Abstract
Introduction: The purpose of this study was to investigate if work-related musculoskeletal disorders (WMSDs) are associated with increased health care use, over and above workers’ compensation health care benefits, in the period prior to and following a workers’ compensation claim indicating gradual progression and declining function associated with musculoskeletal morbidity. Methods: This study employed secondary analysis of employment data, workers’ compensation claim data and provincial (universal) medical services data for a cohort of health care workers; and investigated rates of medical care contacts among injured workers with a WMSD claim (n=549) compared to a matched group of non-claim workers. Predictors of health care contacts were estimated using general linear regression. Results: WMSD injured workers had significantly higher rates of health care contacts associated with a claim compared to non-injured workers, over and above workers compensation health care benefits. In the final multi-variable model, a WMSD claim among injured workers was associated with an estimated 69% (95% CI, 1.50, 1.91) increase in health care use for the 12-month period immediately after the injury date compared to non injured workers. Conclusion: The pattern of visits for WMSDs suggests that workers visit general practitioners as part of an ongoing pattern of symptoms, resulting in frequent utilization of health services prior to work disability that is also reflected in health care contacts after return-to-work.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Musculoskeletal disorders are a major source of workplace disability in developed countries [1] accounting for a considerable economic burden of illness [2]. For those judged to be work-related through workers’ compensation systems, claims for work-related musculoskeletal disorders (WMSD) account for the highest years of productivity loss in the United States [3]. In Canada, musculoskeletal sprains and strains comprise approximately 50% of time loss claims for workers [4]. Yet such indicators are likely incomplete as evidenced by studies that examine a variety of data sources for surveillance of occupational disease [5]. Health care utilization studies using sources beyond compensation claim data have demonstrated broader impacts of occupational disease [6] including for WMSDs [7, 8]. Although traditionally framed in workers’ compensation circles as more acute events or ‘injuries’, proposed models of musculoskeletal morbidity suggest these disorders are more gradual in onset with fluctuations in disability and severity [9] associated with a variety of aggravating factors [10]. Yet empirical data to support such models is limited.
Within workplace or occupational studies, there is a reliance on the investigation of workers’ compensation outcomes (e.g. start of claim for etiologic studies or return-to-work/claim closure for rehabilitation/clinical studies). However, studies of health care utilization suggest that visits to general practitioners may provide an early indication of musculoskeletal morbidity [11, 12] with relevance to epidemiological research and prevention programs, or may persist along a disability trajectory [12, 13] with relevance to clinical research and rehabilitation programs. However, only a few of these studies are specific to workplace injuries and occupational populations [14, 15]. A greater understanding of health care utilization patterns among workers is warranted. For research on the epidemiology of musculoskeletal outcomes and for the development of prevention programs, it is important to understand the earliest onset of symptoms associated with work characteristics and work disability. For research on clinical outcomes and for the development of health care and rehabilitation services, it is important to know how and when musculoskeletal symptoms affect the decision to seek medical attention along the disability trajectory and relative to work disability or return-to-work outcomes [15].
We had an opportunity to describe more fully health care utilization associated with WMSDs and examine evidence related to more extended models of WMSDs through use of a unique data set, the British Columbia Linked Health Database (BCLHD). We could isolate medical services billed to the publicly-funded health care system that represent additional services beyond those covered by workers’ compensation benefits as an indicator of an episodic progression of musculoskeletal morbidity. We focused on a group of hospital workers because of the ongoing burden of WMSDs in the health care sector [16], slower declines in workers’ compensation claims for this group [17] and long-term disability claims almost double that of other sectors [18]. Our primary hypothesis was that health care utilization for WMSDs, over and beyond that paid for by workers’ compensation systems, would be higher among injured hospital workers with WMSD claims in comparison to a group of workers without any claims, controlling for relevant confounders.
Methods
Design
This was a retrospective follow-up study (1987–1997) whereby existing employee records, workers’ compensation records and provincial health care billing records were linked together in order to investigate the patterns of health care use associated with WMSD claims among a study group of hospital workers and a comparison sample of hospital workers without claims.
