinical deterioration during the year [19].
Even fewer studies have focused on the impact of anxiety on physical functioning among HF patients. Two cross-sectional studies showed that anxiety was associated with lower quality of life [20] and physical functioning [21]. One prospective investigation suggested that anxiety predicted severe deficits in activities of daily living over 1 year after adjusting for age, gender, and NYHA class [20]. In sum, while these studies provided preliminary indication that depression and anxiety are associated with poorer physical functioning among HF patients, more longitudinal investigations are needed to scrutinize the prospective influences of these psychological variables of emotional distress.
Social support is a psychological factor that has long been recognized for its salutary influence on health. The research on social support in HF patients, however, has yielded mixed results. The lack of social support was found to predict mortality in one study [22] but not in another [4]. In a study examining physical functioning, HF patients who were unmarried or who rarely received visits from or made visits to family or friends were at significantly higher risk of serious impairment in activities of daily living at 1 year than those with higher levels of social integration after adjusting for age, medication assignment, ejection fraction, NYHA class, and HF diagnosis. However, this effect was no longer significant after further adjusting for history of diabetes, chronic obstructive pulmonary disease, cerebrovascular accident, baseline risk status, and clinical deterioration during the year [19]. Another study followed HF patients over 1 year and did not find a significant association between baseline social support and quality of life after adjusting for baseline quality of life, demographic background, and clinical variables [23]. Increases in social support in this study, however, did predict improvement in quality of life after adjusting for the same covariates [23].
There are several notable limitations in the current literature that render the interpretations of these findings difficult. First, the measures of depression and anxiety used in prior studies included many somatic symptoms confounded with the physical ailments of HF, such as fatigue, lack of appetite, and insomnia in depression, as well as trembling, shaking, and shortness of breath in anxiety. Inclusion of these items had likely inflated their associations with physical health status. Second, the anxiety measures in prior research also appeared to contain many depressive symptoms, thereby compromising the validity of the findings. Third, there is a general lack of prospective research investigating whether these psychological factors and their changes predict changes in physical health functioning over time. Finally, the physical health functioning examined in prior studies primarily focused on the general activities of daily living and did not directly assess items specifically related to HF.
This study examined the following research questions and hypotheses. First, we investigated the prevalence of depression and anxiety using measures that did not contain somatic items that confounded the symptoms of HF. It was hypothesized that both depression and anxiety were highly prevalent in HF patients. Second, it was hypothesized that lower depression and anxiety and higher social support were concurrently associated with HF-related physical health functioning. Third, it was postulated that these psychological factors and their changes independently predicted the decline or improvement of physical health functioning over 6 months.
Methods
Participants
The participants were 238 patients with HF recruited from the Cardiology Outpatient Clinic of the University of Miami Medical Center. All patients were confirmed by the attending cardiologists to meet clinical criteria for HF. Eligible patients were at least 18 years of age and had a primary diagnosis of HF. Patients were excluded if they were receiving treatment for another life-threatening medical condition (e.g., cancer) that confounded the assessment of their health status, if they showed active psychotic symptoms or cognitive deficits that prevented them from understanding and responding to interviews and questionnaires, or if they declined to provide informed consent. At 6 months, 164 participants completed the follow-up assessments.
Procedures
The participants were interviewed and evaluated by the research staff to provide vital signs, anthropometric measures, and health history. They provided a fasting blood sample and completed questionnaires assessing physical and mental health functioning, psychosocial characteristics, and health behaviors. The research staff also inquired whether patients were currently receiving or had received treatment in the past for depression or anxiety and the types of treatment received. The participants' medical records were reviewed to retrieve relevant medical history and health information.
Participants were reassessed at 6 months after baseline for their physical health functioning and psychological characteristics. This study was approved by the university and hospital institutional review boards. All participants provided informed consent.
