Abstract
The current study explored the relationship between religious coping and cumulative health risk associated with health behavior patterns in a sample of 256 Latina and Caucasian female caregivers of elderly relatives with dementia. Primary analyses examined the relationship between religious coping (both positive and negative) and an overall index of cumulative health risk. Secondary analyses were conducted on the individual health behaviors subsumed in the broader index. Findings revealed that negative religious coping was significantly associated with increased cumulative health risk. Positive religious coping was predictive of decreased cumulative health risk among Latina caregivers but not among Caucasians. Negative religious coping was significantly associated with both an increased likelihood for weight gain and increased dietary restriction. Positive religious coping was associated with decreased likelihood for weight gain in Latinas. Implications for both caregivers and clinicians are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Religious/spiritual methods of coping can have a dramatic impact on psychological, social, and physical functioning (Koenig et al. 1992; Oxman et al. 1995) and can be instrumental in helping individuals to deal with, and find meaning in, stressful life events (e.g., Greene-Bush et al. 1999; Tix and Frazier 1998). Indeed, the benefits of religious coping have been well documented in multiple demographic groups to include family caregivers (Kaye and Robinson 1994; Stolley et al. 1999). Nevertheless, the relationship between religious coping and health behaviors in dementia caregivers has been minimally explored. The aim of the current study was to explore the degree to which religious coping was associated with health behavior patterns in a sample of female caregivers of elderly relatives with dementia.
Caregivers of dementia patients are vulnerable to a host of potential health decrements (Pinquart and Sorenson 2003; Schulz et al. 1995; Vitaliano et al. 1997). Caregiver health behaviors have been posited to be a primary mechanism by which caregiving stressors affect health (Vitaliano et al. 2003), and a growing body of literature has documented an association between dementia caregiving and health risk behaviors (Burton et al. 1997; Connell 1994; Connell et al. 2001; Gallant and Connell 1997). Not only do poor caregiver health behaviors have a significant impact on the physiological health of caregivers, they may undermine a caregiver’s ability to adequately care for his/her loved one (Cohen et al. 1993; Harper and Lund 1990; Lieberman and Kramer 1991; McFall and Miller 1992). Thus, identifying resources, such as religious coping, which enable caregivers to negotiate the stress of caregiving and that protect against health decline, is an extremely important public health undertaking.
Religion and spirituality have long been viewed as protective factors against negative mental health outcomes in the general population (George et al. 2002). Furthermore, research has demonstrated a strong association between religion and positive outcomes in dementia caregivers. For example, in a study of 1,299 caregivers, Hebert et al. (2007) found that organizational religiosity (i.e., church attendance) was inversely associated with depression and complicated grief. A separate study found that increases in religiosity and spiritual support were associated with lower incidences of depression as well as increased self-esteem and self-care (Murray-Swank et al. 2006).
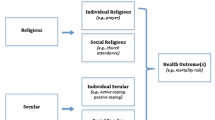
With regard to physical health, it has been posited that religion exerts its influence indirectly by promoting positive health behaviors (e.g., self-care, healthy eating, exercise) and restricting negative health behaviors (e.g., smoking and drug use; Ellison and Levin 1998). Previous work by our laboratory examined this indirect relationship by exploring the degree to which religiosity influences the health behavior patterns of dementia caregivers. Our findings revealed that the pathway between religiosity and health is differentially influenced by various dimensions of religiosity and moderated by ethnicity (Rabinowitz et al. 2009). The objective of the current research was to expand upon the previous study by exploring whether religious coping, a construct distinct from religiosity, is also significantly associated with cumulative health risk and health behavior patterns. The overarching aim was to ascertain whether behavioral and cognitive coping mechanisms tied to spirituality were significantly related to health behavior patterns in a sample of Caucasian and Latina dementia caregivers and determine whether this relationship was moderated by ethnicity.
Religious coping can be defined as one’s search for significance in difficult life events through religious or spiritual means (Pargament 1997). Methods of religious/spiritual coping differentiate themselves from religiosity (e.g., frequency of prayer, frequency of service attendance, or the subjective importance of religion), in that they are predictive of outcomes even when controlling for dimensions of religiosity (Pargament 1997). Conversely, measures of religiosity have not been found to be predictive of adjustment to life crises after controlling for the effects of religious coping (Pargament 1997). Thus, while tied to religiosity, religious coping must be conceptualized as a related but separate construct (Pargament et al. 1988). Religious coping is distinct not only from religiosity, but also from other non-religious coping mechanisms. Indeed, religious/spiritual coping has been found to predict outcomes even while controlling for the effects of non-religious coping mechanisms (Pargament and Koenig 1997).
