Abstract
The mammary gland is a dynamic organ that continually changes its architecture and function. Reciprocal interactions between epithelium and adipocyte-containing stroma exert profound effects on all stages of its development, even though the details of these events are not fully understood. To address this issue, enormous potential exists in the utilization of synthetic adipose tissue model systems to uncover the properties and functions of adipocytes in the mammary gland. The first part of this review focuses on mammary adipose tissue (or adipocyte)-related model systems developed in recent years and their utility in investigating adipose-epithelial interactions, mammary gland morphogenesis, development and tumorigenesis. The second part shifts to the field of adipose-based breast tissue engineering, focusing on how these synthetic adipose tissue models are being constructed in vitro or in vivo for regeneration of the mammary gland, and their potentials in adipose tissue engineering also are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The mammary gland of a reproductively active female is a dynamic organ that continually changes its architecture and function. Two cellular compartments constitute mammary gland tissue: the epithelium and the surrounding stroma, which are derived embryologically from ectoderm and mesoderm, respectively [1]. Mammary epithelial cells (MECs) represent the fundamental functional part of the mammary gland, while the stromal compartment, comprised of several stromal cells and abundant proteinaceous extracellular matrix (ECM), is crucial for proper patterning and function of the normal mammary gland [2]. Increasing evidence has shown that reciprocal interactions between the mammary epithelium and stromal cells are critical for normal development of the mammary gland, and are also required for tissue homeostasis, as aberrant epithelium-stroma communication can induce and promote tumorigenesis [3–6].
During the past two decades, in vitro and in vivo studies have been conducted to better understand the stromal-epithelial interactions, and many key molecular, structural, and mechanical cues important for maintaining the architecture and function of gland tissue have been identified [7–9]. However, most of these studies have focused on fibroblast-epithelial interactions, in which fibroblasts modulate epithelia cell growth and differentiation [10–12], and few have focused on the role of mammary adipocytes, despite the predominance of adipocytes in the mammary gland.
Adipocytes were originally considered a passive stromal cell type that stored excess energy in the form of lipid droplets, and only more recently has their dynamic role been recognized, revealing their participation in a broad range of physiological processes, such as apoptosis, inflammation, hormonal signaling and angiogenesis [13–15]. Thus, researchers have become interested in the adipocyte’s roles in mammary gland morphogenesis and their influence on the normal or aberrant development of the mammary gland. To address these questions, researchers have developed several synthetic adipose tissue model systems to serve as tools for uncovering the properties and functions of adipocytes in the mammary gland. Here, the first part of this review focuses on mammary adipose tissue (or adipocyte)-related model systems developed in recent years and their utility in investigating adipose–epithelial interactions, mammary gland morphogenesis, development and tumorigenesis. The second part shifts to the field of adipose-based breast tissue engineering, focusing on how these synthetic adipose tissue models are being constructed in vitro or in vivo for regeneration of the mammary gland.
Development of the Mammary Gland
Quite a few elegant studies and comprehensive reviews were previously published to describe the development of the mammary gland [16–18]. Here, only a brief introduction is presented with an aim to provide a context for better understanding those synthetic adipose tissue models for studying or regenerating the mammary gland.
The mammary gland develops along the “milk line”, a linear thickening of epidermis between the anterior and posterior limb buds [16]. Only minimal ductal outgrowth of the mammary rudiment is found before puberty, while with the initiation of puberty, a further development occurs as characterized by a formation of the functional unit of the mammary gland, termed terminal duct lobular unit (TDLU). The final development of the mammary gland occurs during pregnancy and lactation, and entails ductal branching and lobuloalveolar structure development in responses to several hormones from the ovaries and pituitary gland [19–21]. The capability of mammary epithelium to grow, undergo ductal morphogenesis, form alveoli, and produce milk proteins is highly dependent on the stromal tissue environment. Specifically, epithelium structures penetrate into mammary adipose tissue in the gland, associating with an adipocyte-containing stroma throughout all stages of normal morphogenesis and development [16, 18, 19, 22]. Both human and mouse mammary tissues contain large areas of adipose stroma tissue; moreover, both species share several similarities with respect to their developmental events [17, 18]. Thus, by using mouse mammary gland model systems, investigators have collected many clues to address some of the challenging biological issues involved with human mammary glands, including epithelium differentiation and neoplastic transformation. These models, their strengths and limitations, will be discussed in the following section.
Mammary Adipose Tissue-Related Model Systems for Studying Mammary Gland Development and Tumorigenesis
Other than the epithelium contained in the mammary gland, two mesenchymal tissues, the fat tissue and fibroblastic connective tissue surrounding the epithelium, also play key functional roles in mammary gland development. Reciprocal interactions between these two compartments, the parenchymal (composed of epithelial cells) and mesenchymal compartments (including adipocytes and fibroblasts) have been shown to exert profound effect on all stages of gland morphogenesis, development and differentiation [18, 19, 23]. However, mechanisms behind their interactions are not fully understood, creating a need for better in vitro and in vivo models of parenchymal-mesenchymal interactions in physiological and pathophysiological conditions in the mammary gland. Here we focus on mammary fat pad-related tissue systems and adipocyte-based synthetic adipose tissue models that have been successfully employed to probe the cross-talk between adipocytes and mammary epithelial cells. We also discuss the benefits of these models and suggest their possible improvements.
Mammary Fat Pad (MFP)-Based Tissue Model Systems
The course of adipogenesis of the mammary gland and development of MFP during embryogenesis has been well described in previous publications [24–26], yet functions of the MFP have not been fully elucidated [17]. Several studies suggest that the MFP, a matrix of adipose and connective tissue, not only supports mammary epithelium growth physically [27], but also mediates hormone action [28] and synthesizes an array of growth regulator molecules, such as prostaglandin E2 (PGE2) [29], hepatocyte growth factor (HGF) [30], insulin-like growth factors (IGFs) [31], fibroblast growth factors (FGFs) [32] and integrin components [33, 34], that contribute to mammary gland morphogenesis and development. These factors dictate a central role of the MFP in any tissue-engineered mammary gland model.
The “Cleared Fat Pad” Model
Since a mouse’s rudimentary ducts begin to expand into the fat pad at day 16, but do not fully elongate until puberty (∼day 24–30), rudimentary epithelium can be completely excised from a fat pad (typically the fourth MFP) when a mouse is 3 weeks old. This results in a “cleared” fat pad devoid of any epithelium that can be utilized as a site for transplantation [17]. This “cleared fat pad” model is useful for elucidating the endocrine, genetic and heterotypic interactions that drive mammary gland morphogenesis, development and carcinogenesis [35]. In one study, this model has been employed to elucidate an age-related effect on mammary duct elongation mediated by the epithelium-stroma interaction. It was shown that a young, proliferating mammary epithelium transplanted into the MFP could support mammary duct elongation; in contrast, a serially aged mouse mammary epithelium failed to develop due to its decreased capability in stimulating DNA synthesis of the stromal cells. Since DNA synthesis of stromal cells surrounding the end bud is essential for the mammary duct elongation, it is easy to understand the age-dependent effect produced by epithelial cells on the gland morphogenesis [36]. Aging also decreases supportive ability on the stromal side. It has been found that epithelium combined with stroma from fetal mouse MFP was able to undergo normal organogenesis, but when the same epithelia was combined with MFP tissue of 17- to 18-day fetal mice, or postnatal mice, this supportive capacity was decreased, or entirely lost, respectively [37].
