Abstract
Our objective was to expand our understanding of the predictors of Alzheimer’s disease (AD) progression to help design a clinical trial on a novel AD medication. We utilized the Coalition Against Major Diseases AD dataset consisting of control-arm data (both placebo and stable background AD medication) from 15 randomized double-blind clinical trials in mild-to-moderate AD patients (4,495 patients; July 2013). Our ADAS-cog longitudinal model incorporates a beta-regression with between-study, -subject, and -residual variability in NONMEM; it suggests that faster AD progression is associated with younger age and higher number of apolipoprotein E type 4 alleles (APOE*4), after accounting for baseline disease severity. APOE*4, in particular, seems to be implicated in the AD pathogenesis. In addition, patients who are already on stable background AD medications appear to have a faster progression relative to those who are not receiving AD medication. The current knowledge does not support a causality relationship between use of background AD medications and higher rate of disease progression, and the correlation is potentially due to confounding covariates. Although causality has not necessarily been demonstrated, this model can inform inclusion criteria and stratification, sample size, and trial duration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) remains the largest unmet medical need in neurology. AD is a progressive and lethal disease occurring in the brain, and is the 6th most common cause of death in the United States (US). More than 5 million Americans are living with AD. This number is estimated to virtually triple by 2050 with the aging of the “Baby Boomer” generation; as a consequence, the direct costs for care is expected to increase from $203 billion in 2013 to $1.2 trillion [1].
There is no available treatment to prevent, stop or slow the course of AD (i.e., disease-modifying therapies). Currently, four prescription drugs are available on the US market for AD symptomatic relief: donepezil, rivastigmine, galantamine (acetylcholinesterase inhibitors, AChEIs), and memantine (an N-methyl-d-aspartate receptor antagonist). Multiple AD-modifying therapies have failed in development due to several reasons including insufficient understanding of pathogenesis, diagnosis uncertainty, difficult selection of therapeutic targets, and non-optimal clinical trial design [2].
This analysis presents a potential tool to enhance clinical trial design from proof-of-concept through registration studies. A disease-drug-trial model is a useful tool to aid clinical study design by determining (1) the most responsive patient population to treatment, (2) the number of patients to be enrolled in the trial, (3) the trial duration and the optimal timing of response measurement, (4) the optimal outcome measure (e.g., different endpoints measuring different aspects of the disease, combinations of sub-items or composite endpoints), among others [3].
The Alzheimer’s disease assessment scale-cognitive subscale (ADAS-cog) is a widely used, validated measure of cognitive deterioration in clinical trials of patients with mild-to-moderate AD dementia [4], and several models have been developed to describe ADAS-cog. Holford et al. [5–7] in early 1990 s’ described the effect of tacrine in the cognitive function of approximately 2,500 patients with AD with a linear disease progression rate. In 2010, Ito et al. [8] conducted a summary-level model-based meta-analysis of 52 trials and 19,972 patients with mild-to-moderate AD; this analysis employed a linear model for disease progression and rate of progression was a function of the disease severity. Subsequently, Ito et al. [9] performed a patient-level model-based meta-analysis of 817 patients from the Alzheimer’s Disease Neuroimaging Initiative (ADNI); that analysis identified individual covariates influencing changes in the ADAS-cog score predicting curvilinear disease progression rate: age, sex, apolipoprotein E type 4 allele (APOE*4) carrier/non-carrier [10], and baseline disease severity. In 2011, Yang et al. [11] used an exponential model to describe the rate of cognitive decline in patients from the ADNI database (193 patients with AD and 397 patients with mild cognitive impairment); where synchronization method was developed to predict the disease progression timeline for each patient (i.e., the initial time represents the start of the cognitive decline instead of the time of enrollment in the ADNI trial) incorporating changes in cerebrospinal fluid and imaging biomarkers. In 2012, Samtani et al. [12] utilized a generalized logistic model to describe the non-linear rate of disease progression in 191 patients with AD from the ADNI database; this analysis evaluated wide range of covariates (e.g., imaging volumetric brain measures, serum biomarkers, and other baseline cognitive tests) and identified that the disease progression rate was influenced by age, total serum cholesterol, APOE*4 carrier/non-carrier, trail making test (part B) score, and ADAS-cog at each time point. In the same year, Rogers et al. [13] published a model-based meta-analysis incorporating beta regression (restricting predictions to the test range of 0–70) to describe the longitudinal progression of ADAS-cog with summary- and patient-level data; summary-level data was obtained from 73 published trials (representing 17,235 patients), and patient-level data was obtained from the ADNI (186 AD patients) and the Coalition Against Major Diseases (CAMD; 3,223 AD patients, data cut-off September 2010) databases. They improved prediction performance by using a generalized logistic function (via a logit transformation) along with beta-distributed residual variability and included an evaluation of APOE*4 with allele count.