Religious coping is a multidimensional construct that can have both positive and negative effects on outcomes (Pargament 1997). Positive religious coping involves viewing religion and spirituality as being of great support and has been linked to improved physical and psychological outcomes in response to significant external stressors (e.g., “I think of my life as part of a larger spiritual force”, Pargament 1997). Conversely, negative religious coping involves feeling alienated or in conflict with god as a consequence of dealing with stressful life events (Pargament 1997). In many but not all cases, such coping has been associated with negative outcomes in cross-sectional research (e.g., “I wonder whether god has abandoned me”, Pargament 1997).
In the general population, religious coping has been associated with numerous physiological benefits including decreased heart disease, lower rates of stroke, lower mortality rate, and more positive health habits (Seybold and Hill 2001). Although dementia caregivers have been shown to rely increasingly on religious coping as the care recipient’s health declines (Salts et al. 1991; Skaff 1995), comparatively little is known about the relationship between religious coping and health behavior patterns in dementia caregivers.
Although studies have investigated religious coping among caregivers from different ethnic groups, the findings have tended to be equivocal (Haley et al. 1996; Nac/AARP 1997). With regard to Latina caregivers, only a handful of studies on religious coping are extant. Virtually, none examine ethnicity as a moderator variable. Of the studies on religious coping in Latina caregivers, many focus on the potential importance of religiosity, religious coping, spirituality and faith in the conceptualization of disease, and the management of family caregiving among Latino families (e.g., Calderon and Tennstedt 1998; Gallagher-Thompson et al. 1996, 2000). In addition, Latina caregivers have been observed to engage in more religious coping (Coon et al. 2004) and use positive religious coping at a significantly higher rate than their Caucasian counterparts (Mausbach et al. 2003). The extent to which this difference in religious coping affects outcomes such as health behavior patterns has yet to be explored in the caregiving literature.
The current study examined the relationship between religious coping and caregiver cumulative health risk as determined by health behavior patterns in a multicultural sample of female caregivers of elderly relatives with dementia. It was hypothesized that the high levels of positive religious coping would be significantly associated with reduced cumulative health risk as determined by health behavior patterns. Conversely, the high levels of negative religious coping were posited to be associated with increased cumulative health risk. A moderator model was used to ascertain whether ethnicity moderated the relationship between religious coping and cumulative health risk. Exploratory analyses examined the relationship between religious coping and the individual health behaviors that comprised the cumulative health index.
Methods
Participants
Two hundred and fifty-six female caregivers of elderly relatives with significant memory problems were recruited from the community as part of the Palo Alto site of the National REACH (Resources for Enhancing Alzheimer’s Caregiver Health). Women were targeted for inclusion because prior research indicates significant gender differences in response to caregiving (reviewed in Lauderdale and Gallagher-Thompson 2002). Special efforts were made to identify organizations within the Latino community. Key recruitment sites included local diagnostic centers, local Alzheimer’s Association chapters, adult day care programs, Alzheimer’s day care programs, caregiver resource centers, and local senior centers serving the Latino communities. Strategies included the establishment of a community advisory board, staff presentations on a variety of aging and caregiving topics at community agencies, and media advertisement in both Spanish and English. (For additional information on REACH recruitment and retention strategies, see Gallagher-Thompson and Arean 2000; Wisniewski et al. 2003).
The national REACH project developed a standardized telephone-screening tool based on a common set of inclusion/exclusion criteria designed to identify an appropriately diverse yet well-defined target population. Study participants had to be adult caregivers of at least 21 years of age who lived with, and provided four or more hours of care to, family members requiring assistance with at least two instrumental activities of daily living (IADL) or one activity of daily living (ADL) (Katz et al. 1963; Lawton and Brody 1969). Participants must have been in the caregiving role at least 6 months, available by telephone, and planning to stay in the area for the study’s duration. The care recipients needed to have either a physician’s diagnosis of dementia or a recent mini-mental state examination (MMSE) score less than or equal to 23 out of 30 (Folstein et al. 1975).
The majority of REACH sites added entry criteria relevant to site-specific hypotheses. In California, REACH caregivers also had to be female and self-identify as Anglo or Latina. For the care recipients, when a clinical diagnosis of dementia was not available, the results of baseline MMSE, ADL, IADL, and Revised Memory Behavior Problem Checklist (Teri et al. 1992) scores had to be consistent with a diagnosis of dementia as determined by the project geropsychiatrist. Further details are available elsewhere (Wisniewski et al. 2003).
Measures
Demographic Characteristics
The following demographic data pertinent to the current study were gathered: caregiver age, years of formal education, years of caregiving, household income, marital status, employment status, and relationship to family member with memory loss.
Care Recipient Health
At baseline, caregivers were asked to rate care recipient’s physical health exclusive of memory problems and confusion associated with ADRD. Scores ranged from one to five [lower scores indicated poorer physical health (1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent)].
