Abstract
Introduction Occupational and physical therapists are at significant risk of work-related musculoskeletal disorders and injuries. As the therapy workforce ages, and shortages of therapists are predicted, it is important to evaluate differences in injuries and injury behaviors between older and younger therapists. Methods Half of all occupational and physical therapists practicing in Wisconsin were randomly selected for a cross sectional study examining the relationship between aging and characteristics of self-reported work injuries and musculoskeletal symptoms. Results Data from a sample of 1,158 therapists revealed older workers to have similar injury incidence rates, however, days away from work due to injury were higher among older workers. Overall, older and younger therapists were more similar than different, especially in regards to work behaviors. Older therapists tended to report more severe pain symptoms than younger therapists and were two and a half times more likely to report that they changed jobs due to their pain symptoms. Conclusions Older and younger therapists have similar work-related injury experiences. Older workers may be more vulnerable to lost work time and may experience more severe pain symptoms. Many interventions exist to prevent work-related injuries to therapists and more guidance in the best way to integrate these interventions (e.g., mechanical lift devices) into therapy practice is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evidence exists that occupational therapists (OT) and physical therapists (PT) are at similar and substantial risk of work-related musculoskeletal injuries and disorders (WMSD) [1–10]. WMSD include moderate to severe work-related pain and injury and most often affect the low back, neck, shoulder, wrist and hand [1–3, 10]. In fact, recent evidence revealed annual incidence rates of 16.5 per 100 fulltime OT and 16.9 per 100 fulltime physical therapists, an annual prevalence of 27% and a 1 year incidence of 21% [1, 2]. Therapists have reported altering work habits (74%), losing work time (7–32%), working while injured or in pain (95%), and changing jobs or leaving the profession because of WMSD (17–30%) [1, 2, 6, 7, 10]. Of particular concern is the proportion of therapists considering leaving the profession, given predicted shortages and an increasingly medically complex patient population [11].
The nature of the work required of therapists helps explain the high rates of injury. Healthcare jobs tend to be associated with heavy lifting, awkward postures or repetitive motions [12, 13]. Excessive loading during manual patient handling, applying excessive forces during pushing and/or pulling of objects, and the required use of awkward postures during patient care all are high risk behaviors that are associated with WMSDs [14]. Healthcare personnel engage in such high risk activities as transferring patients, lifting patients and repositioning patients repeatedly and throughout the day [15].
Some risk factors for therapist injury are similar to those experienced by healthcare workers in general. Transfers and repositioning, for example, are associated with increased odds of WMSD to the low back [1]. However, therapy specific activities, such as joint mobilization and soft tissue work also are associated with increased odds of WMSD, placing strain on the hands and wrist [1]. Patient care activities are associated with the majority of injuries sustained by occupational therapists and patient lifting accounts for almost three-quarters of these injuries [16]. Therapists with WMSD work more hours and spend more time in direct patient care than those without WMSD [2]. Recent research indicates that increased age also is associated with WMSD [1, 2].
The age of therapists practicing in the United States is increasing [17, 18]. The median age of occupational therapists increased from 36 in 1990 to 42 in 2006. The number of practitioners in the 50–59 year-old group is at its highest level ever, and the percentage of practitioners under age 30 is now just 7.9% [17]. Out of 52,907 physical therapists in the US, over 25% are within the age range of 40–49 years old, while almost 20% are 50–59 years old [18]. In general, the number of workers over 55 years of age is likely to increase by 50% between 2002 and 2012 [19, 20], and the number between 65 and 74 will increase by 83% between 2006 and 2012 [21]. Multiple factors explain this increase, including financial needs at retirement, an increase in the minimum age at which individuals can receive social security, and the abolition of a mandatory retirement age [22].
Age and Impairment
The “graying of the workforce” and an increase in work-related injuries and illnesses has led to inquiry regarding their relationship. Physiological (declines in sensory, motor, and cognitive processes), psychological and medical changes associated with aging affect the ability of older individuals to perform functions associated with daily living [23]. A great deal of the literature on the process of aging describes the many systemic and degenerative changes in the structure and function of the human body. Tendon and ligament stiffening associated with degenerative joint changes lead to a decrease in joint mobility and a reduction in range of movement. Muscle strength decreases, blood pressure rises, posture changes, motor response time slows, and sensory changes in vision and hearing are experienced [24]. In addition, some general conclusions have been reached regarding the nature of age-related changes in cognition. Cognition declines in most individuals by age 74, but these changes differ in severity across individuals. It is important to note; however, that these changes are related to many factors and are less severe in individuals free of chronic disease, who are affluent, have a flexible personality, and a spouse with a high level of cognitive function [24].
