Abstract
Purpose The purpose of this study was to examine the prevalence and risk factors of occupational musculoskeletal injuries (OMIs) among occupational therapy practitioners over a 12-month period. Method A self-administered questionnaire mailed to 500 randomly selected practicing occupational therapists (OTs) and occupational therapy assistants (OTAs) living in the state of Texas. Results A response rate of 38 % was attained with 192 questionnaires returned. In a 12-months working period, 23 % of occupational therapy practitioners experienced musculoskeletal injuries. Muscle strain (52 %) was most reported injury and lower back (32 %) was most injured body part. Years of practicing experience (t = 2.83, p = 0.01), and age x2(2, N = 192) = 8.28, p = 0.02 were found as significant factors associated with injuries among OTAs. No factors were significantly associated with injuries among OTs. Conclusion Patient handling was the primary factor associated with injuries. Also, minimal experience and older age were concluded as risk factors that might contribute to OMIs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Occupational musculoskeletal injuries (OMI) among health care practitioners became a concern to researchers in more than a decade to determine the prevalence and risk factors [1–6]. In 2011, the Bureau of Labor Statistics reported the health care industry with the highest rate in injuries (592 cases in 1000) exceeding manufacturing and transportation and warehousing [3]. Increasing the demands for health care services and the nature of work including physically demanding activities placed health care providers at high risk for OMI [4, 5].
Evidence of OMIs among occupational therapy practitioners is occasionally studied and little understood in concern with prevalence and risk factors [5]. There is a great need to examine the work environment of occupational therapy practitioners because their working conditions are physically demanding due to the necessity of manually lifting and transferring of patients and equipment. Also, occupational therapy practitioners often provide treatment to individuals with physical and developmental disabilities whose treatments typically demand substantial physical effort [5, 6]. Therefore, the purpose of this study was to investigate the prevalence of OMIs among occupational therapy practitioners in the health care environment and to examine the risk factors associated with the injuries.
Background
Few occupational therapy research studies examined the prevalence of OMI among occupational therapy practitioners. They [5–11] found that manual patient handling, lifting and transferring were the most common work activities and risk factors associated with OMIs among health care practitioners despite receiving training on safe patient handling, lifting and transfer in their educational programs. Darragh et al. [6] who examined the prevalence of work-related injuries among occupational therapy practitioners identified more hours of work and patient direct contact as an additional risk factors. Also, Passier and McPhail [12] identified patient handling, work postures, lifting, carrying, and repetitive tasks as risk factors of work-related musculoskeletal disorders among occupational therapy practitioners. Moreover, Alnaser’s systematic review of OMIs [5] identified that work activities of health care professionals including occupational therapy, physical therapy, and nursing demanded high mental concentration, and paying attention to the client’s physical capacity and cognitive function, which were likely to place practitioners under pressure and risk for OMIs.
Research studies in the field of physical therapy and nursing concluded that muscles strains and sprains were the most common types of OMIs. Also, they found that the majority of OMIs occurred in the low back and injuries were reported in varying frequencies in all body parts. In addition, they identified manual patient handling to be the primary risk factor associated with OMIs [2, 8–13]. Also, Nelson et al. [10] and Tabone [11] specifically identified manual patient handling as placing the patients and nurses at risk for injuries. Moreover, Salik and Özcan [2] concluded that inexperience and physical demands of practice placed young physical therapists at higher risk for OMIs.
Research studies concluded that more than 50 % of injured occupational therapists, physical therapists and nurses did not report their OMIs in order to avoid stigmatization, discrimination, and poor performance rating. Some practitioners indicated that they were too busy to report their injuries or they felt becoming accustomed to accidents. Others believed that reporting their injuries might jeopardize current and future career opportunities, thereby working with pain [2, 5–12, 14]. Accordingly, Cromie et al. [7] found that <7.5 % of physical therapists respondents had claimed worker’s compensation.
