Abstract
Asian Americans (AAs) are more likely to use complementary and alternative medicine (CAM) compared to other race/ethnicities, yet previous studies have conflicting results. The 2012 National Health Interview Survey data was analyzed to investigate AA’s (n = 2214) CAM use for treatment. AAs were divided into four subgroups: Chinese, Asian Indian, Filipino, and Other Asian. Only 9% of AAs reported using CAM for treatment, with 6% indicating CAM use specifically for chronic conditions. This could be a form of medical pluralism, a mixture of Eastern and Western health approaches. The “Other Asian” subgroup reported highest use of CAM for treatment. Significant predictors included age (≥ 65 years) and high educational attainment (≥ college degree). Sociodemographic factors were also significant predictors within Asian subgroups. Further investigation of this and other forms of medical pluralism among AAs are needed to explore potential cofounders and risks like underreporting, CAM schedules/dosages, cultural influences, and CAM’s impact on one’s health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asian-Americans (AAs) are more likely to use complementary and alternative medicine (CAM) compared to other races/ethnicities [1,2,3,4]. This is somewhat expected, as many AAs have strong cultural traditions of using Eastern alternative medicine systems [EAMS] (e.g., traditional Chinese medicine, Ayurveda) and healing practices (e.g., yoga, tai chi). Although AAs have reported valuing the use of CAM for wellness, they were less likely to report herbal therapy use for treatment versus non-Hispanic whites (38% vs 59%) [4]. This was an unexpected finding, since EAMS, including use of herbal therapies, have been and are still used by AAs to treat many conditions/diseases [5,6,7,8]. Inconsistencies among studies lead to questions like: are AAs primarily using conventional medicine for treatment of disease/symptoms, or could they be underreporting their use of CAM for treatment? Using prevalence data from national surveys can help clarify how specific AA subgroups use CAM for treatment of medical problems.
To determine different types of CAM reported by disaggregated AA subgroups, studies which analyzed U.S. health data on CAM use were reviewed. Previous studies of the National Health Interview Survey (NHIS) data have found higher rates of CAM use for individuals with chronic conditions or specific acute conditions [10,11,12,13,14,15]. However, these studies did not differentiate CAM use for health and wellness versus treatment of specific health conditions. One study showed that 13.9% of respondents reported CAM use for treatment only, 35.1% for both treatment and wellness, and 51% for wellness only [16]. In the same study, Asians were twice as likely to report CAM use for wellness only compared to treatment only [16]. In addition, few studies have looked at the prevalence of CAM use in the treatment of specific health conditions, such as low back pain (21.1%) [17]; gastrointestinal conditions (3%) [11]; type 1 diabetes (7.1%) and type 2 diabetes (3.4%) [15], and insomnia (1.8%) [18]. However, these studies did not compare differences across races/ethnicities or AA subgroups in the use of CAM for treatment of health conditions.
Asian culture and tradition emphasize the use of EAMS, which provide a holistic approach to treating illnesses, and AAs exposed to both Eastern and Western health approaches are more likely to engage in medical pluralism, defined as “the adoption of more than one medical system in terms of health beliefs, behaviors, or treatments” [19]. The use of CAM to treat health conditions could lead to medical pluralism engagement.
There is an increased interest in understanding medical pluralism in the U.S. and other developed countries, especially with growing evidence of the public’s use of CAM [20]. Scholars attribute the growing awareness and interest in medical pluralism to the realization that we live in a diverse society and that CAM may be but one of many cultural preferences for healthcare and treatment [3, 21, 22]. However, only a few studies have quantified the use of CAM in conjunction with the use of Western medicine [23,24,25,26]. Continuing research in this field is imperative, as CAM use as a type of medical pluralism raises potential healthcare concerns such as choosing to delay access to needed healthcare, potential drug–herb interactions, and healthcare providers’ readiness (or lack thereof) to integrate CAM into treatment regimens.
Therefore, in order to explicate prevalence, patterns, and predictors of CAM use for treatment of health conditions between AA subgroups, a secondary analysis of 2012 NHIS CAM data was conducted to provide insight into how different AA subgroups could potentially use CAM to engage in medical pluralism.
Methods
Data Source and Study Population
The NHIS is an annual survey of U.S. households from noninstitutionalized populations [9]. This study’s sample consisted of Asian adult respondents (> 18 years) of the 2012 NHIS core and CAM supplemental survey. The 2012 NHIS core and CAM supplement survey data, questionnaires, and related documentation can be accessed through https://www.cdc.gov/nchs/nhis/nhis_2012_data_release.htm.
The 2012 NHIS publicly available dataset provides disaggregated race data, dividing AA subgroups into Chinese, Asian Indian, and Filipino; and, to follow confidentiality regulations related to minimum sample size, the remaining AA ethnicities were combined into an “Other Asian” subgroup, including Japanese, Korean, Vietnamese, etc. [9].