The goal of the present analysis is to integrate aspects from the previously published mathematical models and expand our understanding of AD progression. To this end, we utilized an updated CAMD dataset consisting of control-arm data (both placebo and stable background AD medication) from randomized double-blind clinical trials in mild-to-moderate AD patients (4,495 patients; July 2013). We address three critical and relevant questions to the research community working on AD drug development:
-
1.
whether stable background AD medications influence disease progression,
-
2.
whether disease severity of enrolled patients has changed in recent years,
-
3.
whether the number of APOE*4 alleles have different magnitude of effect on disease progression.
For the first question, an exploratory analysis of the longitudinal ADAS-cog mean profile stratified by patients on placebo only versus patients on background AD medication suggests the influence of medication in ADAS-cog trajectory. In spite of all innovations implemented by the most recent publication on the CAMD data [13], the apparent effect of AD medication remains to be investigated. This is important given that 67 % of the patients in the CAMD database were taking at least one AD medication as background therapy. For the second question, we conducted an exploratory analysis on whether baseline disease severity has changed by trial year possibly due to changes in life style, awareness of the disease, diagnostics and patient care. For the third question, the current larger number of genotyped patients in the CAMD database allows for a reevaluation of the effect of the APOE*4 variant on rate of disease progression.
To our knowledge, this is the first time in the context of a non-linear mixed effect modeling of ADAS-cog meta-analysis that a beta-regression with between-study, -subject, and -residual variability has been implemented in NONMEM.
Methods
Data
Data from the CAMD database (with a cutoff in July 2013) was utilized in this analysis. CAMD is a public–private consortium led by the Critical Path Institute, which brings together government, regulatory agencies, academic institutions, pharmaceutical industry and non-profit research organizations. CAMD, launched in September of 2008, aims to advance new tools and methods to enhance the development of new AD and Parkinson’s disease therapies [14]. The consortium focuses on precompetitive sharing of patient-level data from control arms (both placebo and stable background AD medication) from randomized-controlled-trials in AD, conducted by pharmaceutical companies that are members of CAMD. The dataset included 4,495 patients with mild-to-moderate AD from 15 studies. The 11-item ADAS-cog (ADAS-cog11) used in this analysis was has been widely used as a primary endpoint in mild to moderate AD clinical trials, and the same algorithm has been used to derive ADAS-cog11 across clinical studies in the CAMD database. Missing ADAS-cog records or scores before placebo administration were excluded for this analysis. Available patient characteristics include age, sex, enrollment year in the trial, baseline mini-mental state examination (MMSE [15]), APOE*4 genotype (allele combinations), and background use of AD medication (donepezil, galantamine, rivastigmine, or memantine).
Model building process
The model building followed the steps outlined in Fig. 1. Data preparation and visualization were completed using R (version 3.0.2; Vienna, Austria [16]). Selection of the base model structure with incorporation of two levels of random effects (inter-individual and residual variability) preceded covariate model building and incorporation of a third level of random effects for study; finally, model performance was evaluated with goodness-of-fit and visual predictive checks.
Selection of the base model structure
Selection of the base model structure (summarized in Table 1) acknowledged the previously published ADAS-cog longitudinal models [5–9, 11–13] and used NONMEM® (version 7.3.0; Ellicott City, Maryland, USA [17]). The most recently published ADAS-cog longitudinal models utilized generalized logistic functions to describe the non-linear AD progression rate [12, 13]; as such, the Richard’s function with its analytical solution was tested [18] (Eq. 1).
where ADAScog0 is the population baseline ADAS-cog, r is the intrinsic rate of progression, t is time in years, β is the shape factor of the Richard’s function allowing for non-centrality of the inflection of disease progression rate, 70 is the maximum possible observed ADAS-cog score. Other literature models—linear, exponential and 2-parameter logistic models—were also tested for comparison.
Incorporation of three levels of random effects
Three levels of random variability were included in the final model: inter-study, inter-individual (patient) and residual variability. Inter-individual random effects were tested for baseline ADAS-cog (ADAScog0) and intrinsic rate of progression (r) parameters. Normally distributed inter-subject variability of the intrinsic rate of progression was estimated on the linear scale. This structure permitted that, at the patient-level, the cognitive function could capture improvement, decline or lack of change during the study. Log-normally distributed inter-subject variability was estimated for baseline ADAS-cog. This structure prevented the model from predicting nonsensical negative baseline scores at the patient-level. The same error structures were also utilized to account for inter-study variability in the intrinsic rate of progression and baseline ADAS-cog. The incorporation of inter-study variability, though, was only conducted in the final model building process (i.e., after the covariate model building) to minimize computational time.