The “cleared” mammary model is also essential at solving a long-time question: whether stromal or epithelial estrogen receptor-α (ERα) is responsible for mammary gland development. The question developed as a result of contrasting studies. On the one hand, by using MFP-based tissue recombination techniques, researchers found that estrogen receptor-α (ERα) expression in MECs is necessary for ductal elongation in mammary gland [38–40]. A recent study by Mallepell et al. also demonstrated that mammary epithelium is the primary target for estradiol function, and paracine signaling through the epithelial ERα is required for proliferation and morphogenesis in the mammary gland [41]. On the other hand, however, studies using a recombinant tissue comprised of MFP from neonatal Balb/c mice and the epithelium from ERα-disrupted (αERKO) mice supported the fact that stromal ERα was necessary for ductal elongation during mammary gland development in neonatal mice [42]. To rectify these studies, “cleared” MFP tissue (from either 3-week-old female αERKO mice or wild-type mice) engrafted with the MECs from adult αERKO mice or from wild-type counterparts was also reconstructed. Ten weeks after implantation into the nude mice, whole mount analysis of the mammary gland showed that both stromal and epithelial ERα were vital for complete mammary gland development in adult mice. But when the mice were treated with high doses of estradiol and progesterone, stromal ERα was shown to be capable of generating full mammary gland growth. Furthermore, it was determined that ERα-deficient epithelial cells were able to proliferate and develop into a rudimentary mammary ductal structure in an ERα-negative stroma, suggesting that neither stromal nor epithelial ERα are required for mammary rudiments to form in the adult mouse [43]. Collectively, these studies suggest that neonatal and adult mammary tissues might use different tissue-specific roles of ERα in mammary response. The “cleared” MFP model was able to elucidate these juvenile/mature tissue differences and could act as a platform for studying the contributions of growth factors, hormones, and receptors in mammary gland development.
The “Humanized” MFP In Vivo Model
Much progress has been made in recapitulating mouse mammary epithelial morphogenesis and elucidating interactions between epithelium and stroma in mouse mammary gland. However, investigating hormone complex interactions and hormone effects on human mammary gland development and differentiation has been unsuccessful when using a “cleared” MFP model system introduced with human MECs. A number of laboratories have reported that neither human nor bovine mammary epithelium grow well in the mouse MFP, suggesting the need for a “humanized” mouse model [44, 45]. For instance, human MECs injected into the MFP of athymic nude mouse formed small, spherical structures with duct-like epithelial elements. These structures failed to generate extensive or expansive growth even with the treatment of several hormones in vivo [46]. In contrast, co-transplantation of normal tissue from human mammary gland with human stroma has been shown to support human MEC long-term survival (up to 6 month) and enhance their hormone responsive capability [47]. These both stroma- and species-dependent outcomes might be in part due to the histological differences between the adipose-rich mouse MFP and that of the more fibrous human breast stroma [18].
Since human epithelial cells are unable to establish themselves in the mouse mammary stroma or participate in normal mammary ductal morphogenesis, a useful in vivo model might include the incorporation of human stroma into the MFP before the implantation of human MECs. This type of reconstruction of functionally normal human breast tissue in the mouse MFP was recently reported [48, 49]. In these studies, a novel chimeric mammary stroma was developed by co-injecting non-irradiated and irradiated human mammary fibroblasts into the mouse MFP, and then engrafting human MECs to form a resultant “humanized” MFP model. Expansive outgrowths and branches of epithelium ducts were generated by the engrafted human MECs isolated from human organoids from reduction mammoplasty tissues (including myoepithelial and luminal epithelial cells). Moreover, this reconstructed “humanized” MFP was capable of supporting fully functional differentiation of human MECs, as demonstrated by β-casein expression and milk production. Thus, a histologically normal and functional human mammary gland tissue could be constructed successfully in the orthotopic xenograft model by taking advantage of the “tissue recombinant” technique [48]. But it is worthwhile to point out that a mixture of irradiated and non-irradiated fibroblasts prove to be necessary for the humanized MFP reconstruction, as the irradiated fibroblasts facilitate engraftment and invasion of the co-injected nonirradiated cells. So far, this is the most encouraging experimental model that allows for the study of human epithelial morphogenesis and differentiation in vivo. Using this humanized model system, the investigators also revealed disparities in the behavior of ostensibly normal epithelial cells derived from different patients, suggesting its potential in elucidating the contributions of stromal compartment to mammary morphogenesis and transformation.
Adipocyte Culture-Based In Vitro Models
Despite the advances in the study of mammary biology facilitated by the “cleared” MFP and “humanized” MFP models, it should be noted that the “cleared” MFP comprises more than adipocytes and preadipocytes. Several other cell types such as fibroblasts, endothelial cells, and lymphocytes, as well as nerve cells et al. are also involved in this particular model system, any or all of which could produce a direct and/or indirect influence on morphogenesis of the mammary gland [22–24]. This indicates that data collected with these complicated culture systems should be considered with caution. In addition, the complexity of the in vivo environment, including undefined growth factors, hormones, cells, immune reactions, and species-specificity, makes interpreting in vivo models more challenging. Thereafter, to explore heterotypic interactions between adipocytes and epithelial cells in a more controlled and reproducible manner, efforts have been focused on constructing more defined adipocyte-epithelium co-culture models in vitro under cell and tissue culture conditions.
Adipocyte Culture-Based Models for Studying Normal Mammary Gland Development
An original epithelial-adipocyte in vitro two dimensional (2D) co-culture system was reported in which MECs from a pregnant mouse were directly seeded on the top of the mouse preadipocyte cell line 3T3-L1 and demonstrated enhanced proliferative activity compared to the epithelial cells alone [50]. Other co-culture systems using similar 2D culture conditions were also described for studying the effects of adipocytes on epithelial cell growth, differentiation and function [3, 51]. However, these cell culture systems under 2D conditions recapitulate neither tissue architecture nor function of the mammary epithelium in vivo, and are inadequate to assess the role of adipose stroma in physiological development and tumorigenesis of the mammary gland [52, 53]. With the advent of tissue engineering technology, researchers now have the ability to create complex three-dimensional (3D) breast tissue-like cultures, bridging the gap between 2D cell culture and animal systems.
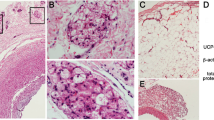
Co-culturing human MECs and adipocytes from the same patient in a 3D collagen gel was described in a paper by Huss et al., in which the MECs maintained a normal intercellular distribution and growth pattern in vitro when co-cultured in the 3D matrix [54], This outcome is encouraging despite the fact that no detailed morphology or function of this system was described. Recently, a successful human 3D adipocyte-epithelium co-culture model was developed in which a non-malignant human epithelial cell line (MCF10A) was co-cultured with predifferentiated human adipose–derived stem cells (hASCs) within a mixture of Matrigel and collagen on a 3D porous silk scaffold [55]. The results demonstrated that the presence of hASCs inhibited epithelial cell proliferation, and also induced alveolar and ductal morphogenesis. Most importantly, co-cultures with adipocytes in the 3D culture condition enhanced epithelial cell functional differentiation as evidenced by the proper polarity and increased functional gene (casein-α/β) expression levels. In contrast, only alveolar structures with reversed polarity were observed in the epithelial monocultures (Fig. 1). In addition, by using this 3D co-culture model, ductal morphogenesis effect exhibited by the co-culture was shown to be correlated with HGF secretion from the predifferentiated hASCs, indicating a critical role of adipocytes in mammary epithelial morphogenesis and development. Thus, an in vitro co-culture model on 3D silk scaffolds with a physiologically relevant microenvironment for epithelial cells and stromal cells was developed. This model allows for investigations into tissue organization and epithelial morphogenesis in normal or diseased mammary gland development.