Data sources
The data were derived from two sources: the human resources database of a large acute care hospital in the lower mainland of the Canadian province of British Columbia and the BCLHD. The hospital’s employee records permitted delineation of the entire study sample, excluding physicians and students who were not employed directly by the hospital. The workforce was restricted to those who had been employed at the hospital for at least one year between 1987 and 1997 (n=5,029). These years were chosen based on the availability of health care utilization data.
In British Columbia, access to health care billing records and workers’ compensation records for research purposes is made possible by application to the Ministry of Health according to their Access Policy for Research Uses of Linked Health Data [19]. The BCLHD, developed by the Centre for Health Services and Policy Research (CHSPR) at the University of British Columbia under contract to the Ministry of Health makes key health care files in the province linkable to one another for the purposes of research [20], including the medical services billing records file and the workers’ compensation claim file. CHSPR confidentially linked our hospital employee sample with their health care and compensation records for the years 1987–1997, achieving 97% coverage of hospital employees linked to the BCLHD. CHSPR then provided the linked data set to the research team with all unique identifiers removed from the records.
Study sample
From our health care worker cohort (n=5,029), we identified all workers with a workers’ compensation claim between 1987 and 1997. Workers’ compensation claims were restricted to time-loss, short-term disability claims, those where a payment is made for lost income (versus health care claims only) and the worker was expected to return to work (versus permanent disability awards) (n=1,581 claims).
Claims were restricted to the first occurrence where multiple claims were recorded per person during the follow-up period (n=907). We were interested in capturing musculoskeletal sprains and strains more typically associated with the cumulative effects of work and recurrent or episodic in nature. Using classification lists developed by others [21, 22], we identified musculoskeletal disorders from International Classification of Diseases 9th Revision [23] diagnoses codes included in claim records. Among WMSD injured workers (n=627), we excluded claims with a 1987 injury date to assure that this employee sample was claim free for at least one year and to reduce the prior claim effects on health care use, and those with an injury date in 1997 to allow a minimum of one year of follow-up for health care utilization (final sample = 549). The study sample is summarized in Fig. 1.
A comparison group of non-injured workers was randomly selected from the subset of the hospital workforce with no workers’ compensation claim during the entire follow-up period. The comparison group of non-injured workers was age- and gender-matched to the injured worker group using a 1:1 matching procedure.
Measurement of health care utilization
We were interested in the individual-level use of publicly-funded health care services above and beyond those health services reimbursed by the workers’ compensation system for our study sample of injured workers and the comparison sample of non-injured workers. Information was available on all fee-for-services payments to physicians and alternate providers by the Ministry of Health in British Columbia from 1987 to 1997 inclusive. At the individual level, a health care contact was defined by a unique combination of the service billing date and the provider code. For example, an individual with multiple billing records on the same day seeing a single provider was counted as one contact. A unique billing record defined a health care service. For example, the provision of a General Practitioner (GP) examination plus two pathology tests regardless of the provider or the date was counted as three services. Contacts and services were enumerated for providers relevant in the treatment of musculoskeletal morbidity (GP, specialist, chiropractor, physical therapist and massage therapist).
Initially, the mean rate (# per person per year) of health care contacts and services was analyzed by calendar year from 1987 to 1997 to identify temporal trends in utilization. Then, building upon the work of Hertzman and colleagues [24], we constructed individual trajectories of health care utilization based on 12-month follow-up periods. To permit valid comparisons, utilization was aggregated for the same time periods for WMSD injured workers and for matched non-injured workers. We chose the claim injury date as the aggregation start date for each worker and matched non worker. All aggregation and rates calculation were conducted in SAS [25].
Analyses
Initially, sequences of rates over corresponding 12-month periods were graphed for the WMSD claim group and the matched non-claim group to permit visual inspection. T-tests were conducted to compare the mean annual rate of contacts and services pre and post injury date and between claim and comparison group.