Age and Work Injury
Although the literature points to an increased risk for injury due to associated age-related changes, there is also general consensus that as age increases, both the number of injuries and injury rates decline [25, 26]. Experience, maturity and judgment of older workers may explain their lower injury rates [27]. However, there appears to be an increased risk of severe and fatal work-related injuries in older workers [26, 28–31]. Research is mixed about longer recovery periods [28, 32], but older workers do appear more likely to receive surgical interventions for their injuries [28] and may experience subsequent disability due to age-related changes in cognitive function, health, and recuperative ability [33–36]. In addition, older workers may experience more lost work time associated with injury and may be less likely to return to work following an occupational injury, although again, research is mixed on these assertions [28, 37, 38]. The body’s resilience to chronic wear and tear is reduced with age. Therefore, injury risk attributed to overuse, often labeled “cumulative trauma disorder” and identified as work-related musculoskeletal disorders (MSDs), increases with age [25, 39].
Given the high rates of injury among therapists, the physical demands of their work, and the advancing age of practicing therapists, analysis of the patterns of musculoskeletal injury and disorders must be undertaken. The purpose of this study, therefore, was to assess the differences in WMSD and work practices among older and younger therapists. Specifically, the following questions were posed:
-
1.
Do older therapists have higher rates and prevalence of work-related injury (WRI) than younger therapists?
-
2.
Are older therapists more likely to experience severe work-related injury or disorder than younger therapists?
-
3.
Do work practices and behaviors among older therapists with work-related injuries and disorders differ from younger therapists?
Methods
Participants
The target population for this study included (1) all licensed occupational and physical therapists who (2) resided in the state of Wisconsin. The study investigators used a random number table to select 50% of all occupational therapists (1,436 OTs) and 50% of all physical therapists (1,861 PTs) from the state licensure list. Participants were subsequently excluded if they had not worked in any of the prior 3 years of interest. Participants ages 55 and older were considered ‘older workers’ and those under 55 were considered ‘younger workers’. Fifty-5 years of age was selected as the cut-point for older worker based on data that suggest that workers 55 years and older and are at greater risk of severe injuries, as measured by days away from work, and fatal injuries.
Instrumentation
Researchers developed a survey designed to assess work-related injuries and musculoskeletal disorders, based on the surveys created by Holder et al. [3] and Campo et al. [1]. Holder et al. created a measure of work-related injuries in physical therapists. However, past research has revealed that therapists are hesitant to report their injuries to an employer, and that they often minimize their symptoms, self-treat and seek treatment from colleagues [1, 4]. To account for underreporting, and concerns that therapists may not consider their symptoms to be a musculoskeletal injury, we adapted the survey created by Campo et al. [1], which captures musculoskeletal symptoms and uses a case definition to identify symptoms of sufficient severity, duration, and frequency to define as a work-related musculoskeletal disorder.
The final instrument included measures of work-related injury (WRI), work-related pain/discomfort and work-related musculoskeletal disorder (WMSD). The survey consisted of three parts: Section A: demographic and work history information; Section B: a self-report of work-related musculoskeletal injuries sustained in each of the past 3 years; and Section C: questions about musculoskeletal symptoms experienced the prior year, including frequency, duration, and severity. Participants completed section B or C, but not both. Section B was completed by therapists who indicated that they had sustained a work-related injury in any or all of 3 years: 2004, 2005, 2006.
Therapists who stated that they had not experienced a work-related injury proceeded to Section C, where they were asked to complete information about work-related musculoskeletal symptoms they may have experienced in the past 12 months. The intent was to capture therapists who may be experiencing musculoskeletal symptoms, but would not consider them a work-related injury. Researchers used a stringent case definition of work-related musculoskeletal disorder (WMSD) to identify therapists with pain severe enough to interfere with work, based on the work of Campo et al. [1]. The definition identified pain/discomfort serious enough to cause problems at work as WMSDs, but avoided minor complaints. The definition identified an individual as having a WMSD if he/she rated pain of at least 4/10 on a visual analog scale (from 0 to 10) that lasted more than 1 week or was present at least once a month.