where ADAScog0 is the population baseline ADAS-cog; ADAScog0ij is the individual baseline ADAS-cog; r is the population intrinsic rate of progression; rij is the individual intrinsic rate of progression; ηstudy is the inter-study random effect, \( \eta_{{{\text{baseline}}_{\text{i}} }}^{\text{study}} \sim {\text{N}}\left( {0, \omega_{\text{baseline,study}}^{2} } \right),\,\eta_{{{\text{intrinsic}}\;{\text{rate}}_{\text{i}} }}^{\text{study}} \sim {\text{N}}\left( {0, \omega_{{{\text{intrinsic}}\;{\text{rate}},\;{\text{study}}}}^{2} } \right); \) ηpatient is the inter-individual random effect, \( \eta_{{{\text{baseline}}_{\text{ij}} }}^{\text{patient}} \sim {\text{N}}\left( {0,\omega_{\text{baseline,patient}}^{2} } \right),\, \eta_{{{\text{intrinsic}}\;{\text{rate}}_{\text{ij}} }}^{\text{patient}} \sim N\left( {0,\omega_{{{\text{intrinsic}}\;{\text{rate,patient}}}}^{2} } \right). \)
Residual variability was assumed to be beta-distributed [13, 19, 20]. Because ADAS-cog is bounded between 0 and 70, the expectation for progression should be non-linear given the ceiling and floor effects; in addition, the error distribution should be heteroscedastic since the variance must approach zero as their mean approach the boundaries [19]. The combination of a logistic model with beta-distributed residuals, also known as beta regression, constrains the model predictions to the 0–70 range.
The probability density function of the beta distribution [20], with ADAS-cog score as the dependent variable is:
where \( ADAScog \in \left( {0,1} \right) \); α and β are shape parameters with α pulling the density toward 0 and β pulling the density toward 1, α > 0, β > 0; Γ(…) denotes the gamma function.
According to Eq. 4, the probability density function goes to zero if ADAS-cog equals 0 or 1 which explains why ADAS-cog must belong to the open unit interval (0,1). As a consequence the following transformation [20] of ADAS-cog was performed:
where n is the total sample size (n = 4,495); 0 is the lowest and 70 is the highest possible ADAS-cog score. The rationale for the above transformation is discussed in the supplemental material of Smithson and Verkuilen [20]. Assuming ADAS-cog~\( beta\left( {\alpha ,\beta } \right) \), then:
where μ is the expected value of the beta distribution; σ2 is the variance of the beta distribution; \( \tau = \alpha + \beta \). Therefore, the dispersion of the distribution is determined by μ and τ.
Within NONMEM, τ was estimated as a fixed effect parameter and μ corresponded to the individual ADAS-cog prediction. The shape parameters α and β were then calculated as below and substituted into Eq. 4:
Nemes’ approximation to the gamma function was incorporated in the model [19]:
where X represents α, β, or (α + β) in the probability density function (Eq. 4).
The NONMEM Laplacian estimation method was used to take into account the second derivative of the inter-individual variability parameters.
Covariate model building
Although age and MMSE may have undergone variation over time, we have considered only baseline values for modeling purpose. Only 6 of 15 studies had APOE*4 genotype information; for other studies, genotype was not performed or genetic data was not provided. APOE*4 was categorized as 0 (non-carrier), 1 (heterozygous), 2 (homozygous), and 3 (unknown). There were no missing values for the other covariates.
The selected base model structure (Richard’s function) intrinsically accounts for disease severity on the rate of progression (i.e., ADAS-cog score at a specific time point). MMSE was not included in the covariate model building because it is an alternative measure of cognitive impairment or disease severity. Similar to what was demonstrated by Ito et al. [8], baseline MMSE scores were highly correlated with baseline ADAS-cog scores (Fig. 2). In addition to the covariates reported in the literature, we investigated the effect of stable background AD medication and patient enrollment year in the trial.
Before performing the covariate model building, we examined the presence of correlation among the covariates of interest. Figure 3 shows that there was a correlation between the patient enrollment year in the trial (START) and APOE*4 genotype (APOE4) as well as use of AD medication (COMED). In trials before ~2001, APOE*4 genotyping was not performed and controls were not taking AD medication. For this reason, the patient enrollment year in the trial was not included in the covariate model building. Each covariate was tested as predictor of baseline ADAS-cog and intrinsic rate of progression using a stepwise covariate model building in Perl-speaks-NONMEM (PsN, version 3.5.4; Uppsala, Sweden [21]).
An exploratory analysis on how baseline disease severity changed from 1994 to 2008 was conducted and compared to literature data. The literature data (summary-level) from 1990 to 2008 was obtained from Ito et al. [8] and updated with studies through 2010. This updated dataset was used in the disease progression model by Rogers et al. [13].
Model selection criteria
Overall model selection was guided by objective function value (OFV, NONMEM version 7.3.0; Ellicott City, Maryland, USA [22]) and Akaike information criterion (AIC [23]) with a per-parameter (k) penalty of 6.635 (AIC = 6.635k + OFV, equivalent to χ2 with 1 df, P = 0.01). In addition, goodness-of-fit plots were generated. Ill-conditioning of the parameter space was assessed by inspecting the eigenvalues of the covariance matrix. The ratio of the largest to the smallest eigenvalue (i.e., condition number) was not to exceed 1,000.