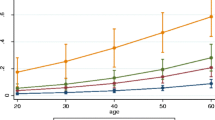
To arrive at adjusted estimates of the effect of claim status, regression analyses were conducted on the number of health care contacts, using the combined WMSD claim and non-claim groups as the analytical sample. For the regression analyses, we used the negative binomial model to account for the over dispersion of the distribution of number of health care contacts (variance-mean ratio ranged from 4 to 9 for each 12-month period). When data are over dispersed, the estimates from the Poisson regression model are inefficient with underestimated standard errors and overestimated chi-square statistics. The negative binomial model is a generalization of the Poisson model and it produces efficient estimates when mean-variance equality of the Poisson model is not met [26]. The likelihood-ratio test comparing the Poisson model to negative binomial model supports the use of the negative binomial model at the 0.01 level.
Separate models were run for each 12-month period before and after injury date/comparison date, exhausting the years of data available. Variables included in the model were selected based on evidence of an association with musculoskeletal disorders in the literature and on the data available in the administrative data files (job tenure, occupation, prior hospitalization—study groups were already matched on age and gender). Pearson chi-square tests for each model indicate a good fit to the data with the ratio of the goodness-of-fit chi-squares to its degrees of freedom ranging from 1.05 to 1.28.
Results
Study sample
The WMSD claim group and comparison non-claim group had similar age and gender distributions (Table 1). The WMSD claim group had a higher representation of care aides (24.2%) and support services occupations (19.9%) than the comparison group. Ninety-four percent of all WMSD claims were categorized as sprains and strains. Over half (53%) involved the back, 17% the upper-limb, 12% the lower-limb and 7% involved the neck. The WMSD claim group was representative of the overall claim population at the hospital. The overall claim population had a comparable percentage of women (72.2%) and mean age at time of injury (39.9 years, SD 9.7) to the WMSD sub sample. Registered nurses were overrepresented in the WMSD claim group (40.8%) compared to the overall claim population (29.6%), while support services workers were underrepresented in the WMSD claim group (19.9% verses 29.6% in the overall claim population). The majority of injuries in the overall claim population involved musculoskeletal diagnoses (93.0%), although these involved sprains and strains of interest in this study (72.7%) as well as acute musculoskeletal injuries such as fractures, dislocations and contusions (20.2%). Less than 1% of all claims were for infectious diseases, acute stress reactions, burns, diseases of the sense organs (e.g. hearing loss), hernias, contact dermatitis and other unspecified conditions respectively.
Health care utilization
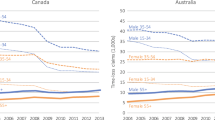
Health care utilization in the study sample was comparable to that based on health care utilization records of respondents in the 1994 National Population Health Survey [27]. For example, the overall mean number of GP contacts was 6.53 per year among the entire study sample compared to 5.92 contacts per year among all female survey respondents. Rates of health care contacts for the WMSD claim group (5.82 GP contacts/year pre injury and 7.02 contacts/year post injury) were also comparable to other studies [28] of health care utilization among disability groups (7.4 GP/specialist and chiropractor visits/year for individuals with low back disability claims). Overall, virtually all health care utilization increased over time (Fig. 2 for general practitioner (GP) contacts). Examination of the data by calendar year indicated that this was not a secular trend but rather an age-related trend.
Comparison of health care contacts
The WMSD claim group had significantly higher rates for most health care contacts regardless of the type of provider. In particular, in the pre-injury follow-up periods, the WMSD claim group had significantly (p < 0.001) more GP contacts per 12-month observation period (average 5.82/period, SD=0.10) than the matched non-claim group (average 4.13/period, SD=0.09) (Fig. 2). As well, the WMSD claim group had significantly more contacts during the post-injury follow-up periods compared to the pre-injury follow-up period (average 7.01/period, SD 0.14), whereas rates of health care contacts did not change significantly from the pre-injury follow-up period to the post-injury follow-up period for the non-claim group (4.32/period, SD 0.12).
For the WMSD claim group, the average number of contacts per 12-month period increased gradually, rising from 5.57 GP contacts at the start of follow-up to 6.28 GP contacts immediately preceding the claim date. The average number of contacts increases significantly for the 12-month period immediately following the claim date to 7.2 GP contacts. Although the number of contacts starts to decline post-injury, the rate remained higher than pre-injury levels with 6.73 GP contacts at the end of follow-up.