Religious Coping
The long form of the brief religious coping scale (BRCOPE; Pargament 1999) was used to assess religious coping. The long form of the measure consists of 2 subscales of 5 items each, designed to measure positive (e.g., “Tried to find a lesson from God in this”, “Looked to God for strength, support, and guidance in this”), and negative (e.g., “Wondered whether God had abandoned us”, “Felt that my relative’s dementia was God’s way of punishing me for my sins and my lack of spirituality”) religious coping, respectively. Response options ranged from 0 = Not at all to 3 = A great deal. Because the current study was focused on a situational rather than the dispositional assessment of religious coping, instructions were modified to ask to what extent over the last month the respondent used each strategy in coping with her relative’s dementia. The overall Cronbach’s alpha for the scale was 0.85.
Religiosity
Participants were assessed using single-item global religiosity measures (GRMs), which included the following three questions: a) “How often do you usually attend religious services, meetings and/or activities?”(i.e., organizational religiosity), “How often do you pray or meditate?” (i.e., non-organizational religiosity), and “How important is your spirituality or religious faith to you?” (i.e., subjective religiosity). Response options for frequency of attendance and prayer were 1 = Never, 2 = Once a year, 3 = A few times a year, 4 = At least once a month, 5 = At least once a week, and 6 = Nearly every day. Response options for the importance of religion were 1 = Not important, 2 = Somewhat important, 3 = Important, and 4 = Very important.
Caregiver Health Behaviors
Five health behaviors (smoking, alcohol consumption, weight maintenance, exercise, and diet) were measured as part of the REACH baseline interview with items adapted from the Nutrition Screening Initiative (NSI), which was sponsored by the American Academy of Family Physicians and the American Dietetic Association (Posner et al. 1993). Three items (“Do you eat fewer than 2 meals per day”, “Do you consume three or more alcoholic drinks per day”, and “Have you gained six pounds in the last six months”) were taken directly from the NSI. Two additional items were added by the REACH coordinating center. The first addressed routine engagement in vigorous exercise, “Do you do vigorous exercises for 15–30 min or more at least three times a week?” The second evaluated smoking habits, “Do you smoke cigarettes now?”
Responses to all five items were dichotomous (0 = no, 1 = yes) and are summed to form a 5-point scale where zero indicated low cumulative health risk and five indicated high cumulative risk. Exercise was reverse coded when creating the cumulative health risk scale in order to reflect it being a positive health behavior. This scale was previously used in a cross-site study from the National REACH project examining coping, appraisals, and well being in Caucasian and Latina caregivers (Coon et al. 2004).
Data Analysis
Data Preparation
Preliminary data screening was conducted prior to running the primary analyses. Little MCAR’s test was utilized to conduct missing value analysis, and the results confirmed that data were missing completely at random (χ 2 = 20.95, df = 20, P = 0.46). Additionally, no study variables contained more than 3% missing values.
Multivariate outliers were examined by calculating the Mahalnobis distance of multivariate residuals of all predictor variables (Tabachnick and Fidell 1996). Using a conservative alpha of 0.001 for 8 degrees of freedom (determined by the number of study variables), any distance that exceeded the χ2 critical value of 26.125 was considered a multivariate outlier. No cases met this criterion (the greatest observed distance was 24.74).
The distribution of data was evaluated by visual inspection and by calculating skewness statistics and standard errors. Skewness statistics were divided by the corresponding standard error in order to derive a z-score. Any z-score with an absolute value greater than “2.0” was considered to have a skewed distribution. Negative religious coping was observed to have a positively skewed distribution and was transformed using square root transformation.
Primary Analyses
A multiple linear regression approach was used to test the a priori hypotheses. Prior to conducting the analyses, all continuous predictor variables were centered at the mean by subtracting the grand mean from the individual scores. As indicated by Kraemer and Blasey (2004), centering data serve to diminish problems resulting from multicollinearity while increasing both the precision of parameter estimation and the power of statistical testing of those parameters. Ethnicity was contrast coded ‘0.5’ and ‘−0.5’. To assess for moderator effects for ethnicity, two interaction terms were created by multiplying the two religious coping variables by the dichotomously coded ethnicity variable (Holmbeck 2002).
Ethnicity, the two religious coping variables, and the two interaction terms were entered as independent variables into the regression equation. Cumulative health risk served as the dependent variable. Age and care recipient health status were entered into the regression equation as covariates because, in a previous study using the same sample, they were observed to be significant predictors of cumulative health risk associated with health behavior patterns (Rabinowitz et al. 2007). Furthermore, because age is highly correlated with education, it served as a proxy variable for education without adding a highly collinear variable into the regression equation. Care recipient physical health was entered as a covariate in order to control for variability in objective stress associated with caregiving and in provision of care. In Rabinowitz et al. (2007), both MMSE and total IADL/ADL’s provided by the caregiver were also used for this purpose, but only care recipient physical health was significant in the overall model.
Significant main effects in the anticipated direction would confirm the a priori hypothesis. Significant interaction effects would provide evidence of a moderating effect for ethnicity (Holmbeck 2002). In order to explore the nature of any significant interactions, post hoc probing using simple slopes was conducted according to the procedures outlined by Holmbeck (2002).