To evaluate the validity of the survey, five occupational therapists and five physical therapists completed and critiqued it. The therapists were asked to provide feedback on the clarity, phrasing, and importance of the questions. Based on their responses, several questions were changed and/or removed and the final product readied for dissemination.
Procedures
This survey study examined the relation between age and self-reported work-related injury and self-reported musculoskeletal symptoms; age and characteristics of injury, symptoms, and disorders; and age and worker practices.
Investigators mailed a cover letter, demographic information page, two-page questionnaire, and a stamped, self-addressed envelope to 3,297 therapists in Wisconsin. All responses were confidential and no personal identifiers were included in the survey. After a 3-week waiting period, the mailing was repeated. No surveys were opened until the second mailing was completed.
Data Analysis
Three-year injury incidence rates were calculated for injuries. A 3-year rate was used to increase the stability of the incidence rate by increasing the number of cases. Overall injury rates and rates were calculated for injuries that resulted in at least a half day away from work.
Injury incidence rates per 100 full-time workers for older and younger workers were calculated using the following formula:
The total number of therapists injured was used in the numerator rather than the total number of injuries. Therapists were able to report multiple injuries within each year. Because we were unable to determine whether each injury event within a year was separate and distinct, or an aggravation of the original injury, we coded the number of injuries dichotomously (‘not injured’ or ‘injured’). However, injuries reported by therapists in multiple years were included, so if they reported an injury in each of the 3 years, three injuries were included in the numerator. Confidence intervals for the incidence rates were estimated using the method described by Haenszel et al. [40], for data following a Poisson distribution for rare events. Rates also were compared using the following formula;
where
Z scores in excess of 1.96 indicated a statistically significant difference in rates at a P-value of 0.05.
Basic descriptive and inferential analyzes, including independent sample t-tests, Pearson chi-square, and odds ratios, were conducted to compare older and younger workers on the personal and professional factors associated with pain/discomfort, work-related musculoskeletal disorders (WMSDs), and work-related injuries, and their reporting and treatment seeking behaviors. Work practices include patient treatment, time off from work, and the proportion of occupational and physical therapists that have changed practice area because of symptoms or injuries. Participants who reported work-related injuries answered the above questions based on the injury that most interfered with their work.
Results
Participants
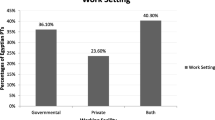
The survey was sent to 3,297 physical and occupational therapists licensed and living in the state of Wisconsin, and 1,189 (36%) responded. Of these, 31 were excluded because they had retired, decided to stay-at-home with their children, or had not filled out the form completely. The final sample size was 1,158 therapists (681 physical therapists and 477 occupational therapists), with 153 workers aged 55 or older, representing 13% of the sample. The average age of the older workers was 59 years and of younger workers was 40 years (Table 1). Additionally, 83% of older and 87% of younger workers were female. The older workers had an average of 31 years of experience and the younger had an average of 16 years. Older therapists worked a similar number of hours per week as their younger peers (t = 1.77; P = 0.08), but spent approximately 2 h less per week in patient care (t = −2.17; P = 0.03).
Injury Incidence, Prevalence, and Characteristics
Because the low number of older workers decreased the stability of annual rates, we calculated 3 years incidence rates for all injuries and injuries involving at least a half day away from work (Table 2). The injury incidence rate for older workers (12.43 per 100 full-time workers) was not significantly different from younger workers (14.15 per 100 full-time workers). However, the 3-year injury incidence rate for injuries requiring at least a half day away from work among older workers (5.82 per 100 full time workers) was higher than for younger workers (2.72 per 100 full-time workers). The 3 years prevalence for work-related injury was 19.6% among older workers and 21.4% among younger workers.
We assessed whether older workers were at increased risk of sustaining multiple injuries as compared to younger workers, and were unable to detect a difference (Table 3). Older workers were no more likely to report the injury, seek treatment, change jobs, or consider changing jobs because of their injury than their younger peers. In fact, 22% of younger workers were considering changing jobs and 10% reported they had changed jobs because of their injury compared to 17% of older workers considering a job change and 0% who reported a job change. Older workers also were no more likely to limit patient contact time, alter their work habits, or report that work exacerbated their symptoms.