Measures
Physical Health Functioning
Physical health functioning was assessed by the physical dimension of the Minnesota Living with Heart Failure Questionnaire (MLHFQ) [24, 25]. The MLHFQ assesses the degree to which HF impairs one's life in various domains, including physical functioning, emotional functioning, social life, and daily living, on a scale from 0 (not at all) to 5 (very much). The instrument demonstrates excellent reliability and validity, and is widely used to evaluate HF patients [26]. Physical functioning (e.g., limited physical capacity, fatigue, shortness of breath) and emotional functioning (e.g., depression, worry, and low self-esteem) constitute two major domains of the MLHFQ [25]. This study focused on physical functioning as the emotional items in the MLHFQ overlapped with the predictors of interest (depression and anxiety). The physical items assess the degree to which HF causes difficulties with sitting or lying down to rest, fatigue, shortness of breath, climbing stairs, house chores or yard work, sleeping at night, and activities with family or friends. The internal consistency of these items was excellent with Cronbach's α = .94. An average score was used in the analysis. High scores indicate poorer functioning.
Depression
Depressive symptomatology was measured by the Center for Epidemiologic Studies Depression (CES-D) scale whose reliability, validity, and clinical utility have been well established [27, 28]. It contains items representing clinical manifestations of depression, including feeling sad and blue, low self-worth, hopelessness, lack of interest, interpersonal difficulties, and somatic complaints on a scale from 0 (rarely or none of the time) to 3 (most or all of the time).
The factor analytic research on the measurement structure of CES-D has identified that somatic items are one of the major domains of depressive symptoms [29, 30]. These somatic items include poor appetite, restless sleep, inability to get going, talking less, feeling that everything is effortful, trouble concentrating, and being bothered by things. They are problematic in assessing mood disturbances in HF patients because they overlap with symptoms and difficulties stemming from the physical ailments. Therefore, they were removed from the CES-D to avoid confounding with physical functioning and overestimating depression severity. The CES-D without somatic items was used for both predictive and descriptive analyses. In order to use the cut-off scores with the original scale, the sum scores were prorated. The internal consistency reliability of the modified scale was high with Cronbach's α = .85.
Anxiety
Anxiety was measured by the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS) [31]. It consists of seven items tapping symptoms of worry, fear, inability to relax, and feelings of panic. Unlike other measures of anxiety, the HADS was developed specifically for medical patients. It does not contain somatic signs of anxiety, such as heart palpitation, sweating, and dizziness, which are often confounded with symptoms of physical diseases. It showed high reliability with Cronbach's α = .82. A sum score was used in the analysis.
Social Support
The 18-item Medical Outcome Study Social Support Survey is a valid and reliable instrument developed to assess the perceived availability and levels of social support among patients with chronic illness [32]. It contains items of emotional, informational, affectionate, and tangible support, as well as positive social interactions on a scale from 1 (none of the time) to 5 (all of the time). The internal consistency was excellent (Cronbach's α = .97). An average score was used in the analysis.
Other Clinical and Health Variables
A number of clinical and health variables were extracted from the medical records. These included the NYHA classification, left ventricular ejection fraction, history of cardiovascular disease, history of cardiac surgery, implanted devices, cardiac risk factors (hypertension, dyslipidemia, and diabetes), psychiatric history, and prescribed medications.
Statistical Analysis
Multiple regression analyses were conducted to examine whether depression, anxiety, and social support were associated with physical health functioning at baseline and at 6 months while controlling for demographic and medical covariates. Each psychological variable was first tested separately, and then they were tested together if multicollinearity was not a concern. Standardized regression coefficients are presented in the Results section.
All analyses were adjusted for demographic and medical covariates, including age, gender, marital status, education, NYHA class, and treatment for depression or anxiety. These control variables were selected because they were commonly included in prior research, thus facilitating comparisons across studies. They were also selected on the basis of the literature suggesting that they are associated with both psychological distress and physical functioning in heart failure patients [16, 18, 33, 34]. We also considered and tested left ventricular ejection fraction, time since HF diagnosis, and various cardiac medications listed in Table 1 as potential covariates. None were significantly related to physical functioning except that angiotensin-converting enzyme inhibitors were correlated with baseline physical scores (r = −0.15, p = .03). The use of angiotensin-converting enzyme inhibitors was added as a covariate in analyses with baseline physical functioning as the outcome.