King et al. [15], Alnaser [5], Cromie et al. [7], and Hollingdale [9] explained that occupational therapists, nurses and physical therapists with OMIs developed response strategies to lessen the symptoms and to prevent future episodes. Physical therapy, occupational therapy, and nursing practitioners’ response strategies included changing work habits and activities; using proper body mechanics; avoiding prolonged awkward postures; avoiding stressful positions during treatment sessions to prevent aggravation or recurrence of injuries [2, 5, 6, 13, 14], reducing direct contact with patients and changing work setting [15, 16], participating in educational courses and trainings on proper lifting techniques and use of lifting mechanical devices; developing the habit of asking coworkers for help; reducing workload; and engaging in strengthening exercises [2, 13].
Method
Participants
The Texas Board of Occupational Therapy Examiners (TBOTE) database was used to contact the occupational therapy practitioners. A total of 500 practitioners were randomly selected from the database. Using a random number table, participants were equally split between OTs and OTAs. Inclusion criteria included having at least 1 year of clinical experience and working as a therapists for at least 1 month during the past 12 months. For this sample size, a margin of error was ±4.2 % at a 95 % level of confidence which reflected our high certainty in the results of this study.
Instrumentation
The survey, which was adapted from Holder et al. [8], was a self-administered questionnaire with closed-ended questions. It was reviewed by expert panel and was tested for face and content validity and test–retest reliability. Minor modifications were incorporated in the instrument to fit the population and purpose of this study. The modified survey included three sections. Section I was a self-report of OMIs sustained in the past 12 months including types of injuries, injured anatomical areas, work settings, activities provoking injuries, reporting of injury, treatment, loss of work time, symptoms exacerbating activities, and responses to injuries. Based on the literature review, a list of possible responses were included to the question with regard to reporting of injuries in order to speculate on reasons for not reporting. Also, more responses were added with regard to strategies taken to avoid future injuries in order to include most possible selections. Section II was a self-report inquiring about the psychosocial issues experienced by the participants. These information were used for an anticipated follow up study. Section III included demographical questions such as age, years of experience, practice setting, hours in direct contact with patients, gender, height, and weight.
A respondent reporting no episode of OMI in the previous 12 months was asked to skip Section I and II and to respond to Section III only. If a respondent answered “yes” to injury, then he/she was instructed to complete all three sections.
Procedure
Approval from the Institutional Review Board of Texas Women’s University was obtained. A copy of the survey, consent form, self-addressed, and stamped envelope to encourage responding were mailed to the 500 randomly selected occupational therapy practitioners. Follow-up reminder letters were sent to non-respondents after 2 weeks. All responses were confidential.
Study Design
A cross-sectional design was used in this study. OMI defined as a sudden or cumulative injury occurs at the workplace and effects the musculoskeletal system (muscles, bones, ligaments, and connective tissues) and nervous tissues. By definition, OMI produces aches, pain, and/or discomfort for 3 days or more leading to one or more of the following: limitation in execution of work tasks, restriction in participation in daily life activities and roles, requiring medical treatment and/or resulting in time off from work. In this study, all variables relating ot OMIs were self-reported. The main variables of examination included symptoms of OMIs, body part injured, activities linked with OMIs, and practice setting; and actions taken after injury. Variables were measured on a nominal scale.
Data Analysis
The Statistical Package for the Social Science (SPSS) [17] was used for analysis. Descriptive statistics were used to summarize the demographics and OMIs of the respondents. Chi square tests was executed to determine an association between the two levels of practitioners in terms of their age and weight. In order to use Chi square, age and weight were categorized in increments of ten by years and pounds to establish if any particular group had a greater risk for OMI. An independent t test was performed to determine the differences in years of experience and direct patient contact between the injured and non-injured practitioners. Alpha level was set at p ≤ 0.05.
Results
Participants
Eligible for analysis were 192 questionnaires resulting in 38 % response rate, which was a realistic response rate of most research studies [18]. Occupational therapists completed 130 surveys (68 %) and occupational therapy assistants completed 62 surveys (32 %). The mean age was 39.53 ± 8.91 years. Male respondents were 17 (9 %) and female respondents were 175 (91 %), which represent the typical distribution of occupational therapy practitioners by gender. Table 1 illustrated the practitioners mean and standards deviations with regard to age, years of experience, and hours in contact with patients.