Once the final model was identified, 500 datasets identical in structure and covariate values to the original dataset were simulated, using the parameter estimates from the final model to evaluate the model performance. The longitudinal ADAS-cog scores over time stratified by covariate were generated and visually compared with the observed data (visual predictive check, VPC) at each selected percentile (5th, 50th, 95th). The model was also run using the Markov chain Monte Carlo Bayesian estimation method to obtain confidence intervals for the parameter estimates.
Results
Data summary
Table 2 describes the patient characteristics stratified by study. Patients with mild and moderate stage of the disease were approximately equally distributed for the combined studies. From the 15 studies, 8 studies had control arms on stable AD medication (66.7 %). From the 42.8 % of the patients with known APOE*4 genotype across all studies, 42 % were non-carriers (0 alleles), 44 % were heterozygous (1 allele), and 14 % were homozygous (2 alleles) for this genetic variant which aligns with previous reports [24].
Base model selection
Base models were tested for each of the literature-reported model structures as described in the methods section with model forms, characteristics, and AIC presented in Table 1. Richard’s function, a 3-parameter or generalized logistic model (Eq. 1), was the most appropriate to describe AD progression over time as assessed by AIC. Richard’s function allowed for an asymmetric, inverted, concave relationship between disease progression rate and severity (Fig. 4). The parameter β allowed for asymmetry with respect to the inflection point which was estimated to occur at an ADAS-cog of ~52.
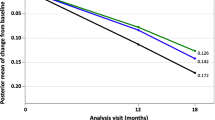
Final model
Richard’s function was utilized as the base model for the covariate model building. The final model parameter estimates are presented in Table 3. NONMEM code is presented in the Appendix. The identified covariates of baseline ADAS-cog were sex and APOE*4 genotype. Baseline ADAS-cog was lower for males when compared to females and increased with the number of APOE*4 alleles. The identified covariates of rate of progression were age, APOE*4 genotype and AD medication status. Patients who were younger, on stable background AD medication, and with more APOE*4 alleles had a higher rate of progression. The count of APOE*4 alleles (when known) showed a linear allelic effect on disease progression. In addition, the estimated average number of APOE*4 copies in patients with unknown genotype was very similar to the observed average number of copies in patients with known genotype (0.78 vs. 0.72, respectively). As consequence, we considered APOE*4 genotype as a continuous variable in the final model and imputed missing allele count as 0.72. Importantly, similar estimates were obtained for APOE*4 effect on both baseline and rate of progression when the model was run excluding patients with imputed genotype. The model-predicted average ADAS-cog progression stratified by covariates is presented in Fig. 5. Although patient enrollment year in the trial was not included in the covariate model building, Fig. 6a depicts patient enrollment year in the trial versus the baseline MMSE and shows that the baseline disease severity has only slightly changed from 1994 to 2008 (from approximately 19.5–20.7, P < 0.0001; based on the linear regression analysis in the individuals who were not on background AD medication). This finding is in agreement with the literature (summary-level) data presented in Fig. 6b.
Observed baseline disease severity over year. a Circles indicate each individual patient data, and line is the weighted linear regression. b Circles indicate mean values from each published trial, size of the circle is proportional to the number of patients in the trial, line is the weighted linear regression by number of patients in the trial, and shaded area is the standard error
Inter-individual variability was larger than inter-study variability. The inter-individual variability for baseline ADAS-cog was about twofold higher than that of the rate of progression (0.395 vs. 0.203, respectively). The inter-study variability was lower for both baseline ADAS-cog and rate of progression (0.099 vs. 0.026).
Evaluation of model performance
Model selection criteria suggest the appropriateness of the model in describing the longitudinal changes in ADAS-cog score. The residuals plots (Supplementary Figure S1) did not indicate a trend of the residuals versus the population predictions and time. The observed ADAS-cog scores versus individual predictions approximated the identity line; the same was not quite observed for population predictions, likely due to the skewness in ADAS-cog scores. Figure 7 shows the VPCs stratified by study, number of APOE*4 alleles and use of background AD medication. Most of the observed data lie within the 5th and 95th percentiles of the simulations, and the observed and predicted percentiles are similar indicating reasonable estimation. In addition, the condition number from the Laplacian estimation method was 473 and the final parameter values were estimated with good precision when utilizing the Markov chain Monte Carlo Bayesian estimation method, and shrinkage was minimal for inter-study, inter-individual, and residual variability (Table 3).
