Abstract
Physical therapy, hemodialysis and radiation oncology departments in which patients go through lengthy and periodic treatments need to utilize their limited and expensive equipment and human resources efficiently. In such departments, it is an important task to continue to treat current patients without any interruption along with incoming patients. In this study, a patient scheduling approach for a university radiation oncology department is introduced to minimize delays in treatments due to potential prolongations in treatments of current patients and to maintain efficient use of the daily treatment capacity. A simulation analysis of the scheduling approach is also conducted to assess its efficiency under different environmental conditions and to determine appropriate scheduling policy parameter values. Also, the simulation analysis of the suggested scheduling approach enables to determine appropriate scheduling parameters under given circumstances. Therefore, the system can perform more efficiently.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patient scheduling in hospitals includes a high amount of complexity due to inherent dynamics of the processes and the distributed organization structure of hospitals. For treatment, patients visit different units according to their illness.
The patient scheduling approaches in literature can be classified according to their solution methodology as analytical, perceptional solution approach and simulation. In one of the initial studies on this topic was performed by Fetter and Thampson [3]. They examined the appointment intervals on the waiting times for the patients and the waste times for physicians by using computer simulation. Soriano [14] mentioned that the system had more advantage to give an appointment for two patients at the same time to use physicians efficiently. It was assumed that patients came to policlinic on time and the patients’ inspection times matched up to the Gamma distribution. Rising et al. [12] advised to program the appointment periods that straighten the patients’ arriving manner and the demand curve when the demand was uncertain. In this study, the waiting line computer simulation models were used to plan receiving of patients. Babes and Sarma [1] put forward the simulation approach as an alternative method for the analytic methods in the case of limited resource quantity, quantity of the beginning patients at random, non-exponential distribution of the service times, the service units with late beginning times. Jeang [6] developed a simulation model as a tool to describe the behavior of the inpatient admission system in hospital. Due to the complex system, the author used SIMAN software to develop a simulation model.
Brahmi and Worthington [2] used the queue model M(t)/G/s which allowed the patient arriving frequency depend on time for the outpatient treatment policlinics. In a similar study, Ho and Lau [4] compared some kind of appointment rules in terms of total cost. Ho and Lau [5] evaluated the impact of operating conditions on the performance of appointment scheduling rules in service systems. Rohleder and Klassen [13] used simulation approach to examine the performance of dynamic appointment scheduling rules.
Standridge [16] described a structure for an expert system that modeled patient appointment scheduling and the integration of such an expert system within a simulation model. Expert system for a small animal veterinary clinic was presented. Su and Shih [15] used simulation approach to understand the effect of various scheduling policies on patients and to determine throughput and waiting times of patients.
Paulussen et al. [7] proposed an agent based approach in which the patients and hospital resources were modeled as autonomous agents with their own goals, reflecting the decentralized structures in hospitals. In this multi-agent system, the patient agents competed over the scarce hospital resources. Paulussen et al. [8] considered the situation in which the necessary medical treatments were often not completely determined at the beginning of the treatment process. Further, they took the duration of the treatments as stochastic. The contribution of this paper was the introduction of a novel multi-agent based distributed approach to patient scheduling under variable pathways and stochastic process durations. Paulussen et al. [9] described a hospital simulation system which allowed the benchmark of different coordination mechanisms including the current practice in hospitals.
Podgorelec and Kokol [11] developed a powerful automated scheduling method for highly constrained situations based on genetic algorithms and machine learning. They applied the described method to a problem of scheduling patients with different therapy needs to a limited number of therapeutic devices, but the algorithm can be easily modified for use in similar situations.
The main differences of this study are to advise the slack capacity approach for the patients scheduling problem and to determine the suitable working circumstances by simulation approach. Our purpose is to minimize delays in treatments due to potential prolongations in treatments of current patients and to maintain efficient use of the daily treatment. Efficient utilization of human resources and limited expensive equipment are very crucial in some department such as hemodialysis and radiation oncology where patients go through lengthy and periodic treatments. So, it is an important task to continue to treat current patients without any interruption along with incoming patients.