OMIs Among Occupational Therapy Practitioners
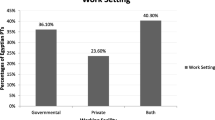
Overall, 44 practitioners (23 %) experienced OMIs within the 12-month duration. Muscle strain (52 %) was most reported injuries and the low back (32 %) was most injured body part (See Table 2). Also, hospitals (30 %) and rehabilitation centers (18 %) were most common settings to find OMIs and followed by private practice (16 %) and skilled nursing facility (14 %).
Twenty three percent of OTs (n = 30) experienced OMIs in the past 12-months. OTs with injuries indicated that muscle strain (67 %) was most occurring injury and the low back (37 %) was most injured body parts (See Table 2). The majority of OTs with injuries experienced OMIs in hospitals (40 %) followed by rehabilitation centers (20 %). Between injured and non-injured OT respondents, the independent t test showed no significant differences for years of experience (µ = 12.12, SD = ±8.30), t(129) = 0.54, p = 0.59, and direct contact hours, (µ = 22.65, SD = ±12.70), t(129) = −1.42, p = 0.16. Additionally, age with x2(2, N = 192) = 3.68, p = 0.29 showed no association with occurrences of injuries among OTs.
With regards to OTAs (n = 14), 23 % suffered from OMIs during the 12-month period. OTAs with injuries specified ligament sprain (29 %) as most common injury and wrist and hand (27 %) as the main injured body parts (See Table 2). Injuries among OTAs were largely identified in skilled nursing facility and private practice (29 %).
Although the independent t test showed no significant difference in the number of direct patient contact hours for OTAs (µ = 28.0, SD = ±12.72), t(61) = −1.18, p = 0.25. There was a significant difference in years of experience between injured and non-injured OTA respondents (µ = 8.87, SD = ±5.69), t(61) = 2.83, p = 0.01 (see Table 3). In addition, age (x2(2, N = 192) = 8.28, p = 0.02) was associated with injury among young (24–33 years old) OTA respondents (see Table 4). However, the association was weak based on Cramer’s V, v = 0.37.
Activities Associated with OMIs
Table 5 illustrated that occupational therapy practitioners performed activities that increased their risk for injuries. Reported activities included lifting (21 %) and transferring (20 %) of patients. These two activities were most common activities being performed when respondents were injured. In addition, 52 % of the injured respondents indicated that exacerbation and recurrence of symptoms were due to continued clinical practice. Also, they reported that maintaining a position for prolonged periods (18 %), transferring (13 %), and lifting (12 %) aggravated the symptoms when they returned to work.
Responding to Injury
Results showed that 58 % of OTs and 71 % of OTAs with injuries did not officially report their injuries. Table 5 illustrated the reasons for disregarding to report the injuries. OTs (31 %) indicated that they became used to being injured and OTAs (21 %) reported that they were too busy to report their injuries. In addition, OTs (46 %) and OTAs (35 %) sought medical treatment from physicians. Moreover, OT and OTA respondents (<30 %) missed half day or more from work due to their injuries. However, the majority of respondents (>85 %) indicated that they practiced some physical responses such as improving their body mechanics and exercising and they applied behavioral changes such as asking for help from other personnel or limiting patients contact to prevent reoccurrences of the injuries (See Table 5).
Discussion
The results of this study showed that nearly one-fourth of occupational therapy practitioners experienced OMIs in a 12-month duration. This percentage of injury is alarming and deserves immediate attention to develop strategies and policies to eliminate or reduce the number of injuries.
This study supported previous findings that the back strain was one of the most common type of injury for health care professionals including occupational therapy, physical therapy and nursing [2, 5–10, 14, 19]. The high incidence of low back, shoulder, and knee injuries were likely due to patient handling that demands significant physical effort. Lifting and transferring of patients were the most reported activities performed when injuries occurred in addition to maintaining prolonged posture and awkward positions, and performing repetitive tasks. These findings were also concluded by other studies [2, 5–8, 14, 19]. In addition, these injuries were more common among OTAs than OTs (see Table 1) which were likely do to the nature of the OTAs roles including carrying out the treatment plans, putting significant hours of interaction with patients, preparing equipment and assessment tools, and transferring patients to the therapy rooms as would be instructed by the OTAs.