Similar trends of higher utilization among the WMSD claim group compared to the non-claim group and of higher utilization following the injury date for the claim group were observed for chiropractor, physiotherapist, specialist, and massage therapist contacts. For example, massage therapy increased significantly (p < 0.001) from 2.6 contacts per person several years prior to the injury date up to 16.4 contacts per person in the period immediately before the injury date (Fig. 3). In contrast to the other types of providers, there was a notable drop in contacts immediately after the injury date. This may be attributable to a transfer to workers’ compensation health care utilization following the initiation of a disability claim. This pattern was not observed among the non-claim group. For example, the non-claim group had significantly fewer contacts per year on average with massage therapists (p < 0.01) than the WMSD claim group, both for the pre-injury date follow-up periods (5.41 contacts/year, SD 0.47) and the post injury follow-up periods (6.24 contacts/year, SD 0.50).
Comparison of diagnostic services
Overall, there were no significant differences in the number of radiology services, pathology services or other diagnostic services used by the WMSD claim group compared to the non-claim group, either before or after the injury date (results not shown).
Adjusted estimates of claim effects
In the final multi-variable models controlling for job tenure, occupation, and prior hospitalizations, having a future WMSD claim was associated with an estimated 49% increase (95% CI 1.31, 1.69) in general health care utilization for the 12-month period immediately preceding the injury date compared to never having a claim (Table 2). The effect of claim status are evident during the 6 years leading up to the injury date, but not prior to this (OR=1.29, 95% CI 0.92, 1.79 for seven years pre-injury).
Claim status was further associated with an estimated 69% increase (95% CI 1.50, 1.91) in health care contacts for the 12-month period immediately after the injury date (Table 2). The effect of claim status remains significantly elevated for all 12-month follow-up periods after the injury date (OR=1.45, 95% CI 1.19, 1.78 for seven years post-injury) in comparison to those without a claim. Although the effect size diminishes with time, it only begins to return to pre-injury levels at five years post-injury (OR=1.44, 95% CI 1.22, 1.69).
Pearson chi-square tests for each model (i.e., 12 month follow-up periods for rates of health care contacts) indicate a good fit to the data (test statistic divided by the degrees of freedom range from 1.05 to 1.28). Although nursing care aides, support service workers such as housekeeping and dietary aides, and clerical workers each had several odds ratios significantly above 1, fit of models with job tenure and occupation variables were not significantly different from models with these variables excluded.
Discussion
Our study found that a WMSD claim among hospital workers was associated with increased publicly-funded health care use, over and above workers’ compensation health care use, both before and after injury date in comparison to non injured hospital workers. Descriptive differences in health care utilization profiles over time were most remarkable for the main source of primary care in Canada—general practitioners. The rate of GP contacts per person per 12-month period tended to increase gradually over time during the periods leading up to the injury date, with a significant increase in utilization after the injury date. Although the rate of contacts per person per 12-months started to decrease after the initial 12 month period post injury, it never returned to pre-injury levels. This was consistent with findings from the pioneer study investigating health care use among injured workers in British Columbia across industries and injuries [24].
In the final multi-variable models, WMSD claim status significantly predicted increased contacts with the health care system after adjustment for demographic characteristics, occupation, and prior hospitalizations (co-morbidity measure). The effect size was elevated for six years leading up to the injury date, peaked after the injury date and was sustained for the entire follow-up period after the injury date.
This unique dataset provided an opportunity to describe the potential shifting of health care to the publicly-funded health care system from the workers’ compensation system for episodic or recurrent conditions such as WMSDs, both before a worker goes on work disability benefits, and after when a worker returns to the job following a work-related injury, lending support to a model of gradual progression or functional decline associated with musculoskeletal morbidity overtime.
Observed increases in health care utilization among the WMSD claim group is consistent with recent findings from the National Ambulatory Medical Care Survey (NAMCS) in the United States [29]. Results indicated that patients with a work-related condition had significantly increased odds of receiving certain types of health care including x-rays, physical therapy, and counseling during a physician visit, compared to patients for non-work related conditions. Similar findings were observed for those patients specifically with work-related injuries, although separate models were not constructed to compare musculoskeletal injuries to acute injuries. The NAMCS did not allow for long-term follow-up of health care utilization. A follow-up study of health care costs during periods of work disability for occupational low back pain [14] indicated increasing costs with the length of time on compensation (disability windows from <30 days to >180 days). The top three sources of health care costs were diagnostic procedures, surgery and physical therapy. We did not find a significant increased risk of diagnostic services associated with a WMSD claim in this study. It may be that increases in these types of services are captured by windows closer to the claim date and by the workers’ compensation system rather than the publicly-funded health care system.