Musculoskeletal Symptoms
Among older workers, 43% reported work-related pain or discomfort, quite similar to their younger colleagues (47%) (Table 4). Most reported pain as the primary symptom (31%), followed by fatigue (11%), though many therapists wrote in ache, tenderness, tightness, and stiffness as other symptoms. The most common sites of symptoms were the low back, neck, and shoulder for the younger workers, and the low back, hand, neck, and knee for the older workers. The older workers reported pain the hands more often than the younger workers, and younger workers more often reported pain in the neck and shoulder (Table 5).
Among those therapists with symptoms that were not considered severe (did not meet our case definition of WMSD), older and younger therapists were quite similar. About half of both older and younger therapists reported that they experienced their symptoms during patient treatment (48%) and about 11% of older and 16% of younger workers stated that their symptoms interfered with patient treatment. Older workers were no more likely to seek treatment because of their symptoms, miss work, work while in pain, or limit patient contact time than their younger counterparts.
Older workers were, however, two and a half times more likely to report that they changed jobs because of their symptoms (χ 2 = 8.234; P = 0.004). Older workers tended to report more severe symptoms, and though not statistically significant, there appeared to be a tendency for a higher proportion of older therapists to meet the case definition of WMSD (P = 0.072).
Work-Related Musculoskeletal Disorders
It remains unclear as to whether older workers in general were more likely to meet the case definition of WMSD than younger therapists (O.R. 1.70; 95% C.I.: 0.949, 3.03). Among those who did meet the criteria for a WMSD, older workers were more likely to report that they had changed jobs because of the WMSD. While not statistically significant, it appeared that older workers might be more likely to miss work and consider a job change because of the WMSD. No other differences were observed between younger and older therapists.
Because of the vulnerability of women to WMSD, analyses of female therapists were conducted. A significantly higher proportion of female therapists did meet the criteria for WMSD than younger female therapists (χ 2 = 6.158; P = 0.013). In fact, the odds of being female were 9.6 times as high among those meeting the case definition of injury as among those who did not. Women with WMSD were more likely to report their symptoms than their younger colleagues (χ 2 = 4.828; P = 0.028). No conclusions can be drawn about the differences between older and younger male therapists because so few men met the criteria for WMSD. Interestingly, while female workers who met the case definition of WMSD were just as likely to alter their work practices because of their symptoms as younger women, those with symptoms not severe enough to meet the definition were 1.4 times more likely to alter their work than the younger therapists.
Discussion
The results of this study echo previous studies examining the relationship between aging and occupational injury. Demographically, the therapists were more similar than different. Most of the older and younger therapists were female, reported themselves to be in good or excellent health, and about one-third held graduate degrees.
The 3-year injury incidence rate for injuries did not differ between groups, and older workers were no more likely than younger to report multiple injuries during the 3 years period. They also were no more likely to report work-related pain than the younger therapists.
All therapists had injury incidence rates that are higher than those in many other industries. The national rate in private industry for nonfatal injuries and illness is 4.4 per 100 fulltime workers in 2006, and 2007 injury incidence rates in other physically demanding professions were lower than therapist rates: construction had a rate of 5.2 per 100 fulltime workers, manufacturing was 5.1 and agriculture was 5.0 [41]. It is critical to note that the BLS rates are based on total recordable cases, and we have no way of knowing whether all the injuries reported by the therapists were recordable. It also is important to note that our injury incidence rates do not include therapists who met our criteria for WMSD. For an important point of comparison, hospitals and nursing homes reported injury incidence rates of 7.1 and 8.4, respectively, for 2007. In this study, about 30% of therapists worked in these two settings.
The 3-year incidence rate for injuries requiring at least a half day off work was higher among the older therapists in this study, and therapists who met the case definition for WMSD were slightly more likely to miss work. This finding is consistent with the findings of many researchers, who report that older workers seem to experience more severe injuries [22, 36, 42]. Severity, often defined by longer recovery time or lost work time, also refers to more severe injuries [43]. Fractures, for example, represent a higher proportion of non-fatal injuries in older workers as compared to younger workers [43]. In the present study, older therapists were no more likely to report fractures than younger therapists, and strains, sprains, and tendonitis were among the most common complaints for all therapists.
Physical and occupational therapy are professions requiring physical exertion, awkward position, and repetitive movements. While the physiology behind the injuries in this study is beyond the scope of our analysis, we do know that jobs requiring physical effort, stooping or kneeling, and heavy lifting have been associated with increased risk of injury in older workers [35]. All these activities are associated with the practice of occupational and physical therapy, and likely interact with musculoskeletal vulnerability associated with the aging process, such as decreased strength and joint range of motion. For example, muscle strength appears to stay relatively stable with only slight declines until about the age of 50, at which time strength declines about 15% per decade [44–51]. Inadequate muscle strength may lead to increased susceptibility to lifting injuries [52], which accounted for about half of the injuries reported by the older therapists in this study. Other risk factors to consider include vision and hearing changes associated with aging; both of which have been associated with increased risk of workplace injury in older workers [35].