The present study found that respondents experienced episodes of OMI most frequently in hospitals. Similar conclusion was developed by Darragh et al. [6], Salik and Özcan [2], Bork et al. [14] and Holder et al. [8]. A possible explanation is that patients with more acute conditions and more dependent status are likely to be found in occupational therapy units at hospitals. These types of patients need more care and handling that compel occupational therapy practitioners to exert greater physical effort.
Years of experience showed a significant association with OMIs among OTAs. Possible explanation was that newly graduate OTAs might not have enough experience with practical methods of transferring or lifting. Also, age of OTAs was found significantly associated with OMI; however, the association was weak. Fifty percent of respondents with injuries were between the age of 24 and 33. Likely justification was that young OTAs might be reluctance to ask for help and be eager to demonstrate their skills and independence. In fact, research studies have found that the highest reported episodes of OMIs were among younger health care practitioners [2, 5].
The majority of respondents did not officially report their injuries, which consistent with the findings by Darragh et al. [6], Cromie et al. [7], and Holder et al. [8]. Surprisingly, they stated that they “became accustomed to injury,” which was an indication that injuries were expected due to the nature of the work activities that demanded great physical effort and treatment of a large number of patients. Some practitioners simply did not have the time to report their injuries, which likely due to having heavy workloads. Others OT practitioners indicated that they experienced the symptoms of their injuries few days later when it was too late to report the injury. Most institutions’ policies would deny any injury claim after leaving the work premises or 24 h after the incident.
Unfortunately, more than half of respondents with injuries indicated that their symptoms were aggravated due to continued clinical practice. Respondents reported that they continued to work, despite pain and before gaining full recovery. The reasons seemed to be multiple including: (1) an insufficient number of days of sick leave, (2) financially unable to recover without pay, (3) feelings of guilt for making others to carry out their workloads, (4) fear of stigmatization by co-workers, (5) to avoid being perceived as incompetent, and (6) fear of job loss.
Similarly, less than 50 % of the respondents with injuries consulted physicians for medical advice. Possible reasons for not seeking medical treatment were feelings of embarrassment of being in the medical field and getting injured, attempting to self-diagnose and to self-treat the injuries, or to seek treatment from co-workers, which were similarly found among other health care providers [2, 5, 16].
In this study, the majority of the occupational therapy respondents with injuries reported developing response strategies as a result of the experiencing injuries. These response strategies seemed to be a natural behavior that allowed changes in the person’s behaviors, occupational activities and/or environment in order to regain full control, to improve performance, and to prevent future injuries.
Limitations
First, the survey consisted of only closed-ended questions, which did not provide the respondents with opportunities to further express valuable information regarding their experiences. In addition, it was a self-report survey, so there were great amount of subjectivity in which the responses were subjected to selection bias and recall bias. Also, this cross sectional study could not provide information about the cause of injuries; it could only provide an association between variables. Finally, 38 % response rate could reflect the presence of a biased sample. Therefore, future studies might include a larger sample size that covered more states to generate more robust data.
Conclusion
Patient handling was the primary factor associated with OMIs, and symptoms of injuries were exacerbated by continued practice. Inexperience (6 years or less) and young age (33 or less years) were found to be significantly associated factors with OMIs among occupational therapy assistant respondents only, indicating that this level of practitioners might need more training to avoid injury. Results also concluded that different response strategies were used by both levels of practitioners to lessen their injury, prevent future episodes and improve performance. Similar findings were established among other health care professionals including physical therapists and nurses.
Based on the findings, several recommendations of this study are made. First, developing prevention and wellness programs to reduce OMIs are needed. Successful programs may increase productivity, reduce cost of injuries, and improve quality of care. Health care organization may need to consider enacting “maximum-manual-lift” and “maximum workload” legislative policies in all practice environments. “maximum-manual lift” implies that health care professionals are not required to lift clients at certain weight, currently defined as 35 pounds [20]. Use of mechanical lifts and transfer equipment may be effective strategy for prevention of OMI in occupational therapists, but additional research on this topic is necessary. In addition, “maximum workload” policy should set a maximum number of clients to be seen in 1 day and allow health care professionals the right to refuse additional clients. Educational programs need to consider courses in safety and OMI prevention that would protect the practitioner as well as the patient from injuries.