Visual Predictive Check (VPC) from N = 500 Simulations. Solid and dashed black lines are observed median, 5th and 95th percentiles, and shaded areas are corresponding predicted intervals from the final model. Horizontal red dashed line is ADAS-cog baseline (22.2) for an average patient with mild-to-moderate AD in the CAMD database. A difference variance structure was used for Study 1131 in which patients with milder AD were enrolled (Color figure online)
Discussion
This work utilized the accumulated knowledge on AD progression through the ADAS-cog longitudinal models available in the literature and expanded our understanding of the predictors of AD progression rate. In this analysis, we tested all model structures published previously [5–9, 11–13] and chose a generalized logistic function (i.e., Richard’s function) to describe changes in ADAS-cog over time for patients with mild-to-moderate AD dementia. This analysis also incorporated a mixed-effects beta regression along with a third level of random effect for study in NONMEM.
Our analysis shows that an average (i.e., typical) patient with mild-to-moderate AD in the CAMD database is represented by a 75-year-old female on standard-of-care AD therapy and APOE*4 status unknown (i.e., genotype information was not available). We considered APOE*4 genotype as a continuous variable in the final model and imputed missing allele count as 0.72 (i.e., the observed average number of alleles in patients with known genotype) as described in the results section. This patient would enter a study with a baseline ADAS-cog score of 22.2 and an initial rate of progression of 3.4 ADAS-cog points/year. The estimated baseline ADAS-cog agrees with the observed average baseline ADAS-cog score of 24 reported in the Table 2. The rate of progression aligns with the work conducted by Rogers et al. [13] who reported a rate of natural disease progression of 3.97 ADAS-cog score/year for an average 75-year-old female with MMSE of 21 and APOE*4 heterozygous. According to the mapping function proposed in Fig. 2, an MMSE of 21 corresponds to an ADAS-cog score of 22.4. Compared to the baseline ADAS-cog of an average patient, males had a ~5 % lower baseline value; APOE*4 non-carriers and homozygous, a ~2.7 % lower and ~4.8 % higher baseline value, respectively (Fig. 6). Compared to the initial rate of progression for such an average patient, individuals who are not on AD medication had a ~30 % lower progression rate. Additionally, APOE*4 non-carriers had a ~14 % lower progression rate, while APOE*4 homozygous have a ~25 % higher rate (Fig. 5). In addition, younger baseline age was associated with higher rate of progression (i.e., a 70-year-old had a ~12 % higher, and an 80-year-old, a 12 % lower initial rate when compared to a 75-year-old patient).
The asymmetric, inverted, concave relationship between AD progression rate and severity was appropriately described by the Richard’s function. This function describes an increase in the rate of change when ADAS-cog is below the inflection point, and a decrease in the rate of change when ADAS-cog is above the inflection point (Fig. 4). The restriction in the rate of increase in ADAS-cog score is imposed by the second term of the Richard’s function (Eq. 1): as ADAS-cog scores approach 70, the rate of change tends to zero, reflecting a vertical asymptote in rate or plateau in score (Fig. 4). This is coherent with what is seen in clinical practice: patients with very severe AD dementia tend to experience loss of speech which compromises their ability to perform the tasks that compose the ADAS-cog scale [4]. As a consequence, ADAS-cog scores mathematically plateaus, and the worsening in cognitive impairment can no longer be captured by the scale (i.e., ceiling effect). In severe AD dementia, other clinical endpoints are recommended, for instance, the Severe Impairment Battery [25]. Another aspect is that the shape parameter of the Richard’s function allows for an inflection point that is not restricted to the midpoint of the scale. In this analysis, the estimated inflection point of 52 is closer to the top of the scale, and similar to the inflection point of 46 estimated in the previous work utilizing CAMD data [13].
The incorporation of beta-distributed residual variability along with a logistic model constrained the model prediction within the realistic range of ADAS-cog scores of 0–70. The variance of the beta distribution depends on the expected value and τ as shown in Eqs. 6 and 7. This accommodates the heteroscedasticity of the residual variability because the variance is lower when ADAS-cog scores are close to the boundaries. In our analysis, we estimated a τ of 87.5. For example, for an expected ADAS-cog score of 22.2, the calculated standard deviation of the beta distribution is ~0.05.
The predictors of baseline ADAS-cog were sex and APOE*4 genotype; whereas the predictors of rate of progression were baseline age, APOE*4 genotype and AD medication status. Their effects were statistically significant based on the 95 % confidence intervals which did not include zero (Table 3). Previous AD models showed a faster disease progression rate related to increase in disease severity [8, 9, 12], younger baseline age [9, 12, 13], APOE*4 carrier status [9, 12, 13], and female [9, 13]. The Richard’s function intrinsically accounts for the effect of disease severity in the rate of progression by considering the ADAS-cog score at any time point (e.g., rate of progression increases with ADAS-cog score below the inflection point); hence, all covariates associated with a higher rate of progression have additional effects given a certain disease severity.