The older female therapists in our study were more likely to meet our criteria for a WMSD than younger female therapists and male therapists. Females typically are more vulnerable to the musculoskeletal changes that occur with age [53]. For example, females typically have about 65% of the strength of men, and age-related declines will affect them more profoundly [52]. The effects of physically demanding work, and possibly the musculoskeletal demands on the body may have effects outside work not limited to musculoskeletal injury. Aittomaki et al. [53] reported an association between physically demanding work and role limitations outside of work among older women, and they may experience more role limitations than their male counterparts. Of interest was that older female therapists with mild musculoskeletal symptoms were more likely to alter their work habits because of those symptoms than their younger colleagues. This could provide some insight into longevity: that these women represent therapists who are more willing to adapt their work habits when symptoms are mild, and are able to stay in the profession longer. Alternatively, this could reflect the experience of the older therapists, who are now more aware of age-related changes and limitations, and are taking steps to prevent injury as older workers.
Most work practices and behaviors did not vary between older and younger therapists. They are equally likely to report their injuries or symptoms, work while in pain, and to report that clinical practice increases their symptoms. All were equally unlikely to limit patient contact time, indicating that productivity was not affected differentially by age.
Older workers with pain and WMSD were more likely to change jobs than the younger therapists. The same did not hold true for those who reported an injury. The reasons for this difference are unclear, but it is possible that the conditions captured by the case definition of WMSD reflect ongoing symptoms. We did not ask about severity of symptoms when we asked about injuries, only when we asked about musculoskeletal pain. Therefore, we may be capturing therapists who are experiencing more active symptoms. Among those older therapists who reported that they did change jobs because of the symptoms, it is possible this was due to more opportunities because of their experience and community connections.
Of importance to this group in particular, is that certain behaviors can combat the musculoskeletal declines associated with aging. Extra-curricular sports and leisure activities may be protective for neck and shoulder pain [53–55]. Strength training, exercise, programs, and regular physical activity all have been shown to delay age-related changes in strength, fitness, and physical capacity [53, 56–58]. Since many of the injuries experienced by this group are associated with lifting, moving, and manipulating patients, preserving strength and physical capacity could be of tremendous benefit.
Limitations
More research needs to be done to understand the relationship between the aging therapist population and work-related injuries. Some limitations of this study are the small number of older therapists surveyed compared to the younger group and the lack of comparable numbers according to gender. The uneven group sizes may have skewed the reliability of the findings for older therapists and smaller numbers of older therapists may have decreased the precision of the rates. Larger sample sizes and more equivalent numbers of males and females would increase the ability to make generalized statements. Another variable worth exploring is the influence of the type of health care facility or workplace in which the therapists practice. Facilities vary in job demands and schedules based upon their clientele and treatment area. For example, hand therapists would likely report their job demands to be less physically demanding than an inpatient rehabilitation units within a large hospital.
This study may have been vulnerable to the healthy worker effect, in which healthy workers stay in the workforce while less healthy workers retire, change professions, or move into a less physically demanding position, such as management. In the present study, about 2% of both older and younger workers reported that they worked in administration. This may be a reporting error, with therapists reporting on the type of setting they worked in as opposed to the job title within that setting; however, these numbers do not indicate that older therapists have moved into management. It is likely that this study captured those therapists with the physical capacity to continue working in physically demanding settings (over 60% worked in acute care/rehab, schools and skilled nursing facilities). That individuals with greater fitness remain in demanding jobs is supported by other studies [52, 57, 59] and all the physical and occupational therapists in this study rated their health as good or excellent. Research indicates that many of the musculoskeletal declines seen in older adults are due to physical inactivity and a sedentary lifestyle, which may not describe our population, and may explain why few differences existed between the older and younger therapists.
Finally, generalizability of the study may be limited. The study sampled only therapists living and practicing in Wisconsin. It is possible that these therapists do not represent therapists nationally. The study also relied on self-report. With a response rate of about 36%, it is possible that the numbers are skewed due to a self-selection bias, with symptomatic therapists more likely to respond. In that case, these participants may not represent the majority of therapists practicing today.