Schematic of breast tissue engineering using silk protein scaffolds. Both acinar and ductal structures were generated within the co-culture or tri-culture systems, in contrast to the only acinar structures in monoculture. Images (a) and (b) show growth of epithelial cells in the culture systems (green fluorescence notes the live cells shown via live/dead staining, Ref [62, 112])
Adipocyte Culture-Based Models for Studying Mammary Gland Tumorigenesis
In addition to the roles adipocytes play in physiological processes discussed above, the roles they play in pathophysiological processes, such as carcinogenesis, are extensive [19, 56, 57]. As a second leading cause of cancer-related death for women in the United States [58, 59], breast cancer correlates with a complex set of interactions between mammary epithelial cells and their stroma [60]. In fact, epithelial cells undergo similar processes during carcinogenesis, and rely on many of the same soluble or insoluble signals, as they do during mammary gland morphogenesis and development, and adipocytes play supporting roles in both cases [56, 57]. To better understand the complex effects of mammary adipocytes during breast cancer initiation, progression and development, investigators have sought to develop synthetic model systems that could be employed to elucidate the interactions between breast cancer cells and adipocytes in vitro and in vivo.
Using a simple 2D co-culture system, the state of preadipocyte differentiation has been shown to affect the clonal growth of breast cancer cells under anchorage-independent conditions in vitro [61]. In this model, proliferating preadipocytes served as a feeder layer in a 2D co-culture system and stimulated breast cancer cell growth significantly. By contrast, after differentiation, the mature adipocyte feeder layer inhibited cancer cell growth, suggesting that adipocytes at different developmental stages produce different factors and exert different influences on breast cancer cell behavior. Consistent with this study, an indirect co-culture system (using Boyden chambers coated with Matrigel) showed that both murine and human ASCs promoted breast cancer cell growth and migration in vitro [62]. Models examining ASC homing to tumor sites also showed tumor-promoting effect of ASCs when they were co-injected into the MFP or when injected intravenously, indicating that not just local ASCs, but also distal ASCs play a role in tumor growth and metastasis [62].
The only synthetic 3D co-culture model system reported for the study of crosstalk between adipocytes and breast cancer cells utilized mature adipocytes and breast carcinoma cells in a 3D collagen gel [63]. However, the results in the 3D model contradicted that of the 2D culture system and reported that preadipocytes inhibited T47-D breast cancer cell growth while mature adipocytes promote cancer cell proliferation. To explain this discrepancy, the authors claimed that different cell sources (primary (pre)adipocytes vs. the 3T3-L1 cell line, and different breast cancer cell lines), distinct culture systems (3D vs. 2D), and growth assay methods might contribute to the discrepancy among these studies. However, it should be pointed out that more caution should be taken when interpreting the data collected from different culture models. To reach some consensus on clarifying the roles of adipocytes or preadipocytes during breast tumorigenesis and cancer progression, more 3D synthetic culture models that mimic the microenvironment in vivo are needed.
Adipocyte-related variables that affect tumor initiation and progression are numerous. Clinically, several investigations have found that high total body fat content is linked to increased risk of breast cancer [64]. This association might partly be explained by the tumor promotional role of adipocytes as described above. However, it appears contradictory to other clinical studies that have recognized a relationship between decreased mammary fat content and increased breast cancer. It has been shown that a decreased mammary fat percentage leads to an increased mammographic density, whereas the latter is highly correlated with high risk of breast cancer [65, 66]. Thus, the role of adipocytes in the background of increasing density in breast cancer risk is quite controversial. A cell culture model for further investigating the roles of adipocytes in breast tissues with different densities would give more insight into the relationships between mammary adipocytes and gland density and how they could influence tumorigenesis.
Adipose Tissue Model Systems for Regenerating Mammary Glands
In addition to providing a useful model system for studying the mammary gland, synthetic adipose tissue models also serve as the foundation for mammary gland regeneration. The need for breast tissue regeneration is driven clinically by the widespread impact of lumpectomies or mastectomies from trauma, cancer or other disease. Aesthetic or functional surgeries are often desired for the psychological well-being of patients with soft tissue defects, especially breast cancer resection [67–70]. Hence, the second part of this review shifts towards adipose tissue engineering for mammary gland regeneration. The focus is on state-of-the-art bioengineering approaches to adipose tissue modeling, including analysis of appropriate cell types and biomaterial scaffolds.
A brief introduction to breast tissue histology is necessary to better understand the principles, procedures and applications of synthetic adipose tissue models for mammary gland tissue regeneration. As mentioned above, the breast is a specialized organ composed of glandular, ductal structures that are embedded in adipose and fibrous tissue. The adipose tissue is comprised of numerous fat lobules, and each fat lobule involves around 102 ∼ 103 adipocytes [68]. Unilocular and/or multilocular lipid droplets appear in the cytoplasm of mature adipocytes, with sizes ranging from 25 to 200 μm. Abundant vascularization is an important feature of adipose tissue in the body, as evidenced by the fact that each fat cell in the adipose tissue is in contact with at least one capillary, providing a vascular network that allows active metabolism of adipocytes and continued growth of the tissue [67]. These histological characteristics should be taken into account when a synthetic adipose tissue system is designed in vitro.
Cell Types
Prior to initiating the construction of 3D adipose tissues in vitro, one must consider the most appropriate cell type. Initially, autologous mature adipocytes obtained from liposuction and aspirate operations were postulated to be superior cell candidates for adipose tissue engineering, because they possess a terminally differentiated phenotype and function, and minimize the need for immunosuppressive therapy. Unfortunately, neither autologous fat transplantation nor mature adipocyte-based 3D adipose tissue construction has shown encouraging results [54]. First, due to insufficient angiogenesis and mechanical damage, significant resorption of the transplanted fat tissue was observed, and tissue volume was not restored. Second, mature adipocytes, which possess a cytoplasm composed of 80–90% lipid, are prone to be traumatized by the mechanical forces of aspiration, leading to low cell harvest of approximately 10% viable cells. Finally, these fragile adipocytes could not be expanded in culture to obtain abundant cell numbers due to their terminally-differentiated state. After being transplanted in vivo, they tend to form cysts or localized necroses, further discouraging their use in adipose tissue engineering [54, 71].
With the development of stem cell biology in recent years, more investigators have focused on stem cell-based adipose tissue engineering for regenerating mammary gland tissue [72]. Stem cells are defined as those cells having the capability to perpetuate themselves through self-renewal and generate lineage-specified mature cells through differentiation. They can be isolated from a variety of sources including embryos, umbilical cord blood, and adult tissues [73–75]. Recent advances in stem cell research have also enabled the generation of induced pluripotent stem cells (iPSCs) from both fetal and adult mouse fibroblasts through reprogramming by transduction of defined transcription factors or by cell-cell fusion technology [76]. Due to their pluripotent nature and self-renewal capacity, stem cells are useful platforms for tissue regeneration and cell-based therapeutics.