The effects of APOE*4 genotype on the rate of AD progression is noteworthy. Our analysis indicates an additive allelic effect on disease progression (Fig. 5b). This is a novel finding for the AD research community. Although the APOE*4 has been associated with a higher rate of disease progression in previous publications, Ito et al. and Samtani et al. modeled the APOE*4 genotypes as two categories (i.e., non-carriers vs. carriers) [9, 12]. Rogers et al. [13] modeled APOE*4 genotype as three categories (i.e., non-carriers, heterozygous and homozygous) but the estimated rate of disease progression in heterozygous did not statistically differ from that in non-carriers. APOE*4 has been implicated as the strongest risk factor for developing late onset AD but the mechanism remains unclear [10, 26]. It has been hypothesized that the APOE*4 variant is associated with build-up of amyloid plaques in the brain, a hallmark of AD pathology believed to contribute to neuronal death [10]. For example, Corder et al. [27] reported that the risk for AD increased from 20 to 90 % and the average age of disease onset decreased from 84 to 68 years with increasing number of APOE*4 alleles in 42 families. Also, Xu et al. [28] reported that one APOE*4 allele has been associated with increased risk of mild cognitive impairment, whereas two APOE*4 alleles have been associated with increased risk of dementia suggesting that APOE*4 homozygous patients have a very short transition through the mild cognitive impairment stage. Therefore, our findings are coherent with prior findings of a significant allelic effect on disease progression.
The effect of AD medication status on the rate of progression should be interpreted with caution. In this analysis, we have observed a faster progression in patients on stable background AD medications compared to those who are not receiving AD medication (Fig. 5a). First, the number of patients who are not receiving AD medication in studies longer than 30 weeks represents a minor sample size (N = 475, ~15 %) as compared to the total number of patients in such studies (N = 3,196). Second, the current standard-of-care medications for AD are AChEIs or/and memantine, which are all approved as symptomatic drugs (i.e., not disease modifying). As a consequence, these drugs are expected to have an effect equivalent to a reduction in the baseline ADAS-cog (i.e., offset effect), but not to affect the rate of disease progression. Therefore, the higher rate of disease progression in patients on stable background medication is unexpected. Third, if patients who are on AD medication truly had a higher baseline ADAS-cog, their disease should progress at a higher rate according to the Richard’s function (the rate of change in ADAS-cog increases with ADAS-cog score below the inflection point; Fig. 4). However, this higher “true” baseline hypothesis would not fully explain the >20 % higher rate of progression with patient on stable background medication considering the relatively small symptomatic effect of AChEIs or memantine (e.g., the effect size of AChEIs is 2–4 points decrease in ADAS-cog [8]). One possible explanation is that patients who are already on stable background AD medication are in a more severe stage of the disease than patients who are not, and this is not adequately captured by baseline MMSE and ADAS-cog; in this case, the underlying disease progression is faster in patients on AD medication, which would not be modified by purely symptomatic agents, like the ones received by this population. In studies 1013 (81 % of the patients on AD medication) and 1014 (76 % of the patients on AD medication), patients on AD medication had an average higher baseline ADAS-cog and faster disease progression (Fig. 8). A possible more convincing explanation is that potential confounders are not available in the CAMD database; for instance, other aspects besides cognition (i.e., impaired ability to function and perform in daily life, behavioral problems and co-morbidities) that lead clinicians to diagnose AD and prescribe medications [29, 30]. No single assessment tool can capture the multifaceted aspect of AD progression; hence, decisions as to treatment strategies were made not only on the basis of a single outcome measure. Therefore, the current knowledge does not support a causality relationship between use of standard-of-care medications and higher rate of disease progression. This observed correlation is likely due to underlying information currently unavailable in the trials integrated within the CAMD database, which can help explain several additional aspects of AD progression. It is also noted that AD medication is a significant covariate only for the rate of progression and not for the baseline ADAS-cog. There are two possible explanations for this: (1) in studies 1013 and 1014, the number of patients who are not on AD medication is much smaller when compared to the number of patients who are on AD medication (Fig. 8); (2) except studies 1013 and 1014, the other studies had only patients who either used or did not use background AD medication; hence, large inter-individual and inter-study variability may have masked the AD medication effect for baseline ADAS-cog.