Recommendations for Further Research
An investigation into the characteristics of older therapists that allow them to continue to practice would assist with the promotion of behaviors to increase longevity. The therapists with the greatest clinical experience are the ones at risk of injury and WMSD, and to design strategies to promote longevity would be beneficial to younger therapists and patients. In addition, an assessment of the practice settings and the work habits of older therapists within these settings would help illuminate how aging clinicians are continuing to work.
Conclusions
Older therapists appear to be at greater risk of injuries requiring time away from work and at greater risk of sustaining WMSD than younger therapists. Predicted shortages of healthcare personnel and a medically complex patient population make it critical to keep therapists in the profession, especially those with clinical expertise and many years of experience. Safe patient handling and movement programs have decreased work-related injuries in nursing personnel, and the equipment can be adapted for use in therapy [13, 14, 60]. While this may not prevent all injuries, it will prevent a substantial proportion [16]. Further work must be done to identify ways to reduce musculoskeletal strain associated with manual therapies, like joint mobilization and soft tissue work, and other therapy specific activities associated with musculoskeletal burden.
References
Campo M, Weiser S, Koenig K, Nordin M. Work related musculoskeletal disorders in physical therapists: a prospective cohort study with 1-year follow up. Phys Ther. 2008;88:608–19.
Darragh AR, Huddleston W, King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am J Occup Ther. 2009;63:351–62.
Holder N, Clark H, Diblasio J, Hughes C, Scherpf J, Harding L, et al. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys Ther. 1999;79:642–52.
Waldrop S. Work-related injuries: preventing the PT from becoming the patient. PT Mag Phys Ther. 2004;12:34–41.
Bork BE, Cook TM, Rosencrance JC, et al. Work-related musculoskeletal disorders among physical therapists. Phys Ther. 1996;76:827–35.
Cromie JE, Robertson VJ, Best MO. Work related musculoskeletal disorders in physical therapists: prevalence, severity, risks and responses. Phys Ther. 2000;80:336–51.
Glover W, McGregor A, Sullivan C, Hague J. Work-realted musculoskeletal disorders affecting members of the Chartered Society of Physiotherapy. Physiotherapy. 2005;91:138–47. doi:10.1016/j.physio.2005.06.001.
West DJ, Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Aust J Physiother. 2001;47:179–86.
Mierzejewski M, Kumar S. Prevalence of low back pain among physical therapists in Edmonton, Canada. Disabil Rehabil. 1997;19:309–17.
Molumphy M, Unger B, Jensen GM, Lopopolo RB. Incidence of work-related low back pain in physical therapists. Phys Ther. 1985;65:482–6.
BLS. The Job Openings and Labor Turnover Survey (JOLTS). 2008. http://www.bls.gov/jlt/. Accessed 6 May 2008.
HermanMiller for Healthcare.[homepage on the internet]. Michigan:Herman Miller. c.2008. Research Summaries: Ergonomics: Good news for healthcare workers, 2003. http://www.hermanmiller.com/hm/content/research_summaries/pdfs/wp_ergogoodnews0503.pdf. Accessed January 21 2008.
Li J, Wolf L, Evanoff B. Use of mechanical patient lifts decreased musculoskeletal symptoms and injuries among health care workers. Injury Prevention. 2004;* 10:212–216.
Waters T, Collins J, Galinsky T, Caruso C. NIOSH research efforts to prevent musculoskeletal disorders in the healthcare industry. Orthop Nurs. 2006;25:380–9.
Menzel NN, Brooks SM, Bernard TE, Nelson A. The physical workload of nursing personnel: association with musculoskeletal comfort. Int J Nurs Stud. 2004;41:859–67. doi:10.1016/j.ijnurstu.2004.03.012.
Bls.gov.[homepage on Internet] Washington, DC; US Bureau of Labor Statistics; c.2004. http://www.bls.gov/iif/oshcdnew.htm#04b. Accessed 1 may 2009.
American Occupational Therapy Association. 2006 AOTA workforce and compensation survey: occupational therapy salaries and job opportunities continue to improve. OT Pract. 2006;11:10–2. Electronic Version.
APTA.org [homepage on the Internet] Virginia: American Physical Therapy Association; c2007. http://www.apta.org. Accessed 2008 Jan 21.