Progress has been made in stem cell-related adipogenesis, which offers promise for adipose tissue engineering and mammary gland regeneration. For instance, directed differentiation of human embryonic stem cells (hESCs) into adipocytes was reported by plating embryoid bodies (EBs) in supplemental modified differentiation medium [77]. Adipocyte precursor cells with a characteristic morphology and proliferative activity could be generated from hESCs transduced with lentivirus carrying Oct4 short hairpin RNA (shRNA) [78]. In comparison with the wild-type hESCs, these genetically-modified cells displayed a remarkably higher lineage-specific spontaneous differentiation capability towards adipocytes. After 2 weeks of spontaneous differentiation under feeder-free conditions, approximately 60–70% of the cells exhibited mature adipocyte morphology as well as the expression of multiple adipocyte-specific mRNAs as assessed by RT-PCR. Recently, adipogenic differentiation of four human iPSC lines was investigated. After 12 days of EB formation and an additional 10 days of differentiation on poly-L-ornithine and fibronectin-coated dishes with adipogenic differentiation “cocktails”, human iPSCs exhibited lipid accumulation and transcription of adipogenesis-related molecules (C/EBPα, PPAR-γ2, leptin and aP2), thereby displaying an adipogenic potential comparable to hESCs [79]. This work further supports the fact that adipocytes with a mature phenotype and function could be generated from multipotential stem cells under specific induction conditions, and points to the possible utility of ESC-derived adipocytes for adipose tissue construction.
Besides the pluripotential stem cells, adult stem cells isolated from some tissues or organs have also shown promise as alternative cell sources for adipose tissue engineering. These adult stem cells can be easily harvested, purified, and are readily expanded in culture, offering not only a potentially-unlimited supply of cells, but also the ability to define and control cellular constituents [80]. Mesenchymal stem cells (MSCs), which can be isolated via minimally-invasive procedures from the bone marrow or other connective tissue in the body, are highly expandable in culture and can be readily induced to differentiate into adipose tissue-forming cells after exposure to a well-established adipogenesis supplement. Currently, bone marrow-derived MSCs (BMSCs) have been investigated extensively and well-characterized for clinical application [81]. By contrast, ASCs, another type of MSC, have only recently been isolated and characterized from adipose tissue of young donors [82–84]. Methods to culture human ASCs in serum-free, chemically defined medium have been established, and these hASCs retained their ability to undergo adipogenesis over 160 population doublings with stable expression of molecular markers and functional properties of human adipocytes [82]. This finding could prove significant when culturing cells for the formation of adipose tissues. ASCs show many advantages over BMSCs, such as minimally invasive harvesting procedure (aspiration and excision), more clinically-relevant numbers of extractable cells (adipose tissues represent an even more plentiful reservoir of adult stem cells [∼2%] than bone marrow [0.002%] or other connective tissues), and more active proliferation than that for BMSCs [85, 86]. More importantly, the adipogenic capacity of ASCs is higher than the other differentiation lineages if only a suitable 3D scaffold is provided [87]. For these reasons, there is a great interest in ASC applications for adipose tissue engineering [88].
Preadipocytes, found in the stromal-vascular fraction of adipose tissue, are also able to differentiate into mature adipocytes [89]. Preadipocyte clonal lines from rodents (3T3-L1 cells) have been utilized to gain insight into the molecular mechanisms of adipogenesis and drug screening [90]. Human preadipocyte sources, however, are prone to having a decreased differentiation capacity with elevated passage number before their growth stops and replicative senescence is reached [91]. Although this limitation can be circumvented by genetic modification, these transduced cell lines fail to recapitulate the lipolytic responses specific to human adipocytes and secretion of specific adipocytokines upon differentiation. Furthermore, chromosomal abnormalities were also observed in some transduced cell lines, impeding their wide application in engineering of adipose tissue [92, 93]. No attempt has been described for separating preadipocytes from ASCs in the context of adipose tissue engineering.
Biomaterial Scaffolds
Numerous scaffolds for tissue-engineered adipose have been investigated. With respect to biomaterial scaffold-based de novo adipogenesis, ASCs or preadipocytes can be cultured on suitable polymeric scaffolds with appropriate growth factors, and form 3D constructions for implantation into a patient’s breast defect site [85, 94]. In addition to providing structural stability for developing adipose tissues, scaffolds with desirable biochemical and biophysical cues can direct ASCs or preadipocyte behavior and function. A desirable scaffold for synthetic adipose tissue construction should possess biocompatibility, degradability, and soft tissue-like mechanical properties with support for vascularization [94]. A number of biomaterials have been exploited for adipose tissue engineering in vitro and in vivo, and advantages and disadvantages of these systems have been reported [94, 95]. The focus of this section of this review is on recent applications of natural and synthetic polymers for adipose tissue construction, updating progress in the field of adipose tissue-related mammary gland regeneration.
Naturally-Derived Biomaterials
Natural biomaterials are found as components of the native ECM or those generated by biological systems. Their application in regenerative medicine is advantageous with respect to biocompatibility, and mechanical and biological properties, which match those that exist in vivo. As a major component of native ECM, collagen has been utilized extensively as a natural biomaterial, in gel, sponge, and microbead forms, to support the adipogenic differentiation of ASCs and precursor cells. Human preadipocyte-loaded collagen sponges with uniform 40 μm pore sizes and regular lamellar structures promoted well-vascularized adipose-like tissue formation after being implanted into immuno-deficient mice. However, significant graft weight loss was observed after 3 weeks in vivo [96]. By optimizing cell seeding density and controlled-release of growth factor supplements, hASC loaded-type I collagen scaffolds supported de novo adipogenesis up to 24 weeks. This was evidenced by the successful outcomes of larger functional adipose tissue formed after implantation [97]. To enhance the structural stability of collagen-based sponges, a highly porous collagen-hyaluronic acid (HA) scaffold was produced by a controlled freeze-drying technique and crosslinked with 1-ethyl-3-(3-dimethy-laminopropyl)-carbodiimide hydrochloride. These scaffolds supported the proliferation and differentiation of 3T3-L1 preadipocytes, enhanced functional gene expression, and offered robust, freely-permeable 3D matrices that enhanced mammary adipose tissue development in vitro [98]. To form a complex tissue that more closely resembles the normal human breast, collagen gels have also been used as a 3D biological matrix upon which preadipocytes were co-cultured with human MECs isolated from the same patient. A pattern of ductal structures of human MECs within clusters of adipocytes was observed, which is much more similar to the architecture of breast tissue. This result indicates the potential for breast tissue to be regenerated in vitro on a 3D collagen scaffold and later implanted for the regeneration of mammary gland [54].
Due to their soft, tissue-like mechanical properties, cross-linked gelatin-based scaffolds have been considered as candidates for adipose tissue engineering. Moreover, their biodegradation rate can be controlled by the extent of chemical cross-linking. Human MSCs were seeded on gelatin sponges and exposed to adipogenic differentiation medium in vitro; the resulting constructs showed accumulated lipid droplets and expanded with culture [87]. In combination with the collagen scaffolds, gelatin microspheres containing basic FGF enabled hASCs to induce maximum adipose tissue formation at the implanted site [99]. Recently, in combination with polyglycolic acid and polypropylene meshes, gelatin sponges seeded with hASCs have been shown to support completely differentiated, vascularized adipose tissue in vivo. More importantly, the constructs retained their predefined shape and dimensions for up to 6 months. This is the most sustainable adipose tissue construct reported, suggesting its potential in the field of mammary gland tissue engineering [100].