Limitations of this analysis include the need to develop a dropout model utilizing this updated CAMD database. The average dropout was estimated as 14 % (95 % CI 10–17 %) using a random effects meta-analysis model (metafor package in R), which accounts for between-study variability and heterogeneity. Thus, accounting for missing data becomes important when conducting simulation-based diagnostics or clinical trial simulations. Although the VPC presented in Fig. 7 does not seem greatly compromised, dropout should be accounted for when utilizing this model as a clinical trial simulation tool. An average higher baseline ADAS-cog—26.1 (95 % CI 23.9–28.3) versus 23.8 (95 % CI 22.5–25.0)—and an average older age—75.8 (95 % CI 74.7–76.9) versus 73.9 (95 % CI 73.0–74.7)—was estimated for patients who dropped out using a random effects meta-analysis model. This is in agreement with the dropout model developed by Rogers et al. [13] Second, we have only utilized data from the CAMD database, hence, control-arm data. For this reason, we were not able to differentiate between underlying natural disease progression and placebo effect in the clinical trials. Based on a summary-level meta-analysis of 52 trials, Ito et al. [8] estimated that the maximum placebo effect occurred at around 11 weeks, and disappeared within a year. Third, because year of enrollment was found to be correlated with availability of APOE*4 genotype information and AD medication status, we have not systematically tested its effect on ADAS-cog baseline and rate of progression. However, year of enrollment versus the baseline MMSE indicates that the baseline disease severity has only slightly changed from 1994 to 2008 (Fig. 6a). Fourth, other biomarkers such as cerebrospinal fluid and imaging volumetric brain measures could not be tested as predictors of disease severity or progression due to the unavailable biomarker information in the current CAMD database.
In summary, to our knowledge this is the first work that evaluates the effect of stable background AD medication (vs. placebo only) and the effect of APOE*4 genotypes across 15 clinical studies using patient-level data from the CAMD database on baseline ADAS-cog and its rate of progression. We also investigated whether baseline disease severity had changed between older and more recent trials, possibly due to changes in life style, awareness of the disease, diagnostics and patient care. Our model suggests that faster AD progression is associated with younger baseline age and higher number of APOE*4 alleles, after accounting for baseline disease severity. APOE*4, in particular, seems to be implicated in the AD pathogenesis, and genotyping is especially important for reducing variability in trial results. To be interpreted with caution, patients entering studies on stable background AD medications appear to have a faster progression than those without background AD medication. The current knowledge does not support or implicate a causality relationship between use of background AD medications and higher rate of disease progression, and the association, if validated, might be due to confounding covariates. Although causality has not necessarily been demonstrated, these factors can inform inclusion criteria and stratification, sample size, and trial duration. Finally, this work expands our understanding of the predictors of AD progression and our model informs relevant aspects to help design a clinical trial on a novel AD medication.
References
Alzheimer’s Association (2013) 2013 Alzheimer’s disease facts and figures. Alzheimers Dement 9(2). http://www.alz.org/downloads/facts_figures_2013.pdf. Accessed 29 July 2013
Mangialasche F, Solomon A, Winblad B, Mecocci P, Kivipelto M (2010) Alzheimer’s disease: clinical trials and drug development. Lancet Neurol 9(7):702–716. doi:10.1016/S1474-4422(10)70119-8
Gobburu JV, Lesko LJ (2009) Quantitative disease, drug, and trial models. Annu Rev Pharmacol Toxicol 49:291–301. doi:10.1146/annurev.pharmtox.011008.145613
Rosen WG, Mohs RC, Davis KL (1984) A new rating scale for Alzheimer’s disease. Am J Psychiatry 141(11):1356–1364
Holford NH, Peace KE (1992) Methodologic aspects of a population pharmacodynamic model for cognitive effects in Alzheimer patients treated with tacrine. Proc Natl Acad Sci USA 89(23):11466–11470
Holford NH, Peace KE (1992) Results and validation of a population pharmacodynamic model for cognitive effects in Alzheimer patients treated with tacrine. Proc Natl Acad Sci USA 89(23):11471–11475
Holford NH, Peace K (1994) The effect of tacrine and lecithin in Alzheimer’s disease. A population pharmacodynamic analysis of five clinical trials. Eur J Clin Pharmacol 47(1):17–23
Ito K, Ahadieh S, Corrigan B, French J, Fullerton T, Tensfeldt T (2010) Disease progression meta-analysis model in Alzheimer’s disease. Alzheimers Dement 6(1):39–53. doi:10.1016/j.jalz.2009.05.665
Ito K, Corrigan B, Zhao Q, French J, Miller R, Soares H, Katz E, Nicholas T, Billing B, Anziano R, Fullerton T (2011) Disease progression model for cognitive deterioration from Alzheimer’s Disease Neuroimaging Initiative database. Alzheimers Dement 7(2):151–160. doi:10.1016/j.jalz.2010.03.018
Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW, Fagan AM, Morris JC, Mawuenyega KG, Cruchaga C, Goate AM, Bales KR, Paul SM, Bateman RJ, Holtzman DM (2011) Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med 3(89):89ra57. doi:10.1126/scitranslmed.3002156
Yang E, Farnum M, Lobanov V, Schultz T, Verbeeck R, Raghavan N, Samtani MN, Novak G, Narayan V, DiBernardo A, Alzheimer’s Disease Neuroimaging Initiative (2011) Quantifying the pathophysiological timeline of Alzheimer’s disease. J Alzheimers Dis 26(4):745–753. doi:10.3233/JAD-2011-110551
Samtani MN, Farnum M, Lobanov V, Yang E, Raghavan N, Dibernardo A, Narayan V (2012) An improved model for disease progression in patients from the Alzheimer’s disease neuroimaging initiative. J Clin Pharmacol 52(5):629–644. doi:10.1177/0091270011405497
Rogers JA, Polhamus D, Gillespie WR, Ito K, Romero K, Qiu R, Stephenson D, Gastonguay MR, Corrigan B (2012) Combining patient-level and summary-level data for Alzheimer’s disease modeling and simulation: a beta regression meta-analysis. J Pharmacokinet Pharmacodyn 39(5):479–498. doi:10.1007/s10928-012-9263-3
Critical Path Institute. Coalition Against Major Diseases database. http://c-path.org/programs/camd/. Accessed 14 Feb 2014
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
R Core Team (2013) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/
Beal S, Sheiner LB, Boeckmann A, Bauer RJ (2010) Nonlinear Mixed Effects Model Program (NONMEM) version 7.1.2, Icon Development Solutions, Ellicott City, MD, USA. http://www.iconplc.com/technology/products/nonmem
Tsoularis A, Wallace J (2002) Analysis of logistic growth models. Math Biosci 179(1):21–55
Xu XS, Samtani MN, Dunne A, Nandy P, Vermeulen A, De Ridder F, Alzheimer’s Disease Neuroimaging Initiative (2013) Mixed-effects beta regression for modeling continuous bounded outcome scores using NONMEM when data are not on the boundaries. J Pharmacokinet Pharmacodyn 40(4):537–544. doi:10.1007/s10928-013-9318-0
Smithson M, Verkuilen J (2006) A better lemon squeezer? Maximum-likelihood regression with beta-distributed dependent variables. Psychol Methods 11(1):54–71. doi:10.1037/1082-989X.11.1.54
Lindbom L, Pihlgren P, Jonsson EN (2005) PsN-Toolkit—a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 79(3):241–257. doi:10.1016/j.cmpb.2005.04.005
Beal S, Sheiner LB, Boeckmann A, Bauer RJ (2013) Nonlinear Mixed Effects Model Program (NONMEM) version 7.3.0, Icon Development Solutions, Ellicott City, MD, USA. http://www.iconplc.com/technology/products/nonmem
SAGE Publications I Akaike Information Criterion (2007) Encyclopedia of measurement and statistics. SAGE Publications, Inc. SAGE Publications, Inc., Thousand Oaks, CA. doi:10.4135/9781412952644
Crean S, Ward A, Mercaldi CJ, Collins JM, Cook MN, Baker NL, Arrighi HM (2011) Apolipoprotein E epsilon4 prevalence in Alzheimer’s disease patients varies across global populations: a systematic literature review and meta-analysis. Dement Geriatr Cogn Disord 31(1):20–30. doi:10.1159/000321984
Schmitt FA, Ashford W, Ernesto C, Saxton J, Schneider LS, Clark CM, Ferris SH, Mackell JA, Schafer K, Thal LJ (1997) The severe impairment battery: concurrent validity and the assessment of longitudinal change in Alzheimer’s disease. The Alzheimer’s Disease Cooperative Study. Alzheimer Dis Assoc Disord 11(Suppl 2):S51–S56
Liu CC, Kanekiyo T, Xu H, Bu G (2013) Apolipoprotein E and Alzheimer disease: risk, mechanisms and therapy. Nat Rev Neurol 9(2):106–118. doi:10.1038/nrneurol.2012.263
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261(5123):921–923
Xu WL, Caracciolo B, Wang HX, Santoni G, Winblad B, Fratiglioni L (2013) Accelerated progression from mild cognitive impairment to dementia among APOE ε4ε4 carriers. J Alzheimers Dis 33(2):507–515. doi:10.3233/JAD-2012-121369
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH (2011) The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):263–269. doi:10.1016/j.jalz.2011.03.005
Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B (2002) Guidelines for managing Alzheimer’s disease: part II. Treatment. Am Fam Physician 65(12):2525–2534
Acknowledgments
The authors would like to thank Dr. Mahesh Samtani (Johnson and Johnson Pharmaceutical Research and Development) for his technical guidance and invaluable input in conducting the analysis. The authors would also like to acknowledge CAMD database management team to provide the assembled dataset and to respond authors’ queries. All authors are employees of Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
The Coalition Against Major Diseases: Data used in preparation of this article were obtained from the Coalition Against Major Diseases (CAMD) database (http://codr.c-path.org). A complete listing of CAMD members can be found at: http://c-path.org/programs/camd/.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: NONMEM 7.3 code for final model
Appendix: NONMEM 7.3 code for final model




Rights and permissions
About this article
Cite this article
Conrado, D.J., Denney, W.S., Chen, D. et al. An updated Alzheimer’s disease progression model: incorporating non-linearity, beta regression, and a third-level random effect in NONMEM. J Pharmacokinet Pharmacodyn 41, 581–598 (2014). https://doi.org/10.1007/s10928-014-9375-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-014-9375-z