Exploratory Analyses
Binary logistic regressions were utilized to explore the relationship between religious coping and the individual health behaviors subsumed in the cumulative health risk index. The distribution of data was evaluated for each health behavior variable in order to ensure that the data met requisite assumptions. The variable assessing drinking (i.e., drinking more than two drinks per day) was found to have an extremely skewed distribution of yes/no responses with only 3 participants in the whole sample (and no Latinas) endorsing the behavior (see Table 1), and thus, it was not included in the analysis. It has also been recommended that, in order to achieve reliable parameter estimates, there be at least 10 events per parameter in the model for the smaller of the classes of the dependent variable (Peduzzi et al. 1996). Smoking did not meet this standard and thus, it too was not included in the exploratory analyses. The same predictors used in the primary analysis were regressed on the following dependent variables: a) dietary restriction, b) weight gain, and c) exercising. As in the primary analyses, significant interactions were evaluated according to the procedures delineated by Holmbeck (2002).
Results
Descriptive Data
Descriptive statistics were calculated for demographic and study variables. Differences across ethnicity on continuous variables were examined with t-tests for independent samples. Chi-square tests were utilized to assess ethnic differences on categorical variables. Results of these analyses, along with descriptive data, are presented in Table 1.
Religious Coping
Positive religious coping was the predominant coping mechanism identified by the sample. The mean positive religious coping score was 8.64 in contrast to a mean of only 1.6 for negative religious coping. Significant ethnic differences emerged on positive religious coping (t = 9.70, P < 0.01) with Latinas endorsing more positive religious coping (M = 11.43) than their Caucasian counterparts (M = 6.54). There were no significant ethnic differences in negative religious coping.
Religiosity
Statistically significant differences were observed between Caucasians and Latinas across all three domains assessed. Latinas consistently reported more religiosity than Caucasians (subjective: t = −3.18, P < 0.01, 3.60 vs. 3.22; non-organizational: t = −4.04, P < 0.001, 5.71 vs. 4.99; organizational: t = −5.22, P < 0.001, 4.04 vs. 3.0).
Health Characteristics
The sample reported being in good overall health as 64.91% of caregivers rated their health between good and excellent. The mean cumulative health risk index score for the entire sample was 1.28. In terms of health behaviors, 92.8% of caregivers did not smoke, 98.86% did not drink, and over 30% (32.2%) engaged in vigorous exercise at least twice a week. Further, 38.6% of the caregivers reported having gained more than ten pounds in the preceding 6 months, and 15.15% reported eating fewer than 2 meals per day. Latina caregivers were significantly more likely than Caucasians to eat less than two meals per day (χ 2 = 4.86 P = 0.02) and experience recent weight gain (χ 2 = 6.42 P = 0.04).
Of the health conditions reported by the caregivers, high blood pressure was the most common with over 30.3% endorsing this condition. Only 8.33% of caregivers reported diabetes, 14.02% reported a diagnosed heart condition, and 4.6% of the caregivers had a history of a stroke. Caucasian caregivers had a significantly higher rate of heart conditions (χ 2 = 7.71, P = 0.02) and cancer (χ 2 = 4.36, P = 0.04) than Latinas, but Latinas were significantly more likely to have diabetes (χ 2 = 9.53, P < 0.01).
Primary Analyses
It was hypothesized that positive religious coping would be significantly associated with reduced cumulative health risk, and negative religious coping was posited to be associated with increased cumulative health risk. Multiple linear regression was used to test these a priori hypotheses. With all predictors entered in the regression equation, the overall model was significant (F [264, 7] = 6.09, P < 0.001) and accounted for 15% of the variance in cumulative health risk (R 2 = 0.15). After controlling for age and care recipient health status, there was a significant main effect for negative religious coping (t = 2.49, P = 0.01), with increased negative religious coping being associated with increased cumulative health risk. A significant interaction emerged between positive religious coping and ethnicity (t = 1.94, P = 0.05), indicating the presence of a moderating effect for ethnicity (Table 2).
Post Hoc Probing
To explore the moderating effect for ethnicity, post hoc probing using simple slopes was conducted according to the procedures delineated by Holmbeck (2002). In these analyses, positive religious coping was found to be significantly associated with reduced cumulative health risk among Latina caregivers (t = −2.64, P = 0.01), but not among Caucasians (t = 0.04, P = 0.45).
Secondary Analyses
Binary logistic regressions were utilized to explore the relationship between religious coping and the individual health behaviors subsumed in the cumulative health risk scale for which there was a reasonable distribution of responses. These variables were a) weight gain, b) dietary restriction, and c) exercising.