Future research studies should attempt to evaluate the effectiveness of prevention programs aimed at reducing episodes of OMIs among occupational therapy practitioners as well as other health care providers. The psychosocial issues that usually accompany OMIs are another area in need of investigation.
References
Bureau of Labor Statistics, U.S. Department of Labor. Workplace injuries and illnesses in 2012. (Publication No. 13-2257). Washington, DC; 2013.
Salik Y, Özcan A. Work-related musculoskeletal disorders: a survey of physical therapists in Izmir-Turkey. BMC Musculoskelet Disord. 2004;5(1):27–35.
Bureau of Labor Statistics, U.S. Department of Labor. 2011 survey of occupational injuries and illnesses: summary estimates charts package. Washington, DC; 2012.
Bureau of Labor Statistics, U.S. Department of Labor. Occupational outlook, 2010–2011 Edition, occupational therapists, on the internet at http://www.bls.gov/oco/ococ078.htm (2011).
Alnaser MZ. Occupational musculoskeletal injuries in the health care environment and its impact on occupational therapy practitioners: a systemic review. Work. 2007;29(2):89–100.
Darragh AR, Huddleston W, King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am J Occup Ther. 2009;63:351–62.
Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 2000;80(4):336–51.
Holder NL, Clark HA, DiBlasio JM, Hughes CL, Scherpf JW, Harding L, et al. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapists assistants. Phys Ther. 1999;79(7):642–52.
Hollingdale R. Back pain in nursing and associated factors: a study. Nurs Stand. 1997;11(39):35–8.
Nelson A, Owen B, Lloyd J, Fragala G, Matz M, Amato M, et al. Safe patient handling and movement: preventing back injury among nurses required careful selection of safest equipment and techniques. The second of two articles. Am J Nurs. 2003;103(3):32–43.
Tabone S. Safe patient handling. Tex Nurs. 2005;79(3):10–1.
Passier L, McPhail S. Work related musculoskeletal disorders amongst therapists in physically demanding roles: qualitative analysis of risk factors and strategies for prevention. BMC Musculoskeletal Disorders. 2011;12:24.
de Castro AB. Handle with care: the American Nursing Association’s campaign to address work-related musculoskeletal disorders. Online J Issues Nurs. 2004;9(3):103–18.
Bork BE, Cook TM, Rosecrance JC, Engelhardt KA, Thomason MJ, Wauford IJ, et al. Work-related musculoskeletal disorders among physical therapists. Phys Ther. 1996;76(8):827–35.
King P, Huddleston W, Darragh AR. Work-related musculoskeletal disorders and injuries: differences among older and younger occupational and physical therapists. J Occup Rehabil. 2009;19:274–83.
Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders and culture of the physical therapy. Phys Ther. 2002;82(5):459–72.
IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.
Portney LG, Watkins MP. Foundations of clinical research: application topractice. Norwalk, Connecticut: Appleton & Lange; 2008.
Alrowayeh HN, Alshatti TA, Aljadi SH, Fares M, Alshamire MM, Alwazan SS. Prevalence, characteristics, and impacts of work-related musculoskeletal disorders: a survey among physical therapists in the State of Kuwait. BMC Musculoskelet Disord. 2010;11:116–27.
Water TR, Putz-Anderson V, Gerg A. Applications manual for the revised NIOSH lifting equation. DHHS (NIOSH) Publication No. 94–110. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 1994.
Conflict of interest
Author, Musaed Z Alnaser, declares that has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alnaser, M.Z. Occupational Therapy Practitioners with Occupational Musculoskeletal Injuries: Prevalence and Risk Factors. J Occup Rehabil 25, 763–769 (2015). https://doi.org/10.1007/s10926-015-9584-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-015-9584-3