Liss and colleagues [30] found that workers with compensation claims for occupational asthma, another chronic and recurrent condition, suffer higher rates of hospitalizations than other workers. As well, Williams and colleagues [14] reported increasing surgical costs (i.e., hospitalizations) among workers with occupational low back pain during the later periods of work disability (>180 days on disability payments). Our analysis did not focus on hospitalizations but rather out-patient services as a more sensitive measure of gradual progression or declining function of the musculoskeletal system. In fact, a sub-analysis of our data did not find an increased risk of hospitalization among the WMSD claim group compared to the non-claim group (data not shown).
The lack of an association with hospitalizations in this study may be a reflection of changes in medical practices during the study follow-up period. Lavis and colleagues [31] observed two major trends in hospital admission rates for neck or back problems between 1982 and 1992 within the Canadian context—a decrease for non-surgical hospitalizations by 52%, but an increase for surgically-treated hospitalizations by 14% (similar trends were observed in the US sample). The authors hypothesized that the decrease in non surgical hospitalizations may reflect an awareness of evidence that in-patient treatments (e.g., bed-rest and traction) are ineffective, and that many diagnostic tests that once required admission can now be done on an outpatient bases. Hospitalizations associated with surgical procedures may also not be a sensitive indicator of episodes of musculoskeletal symptoms among an active workforce, with workers opting to delay surgical procedures until after they retire as a last treatment option given the recovery period.
It was hypothesized that observed increases in health care utilization during and after a musculoskeletal injury might be work-related, even though they were not reimbursed by the workers’ compensation system but rather the publicly funded health care system. Dembe and colleagues [29], as part of the NAMCS study described above, estimated that 17.8% of visits for work-related conditions were paid for by sources other than workers’ compensation insurance. This is consistent with Canadian [32] and US studies [33] that have shown an under-reporting of workplace injuries to workers’ compensation systems.
The nature of these types of injuries may result in episodes of pain and discomfort prompting employees to see a health care provider for relief of symptoms prior to crossing a threshold where the symptoms necessitate time off work. As well, returning to work following a compensation claim with continued exposure to conditions associated with musculoskeletal morbidity compounded by existing tissue damage of the musculoskeletal system may also lead to continued episodes of pain and discomfort necessitating medical care [10]. Previous studies show that the majority of individuals reporting musculoskeletal conditions, including workers with musculoskeletal symptoms [15], seek medical care from a general practitioner [11, 34]. For recurrent conditions with episodes of pain that do not result in work absence but rather discomfort or work limitations, individuals may find it easier to visit their general practitioner for relief of symptoms rather than to pursue compensation benefits for health care. The episodic nature of these conditions may also explain the lack of an observed dose-response relationship in our data leading up to an injury (ORs ranged from 1.34 three years prior to injury to 1.65 five years prior to injury) with fluctuations in pain and symptoms depending upon various factors such as the nature of workplace exposures or clinical treatment. While we hypothesized increased health care utilization associated with musculoskeletal morbidity, the lack of a dose-response relationship does not provide strong evidence for a gradual progression leading to workplace disability. Future work investigating shorter windows such as 3 or 6 months prior to work disability may be more informative.
It should be noted that this dataset could not distinguish between incident cases and prevalent cases of WMSD. The injured worker group may have had prior workers’ compensation claims not captured by the data available for this study (pre 1987) that explained increased health care utilization. We were able to restrict our sample to individuals within a minimum of one-year without an injury and the majority of the study sample was claim free for more than 2 years. However, the majority of individuals who make a claim to the workers’ compensation system in British Columbia have more than one claim during their working history [24]. A better understanding of the precursors of work-related injuries may help explain the increased rates of health care utilization among injured workers in general, including their previous claim history, labour market experiences or other life course trajectories that we do not understand. For example, a study of self-reported health care utilization among adults in Belgium found that respondents with daily low back pain were more likely to report health care utilization (health visit, medication, x-ray, history) than respondents with less frequent pain [35].