Weight Gain
The omnibus test of coefficients (which may be interpreted as a test of how well predictors in the model jointly predict the dependent variable) for the model predicting dietary restriction (eating fewer than 2 meals per day) was significant (χ 2 = 40.811, df = 7, P < 0.001), suggesting that the model was a good fit for the data. The Nagelkerke’s R 2 value (which serves as an approximation of OLS R 2 values and provides an estimate of the amount of variance in the dependent variable accounted for by the model) for the model was 0.20.
After controlling for age and care recipient health status, significant main effects were observed for positive religious coping (B (unstandardized regression coefficient) = −0.1, Wald = 5.33, P = 0.02), with increased positive religious coping being associated with a reduced likelihood for weight gain, and for negative religious coping (B = 0.18, Wald = 7.46, P = 0.01), with increased negative religiosity being significantly associated with increased weight gain. A significant interaction was observed for ethnicity and positive religious coping (B = 0.21, Wald = 6.44, P = 0.01). Post hoc probing of the significant interaction revealed that positive religious coping was significantly associated with a reduced likelihood for weight gain among Latinas (B = −0.22, Wald = 8.27, P = 0.01), but not among Caucasians (B = 0.01, Wald = 0.07, P = 0.77).
Dietary Restriction
The omnibus test of coefficients for the model predicting dietary restriction was significant (χ 2 = 33.02, df = 7, P < 0.001), suggesting that the model was a good fit for the data. The Nagelkerke’s R 2 value was 0.21. A significant main effect was observed for negative religious coping (B = 0.24, Wald = 9.81, P < 0.01), with increased negative religious coping being associated with increased dietary restriction. There were no significant interactions.
Discussion
The current study examined the degree to which both positive and negative religious coping were associated with health behavior patterns in a multicultural sample of female caregivers of elderly relatives with dementia. It was hypothesized that positive religious coping would be related to reduced cumulative health risk. Conversely, negative religious coping was posited to be significantly related to increased cumulative health risk. Analyses were run on both a cumulative health risk index and on the individual health behaviors subsumed in the overarching index. Moderator analyses were also conducted to explore a moderating effect for ethnicity on the relationships between religious coping and health behavior patterns.
Overall, the findings suggest that negative and positive religious coping have a differential effect on health behavior patterns with positive religious coping being moderated by ethnicity. Specifically, negative religious coping was significantly associated with increased cumulative health risk whereas positive religious coping was significantly related to decreased cumulative health risk among Latina caregivers but not among Caucasians. The findings for negative religious coping were consistent with previous studies linking negative religious coping to poor outcomes in response to tragedy (Koenig et al. 1998; Pargament et al. 2004). With respect to individual health behaviors, negative religious coping highly influenced dietary practices in that it was significantly associated with both an increased likelihood for weight gain and increased dietary restriction. Positive religious coping was related to improved dietary practices among Latinas for whom it was also associated with decreased likelihood for weight gain.
An important aspect of the findings is that health behavior patterns were predicated on the type of religious coping utilized. Stated differently, it was not a matter of whether a caregiver used religion to cope with caregiver stress but rather, how a caregiver used religion to cope, which influenced health behavior patterns. These findings lend support to the notion that religious coping is a multifaceted construct comprised of both positive and negative dimensions that exert a unique and sometimes independent effect on outcomes. The implication is that when exploring religion as a resource, clinicians and researchers should not only differentiate between religiosity and religious coping, but also further ascertain the type of religious coping used.
Although positive and negative religious copings are frequently used in conjunction with one another (Pargament 1997), an individual’s dominant style may afford insight into how individuals will respond to stress and the types of outcomes that they will experience. According to the current data, the subset of individuals who are likely to use more negative religious coping may be at increased risk for poor health outcomes. These findings make it increasingly important to identify factors that are predictive of and contributory to a predominant use of negative religious coping in response to caregiving stressors.
Explanations for why someone may have a predilection to use negative rather than positive religious coping may be found in how an individual perceives his or her spiritual relationship with his or her higher power. Alternatively, negative religious coping may be a manifestation of underlying cognitive tendencies toward negative interpretation of difficult events more generally. For example, item content reflects a tendency to interpret adverse events as punishment from god. The process may be similar to that described in cognitive theories of depression where depressed individuals interpret life experiences in a distorted, negative manner. Thus, individuals with a tendency to engage in cognitive distortions may also be inclined to apply a negative heuristic to religion when confronted with exogenous stressors. To this point, a Spanish study found an association between depression and religiosity in children caregivers, while spousal caregivers displayed a negative relationship between the two (Zunzunegui et al. 1999). An examination of religious coping and cognitive styles may provide further insight into the complex interplay between factors implicit in caregiving and health outcomes. Future studies may benefit from exploring the relationship between depressogenic cognitive styles and the prevalence of negative religious coping.