Silks are naturally occurring protein polymers produced by a wide variety of insects and spiders. As the core protein filament, silk fibroin is a versatile natural biomaterial that has been utilized in a range of tissue engineering studies [101–103]. Biocompatibility, slow degradability and remarkable mechanical properties, as well as controlled molecular structure and morphology through versatile processing and surface modifications, constitute the reasons for interest in this protein as a tissue engineering scaffold [104–106]. To meet different requirements for different applications, various silk formats have been developed, such as films, fibers, meshes, hydrogels, and porous sponge scaffolds. These materials support stem cell adhesion, proliferation, and differentiation in vitro and promote tissue repair in vivo [107–109]. Silk scaffolds with hMSCs or hASCs supported significant up-regulation of adipogenic gene expression and lipid accumulation following cultivation in adpogenic medium [110]. After 4 weeks of implantation in a rat muscle pouch defect model, silk scaffolds supported in vivo adipogenesis either alone or when seeded with hASCs or hMSCs. In contrast, collagen and poly-lactic acid (PLA)-based scaffolds rapidly degraded following implantation. These results suggested that macroporous silk scaffolds offer an important platform for cell-based adipose tissue engineering, and in particular, provide longer-term structural integrity to promote the maintenance of adipose tissue in vivo. Using similar silk scaffolds, an in vitro 3D model for human vascularized adipose tissue was generated by co-culturing hASCs and human umbilical vein endothelial cells (HUVECs) [111]. Moreover, a 3D culture surrogate of complex human breast tissue that included a tri-culture system, composed of human MECs, predifferentiated hASCs and mammary fibroblasts in a Matrigel™/collagen mixture in porous silk scaffolds was also developed [112]. In this complex tri-culture system, the presence of stromal cells induced both alveolar and ductal morphogenesis and also enhanced casein-α and β expression when compared with co-cultures or monocultures. Hence, this experimental model provides an informative human breast tissue system with which to study normal breast morphogenesis and neoplastic transformation. It suggests that a combination of 3D porous silk scaffold and stem cells (especially hASCs) represent encouraging option for stem cell-based adipose tissue engineering (Fig. 1).
Synthetically Derived Biomaterials
Several synthetic biomaterials have also been utilized in bioengineering adipose tissue in vitro and for de novo adipogenesis in vivo [94, 113]. This is due to their tunable mechanical properties, chemical properties and degradability, as well as biocompatibility. Copolymer scaffolds of PLGA (poly-lactic-co-glycolic acid) seeded with rat preadipocytes has been shown to support adipogenesis after subcutaneous implantation for up to 2 months [114]. However, the volume of generated adipose tissue decreased in a long-term study (up to 12 month) [72]. Volume-stable adipose tissues were engineered in vivo using a mechanical support structure of dome-shaped poly(glycolic acid) fiber-based matrices with PLGA [115]. In this study, the PLGA scaffolds were placed into subcutaneous pockets of athymic mice and human preadipocytes suspended in a fibrin matrix were injected into the space under the support structures. Six weeks after implantation, the original implant displayed significant adipogenesis with stable volume when compared to the control group, suggesting the potential of PLGA scaffolds for augmentation of adipose tissue with volume conservation.
Other than PLGA-based scaffolds, photopolymerizable polyethylene glycol (PEG)-base hydrogels that conjugated with both degradation sites and cell adhesion ligands have also been shown to support preadipocyte proliferation and differentiation subsequent to polymer degradation in vivo [116]. Recently, to better understand the mechanisms of adipose tissue differentiation, especially the role of 3D microenvironment in de novo adipogenesis in vivo, in vitro culture systems that closely mimic the geometry of the native adipose tissue were developed. In these studies, mouse preadipocytes or ESCs were seeded onto the nonbiodegradable fibrous polyethylene terephthalate (PET) or electrospun polycaprolactone (PCL), and were induced into differentiation with an adipogenic cocktail medium [117, 118]. The results showed that compared with the 2D culture system, these 3D matrices offer more advantages in promoting the lineage differentiation of those stem cell (preadipocyte or ESCs) into mature adipocytes, as demonstrated by their (differentiated cells) more developed morphology, enhanced functional activity, and increased gene and protein expression level. These further support the utility of synthetic biomaterial scaffolds in constructing adipose tissue model, suggesting their central role in regenerating more suitable microenvironment for adipogenesis.
Conclusions and Future Challenges
Utilization of synthetic adipose tissue models has been effective in studying mammary gland morphogenesis, development, and tumorigenesis, and for regenerating mammary gland tissue in vitro or in vivo. Given that the multiple cell types contribute to the overall complex character of mammary gland tissue, it is imperative to include several stromal cell types for investigating paracrine signaling or cell-cell contact mediated epithelial behavior. Hence, one of the major challenges ahead is to propel the design of synthetic adipose tissue model systems further and incorporate multiple cell types, such as epithelial cells, fibroblasts, endothelial cells, and macrophages into a single system [119]. This, along with incorporation of adequate matrix scaffolds, will allow us to generate more complex, realistic mammary gland tissue models. In addition, model systems should be developed that recapitulate the complex hormonal signaling unique to the mammary gland. Establishment of hormone responsive MEC and stromal cell lines will significantly broaden the utility of synthetic epithelial-adipose tissue models for the investigation of mammary development and tumorigenesis [119]. To address this challenge, interdisciplinary collaborations are needed. With the evolutions in cell and developmental biology, material science, biological microfabrication as well as nanobiotechnology, it is plausible to construct designer tissue models in which the chemistry, geometry, and mechanics can be controlled at every scale. These strategies will allow for an improved understanding of the dynamic interplay that exists between different cells of the mammary gland, under both normal and aberrant conditions, such as those encountered in breast cancer. These types of models will also contribute to adipose tissue engineering for regenerating mammary gland tissue.
Abbreviations
- MEC:
-
Mammary epithelial cells
- MFP:
-
Mammary fat pad
- ECM:
-
Extracellular matrix
- 2D:
-
Two dimensional
- 3D:
-
Three dimensional
- IGF:
-
Insulin-like growth factor
- PGE-2:
-
Prostaglandin E2
- HGF:
-
Hepatocyte growth factor
- FGFs:
-
Fibroblast growth factors
- PR:
-
Progesterone receptor
- ERα/β:
-
Estrogen receptor α/β
- αERKO mice:
-
Estrogen receptor α-disrupted mice
- E2:
-
Estradiol
- ESCs:
-
Embryonic stem cells
- iPSCs:
-
Induced pluripotent stem cells
- EBs:
-
Embryoid bodies
- hMSCs:
-
Human mesenchymal stem cells
- BMSCs:
-
Bone marrow derived mesenchymal stem cells
- ASCs:
-
Adipose-derived stem cells
- hASCs:
-
Human adipose-derived stem cells
- TDLUs:
-
Terminal duct lobular units
- shRNA :
-
Short hairpin RNA
- HA:
-
Hyaluronic acid
- HUVEC:
-
Human umbilical vein endothelial cells
- PLGA:
-
Poly L-lactic acid
- PLA:
-
Poly-lactic acid
- PEG:
-
Polyethylene glycol
- PET:
-
Polyethylene terephthalate
- PCL:
-
Polycaprolactone
References
Daniel CW, Silberstein GB. Postnatal development of the rodent mammary gland. In: Neville MC, Daniel CW, editors. The mammary gland development, regulation, and function. New York: Plenum; 1987. p. 3–36.
Parmar H, Cunha GR. Epithelial-stromal interactions in the mouse and human mammary gland in vivo. Endocr Relat Cancer. 2004;11:437–58.
Levine JF, Stockdale FE. Cell-cell interactions promote mammary epithelial cell differentiation. J Cell Biol. 1985;100:1415–22.
Schmeichel KL, Weaver VM, Bissell MJ. Structural cues from the tissue microenvironment are essential determinants of the human mammary epithelial cell phenotype. J Mammary Gland Biol Neoplasia. 1998;3(2):201–13.
Cunha GR, Hayward SW, Wang YZ. Role of stroma in carcinogenesis of the prostate. Differentiation. 2002;70:473–85.
Cunha GR, Hayward SW, Wang YZ, Ricke WA. Role of the stromal microenvironment in carcinogenesis of the prostate. Int J Cancer. 2003;107:1–10.