Materials and method
Materials
The patients that come to the radiation oncology department have been diagnosed in other departments or operated before. The arrivals of the patients are at random and it is possible to suggest a model by using Poisson Processes. As an implementation location of this study, the treatment unit of Radiation Oncology Department of Medical Faculty of Cukurova University, which works on all weekdays, is chosen. According to patient receiving policy, incoming patients are only accepted on Monday, Tuesday or Wednesday. The number of patients to be treated is determined with regard to the number of patients whose treatments would end that week. Because of the random treatment times, the number of patients changes every week. Service authorities mentioned that there is a seasonal trend in the quantity of applications for treatments; however the average quantity of daily receiving new patients is about five. Since the hospital is a regional hospital, the patients who apply for the treatment can generally be given appointments for the next 5 months.
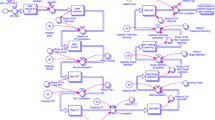
The flow diagram of patients in Radiation Oncology Department is given as a summary in Fig. 1.
The patients who come from other departments go into the simulator device that proves the treatment method and the region of cancer. The patient is treated by Cobalt Device, Linear Accelerator or Demapan Device according to the kind of cancer and the features of the patient. After treatment is completed, tests are performed in order to find out whether patients need any more treatments.
In this system, there is a bottleneck in Cobalt Device, because most of the patients are treated by this device. Therefore, in this study, scheduling of Cobalt Device is considered. The treatment times of patients change according to the kind of cancer as mentioned in Table 1.
The patients who need palliative treatment involve shorter treatment periods (10–15 days). After first ray period, as a result of tests done, there may be need for a second ray period with a low probability (approx. 3%). But a third ray period is not considered because of the both weak structure of patient and a low probability of necessity.
In a system with a low frequency of patients, the deterministic factor is maximum waiting time and taking this time high causes delays at appointments.
Method
Scheduling approach
The slack capacity approach is suggested for scheduling of the patients who apply to the Radiation Oncology Department. According to this approach, some part of the daily patient capacity is reserved as a slack capacity (c s) in order to prevent the treatment delays. Data belonging to current patients have been gathered from the policlinic record during 60 sequent weekdays to determine patient coming process. The K–S test that is more powerful to determine which distribution matches to the daily patient quantity has been preferred to the χ 2 test. The K–S test shows that the Poisson arriving process is appropriate at significance level of p < 0.05. The patients applied are divided in to two groups as palliative and normal in respect of treatment times. The palliative patients are in less serious conditions and needs shorter treatment times.
The variables, which have been used in this study, are explained below;
- i :
-
Daily sitting number. i = 1,....60
- λ :
-
Current patient’s arriving frequency
- f i :
-
The day when the ith treatment slice is emptied
- c s :
-
Slack capacity (patient)—control parameter
- t max :
-
The maximum time that is allowed between application day and appointment date as day—control parameter
- c n :
-
Normal capacity (patient)
- t a :
-
Patient application day
- t 0 :
-
Existent day
- t r :
-
Appointment day
- t t :
-
Time of a ray treatment
- k :
-
Course number of patients
The patient algorithm that based on reserving a slack capacity has been explained step by step below;
-
Step 1:
According to application date, determine the next patient.
-
Step 2:
If max {min {f i } − t a, 0} ≤ t max,
-
i ≤ 60 − c s
-
t r = min {f i } and determine the sitting number (k),
-
i ≤ 60 − c s
-
-
go to the third step.
-
Otherwise do not accept the patient and stop.
-
-
Step 3:
f k = t r + t t
-
Step 4:
If there is a necessity for second ray,
-
If f k ≤ t 0 , go to the same sitting slice,
-
Otherwise, assign to the first empty slack sitting slice.
-
-
-
Step 5:
Go to the Step 1.
Simulation analysis
In fact, the system examined is a waiting line. However, the analytic waiting line models in the literature should not be applied owing to the complex working logic of the scheduling algorithm applications that have been developed in this study. Therefore, the dynamic discrete-event simulation is the most appropriate one to test the scheduling approach in different circumstances due to the systems’ stochastic structure. The SIMAN simulation model and experiment file, which has been developed for this target, is submitted in additions.