To examine the cross-sectional associations, we tested whether each psychological factor predicted concurrent physical health functioning while controlling for demographic background and medical covariates. For the longitudinal relationships, we tested whether psychological factors significantly predicted the follow-up physical functioning at 6 months while controlling for the standard covariates specified previously and the baseline physical functioning. The inclusion of baseline physical functioning as a covariate allowed us to interpret whether psychological factors were associated with the change in physical functioning over time. Finally, to examine whether the change in psychosocial variables predicted the decline in physical functioning, we computed the change scores for depression, anxiety, and social support over 6 months by subtracting their baseline values from the 6-month values. We then regressed the 6-month physical functioning on depression, anxiety, or social support and its respective change scores while controlling for standard covariates and baseline physical functioning.
Results
Participant Characteristics
Two hundred thirty-eight participants (32% women) completed baseline assessments. Descriptive statistics for key study variables and covariates are presented in Table 1. Participants had a mean age of 54 (SD = 11) years. Approximately half (56%) were married or partnered. Most had completed high school (34%) or at least had some college education (52%). The majority were disabled, retired, or unemployed (76%). The sample was comprised of 26% Caucasians, 24% African Americans, 44% Hispanics, and 5% others.
The participants had a mean left ventricular ejection fraction of 26% (SD = 13%), with 43% reporting a history of coronary artery disease and 40% myocardial infarction. About half (52%) of the participants had an implantable cardioverter defibrillator. Major cardiovascular risk factors were elevated in the group, with 65% being hypertensive, 45% dyslipidemic, 42% obese, and 33% diabetic. For mental health services, 16% of participants reported receiving treatment for either depression, anxiety, or both.
Attrition Analysis
Seventy-four individuals did not return for the follow-ups, including nine patients who died, 15 who received a heart transplant, and 50 who did not respond to repeated requests. To compare the participants who returned with those who did not, we conducted t tests or chi-square tests to examine differences in their demographic and medical characteristics (Table 1). The results showed that they did not differ in their psychological factors (depression, anxiety, and social support), physical functioning, gender, marital status, education, ethnicity, employment status, left ventricular ejection fraction, time since diagnosis, NYHA class, cardiovascular metabolic risk factors, and cardiac history and medications. However, those who did not provide follow-ups were somewhat younger (p = 0.01), exhibited higher diastolic blood pressure (p < 0.01), and were less likely to be on statins (p = 0.02).
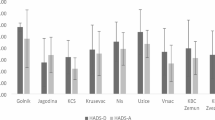
Depression and Anxiety Symptom Severity at Baseline and 6 Months
Using the cut-offs established in prior research on the CES-D [31], 50% of the patients in this study showed no depression (<16), 23% endorsed mild symptoms (16–26), and 27% reported moderate to severe depression (>26). At 6 months, the distribution was largely similar, with 51% showing no depression, 25% mild depression, and 24% moderate to severe depression. Applying the guideline of the HADS [29], 55% of the patients showed little or no anxiety symptoms (<8) at the baseline, 24% indicated borderline anxiety (8–10), and 21% reported severe anxiety (>10) warranting clinical attention. Anxiety severity at 6 months follow-up was similarly distributed at 55%, 26%, and 19%, respectively.
As a group, the average depression and anxiety scores at baseline did not differ significantly from those at 6 months (t = 0.16, p = 0.87, for depression; t = −0.91, p = 0.36, for anxiety). However, the baseline and follow-up scores were moderately correlated at .67 (p < 0.01) for depression and .55 (p < 0.01) for anxiety, suggesting substantial individual differences in the change of depression and anxiety over time.