As well, the injured workers with a WMSD claim appear to permanently increase their use of health care services following a claim in comparison to workers without a claim. This may be explained by a subsequent claim following their ‘first’ claim during the follow-up period. However, the patterns of increased health care utilization following a claim persisted for a sub-analysis of injured workers with only one claim during the follow-up period (data not shown).
Persistent use of health care services after a musculoskeletal injury may represent a cumulative burden of morbidity over the life course as a result of the chronic and persistent nature of the injury. As described by Hagberg and colleagues [10], repeated exposures in combination with existing tissue damage can produce additional damage and secondary responses that necessitate medical attention. This is consistent with the work of Williams and colleagues [14] describing increasing health care costs along the disability pathway (>180 days on compensation benefits). Many employees with back pain will have recurrences in the following year (20–44%) [36]. In a study conducted in an industrial setting in Sweden [37], 35% of all back pain episodes had recurred within 1 month, 70% within 2 months, and 86% within 3 months. In a prospective study of patients with upper-body musculoskeletal pain, half had additional episodes of pain defined by general practitioner visits during the next 12 months, and the total number of visits was double the annual average for patients at the same health care facilities [13].
The pattern of visits for WMSDs suggests that workers visit general practitioners as part of an ongoing pattern of symptoms, resulting in frequent utilization of health services prior to work disability that is also reflected in health care contacts after return-to-work. The significantly higher health care use beyond compensation benefits by workers with WMSD compensation claims in our study indicates more gradual onset and greater persistence than usually captured with the designation “injury”. As well, general practitioner visits may provide an early indicator of musculoskeletal morbidity prior to a workers’ compensation claim for the purposes of epidemiological research, and an indicator of ongoing morbidity after return-to-work for the purposes of clinical and rehabilitation research.
Limitations
According to Wong [38, pages 283–284], “the use of record linkage in occupational and epidemiological research has evolved and improved with the introduction of personal identifying numbers and the availability of larger and more complete databases. Routine analyses of such data could serve as an effective tool for surveillance or hypothesis generation.” However, because these databases are used for administrative purposes, limitations must be recognized.
At the time of the construction of the research database for this project, ICD-9 codes for medical records in the BCLHD were not available to researchers. As a result, it was not possible in the current analyses to limit general health care utilization to those services and contacts that have the most relevance to musculoskeletal morbidity (e.g., GP visits for back pain). Some of the observed excess health care utilization for the WMSD claim group may have been attributable to other medical conditions (e.g., heart disease). Attempts to control for the effects of co-morbid conditions on general health care utilization were made by including a variable for prior hospitalizations during the 12-month follow-up periods in the multi-variable analyses.
Exclusive reliance on administrative data results in missing data on several factors that influence health care utilization. For instance, unobserved individual health practices, privately funded rehabilitation interventions, and injury severity measures could confound any observed associations between claim status and general health care utilization. In this study, smoking status was unavailable in either the employee files from the workplace or the medical files from the BCLHD. However, smoking status would have to be associated with a WMSD claim to systematically bias the results. Studies investigating the link between smoking status and musculoskeletal injuries have been equivocal [39, 40]. As well, socio-economic status is an explanatory variable for health [41]. Occupation was used as a surrogate for differences in socio-economic status in the explanatory models. Increased health care utilization among nursing care aides, support service workers and clerical workers relative to managers, pharmacists and therapists, and registered nurses may reflect socio-economic differences across occupations. However, the small overall effect of occupation within the models may also reflect a relatively homogenous pay scale for the health care sector relative to other sectors in the jurisdiction of British Columbia.
References
Makela M, Heliovaara M, Sievers K, Knekt P, Maatela J, Aromaa A. Musculoskeletal disorders as determinants of disability in Finns aged 30 years or more. J Clin Epidemiol 1993;46(6):549–59.