The moderating effect for ethnicity may be attributable to culturally predicated views regarding the nature and the importance of religion, and in turn, the manner in which religious coping is used across ethnicity. Indeed, the literature describes a significant heterogeneity in the degree to which religious coping affects groups of individuals. For example, Pargament (1997) explains that religious coping may have a more salutary effect among groups with limited access to secular resources and traditional bases of power. This dynamic seems to be borne out in the present study, as positive religious coping was significantly associated with reduced cumulative health risk among Latinas caregivers, who were significantly more likely than Caucasian caregivers to have an income below $20,000 (t = 23.29, P < 0.001), but not among their Caucasian caregiver counterparts. Thus, positive religious coping may be a valuable resource for Latina caregivers that can be drawn upon during times of stress. Further, positive religious coping may be used in a therapeutic setting to help clients negotiate crises and persistent stressors like caregiving.
Additionally, religious coping has been observed to be more helpful in groups for whom religion is most important in their lives (Pargament 1997). This was exemplified in the current study. Latinas, who have been shown in previous studies using the same sample of caregivers to have higher levels of religiosity (Mausbach et al. 2003), were more likely to derive benefit from positive religious coping. Interestingly, it has been demonstrated that increased acculturation in Latina caregivers often results in decreased levels of religious coping (Mausbach et al. 2003). For Latinas who adopt certain aspects of Caucasian culture, religion may, as a result, become comparatively deemphasized. Thus, clinicians should consider acculturation levels when exploring ethnic differences in religious coping as a caregiver resource.
Latinas’ approaches to the caregiving process and role may also be explanatory. For instance, finding meaning in the caregiving process has been associated with the decreased perception of burden or caregiver strain as well as with better health outcomes (Toseland and Smith 2001). It is possible that positive religious coping may relate to meaning-finding, and thus, caregivers who engage in more positive religious coping may benefit from higher levels of meaning-finding and stress related growth. Conversely, a previous study found that caregivers who felt distant or angry with god reported increases in perceived burden (Shah et al. 2001). These findings speak to the need for further investigation into additional variables involved in coping with the caregiving process such as acculturation, perceived burden, appraisals, and meaning-finding.
The current findings should be interpreted in light of certain study limitations to include the gender, ethnic, and geographic characteristics of the sample. First, gender differences could not be assessed because this study limited its sample to female caregivers. Furthermore, participants were recruited from only one region of the US, making it difficult to generalize these results to caregivers from other geographic locales. It is entirely possible that the findings for Latinas in the current study may not hold for Latino caregivers who live outside of Northern California or in areas where access to information and resources in Spanish is even more limited. Finally, a cross-sectional design was utilized and as such, causality could not be inferred and longitudinal changes in religious coping and health behaviors could not be assessed.
Future studies should explore factors that predict the use of negative religious coping so that individuals who may overly rely on such coping mechanisms can be identified. A mediation model may afford insight into whether religious coping exerts its effect on health outcomes directly or via other variables. Of interest would be the degree to which religious coping influences both mood and perceived burden among caregivers, and how these mediating variables may influence health behavior patterns.
Overall, the current study highlights the importance of examining a caregiver’s religious coping style in order to better understand the relationship between spirituality and health. Consistent with previous literature in which positive and negative religious coping were observed to differentially influence outcomes (e.g., Pargament 1997), the current study demonstrates that positive and negative religious coping differentially impact cumulative health risk associated with health behavior patterns in dementia caregivers. Moreover, the findings demonstrate that the relationship between positive religious coping and health behaviors may be moderated by ethnicity. The findings underscore the importance of collaboration between religious leaders, clinicians, and researchers in developing and providing appropriate education and interventions.
References
Burton, L., Newsom, J., Schulz, R., Hirsch, C., & German, P. (1997). Preventative health behaviors among spousal caregivers. Preventative Medicine, 26, 162–169.
Calderon, V., & Tennstedt, S. L. (1998). Ethnic differences in the expression of caregiver burden: Results of a qualitative study. Journal of Gerontological Social Work, 30, 159–178.
Cohen, C. A., Gold, D. P., Shulman, K. I., Wortley, J. T., McDonald, G., & Wargon, M. (1993). Factors determining the decision to institutionalize dementing individuals: A prospective study. The Gerontologist, 33, 714–720.
Connell, C. M. (1994). The impact of spouse caregiving on health behaviors and physical and mental health status. The American Journal of Alzheimer’s Care and Related Disorders and Research, 12, 26–36.
Connell, C. M., Janevic, M. R., & Gallant, M. P. (2001). The costs of caring: Impact of dementia on family caregivers. Journal of Geriatric Psychiatry and Neurology, 14, 179.
Coon, D. W., Rubert, M., Solano, N., Mausbach, B., Kraemer, H., Arguëlles, et al. (2004). Well-being, appraisal, and coping in Latina and Caucasian female dementia caregivers: Findings from the REACH study. Aging & Mental Health, 8(4), 330–345.