Fullerton FN, Toossi M. Labor force projections to 2010: steady growth and changing composition. Mon Labor Rev [serial on the Internet]. 2001. 124: [about 17 p.]. http://www.bls.gov/opub/mlr/2001/11/art2full.pdf. Accessed 2008 Jan 21.
Toossi M. Labor force projections to 2012: the graying of the US workforce. Mon Labor Rev [serial on the Internet]. 2004;127: [about 57 p.]. http://www.bls.gov/opub/mlr/2004/02/art3full.pdf. Accessed 2008 Jan 21.
http://cdc.gov/niosh [Internet Homepage]. Worker Health Chartbook.c.2004. http://www.cdc.gov/niosh/docs/2004-146/default.htm. Accessed 1 May 2005.
state.nj.us/health [homepage on the Internet] New Jersey: New Jersey Department of Occupational Health; c1996. http://www.state.nj.us/health/eoh/survweb. Updated 2008 Sep 05; Accessed 2008 Jan 21.
Garg A. Ergonomics and the older worker: an overview. Exp Aging Res. 1991;17:143–55.
Thomas SA, Browning CJ, Greenwood KM. Rehabilitation of older injured workers. Disabil Rehabil. 1994;16:162–70.
Breslin FC, Smith P. Age related differences in work injuries: a multivariate, population based study. Am J Ind Med. 2005;48:50–6. doi:10.1002/ajim.20185.
Salminen S. Have young workers more injuries than older ones: an international literature review. J Safety Res. 2004;35:513–21. doi:10.1016/j.jsr.2004.08.005.
Rix SE. Health and safety issues in an aging workforce. AARP Issue Brief 49. Washington, DC: AARP; 2001. p. 1–16.
Pransky GS, Benjamin KL, Savageau JA, Currivan D, Fletcher K. Outcomes in work-related injuries: a comparison of older and younger workers. Am J Ind Med. 2005;47:104–12. doi:10.1002/ajim.20122.
BLS.gov.[homepage on Internet] Washington, DC; US Bureau of Labor Statistics; c2002. http://stats.bls.gov/iif/oshcfoil.htm. Accessed 2008 Jan 21.
Bell CA, Stout NA, Bender TR, Conroy CS, Crouse WE, Myers JR. Fatal occupational injuries in the United States, 1980–1985. J Am Med Assoc. 1990;263:3047–50. doi:10.1001/jama.263.22.3047.
Goldberg RL, Bernstein L, Garabrant DH, Peters JM. Fatal occupational injuries in California, 1972–1983. Am J Ind Med. 1989;15:177–85. doi:10.1002/ajim.4700150206.
Rogers E, Wiatrowski W. Injuries, illnesses, and fatalities among older workers. Mon Labor Rev. 2005;128:24–30.
Mitchell O. The relation of age to work-place injuries. Mon Labor Rev. 1988;111: [about 5 p.]. http://www.bls.gov/opub/mlr/1988/07/art2full.pdf. Accessed 2008 Jan 21.
Laflamme L, Menckel E. Aging and occupational accidents: a review of the literature of the last three decades. Saf Sci. 1995;21:145–61. doi:10.1016/0925-7535(95)00059-3.
Zwerling C, Sprince N, Wallace R, David C, Whitten P, Heeringa S. Risk factors for occupational injuries among older workers: an analysis of the Health and Retirement Study. Am J Public Health. 1996;86:1306–9. doi:10.2105/AJPH.86.9.1306.
Benjamin K, Pransky G. Occupational injuries and the older worker: challenges in research, policy, and practice. Southwest J Aging. 2001;16:47–61.
Turner JA, Franklin G, Turk DC. Predictors of chronic disability in injured workers: a systematic literature synthesis. Am J Ind Med. 2000;38:707–22. doi:10.1002/1097-0274(200012)38:6<707::AID-AJIM10>3.0.CO;2-9.
Crook J, Moldofsky H. The probability of recovery and return to work form work disability as a function of time. Qual Life Res. 1994;3(Suppl. 1):S97–109. doi:10.1007/BF00433383.
Putz-Anderson V. Cumulative trauma disorders: a manual for musculoskeletal disease of the upper limbs. London: Taylor and Francis; 1988.
Haenszel W, Loveland DB, Sirken MG. Lung cancer mortality as related to residence and smoking histories: I. White Males. J Natl Cancer Inst. 1962;28:947–1001.
http://www.bls.gov [Internet Homepage]. Workplace injuries and illnesses in 2007; News USDoL c. 2008. http://www.bls.gov/iif/oshsum.htm. Accessed 1 May 2009.