Coyte PC, Asche CV, Croxford R, Chan B. The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res 1998;11(5):315–25.
Fulton-Kehoe D, Franklin G, Weaver M, Cheadle MA. Years of productivity lost among injured workers in Washington state: modeling disability burden in workers’ compensation. Am J Ind Med 2000;37(6):656–62.
Workers’ Compensation Board of British Columbia. Statistics 2002. Richmond, British Columbia: WCB of BC, 2002.
Silverstein BA, Stetson DS, Keyserling WM, Fine LJ. Work-related musculoskeletal disorders: comparison of data sources for surveillance. Am J Ind Med 1997;31(5):600–8.
Liss GM, Kusiak RA, Gailitis MM. Hospital records: an underutilized source of information regarding occupational diseases and exposures. Am J Ind Med 1997;31(1):100–6.
Liss GM, Armstrong C, Kusiak RA, Gailitis MM. Use of provincial health insurance plan billing data to estimate carpal tunnel syndrome morbidity and surgery rates. Am J Ind Med 1992;22(3):395–409.
Park RM, Nelson NA, Silverstein MA, Mirer FE. Use of medical insurance claims for surveillance of occupational disease. An analysis of cumulative trauma in the auto industry. J Occup Med 1992;34(7):731–7.
McGorry RW, Webster BS, Snook SH, Hsiang SM. The relation between pain intensity, disability, and the episodic nature of chronic and recurrent low back pain. Spine 2000;25(7):834–41.
Hagberg M, Christiani D, Courtney TK, Halperin W, Leamon TB, Smith TJ. Conceptual and definitional issues in occupational injury and epidemiology. Am J Ind Med 1997;32:106–15.
Biering-Sorensen F. A prospective study of low back pain in a general population III. Medical service-work consequence. Scand J Rehab Med 1982;15:89–96.
Badley EM, Webster GK, Rasooly I. The impact of musculoskeletal disorders in the population: are they just aches and pains? Findings from the 1990 Ontario Health Survey. J Rheumatol 1995;22(4):733–739.
Rekola KE, Levoska S, Takala J, Keinanen-Kiukaanniemi S. Patients with neck and shoulder complaints and multisite musculoskeletal symptoms—a prospective study. J Rheumatol 1997;24(12):2424–8.
Williams DA, Feuerstein M, Durbin D, Pezzullo J. Health care and indemnity costs across the natural history of disability in occupational low back pain. Spine 1998;23(21):2329–36.
Molano SM, Burdorf A, Elders LA. Factors associated with medical care-seeking due to low-back pain in scaffolders. Am J Ind Med 2001;40(3):275–81.
Workers’ Compensation Board of British Columbia. Health Care Industry: Focus Report on Occupational Injury and Disease. Richmond, British Columbia: WCB of BC, 2000.
Adam MH. Declines in claims frequency continues to offset market losses. ON Workers’ Compens 2001;11(2):1–4.
Canadian Institute of Actuaries. Canadian Group Long-term Disability Termination Experience 1988–1994. Committee on Expected Experience Group Life and Health. Ottawa, ON: Author.
British Columbia Ministry of Health and Centre for Health Services and Policy Research.. Access Policy for Research Uses of Linked Health Data. Vancouver, BC: Author, 1998.
Chamberlayne R, Green B, Barer ML, Hertzman C, Lawrence WJ, Sheps SB. Creating a population-based linked health database: a new resource for health services research. Can J Public Health 1998;89(4):270–3.
Beaton DE, Cole DC, Manno M, Bombardier C, Hogg-Johnson S, Shannon HS. Describing the burden of upper-extremity musculoskeletal disorders in newspaper workers: what difference do case definitions make? J Occup Rehabil 2000;10:39–52.
Coyte PC, Asche CV, Croxford R, Chan B. The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res 1998;11(5):315–25.
International Classification of Diseases (9th Revision). Practice Management Information Corporation: Los Angeles, California, 2003.
Hertzman C, McGrail K, Hirtle B. Overall pattern of health care and social welfare use by injured workers in the British Columbia cohort. Int J Law Psychiatry 1999;22(5–6):581–601.