Psychological Factors and Concurrent Physical Health Functioning
Table 2 presents the results of the regression analyses that tested the associations between the psychological factors and physical health functioning at baseline and 6 months. The results showed that higher depression (β = 0.40, p < 0.01) and anxiety (β = 0.42, p < 0.01), but not social support (β = −0.06, p = 0.32), were significantly associated with lower physical health functioning in separate models after controlling for age, gender, marital status, education, NYHA class, and treatment for anxiety or depression. When all psychological variables were entered simultaneously with standard covariates, both depression (β = 0.25, p < 0.01) and anxiety (β = 0.25, p < 0.01) remained significant while social support (β = 0.04, p = 0.46) still was not. It should be cautioned that depression and anxiety were highly correlated (r = 0.74) and might lead to multicollinearity problems, although the variance inflation factors were still acceptable (<2.50). Among covariates, higher NYHA class (βs = 0.45–0.49, ps < 0.01) was also significantly associated with lower physical functioning in these models.
Psychological Factors and Physical Health Functioning at 6 Months
In the regression analyses for prospective relationships, the results showed that depression (β = 0.15, p = 0.02) and anxiety (β = 0.21, p < 0.01), but not social support (β = −0.03, p = 0.61), predicted the decline in physical functioning in separate multivariate models. When all psychological factors were entered into the model simultaneously, only anxiety (β = 0.18, p = 0.04) was a significant predictor of physical functioning at 6 months. Among other predictors, baseline physical functioning (βs = 0.61–.71, ps < 0.01) also consistently predicted 6-month physical functioning, and the NYHA class (βs = 0.09 to 0.12, ps = 0.16 to 0.05) was significant or marginally significant in the models.
Changes in Psychological Factors and Physical Health Functioning at 6 Months
We also tested whether changes in depression or anxiety scores predicted physical functioning at 6 months while controlling for standard covariates, respective baseline psychological variables, and baseline physical functioning. In the model examining depression, both the increase in depression scores (β = 0.28, p < 0.01) and baseline depression (β = 0.29, p < 0.01) significantly predicted the decline in physical functioning at 6 months. For anxiety, both an increase in anxiety scores (β = 0.23, p < 0.01) and baseline anxiety (β = 0.32, p < 0.01) predicted lower physical functioning at 6 months. For social support, neither the baseline (β =−0.03, p = 0.64) nor its change (β = −0.01, p = 0.94) predicted the physical functioning at 6 months. The model combining depression, anxiety, social support, and their change scores was not tested because of the multicollinearity problem (variance inflation factors = 2.10–3.96).
Discussion
This study showed that both depression and anxiety were common emotional difficulties experienced by HF patients. Approximately half or more of the participants exhibited moderate to severe symptoms of depression or anxiety. This result is particularly alarming, considering that the measures used in this study were devoid of somatic symptoms and could not falsely inflate the severity of these emotional disturbances.
In addition to the observation that emotional distress was common in HF patients, this study also demonstrated that depression and anxiety at baseline independently predicted not only the concurrent physical health functioning but also its decline over a 6-month period while controlling for demographic and medical covariates. Furthermore, the increase in depression or anxiety symptoms over 6 months further predicted the deterioration in patients' physical functioning, which could not be explained by the baseline levels of depression and anxiety, as well as other covariates. Unlike prior studies [14–17, 19, 21], the anxiety and depression measures in this study did not contain confounding somatic items. This constituted more precise tests with conceptually clearer measures and provided stronger evidence for the prospective influences of psychological distress on the physical functioning of HF patients. We are confident that the associations observed were not due to the overlap in items measuring psychological distress and physical functioning impairments. These results also highlight the importance of assessing and monitoring patients' psychological symptoms over time to identify those at higher risk of deterioration.
Although depression and anxiety symptoms appeared to be highly correlated (r = 0.74) in this study, they did not coincide completely. Sixteen percent of the non-depressed patients showed significant anxiety symptoms, while 23% of those without anxiety exhibited elevated depression. This result suggests that both depression and anxiety should be considered in order to sufficiently identify those eligible for further evaluation and services. When both depression and anxiety were present in the analysis to predict physical functioning at follow-up, the effect of anxiety appeared to be somewhat stronger. Due to the high correlation between depression and anxiety, this finding should be interpreted with caution. It does not imply that anxiety should supersede or replace depression as the focus of assessment and intervention as both prognosticate the decline of physical functioning.