Cunha GR, Young P, Christov K, Guzman R, Nandi S, Talamantes F, et al. Mammary phenotypic expression induced in epidermal cells by embryonic mammary mesenchyme. Acta Anat. 1995;152:195–204.
Barcellos-Hoff MH, Ravani SA. Irradiated mammary gland stroma promotes the expression of tumorigenic potential by unirradiated epithelial cells. Cancer Res. 2000;60:1254–60.
Maffini MV, Soto AM, Calabro JM, Ucci AA, Sonnenschein C. The stroma as a crucial target in rat mammary gland carcinogenesis. J Cell Sci. 2004;117:1495–502.
Krause S, Maffini MV, Soto AM, Sonnenschein C. A novel 3D in vitro culture model to study stromal-epithelial interactions in the mammary gland. Tissue Eng. 2008;14:261–71.
Darcy KM, Zangani D, Shea-Eaton W, Shoemaker SF, Lee PP, Mead LH, et al. Mammary fibroblasts stimulate growth, alveolar morphogenesis, and functional differentiation of normal rat mammary epithelial cells. In Vitro Cell Dev Biol Anim. 2000;36:578–92.
Sadlonova A, Novak Z, Johnson MR, Bowe DB, Gault SR, Page GP, et al. Breast fibroblasts modulate epithelial cell proliferation in three-dimensional in vitro co-culture. Breast Cancer Res. 2005;7:R46–59.
Frühbeck G. Overview of adipose tissue and its role in obesity and metabolic disorders. Methods Mol Biol. 2008;456:1–22.
Nawrocki AR, Scherer PE. Keynote review: the adipocyte as a drug discovery target. Drug Discov Today. 2005;10:1219–30.
Rhodes NP. Inflammatory signals in the development of tissue-engineered soft tissue. Biomaterials. 2007;28:5131–6.
Sakakura T. Mammary embryogenesis. In: Neville MC, Daniel CW, editors. The mammary gland: development, regulation, and function. New York: Plenum; 1987. p. p37–63.
Neville MC, Medina D, Monks J, Hovey RC. The mammary fat pad. J Mammary Gland Biol Neoplasia. 1998;3:109–16.
Hovey RC, McFadden TB, Akers RM. Regulation of mammary gland growth and morphogenesis by the mammary fat pad: a species comparison. J Mammary Gland Biol Neoplasia. 1999;4:53–68.
Wiseman BS, Werb Z. Stromal effects on mammary gland development and breast cancer. Science. 2002;296:1046–9.
Howard BA, Gusterson BA. Human breast development. J Mammary Gland Biol Neoplasia. 2000;5:119–37.
Hennighausen L, Robinson GW. Information networks in the mammary gland. Nat Rev Mol Cell Biol. 2005;6:715–25.
Couldrey C, Moitra J, Vinson C, Anver M, Nagashima K, Green J. Adipose tissue: a vital in vivo role in mammary gland development but not differentiation. Dev Dyn. 2002;223:459–68.
Kratochwil K. Epithelium–mesenchyme interaction in the fetal mammary gland. In: Medina D, Kidwell W, Heppner G, Anderson E, editors. Cellular and molecular biology of mammary cancer. New York, 1987. p. 67–80.
Sakakura T, Sakagami Y, Nishizuka Y. Dual origin of mesenchymal tissues participating in mouse mammary gland embryogenesis. Dev Biol. 1982;91:202–7.
Kimata K, Sakakura T, Inaguma Y, Kato M, Nishizuka Y. Participation of two different mesenchymes in the developing mouse mammary gland: synthesis of basement membrane components by fat pad precursor cells. J Embryol Exp Morphol. 1985;89:243–57.
Ailhaud G, Grimaldi P, Négrel R. Cellular and molecular aspects of adipose tissue development. Annu Rev Nutr. 1992;12:207–33.
Zangani D, Darcy KM, Shoemaker S, Ip MM. Adipocyte–epithelial interactions regulate the in vitro development of normal mammary epithelial cells. Exp Cell Res. 1999;247:399–409.
Fendrick JL, Raafat AM, Haslam SZ. Mammary gland growth and development form the postnatal period to post-menopause: ovarian steroid receptor ontogeny and regulation in the mouse. J Mammary Gland Biol Neoplasia. 1998;3:7–22.
Rudland PS, Twiston Davies AC, Tsao SW. Rat mammary preadipocytes in culture produce a trophic agent for mammary epithelia-prostaglandin E2. J Cell Physiol. 1984;120:364–76.
Niemann C, Brinkmann V, Birchmeier W. Hepatocyte growth factor and neuregulin in mammary gland cell morphogenesis. Adv Exp Med Biol. 2000;480:9–18.
Ruan W, Kleinberg DL. Insulin-like growth factor I is essential for terminal end bud formation and ductal morphogenesis during mammary development. Endocrinology. 1999;140:5075–81.
Chakravorti S, Sheffield LG. Acidic and basic fibroblast growth factor mRNA and protein in mouse mammary glands. Endocr. 1996;4:175–82.
Keely PJ, Wu JE, Santoro SA. The spatial and temporal expression of the alpha 2 beta 1 integrin and its ligands, collagen I, collagen IV, and laminin, suggest important roles in mouse mammary morphogenesis. Differentiation. 1995;59:1–13.
Klinowska TC, Soriano JV, Edwards GM, Oliver JM, Valentijn AJ, Montesano R, et al. Laminin and beta1 integrins are crucial for normal mammary gland development in the mouse. Dev Biol. 1999;215:13–32.
Medina D. The mammary gland: a unique organ for the study of development and tumorigenesis. J Mammary Gland Biol Neoplasia. 1996;1:5–19.
Berger JJ, Daniel CW. Stromal DNA synthesis is stimulated by young, but not serially aged, mouse mammary epithelium. Mech Ageing Dev. 1983;23(3–4):277–84.
Sakakura T, Kusano I, Kusakabe M, Inaguma Y, Nishizuka Y. Biology of mammary fat pad in fetal mouse: capacity to support development of various fetal epithelia in vivo. Development. 1987;100:421–30.
Humphreys RC, Lydon J, Omalley BW, Rosen JM. Mammary gland development is mediated by both stromal and epithelial progesterone receptors. Mol Endocrinol. 1997;11:801–11.
Korach KS, Couse JF, Curtis SW, Washburn TF, Lindzey J, Kimbro KS, et al. Estrogen receptor gene disruption: molecular characterization and experimental and clinical phenotypes. Recent Prog Horm Res. 1996;51:159–88.
Bocchinfuso WP, Korach KS. Mammary gland development and tumorigenesis in estrogen receptor knockout mice. J Mammary Gland Biol Neoplasia. 1997;2:323–34.
Mallepell S, Krust A, Chambon P, Brisken C. Paracrine signaling through the epithelial estrogen receptor alpha is required for proliferation and morphogenesis in the mammary gland. Proc Natl Acad Sci USA. 2006;103:2196–201.
Cunha GR, Young P, Hom YK, Cooke PS, Taylor JA, Lubhan DB. Elucidation of a role of stromal steroid hormone receptors in mammary gland growth and development by tissue recombination experiments. J Mammary Gland Biol Neoplasia. 1997;2:393–402.
Mueller SO, Clark JA, Myers PH, Korach KS. Mammary gland development in adult mice requires epithelial and stromal estrogen receptor alpha. Endocrinology. 2002;143:2357–65.
Sheffield LG. Organization and growth of mammary epithelia in the mammary gland fat pad. J Dairy Sci. 1988;71:2855–74.