Statistics for the Applied Sciences. SAS Procedures Manual. Cary, NC: SAS Institute Inc. 2002.
Allison PD. Survival analysis using the SAS system: a practical guide. Cary, NC: SAS Institute Inc., 1999.
Mustard CA, Goel V, Barer ML, Muhajarine N, Derksen S. Validity of self-reported utilization of insured health care services. Institute for Work & Health Working Paper #108. Toronto, ON: Institute for Work & Health, 2000.
Tacci JA, Webster BS, Hashemi L, Christiani DC. Healthcare utilization and referral patterns in the initial management of new-onset, uncomplicated, low back workers’ compensation disability claims. J Occup Environ Med 1998;40(11):958–63.
Dembe AE, Savageau JA, Amick III BC, Banks SM. Office-based medical care for work-related conditions: Findings from the National Ambulatory Medical Care Survey, 1997–1998. J Occup Environ Med 2002;44:1106–17.
Liss GM, Tarlo SM, Macfarlane Y, Yeung KS. Hospitalization among workers compensated for occupational asthma. Am J Respir Crit Care Med 2000;162(1):112–8.
Lavis JN, Malter A, Anderson GM, Taylor VM, Deyo RA, Bombardier C, Axcell T, Kreuter W. Trends in hospital use for mechanical neck and back problems in Ontario and the United States: discretionary care in different health care systems. CMAJ 1998;158(1):29–36.
Shannon HS, Lowe GS. How many injured workers do not file claims for workers’ compensation benefits? Am J Ind Med 2002;42:467–73.
Morse T, Dillon C, Warren N, Levenstein C, Warren A. The economic and social consequences of work related musculoskeletal disorders: The Connecticut upper-extremity surveillance project (CUSP). Int J Occup Environ Health 1998;98:209–16.
Carey TS, Evans A, Hadler N, Kalsbeek W, McLaughlin C, Fryer J. Care-seeking among individuals with chronic low back pain. Spine 1995;20:312–7.
Szpalski M, Nordin M, Skovron ML, Melot C, Cukier D. Health care utilization for low back pain in Belgium: Influence of sociocultural factors and health beliefs. Spine 1995;20(4):431–42.
Von Korff M, Saunders K. The course of back pain in primary care. Spine 1996;21(24):2833-2837.
Bergquist-Ullman M, Larsson U. Acute low back pain in industry: A controlled prospective study with special reference to therapy and confounding factors. Acta Orthop Scand 1977;170:1–117.
Wong O. Use of administrative databases in occupational and environmental epidemiologic research (editorial). Ann Epidemiol 2001;11(5):281–5.
Ekberg K, Karlsson M, Axelson O, Malm P. Cross-sectional study of risk factors for symptoms in the neck and shoulder area. Ergonomics 1995;38(5):971–80.
Skov T, Borg V, Orhede E. Psychosocial and physical risk factors for musculoskeletal disorders of the neck, shoulders, and lower back in salespeople. Occup Environ Med 1996;53(5):351–6.
Marmot M, Shipley M, Brunner E, Hemingway H. Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. J Epidemiol Commun Health 2001;55(5):301–7.
Acknowledgements
This research was supported by the Workers’ Compensation Board of British Columbia through the Finding Solutions Program. The principal investigator was supported by the Institute for Work & Health (Toronto) through the Mustard Post-doctoral Fellowship in Work Environment and Health and currently by the Michael Smith Foundation for Health Research Scholar Award. The Institute for Work & Health, an independent not-for-profit research organization, receives support from the Ontario Workplace Safety and Insurance Board. The authors thank the employees and administration of St. Paul’s Hospital (Vancouver) for their participation in the study and their assistance with data extraction. The authors are also very appreciative of the expertise provided by Kim McGrail at the Centre for Health Services and Policy Research (University of British Columbia) on the BC Linked Health Database. The authors thank Bo Green for his advice on the analysis of the health care utilization data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koehoorn, M., Cole, D.C., Hertzman, C. et al. Health care use associated with work-related musculoskeletal disorders among hospital workers. J Occup Rehabil 16, 402–415 (2006). https://doi.org/10.1007/s10926-006-9022-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-006-9022-7