Ellison, C. G., & Levin, J. S. (1998). The religion-health connection: Evidence, theory, and future directions. Special Issue: Public Health and Health Education in Faith Communities, 25(6), 700–720.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Gallagher-Thompson, D., & Arean, P. (2000). Development and implementation of intervention strategies for culturally diverse caregiving populations. In R. Schulz, et al. (Eds.), Handbook on dementia caregiving (pp. 151–185). New York: Springer.
Gallagher-Thompson, D., Haynie, D., Takagi, K. A., Valverde, I., & Thompson, L. W. (2000). Impact of Alzheimer’s disease education programs: Focus on hispanic families. Gerontology and Geriatrics Education, 20, 25–40.
Gallagher-Thompson, D., Talamantes, M., Ramirez, R., & Valverde, I. (1996). Service delivery issues and recommendations for working with Mexican–American family caregivers. In G. Yeo & D. Gallagher-Thompson (Eds.), Ethnicity and the dementias (pp. 137–152). Philadelphia: Taylor and Francis.
Gallant, M. P., & Connell, C. M. (1997). Predictors of decreased self-care among spouse caregivers of older adults with dementing illnesses. Journal of Aging Health, 9, 373–395.
George, L. K., Ellison, C. G., & Larson, D. B. (2002). Explaining the relationship between religious involvement and health. Psychological Inquiry, 13(3), 190–200.
Greene-Bush, E., Rye, M. S., Brant, C. R., Emery, E., Pargament, K. I., & Riessinger, C. A. (1999). Religious coping with chronic pain. Applied psychophysiology and biofeedback, 24, 249–260.
Haley, W. E., Roth, D. L., Coletin, M. I., Ford, G. R., West, C. A. C., Collins, R. P., et al. (1996). Appraisal, coping, and social support as mediators of well-being in Black and White family caregivers of patients with Alzheimer’s disease. Journal of Consulting and Clinical Psychology, 64, 121–129.
Harper, S., & Lund, D. A. (1990). Wives, husbands, and daughters caring for institutionalized and noninstitutionalized dementia patients: Toward a model of caregiver burden. International Journal of Aging and Human Development, 30(4), 241–262.
Hebert, R. S., Dang, Q., & Schulz, R. (2007). Religious beliefs and practices are associated with better mental health in family caregivers of patients with dementia: Findings from the REACH study. American Journal of Geriatric Psychiatry, 15(4), 292–300.
Holmbeck, G. N. (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27(1), 87–96.
Katz, S., Ford, A. B., Moskowitz, R. W., Jackson, B. A., & Jaffee, M. W. (1963). Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association, 185, 914–919.
Kaye, J., & Robinson, K. M. (1994). Spirituality among caregivers. IMAGE: Journal of Nursing Scholarship, 26, 218–221.
Koenig, H. G., Cohen, H. J., Blazer, F. H., Pieper, C., Meador, K. G., Shelp, F., et al. (1992). Religious coping and depression among elderly hospitalized medically ill men. American Journal of Psychiatry, 149, 1693–1700.
Koenig, H. G., Pargament, K. I., & Nielsen, J. (1998). Religious coping and mental health outcomes in medically ill hospitalized older adults. Journal of Nervous and Mental Diseases, 186, 513–521.
Kraemer, H. C., & Blasey, C. M. (2004). Centering in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research, 13, 141–151.
Lauderdale, S., & Gallagher-Thompson, D. (2002). Men providing care: What do they need and how can we do it? Clinical Gerontologist, 26(1/2), 53–70.
Lawton, M. P., & Brody, E. (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9, 179–186.
Lieberman, M. A., & Kramer, J. H. (1991). Factors affecting decisions to institutionalize demented elderly. The Gerontologist, 31(3), 371–374.
Mausbach, B. T., Coon, D. W., Cardenas, V., & Thompson, L. W. (2003). Religious coping among Caucasian and Latina dementia caregivers. Journal of Mental Health and Aging, 9(2), 97–110.
McFall, S., & Miller, B. (1992). Caregiver burden and nursing home admission of frail elderly persons. Journal of Gerontology, 47(2), S73–S79.
Murray-Swank, A. B., Lucksted, A., Medoff, D. R., Yang, Y., Wohlheiter, K., & Dixon, L. B. (2006). Religiosity, psychosocial adjustment, and subjective burden of persons who care for those with mental illness. Psychiatric Services, 57(3), 361–365.
National Alliance for Caregiving/American Association of Retired Persons. (1997). Family caregiving in the U.S.: Findings from a national survey.
Oxman, T. E., Freeman, D. H., & Manheimer, E. D. (1995). Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosomatic Medicine, 57, 5–15.
Pargament, K. I. (1997). The psychology of religion and coping: Theory, research, and practice. New York: Guilford.
Pargament, K. I. (1999). Religious/spiritual coping. In Multidimensional measurements of religiousness/spirituality for use in health research: A report of the Fetzer Institute/National Institute on Aging Working Group.