In the simulation analysis, the influence of high frequency patients on the system performance has been examined considering different daily patient arriving frequency. Moreover, some suggestions have been put forward to choose the slack capacity and maximum waiting time that are two parameters for the scheduling approach. The variation ranges belong to all the parameters that were used in the experiments are summarized as following;
Patients’ arriving frequency (λ) | 1–10 patients/day |
Slack capacity (c s) | 2, 4, 6, 8 patients |
Maximum waiting time (t max) | 2, 4, 6, 8 days |
The ratio of normal and palliative patient | 80% and 20% |
The probability of second ray | 3% |
Treatment time (normal, palliative) | 30 and 10 days |
These parameters are determined according to physicians’ view in the department of Radiation Oncology in Cukurova University. It has been used an exact factorial experimental design that includes the levels of mentioned parameters to examine the influence of slack capacity and maximum waiting parameter on the performance statistics. In each experiment, five replications have been individually done and the long term performance of the system was examined by using average values of the replications. It is thought that five individual replications are sufficient because it is not to be aimed to make a confidence range for all experiment points. In addition, the effectiveness of the system for the long term has been estimated by means of starting each replication for 20,000 days. The time of 1,000 days at the beginning are reserved for warming up period. The length of warning up period has been determined by examining the graphic that gives the relation between the pilot simulation results and time.
Results of the simulation
The influence of the scheduling parameters and various patient frequencies on the system performance has been examined by the method of simulation modeling. The detailed analysis of the performance variables is given as follows.
-
i)
The percentage of unaccepted patients: As seen from the Fig. 2, when the number of patient needing treatment in the system is much more than the existing capacity, slack capacity is not an important factor that affects the percentage of unaccepted patients. It is reasonable because the number of patients needing for this service exceeds total capacity, and slack capacity occupies a small part of the total capacity. So, impact of slack capacity is very slight. However, the percentage of unaccepted patients is mostly determined by maximum waiting parameter (t max). This means that the main factor is how long the patients will accept to wait before the treatment starts. It is reasonable that if the value of maximum waiting increases, the number of rejected patient decreases.
Also, as seen form the Fig. 3, in the systems where the frequency of patients is too low, the percentage of the rejected patients increases when t max decreases. However, in this system which has low frequency of patient, the impact of slack capacity on the percentage of rejected patient is also important as different from the system having high frequency of patient. Figure 3 shows that unnecessarily increased slack capacity causes increased percentage of rejected patients in this system. The ratio of the rejected patients is rather low in case of low patient frequency when compared to in case of high patient frequency (about 10–18%).
-
ii)
Treatment Delay (day): This variable shows the average delay that has occurred by the capacity already reserved for other patient that needs (need of second ray) a longer treatment than expected. In the systems with a high frequency of patients, the treatment delay is completely determined by the slack capacity. As seen from the Fig. 5, the slack capacity should be about four in order not to delay for treatment (Fig. 4).
In the systems with low frequency patients, the main factor that affects the treatment delay is maximum waiting time and taking this parameter high causes delays in appointments (Fig. 5).
When the patient arriving frequency and slack capacity are evaluated together (Fig. 6), it can be proved that the slack capacity should be increased as the patient arriving frequency increases.
-
iii)
The quantity of the patients waiting in queue: this statistic is naturally affected by maximum waiting parameter (t max) (Fig. 7). Decreasing the maximum waiting time to the acceptable levels dispatches patients to the alternate hospitals and prevents the excessive increasing in the quantity of the patients waiting in queue.
-
iv)
Normal Capacity Usage Ratio (%): Examining Fig. 8; it is proven that normal capacity usage ratio is highly determined by the patient arriving frequency. In the cases of the patients arriving frequency is low, capacity usage ratio decreases to 60%. On the other hand, the systems with the capacity usage rate at 100% have a long patient waiting time.
-
v)
Slack capacity usage ratio (%): In Fig. 9, it seems that taking the slack capacity higher than required causes inefficient usage of total capacity. It is not also forgotten that taking the slack capacity too high causes the treatment delays. In Fig. 9, it seems that the most appropriate value is four patients for the slack capacity. The slack capacity usage ratio decreases approximately below 40% for the higher values than 4.
Conclusion
In this study, the slack capacity approach is developed for scheduling patients in the services that involve periodical treatment. The aim of slack capacity approach is to prevent the appointment postponements that occur because of the uncertainties in treatment times. Additionally, the influence of the scheduling parameters and various patient frequencies on the system performance has been examined by simulation modeling.