Yang J, Tsukamoto T, Popnikolov N, Guzman RC, Chen XY, Yang JH, et al. Adenoviral-mediated gene transfer into primary human and mouse mammary epithelial cells in vitro and in vivo. Cancer Lett. 1995;98:9–17.
Sheffield LG, Welsch CW. Transplantation of human breast epithelia to mammary-gland-free fat-pads of athymic nude mice: influence of mammotrophic hormones on growth of breast epithelia. Int J Cancer. 1988;41:713–9.
Hillman EA, Valerio MG, Halter SA, Barrett-Boone LA, Trump BF. Long-term explant culture of normal mammary epithelium. Cancer Res. 1983;43:245–57.
Kuperwasser C, Chavarria T, Wu M, Magrane G, Gray JW, Carey L, et al. Reconstruction of functionally normal and malignant human breast tissues in mice. Proc Natl Acad Sci. 2004;101:4966–71.
Proia DA, Kuperwasser C. Reconstruction of human mammary tissues in a mouse model. Nat Protoc. 2006;1:206–14.
Levine JF, Stockdale FE. 3T3-L1 adipocytes promote the growth of mammary epithelium. Exp Cell Res. 1984;151:112–22.
Wiens D, Park CS, Stockdale FE. Milk protein expression and ductal morphogenesis in the mammary gland in vitro: hormone-dependent and –independent phases of adipocyte-mammary epithelial cell interaction. Dev Biol. 1987;120:245–58.
Bissell MJ, Rizki A, Mian IS. Tissue architecture: the ultimate regulator of breast epithelial function. Curr Opin Cell Biol. 2003;15:753–62.
Pickl M, Ries CH. Comparison of 3D and 2D tumor models reveals enhanced HER2 activation in 3D associated with an increased response to trastuzumab. Oncogene. 2009;28:461–8.
Huss FR, Kratz G. Mammary epithelial cell and adipocyte co-culture in a 3-D matrix: the first step towards tissue-engineered human breast tissue. Cells Tissues Organs. 2001;169:361–7.
Wang X, Zhang X, Sun L, Subramanian B, Maffini MV, Soto A, et al. Preadipocytes stimulate ductal morphogenesis and functional differentiation of human mammary epithelial cells on 3D silk scaffolds. Tissue Eng. 2009;15:3087–98.
Friedl P, Gilmour D. Collective cell migration in morphogenesis, regeneration and cancer. Nat Rev Mol Cell Biol. 2009;10:445–57.
Visvader JE, Lindeman GJ. Transcriptional regulators in mammary gland development and cancer. Int J Biochem Cell Biol. 2003;35:1034–51.
Mettlin C. Global breast cancer mortality statistics. CA Cancer J Clin. 1999;49:138–44.
Thomsen A, Kolesar JM. Chemoprevention of breast cancer. Am J Health Syst Pharm. 2008;65:2221–8.
Haslam SZ, Woodward TL. Host microenvironment in breast cancer development: epithelial-cell-stromal-cell interactions and steroid hormone action in normal and cancerous mammary gland. Breast Cancer Res. 2003;5:208–15.
Chamras H, Bagga D, Elstner E, Setoodeh K, Koeffler HP, Heber D. Preadipocytes stimulate breast cancer cell growth. Nutr Cancer. 1998;32:59–63.
Muehlberg FL, Song YH, Krohn A, Pinilla SP, Droll LH, Leng X, et al. Tissue-resident stem cells promote breast cancer growth and metastasis. Carcinogenesis. 2009;30:589–97.
Manabe Y, Toda S, Miyazaki K, Sugihara H. Mature adipocytes, but not preadipocytes, promote the growth of breast carcinoma cells in collagen gel matrix culture through cancer-stromal cell interactions. J Pathol. 2003;201:221–8.
Hajian-Tilaki KO, Gholizadehpasha AR, Bozorgzadeh S, Hajian-Tilaki E. Body mass index and waist circumference are predictor biomarkers of breast cancer risk in Iranian women. Med Oncol. 2010; Epub ahead of print].
Boyd NF, Martin LJ, Yaffe M, Minkin S. Mammographic density. Breast Cancer Res. 2009;Suppl 3:S4.
Boyd NF, Martin LJ, Bronskill M, Yaffe MJ, Duric N, Minkin S. Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst. 2010;102:1224–37.
Patrick Jr CW. Adipose tissue engineering: the future of breast and soft tissue reconstruction following tumor resection. Semin Surg Oncol. 2000;19:302–11.
Patrick CW. Breast tissue engineering. Annu Rev Biomed Eng. 2004;6:109–30.
Adissu HA, Asem EK, Lelièvre SA. Three-dimensional cell culture to model epithelia in the female reproductive system. Reprod Sci. 2007;14:11–9.
Nelson CM, Bissell MJ. Modeling dynamic reciprocity: engineering three-dimensional culture models of breast architecture, function, and neoplastic transformation. Sem Cancer Biol. 2005;15:342–52.
Patrick Jr CW, Zheng B, Johnston C, Reece GP. Long-term implantation of preadipocyte seeded PLGA scaffolds. Tissue Eng. 2002;8:283–93.
Gomillion CT, Burg KJ. Stem cells and adipose tissue engineering. Biomaterials. 2006;27:6052–63.
Mimeault M, Batra SK. Concise review: recent advances on the significance of stem cell in tissues regeneration and cancer therapy. Stem Cells. 2006;24:26–33.
Tárnok A, Ulrich H, Bocsi J. Phenotypes of stem cells from diverse origin. Cytom A. 2010;77:6–10.
Leeb C, Jurga M, McGuckin C, Moriggl R, Kenner L. Promising new sources for pluripotent stem cells. Stem Cell Rev. 2010;6:15–26.
Wernig M, Meissner A, Foreman R, Brambrink T, Ku M, Hochedlinger K, et al. In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state. Nature. 2007;448:318–24.
Xiong C, Xie CQ, Zhang L, Zhang J, Xu K, Fu M, et al. Derivation of adipocytes from human embryonic stem cells. Stem Cell Dev. 2005;14:671–5.
Hannan NR, Wolvetang EJ. Adipocyte differentiation in human embryonic stem cells transduced with Oct4 shRNA lentivirus. Stem Cell Dev. 2009;18:653–60.
Taura D, Noguchi M, Sone M, Hosoda K, Mori E, Okada Y, et al. Adipogenic differentiation of human induced pluripotent stem cells: comparison with that of human embryonic stem cells. FEBS Lett. 2009;583:1029–33.
Jackson L, Jones DR, Scotting P, Sottile V. Adult mesenchymal stem cells: differentiation potential and therapeutic applications. J Postgrad Med. 2007;53:121–7.
Zippel N, Schulze M, Tobiasch E. Biomaterials and mesenchymal stem cells for regenerative medicine. Recent Pat Biotechnol. 2010;4:1–22.
Rodriguez AM, Elabd C, Delteil F, Astier J, Vernochet C, Saint-Marc P, et al. Adipocyte differentiation of multipotent cells established from human adipose tissue. Biochem Biophys Res Commun. 2004;315:255–63.
Zuk PA, Zhu M, Ashjian P, De Ugarte DA, Huang JI, Mizuno H, et al. Human adipose tissue is a source of multipotent stem cells. Mol Biol Cell. 2002;13:4279–95.
Cherubino M, Marra KG. Adipose-derived stem cells for soft tissue reconstruction. Regen Med. 2009;4:109–17.
Tanzi MC, Farè S. Adipose tissue engineering: state of the art, recent advances and innovative approaches. Expert Rev Med Devices. 2009;6:533–51.