Several potential mechanisms may explain the relationship between elevated depression or anxiety and decline in physical functioning. First, patients with higher depression or anxiety could have exaggerated their functional decline because of fear and pessimism. Some studies of very frail elderly individuals suggested that emotionally distressed patients tended to underestimate their abilities to perform general daily living tasks [35]. Nevertheless, the present study assessed HF-specific physical functioning, and the effects of depression and anxiety remained substantial after adjusting for covariates. Perception bias alone was not likely to fully explain the observed associations. In addition, Watson and Pennebaker suggest that certain personality traits, such as negative affectivity and neuroticism, might have led the participants to report higher negative emotions and more health complaints at the same time and thus contributed to their association [36]. There are, however, several key differences between the present study and the work of Watson and Pennebaker which was primarily supported by studies of generally healthy undergraduate students with cross-sectional analyses. This study investigated HF patients with both psychosocial factors and health functioning assessed longitudinally, and the physical functioning measure has been shown to predict more objective health outcomes, including disease severity, physical capacity, and mortality [37, 38]. That is, negative affectivity may have explained some but not all of the association between anxiety, depression, and declining health. Second, the broader literature in psychosocial factors and heart disease have suggested several physiological mechanisms that may explain the detrimental effects of depression and anxiety on health, including sympathetic hyper-arousal, reduced heart rate variability, impaired platelet functioning, elevated inflammation, and hypercortisolemia [39, 40]. Third, patients with high depression and anxiety may have neglected self-care, engaged in health-compromising behaviors, and failed to adhere to the demanding dietary and medical regimen for HF [39, 41, 42], all of which may have led to negative health outcomes. Lastly, it is plausible that emotional distress and physical functioning in HF patients are influencing each other in a reciprocal fashion such that heightened emotional distress leads to greater decline in physical functioning, while this health decline may, in turn, exacerbate the emotional distress. That is, anxiety and depression may be both the progenitors and consequences of increased physical impairment. A longitudinal study with multiple repeated assessments of both physical and psychological factors will be needed to disentangle these intricate bidirectional influences.
This study did not find that social support or its change was related to either concurrent or longitudinal measures of physical functioning. However, this finding is not notably at odds with prior research [4, 19, 23], in which studies either did not find an association or observed significant attenuation in the strength of the relationship after adjustment of covariates. A possible explanation may be that the participants reported fairly strong social support in general, thus restricting its variability and predictive utility. Those with low social support may not have been able to manage their illnesses, which resulted in severe impairments or even premature death and prevented them from participating in research. Furthermore, it could be that 6 months was not enough time to allow social support to manifest its influence. For example, one prior study reported that the lack of social support predicted mortality over 6 years [22], whereas, in other studies, social support was not related to health-related quality of life over 1 to 2 years [4, 23]. In addition, social support is a complicated construct with divergent conceptualizations, definitions, and measurements [43]. While this study examined the availability of emotional, informational, and instrumental support, other facets of support, such as social network size and density, social integration, and quality of marriage and social relations were not explored. Further research is needed to scrutinize whether certain dimensions of social support may be more influential in predicting clinical outcomes.
There are some limitations which also suggest directions for future research. First, in addition to deaths and recipients of heart transplants, there was a moderate degree of attrition due to non-responding at 6 months. Although the attrition analysis did not reveal major demographic, medical, and psychosocial differences in general, there were some noticeable differences indicating that dropouts may not have been random. The patients not available at 6 months were somewhat younger, had higher diastolic blood pressure, and were less likely to be on statins. These differences suggested that patients who dropped out might be more isolated and did not have their cardiac risk factors well-controlled or treated. In addition, the study sample appeared to be younger than the usual HF patients, which was likely to reflect the nature of patients from a tertiary care medical center. In addition, the participants were self-selected to take part in this study, resulting in a sample of convenience. We were not able to test whether there had been differences between those who participated and those who did not. These factors may constrain the generalizability of these findings. Furthermore, the depression and anxiety measures assessed symptom severity and did not establish clinical diagnoses as defined in the psychiatric diagnostic manual. We were therefore unable to examine whether clinical psychiatric disorders and the subtypes of depressive and anxiety disorders may have had differential associations with the physical functioning outcomes.