Peek-Asa C, McArthur DL, Kraus JF. Incidence of low back injury among older workers in a cohort of material handlers. J Occup Environ Hyg. 2004;1:551–7. doi:10.1080/15459620490479799.
Silverstein M. Meeting the challenges of an aging workforce. Am J Ind Med. 2008;51:269–80. doi:10.1002/ajim.20569.
Kenny GP, Yardley JE, Martineau L, Jay O. Physical work capacity in older adults: implications for the aging worker. Am J Ind Med. 2008;51:610–25. doi:10.1002/ajim.20600.
Booth FW, Weeden SH, Tseng BS. Effect of aging on human skeletal muscle and motor function. Med Sci Sports Exerc. 1994;26:556–60. doi:10.1249/00005768-199405000-00006.
Goldich RL. Military retirement and personnel management: should active duty military careers be lengthened. Washington, DC: Congressional Research Service; 1995.
Metter EJ, Lynch N, Conwit R, Lindle R, Torbin J, Hurley B. Muscle quality and age: cross sectional and longitudinal comparisons. J Gerontol. 1999;54A:B207–18.
Doherty TJ. The influence of aging and sex on skeletal muscle mass and strength. Curr Opin Clin Nutr Metab Care. 2001;4:503–8. doi:10.1097/00075197-200111000-00007.
Prather H, Foye PM, Stiens SA, Wilder RP, Cianca JC. Industrial medicine and acute musculoskeletal rehabilitation. 6. Occupational health for special populations. Arch Phys Med Rehabil. 2002;83:S25–32. doi:10.1053/apmr.2002.32154.
Kamel HK. Sarcopenia and aging. Nutr Rev. 2003;61:157–67. doi:10.1301/nr.2003.may.157-167. review.
Zuhosky JP, Irwin RW, Sable AW, Sullivan WJ, Panagos A, Foye PM. Industrial medicine and acute musculoskeletal rehabilitation. 7. Acute industrial musculoskeletal injuries in the aging workforce. Arch Phys Med Rehabil. 2007;88(Suppl 1):S34–9. doi:10.1016/j.apmr.2006.12.014.
Shephard RJ. Age and physical work capacity. Exp Aging Res. 1999;25:331–43. doi:10.1080/036107399243788.
Aittomaki A, Lahelma E, Roos E, Leino-Arjas P, Martikainen P. Gender differences in the association of age with physical workload and functioning. Occup Environ Med. 2005;62:95–100. doi:10.1136/oem.2004.014035.
Siivola SM, Levosks S, Latvala K, Hoskio E, Vanharanta H, Keinanen-Kiukaanniemi S. Predictive factors for neck and shoulder pain: a longitudinal study in young adults. Spine. 2004;29:1662–9. doi:10.1097/01.BRS.0000133644.29390.43.
Cassou B, Derriennic F, Monfort C, Norton J, Touranchet A. Chronic neck and shoulder pain, age, and working conditions: longitudinal results from a large random sample in France. Occup Environ Med. 2002;59:537–44. doi:10.1136/oem.59.8.537.
Bellew JW, Symons TB, Vandervoort AA. Geriatric fitness: effects of aging and recommendations for exercise in older adults. Cardiopulm Phys Ther J. 2005;16:20–31.
Ilmarinen JE. Aging workers. Occup Environ Med. 2001;58:546–52. doi:10.1136/oem.58.8.546.
Asogwa SE, Granda Ibarra A, Izmerov N, Kumashiro M, Ramachandran CR, Rantanen J, Su Z. Aging and workforce capacity. World Health Organization: Technical Report Series No. 835. 1993. p. 1–55.
Gall B, Parkhouse W. Changes in physical capacity as a function of age in heavy manual work. Ergonomics. 2004;47:671–87. doi:10.1080/00140130410001658691.
Darragh AR, Campo M, Olson D. Therapy practice within a minimal lift environment: perceptions of therapy staff. Work: A Journal of Prevention. Assessment, and Rehabilitation. 2009. (in press).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
King, P., Huddleston, W. & Darragh, A.R. Work-Related Musculoskeletal Disorders and Injuries: Differences Among Older and Younger Occupational and Physical Therapists. J Occup Rehabil 19, 274–283 (2009). https://doi.org/10.1007/s10926-009-9184-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-009-9184-1