Pargament, K. I., Kennell, J., Hathaway, W., Grevengoed, N., Newman, J., & Jones, W. (1988). Religion and the problem-solving process: Three styles of coping. Journal for the Scientific Study of Religion, 27(1), 90–104.
Pargament, K. I., & Koenig, H. G. (1997). A comprehensive measure of religious coping. Development and initial validation of the RCOPE. Report presented at: Retirement Research Foundation, Chicago, Ill.
Pargament, K. I., Koenig, H. G., Tarakeshwar, N., & Hahn, J. (2004). Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology, 9, 713–730.
Peduzzi, P. N., Concato, J., Kemper, E., Holford, T. R., & Feinstein, A. R. (1996). A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology, 49, 1373–1379.
Pinquart, M., & Sorenson, S. (2003). Differences between caregivers and non-caregivers in psychological health and physical health: A meta-analysis. Psychology and Aging, 18, 250–267.
Posner, B. M., Jette, A. M., Smith, K. W., & Miller, D. R. (1993). Nutrition and health risks in the elderly: The nutrition screening initiative. American Journal of Public Health, 83, 972–978.
Rabinowitz, Y. G., Mausbach, B. T., Atkinson, P. J., & Gallagher-Thompson, D. (2009). The relationship between religiosity and health behaviors in female caregivers of older adults with dementia. Aging and Mental Health, 13(6), 788–798.
Rabinowitz, Y. G., Mausbach, B. T., Thompson, L. W., & Gallagher-Thompson, D. (2007). The relationship between self-efficacy and cumulative health risk associated with health behavior patterns in female caregivers of elderly relatives with Alzheimer’s dementia. Journal of Aging and Health, 19(6), 946–964.
Salts, C. J., Denham, T. E., & Smith, T. A., Jr. (1991). Relationship patterns and role of religion in elderly couples with chronic illness. Journal of Religious Gerontology, 7, 41–54.
Schulz, R., O’Brien, A. T., Bookwala, J., & Fleissner, K. (1995). Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist, 35, 771–791.
Seybold, K. S., & Hill, P. C. (2001). The role of religion and spirituality in mental and physical health. Current Directions in Psychological Science, 10, 21–24.
Shah, A. A., Snow, A. L., & Kunik, M. E. (2001). Spiritual and religious coping in caregivers of patients with Alzheimer’s disease. Clinical Gerontologist, 24(3–4), 127–136.
Skaff, M. (1995). Religion in the stress process: Coping with caregiving. Paper presented at the Annual Scientific Meeting of the Gerontological Society of America, Los Angeles, CA.
Stolley, J. M., Buckwalter, J. C., & Koenig, H. G. (1999). Prayer and religious coping for caregivers of person’s with Alzheimer’s disease and related disorders. American Journal of Alzheimer’s Disease, 14, 181–191.
Tabachnick, B. G., & Fidell, L. S. (1996). Using multivariate statistics. New York: Harper Collins.
Teri, L., Truax, P., Logsdon, R., Uomoto, J., Zarit, S., & Vitaliano, P. P. (1992). Assessment of behavioral problems in dementia: The revised memory and behavior problems checklist. Psychology and Aging, 7, 622–631.
Tix, A. P., & Frazier, P. A. (1998). The use of religious coping during stressful life events: Main effects, moderation, and mediation. Journal of Consulting and Clinical Psychology, 66(2), 411–422.
Toseland, R. W., & Smith, T. (2001). Supporting caregivers through education and training. Washington, DC: Administration on Aging, National Family Caregiver Support Program.
Vitaliano, P., Schulz, R., Kiecolt-Glaser, J., & Grant, I. (1997). Research on physiological and physical concomitants of caregiving: Where do we go from here? Annals of Behavioral Medicine, 19, 117–123.
Vitaliano, P., Zhang, J., & Scanlan, J. M. (2003). Is caregiving hazardous to one’s physical health? A meta-analysis. Psychology Bulletin, 129, 946–972.
Wisniewski, S. R., Belle, S. H., Coon, D. W., Marcus, S. M., Ory, M. G., Burgio, L., et al. (2003). The resources for enhancing Alzheimer’s caregiver health (REACH): Project design and baseline characteristics. Psychology and Aging, 18, 375–384.
Zunzunegui, M., Béland, F., Llácer, A., & Keller, I. (1999). Family, religion, and depressive symptoms in caregivers of disabled elderly. Journal of Epidemiology and Community Health, 53(6), 364–369.
Acknowledgments
Primary support for this research was provided by awards AG13289 by the National Institute on Aging (NIA). Additional support was provided by award AG23989 from the NIA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rabinowitz, Y.G., Hartlaub, M.G., Saenz, E.C. et al. Is Religious Coping Associated with Cumulative Health Risk? An Examination of Religious Coping Styles and Health Behavior Patterns in Alzheimer’s Dementia Caregivers. J Relig Health 49, 498–512 (2010). https://doi.org/10.1007/s10943-009-9300-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-009-9300-8