Despite these limitations, this is one of the first prospective studies to demonstrate that depression and anxiety, as well as their increases over time, independently predict the decline in physical health functioning among HF patients. The results highlight the importance of assessing, monitoring, and managing depression and anxiety in HF patients. Future studies should examine the potential behavioral and physiological mechanisms by which psychological distress may affect physical health functioning, and vice versa, in these patients. Psychosocial interventions that alleviate depression and anxiety may be promising for promoting the mental well-being as well as physical health functioning of distressed HF patients.
References
AHA: Heart disease and stroke statistics—2009 update: American Heart Association, 2009.
Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ: Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006, 48:1527–1537.
Haworth JE, Moniz-Cook E, Clark AL, et al.: Prevalence and predictors of anxiety and depression in a sample of chronic heart failure patients with left ventricular systolic dysfunction. Eur J Heart Fail. 2005, 7:803–808.
Friedmann E, Thomas SA, Liu F, et al.: Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006, 152:940 e941–e948.
De Jong MJ, Moser DK, An K, Chung ML: Anxiety is not manifested by elevated heart rate and blood pressure in acutely ill cardiac patients. European Journal of Cardiovascular Nursing. 2004, 3:247–253.
Albert NM, Fonarow GC, Abraham WT, et al.: Depression and clinical outcomes in heart failure: An OPTIMIZE-HF analysis. Am J Med. 2009, 122:366–373.
Faller H, Stork S, Schowalter M, et al.: Depression and survival in chronic heart failure: Does gender play a role? Eur J Heart Fail. 2007, 9:1018–1023.
Frasure-Smith N, Lesperance F, Habra M, et al.: Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009, 120:134–140, 133p following 140.
Jiang W, Alexander J, Christopher E, et al.: Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001, 161:1849–1856.
Jiang W, Kuchibhatla M, Cuffe MS, et al.: Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004, 110:3452–3456.
Junger J, Schellberg D, Muller-Tasch T, et al.: Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail. 2005, 7:261–267.
Sherwood A, Blumenthal JA, Trivedi R, et al.: Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007, 167:367–373.
Tsuchihashi-Makaya M, Kato N, Chishaki A, Takeshita A, Tsutsui H: Anxiety and poor social support are independently associated with adverse outcomes in patients with mild heart failure. Circ J. 2009, 73:280–287.
Bekelman DB, Havranek EP, Becker DM, et al.: Symptoms, depression, and quality of life in patients with heart failure. J Card Fail. 2007, 13:643–648.
Faller H, Stork S, Schuler M, et al.: Depression and disease severity as predictors of health-related quality of life in patients with chronic heart failure—a structural equation modeling approach. J Card Fail. 2009, 15:286–292 e282.
Gottlieb SS, Khatta M, Friedmann E, et al.: The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004, 43:1542–1549.
Muller-Tasch T, Peters-Klimm F, Schellberg D, et al.: Depression is a major determinant of quality of life in patients with chronic systolic heart failure in general practice. J Card Fail. 2007, 13:818–824.
Vaccarino V, Kasl SV, Abramson J, Krumholz HM: Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol. 2001, 38:199–205.
Clarke SP, Frasure-Smith N, Lesperance F, Bourassa AG: Psychosocial factors as predictors of functional status at 1 year in patients with left ventricular dysfunction. Research in Nursing and Health. 2000, 23:290–300.
Chung ML, Moser DK, Lennie TA, Rayens MK: The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: Testing dyadic dynamics using Actor-Partner Interdependence Model. J Psychosom Res. 2009, 67:29–35.
Muller-Tasch T, Frankenstein L, Holzapfel N, et al.: Panic disorder in patients with chronic heart failure. J Psychosom Res. 2008, 64:299–303.
Murberg TA: Long-term effect of social relationships on mortality in patients with congestive heart failure. Int J Psychiatry Med. 2004, 34:207–217.