Simulation analysis has shown that in the systems with high frequency, the percentage of unaccepted patients is mostly determined by maximum waiting parameter rather than slack capacity. However, in the systems with low frequency, unnecessarily increased slack capacity causes increased percentage of rejected patients in the system. Moreover, the other important performance variable that is examined in both systems is the treatment delay. In the systems with a high frequency of patients, the treatment delay is completely determined by the slack capacity. However, in the systems with low frequency patients, the main factor that affects the treatment delay is maximum waiting time and taking this parameter high causes delays in appointments. The other important consequences from the simulation analysis is also that decreasing the maximum waiting time to the acceptable levels dispatches patients to the alternate hospitals and prevents the excessive increasing in the quantity of the patients waiting in queue and the usage of slack capacity highly diminishes the appointment postponements. However, choosing this capacity too high causes a low capacity usage.
The simulation analysis of the suggested scheduling approach enables to determine appropriate scheduling parameters under given circumstances. Therefore the system performs more efficiently using the appropriate scheduling parameters and this causes minimizing the percentage of unaccepted patients, treatment delay, and the quantity of the patients waiting in queue.
References
Babes, M., and Sarma, G. V., Out-patient queues at the Ibni-Roche Health Centre. J. Oper. Res. Soc. 42:10845–855, 1991.
Brahimi, M., and Worthington, D. J., Queuing models for out-patient appointment systems—a case study. J. Oper. Res. Soc. 42:9731–745, 1991.
Fetter, R. B., and Thampson, J. D., The simulation of hospital systems. Oper. Res. 13:5609–711, 1965.
Ho, C. H., and Lau, H. S., Minimizing total cost in scheduling outpatient appointments. Manage. Sci. 38:121750–1764, 1992.
Ho, C. H., and Lau, H. S., Evaluating the impact of operating conditions on the performance of appointment scheduling rules in service systems. Eur. J. Oper. Res. 112:3542–553, 1999, doi:10.1016/S0377-2217(97)00393-7.
Jeang, A., Inpatient admission system model using SIMAN software. J. Med. Syst. 14:6365–374, 1990, doi:10.1007/BF00996716.
Paulussen, T. O., Jennings, N. R., Decker, K. S., and Heinzl, A., Distributed patient scheduling in hospitals. Proceedings of 18th International Joint Conference on Artificial Intelligence. 1224–1229, Acapulco: Mexico, 2003.
Paulussen, T. O., Zöller, A., Heinzl, A., Braubach, L., Pokahr, A., and Lamersdorf, W., Patient scheduling under uncertainty. Proceedings of the 2004 ACM Symposium on Applied computing (SAC2004). Nicosia: Cyprus, 2004.
Paulussen, T. O., Zöller, A., Heinzl, A., Braubach, L., Pokahr, A., and Lamersdorf, W., Dynamic patient scheduling in hospitals. Coordination and agent technology in value networks. GITO, Berlin, 2004.
Perez, C. A., and Brady, L. W., Principles and practice of radiation oncology. Lippincott-Raven, Philadelphia, p. 2341, 1998.
Podgorelec, V., and Kokol, P., Genetic algorithm based system for patient scheduling in highly constrained situations. J. Med. Syst. 21:6417–427, 2004.
Rising, E. J., Baron, R., and Averil, B., A systems analysis of a university-health-service out-patient clinic. Oper. Res. 21:51030–1047, 1973.
Rohleder, T. R., and Klassen, K. J., Using client-variance information to improve dynamic appointment scheduling performance. Omega-International J. Manage. Sci. 28:3293–302, 2000, doi:10.1016/S0305-0483(99)00040-7.
Soriano, A., Comparisons of two scheduling systems. Oper. Res. 14:1338–397, 1966.
Su, S., and Shih, C. L., Managing a mixed-registration-type appointment system in outpatient clinics. Int. J. Med. Inform. 70:31–40, 2003, doi:10.1016/S1386-5056(03)00008-X.
Standridge, C. R., Using expert systems for simulation modeling of patient scheduling. Simulation. 75:3148–156, 2000, doi:10.1177/003754970007500303.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogulata, S.N., Cetik, M.O., Koyuncu, E. et al. A Simulation Approach for Scheduling Patients in the Department of Radiation Oncology. J Med Syst 33, 233–239 (2009). https://doi.org/10.1007/s10916-008-9184-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-008-9184-2