Zhu Y, Liu T, Song K, Fan X, Ma X, Cui Z. Adipose-derived stem cell: a better stem cell than BMSC. Cell Biochem Funct. 2008;26:664–75.
Hong L, Peptan I, Clark P, Mao JJ. Ex vivo adipose tissue engineering by human marrow stromal cell seeded gelatin sponge. Ann Biomed Eng. 2005;33:511–7.
Gimble JM, Katz AJ, Bunnell BA. Adipose-derived stem cells for regenerative medicine. Circ Res. 2007;100(9):1249–60.
Tchkonia T, Tchoukalova YD, Giorgadze N, Pirtskhalava T, Karagiannides I, Forse RA, et al. Abundance of two human preadipocyte subtypes with distinct capacities for replication, adipogenesis, and apoptosis varies among fat depots. Am J Physiol Endocrinol Metab. 2005;288:E267–77.
Ailhaud G, Hauner H. Development of white adipose tissue. In: Bray AG, Bouchard C, editors. Handbook of obesity. 2nd ed. New York: Marcel Dekker; 2003.
Kirkland JL, Dobson DE. Preadipocyte function and aging: links between age-related changes in cell dynamics and altered fat tissue function. J Am Geriatr Soc. 1997;45:959–67.
Zilberfarb V, Pietri-Rouxel F, Jockers R, Krief S, Delouis C, Issad T, et al. Human immortalized brown adipocytes express functional beta3-adrenoceptor coupled to lipolysis. J Cell Sci. 1997;110:801–7.
Darimont G, Zbinden I, Avanti O, Leone-Vautravers P, Giusti V, Burckhardt P, et al. Reconstitution of telomerase activity combined with HPV-E7 expression allow human preadipocytes to preserve their differentiation capacity after immortalization. Cell Death Differ. 2003;10:1025–31.
Hemmrich K, von Heimburg D. Biomaterials for adipose tissue engineering. Expert Rev Med Devices. 2006;3:635–45.
Choi JH, Gimble JM, Lee K, Marra KG, Rubin JP, Yoo JJ, et al. Tissue engineering for soft tissue regeneration. Tissue Eng Part B. 2010;16:413–26.
Von Heimburg D, Zachariah S, Heschel I, Kühling H, Schoof H, Hafemann B, et al. Human preadipocytes seeded on freeze-dried collagen scaffolds investigated in vitro and in vivo. Biomaterials. 2001;22:429–38.
Tsuji W, Inamoto T, Yamashiro H, Ueno T, Kato H, Kimura Y, et al. Adipogenesis induced by human adipose tissue-derived stem cells. Tissue Eng A. 2009;15:83–93.
Davidenko N, Campbell JJ, Thian ES, Watson CJ, Cameron RE. Collagen-hyaluronic acid scaffolds for adipose tissue engineering. Acta Biomater. 2010;6:3957–68.
Kimura Y, Ozeki M, Inamoto T, Tabata Y. Adipose tissue engineering based on human preadipocytes combined with gelatin microspheres containing basic fibroblast growth factor. Biomaterials. 2003;24:2513–21.
Lin SD, Wang KH, Kao AP. Engineered adipose tissue of predefined shape and dimensions from human adipose-derived mesenchymal stem cells. Tissue Eng A. 2008;14:571–81.
Leal-Egaña A, Scheibel T. Silk-based materials for biomedical applications. Biotechnol Appl Biochem. 2010;55:155–67.
Wang Y, Kim HJ, Vunjak-Novakovic G, Kaplan DL. Stem cell-based tissue engineering with silk biomaterials. Biomaterials. 2006;27:6064–82.
Altman GH, Horan RL, Lu HH, Moreau J, Martin I, Richmond JC, et al. Silk matrix for tissue engineered anterior cruciate ligaments. Biomaterials. 2002;23:4131–41.
Murphy AR, Kaplan DL. Biomedical applications of chemically-modified silk fibroin. J Mater Chem. 2009;19:6443–50.
Amsden JJ, Domachuk P, Gopinath A, White RD, Negro LD, Kaplan DL, et al. Biocompatible films: rapid nanoimprinting of silk fibroin films for biophotonic applications. Adv Mater. 2010;22(15).
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J, et al. Silk-based biomaterials. Biomaterials. 2003;24:401–16.
Lu Q, Zhang X, Hu X, Kaplan DL. Green process to prepare silk fibroin/gelatin biomaterial scaffolds. Macromol Biosci. 2010;10:289–98.
Lovett ML, Cannizzaro CM, Vunjak-Novakovic G, Kaplan DL. Gel spinning of silk tubes for tissue engineering. Biomaterials. 2008;29:4650–7.
Gil ES, Park SH, Marchant J, Omenetto F, Kaplan DL. Response of human corneal fibroblasts on silk film surface patterns. Macromol Biosci. 2010;10:664–73.
Mauney JR, Nguyen T, Gillen K, Kirker-Head C, Gimble JM, Kaplan DL. Engineering adipose-like tissue in vitro and in vivo utilizing human bone marrow and adipose-derived mesenchymal stem cells with silk fibroin 3D scaffolds. Biomaterials. 2007;28:5280–90.
Kang JH, Gimble JM, Kaplan DL. In vitro 3D model for human vascularized adipose tissue. Tissue Eng A. 2009;15:2227–36.
Wang X, Sun L, Maffini MV, Soto A, Sonnenschein C, Kaplan DL. A complex 3D human tissue culture system based on mammary stromal cells and silk scaffolds for modeling breast morphogenesis and function. Biomaterials. 2010;31:3920–9.
Morgan SM, Ainsworth BJ, Kanczler JM, Babister JC, Chaudhuri JB, Oreffo RO. Formation of a human-derived fat tissue layer in P(DL)LGA hollow fibre scaffolds for adipocyte tissue engineering. Biomaterials. 2009;30:1910–7.
Patrick Jr CW, Chauvin PB, Reece GP. Preadipocyte seeded PLGA scaffolds for adipose tissue engineering. Tissue Eng. 1999;5:139–51.
Cho SW, Kim SS, Rhie JW, Cho HM, Choi CY, Kim BS. Engineering of volume-stable adipose tissues. Biomaterials. 2005;26:3577–85.
Brandl FP, Seitz AK, Tessmar JK, Blunk T, Göpferich AM. Enzymatically degradable poly(ethylene glycol) based hydrogels for adipose tissue engineering. Biomaterials. 2010;31:3957–66.
Kang X, Xie Y, Kniss DA. Adipose tissue model using three-dimensional cultivation of preadipocytes seeded onto fibrous polymer scaffolds. Tissue Eng. 2005;11:458–68.
Kang X, Xie Y, Powell HM, James Lee L, Belury MA, Lannutti JJ, et al. Adipogenesis of murine embryonic stem cells in a three-dimensional culture system using electrospun polymer scaffolds. Biomaterials. 2007;28:450–8.
Shaw KR, Wrobel CN, Brugge JS. Use of three-dimensional basement membrane cultures to model oncogene-induced changes in mammary epithelial morphogenesis. J Mammary Gland Biol Neoplasia. 2004;9:297–310.
Acknowledgements
This work has been funded by NIH grant number P41 EB002520 for the Tissue Engineering Resource Center (TERC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, X., Reagan, M.R. & Kaplan, D.L. Synthetic Adipose Tissue Models for Studying Mammary Gland Development and Breast Tissue Engineering. J Mammary Gland Biol Neoplasia 15, 365–376 (2010). https://doi.org/10.1007/s10911-010-9192-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10911-010-9192-y