Bennett SJ, Perkins SM, Lane KA, et al.: Social support and health-related quality of life in chronic heart failure patients. Qual Life Res. 2001, 10:671–682.
Rector TS, Kubo SH, Cohn JN: Patients' self-assessment of their congestive heart failure. Part 2: Content, reliability and validity of a new measure, the Minnesota Living with Heart Failure Questionnaire Heart Failure. 1987:198–209.
Rector TS, Cohn JN: Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: Reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. Pimobendan Multicenter Research Group. Am Heart J. 1992, 124:1017–1025.
Garin O, Ferrer M, Pont A, et al.: Disease-specific health-related quality of life questionnaires for heart failure: A systematic review with meta-analyses. Qual Life Res. 2009, 18:71–85.
Radloff LS: The CES-D scale: A self report depression scale for research in general populations. Applied Psychological Measurement. 1977, 1:385–401.
Radloff LS, Locke BZ: The Community Mental Health Assessment Survey and the CES-D Scale. In M. M. Weissman, J. K. Myers and C. E. Ross (eds), Community Surveys of Psychiatric Disorders. New Brunswick, NJ: Rutgers University Press, 1986, 177–189.
Callahan CM, Wolinsky FD. The effect of gender and race on the measurement properties of the CES-D in older adults. Med Care. Apr 1994, 32: 341–356.
Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res Ther. Apr 1997, 35: 373–380.
Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983, 67:361–370.
Sherbourne CD, Stewart AL: The MOS social support survey. Soc Sci Med. 1991, 32:705–714.
Riedinger MS, Dracup KA, Brecht ML et al.: Quality of life in patients with heart failure: Do gender differences exist? Heart Lung. 2001, 30:105–116.
Rumsfeld JS, Havranek E, Masoudi FA, et al.: Depressive symptoms are the strongest predictors of short-term declines in health status in patients with heart failure. J Am Coll Cardiol. 2003, 42: 1811–1817.
Cress ME, Schechtman KB, Mulrow CD, et al.: Relationship between physical performance and self-perceived physical function. J Am Geriatr Soc. 1995, 43:93–101.
Watson D & Pennebaker JW: Health complaints, stress, and distress: Exploring the central role of negative affectivity. Psychol Rev. 1989, 96:235–254.
Juenger J, Schellberg D, Kraemer S, et al.: Health related quality of life in patients with congestive heart failure: Comparison with other chronic diseases and relation to functional variables. Heart. 2002, 87: 235–241.
Rodriguez-Artalejo F, Guallar-Castillon P, Pascual CR, et al.: Health-related quality of life as a predictor of hospital readmission and dealth among patients with heart failure. Arch Intern Med. 2002, 165: 1274–1279.
Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L: The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005, 45:637–651.
Kubzansky LD, Kawachi I, Weiss ST, Sparrow D: Anxiety and coronary heart disease: A synthesis of epidemiological, psychological, and experimental evidence. Ann Behav Med. 1998, 20:47–58.
DiMatteo MR, Lepper HS, Croghan TW: Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000, 160:2101–2107.
Ziegelstein RC, Fauerbach JA, Stevens SS, et al.: Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000, 160:1818–1823.
House JS, Umberson D, Landis KR: Structures and processes of social support. Annual Review of Sociology. 1988, 14:293–318.
Acknowledgments
The authors would like to extend our gratitude to Drs. Nanette H. Bishopric, M.D., Martin S. Bilsker, M.D., Javier Jimenez, M.D., Ph.D., Sharon Andrade-Bucknor, M.D., and Jay S. Kerzner, M.D., at University of Miami Miller School of Medicine and Dr. Michelle Lister, M.D., at Miami International Cardiology for their assistance in recruiting the participants.
This work was supported by a grant from the American Heart Association and an award from the National Alliance for Research on Schizophrenia and Depression.
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shen, BJ., Eisenberg, S.A., Maeda, U. et al. Depression and Anxiety Predict Decline in Physical Health Functioning in Patients with Heart Failure. ann. behav. med. 41, 373–382 (2011). https://doi.org/10.1007/s12160-010-9251-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9251-z