Measures
CAM Use
2012 NHIS adult CAM supplement survey respondents were asked if they had ever used any of the 38 different types of CAMs. For this study, CAM therapies were categorized into four domains: alternative medicine systems (AMS), biologically-based therapies (BBT), mind–body therapies (MBT), and manipulative- and body-based therapies (MBBT). These CAM domains were based on previous studies’ use of these categories [27,28,29]. If a respondent indicated using any type of CAM within a specific domain, his/her response was coded as a “yes” for that domain. If a respondent indicated use of any of the 2012 NHIS’s 38 CAM therapies, they were coded as a “yes” for using that specific CAM.
Health Conditions Treated with CAM
The main dependent variable was CAM use to treat health conditions. Respondents were asked to choose up to three CAM therapies which they considered important. Additional questions were asked regarding these three CAM therapies, including whether they used these CAMs to treat health conditions. The health conditions were categorized into either acute/other or chronic conditions (see Table 1). If a respondent indicated they used any of their top three CAM therapies for one of the health condition categories, their response was coded as a “yes” for that category. We also computed any use of CAM for treatment of health conditions wherein respondents who indicated CAM use to treat any health condition was coded as “yes” for this variable.
Sociodemographic/Predictor Variables
Sex, age, education level, insurance coverage, place of birth, and reported health status were used as sociodemographic and/or predictor variables of CAM use for treatment of health conditions.
Statistical Analyses
Descriptive statistics were estimated for the sociodemographic/predictor variables using weighted percentages and standard errors. Bivariate analyses were performed using Rao and Scott’s adjusted Pearson’s Chi squared tests to determine racial differences in sociodemographic variables, CAM use, and health conditions for which CAM was used for treatment. A multivariable logistic regression model was fitted to examine predictors of CAM use for treatment of health conditions. To further identify specific predictors of CAM use for treatment of health conditions for each AA subgroup, four separate multivariable logistic regression models were fitted. A p value of < 0.05 was considered significant. All analyses were weighted, accounting for the complex NHIS survey design. R version 3.4.3 [30] and survey package [31] were used to analyze the data.
Ethics Review
This study was approved as a non-human subject research by the University of Hawaii Institutional Review Board.
Results
Descriptive Statistics
A total of 2224 AA 2012 NHIS CAM supplement respondents, were included in this analysis, which corresponds to a population estimate of 12,761,839, and is composed of Filipinos (24.04%); Chinese (19.18%); Asian Indian (20.13%), and “Other Asian” (36.65%). Table 2 provides a summary of sociodemographic characteristics of the total AA sample and the four AA subgroups. Significant differences between AA subgroups were found for age, education level, insurance coverage, place of birth, and reported health status.
Table 2 also shows prevalence of CAM use and types of health conditions for which CAM was used for treatment. Approximately 72% of AAs reported CAM use, with no significant differences between AA subgroups. Significant differences were found between AA subgroups in the use of AMS, BBT, and MBBT. Asian Indians reported the highest use of AMS (26.47%, SE = 3.20) and MBT (32.82%, SE = 3.30), while Filipinos reported the lowest use of AMS (6.10%, SE = 1.09) and MBT (12.36%, SE = 1.91). Filipinos reported the highest use of MBBT (26.34%, SE = 2.44), while Asian-Indians (15.88%, SE = 1.80) had the lowest use of MBBT. The same table presents the most frequently reported top three most important CAMs used by the different AA subgroups.
Around 9% of AAs reported using CAM to treat any health condition, with 6.46% of AAs attributing use to chronic conditions (SE = 0.65). Significant differences were found between AA subgroups in their use of CAM to treat any health condition, acute/other conditions, and chronic conditions. “Other Asian” had the highest use of CAM to treat any health condition (12.14%, SE = 1.49), with 8.97% (SE = 1.30) using CAM to treat a chronic health condition. Asian Indians reported the lowest use of CAM to treat chronic conditions (3.60%, SE = 0.94). Chinese had the highest (5.71%, SE = 1.60) reported use of CAM to treat acute/other conditions and Filipinos the lowest (1.68%, SE = 0.58).
Predictors of CAM Use to Treat Any Health Condition
Pooled Data
Table 3 summarizes the logistic regression model of pooled data for AAs’ report of CAM to treat health conditions. “Other Asian” were twice as likely to report CAM use to treat any health condition (OR 2.13, 95% CI [1.25, 3.65]) compared to Filipinos. AAs ≥ 65 years old were almost twice as likely to report CAM use to treat any health condition compared to those who were between 18 and 39 years old (OR 1.88, 95% CI [1.10, 3.18]). AAs reporting some college or an associate degree (OR 1.96, 95% CI [1.16, 3.29]) or a bachelor’s degree or higher (OR 2.49, 95% CI [1.54, 4.00]) were significantly more likely to report CAM use to treat any health condition. Lastly, those reporting very good to excellent health were less likely to use CAM to treat any health condition (OR 0.66, 95% CI [0.45, 0.97]).
AA Subgroups
Table 4 summarizes the logistic regression models within each AA subgroup. Filipinos born outside the U.S. were more likely to report CAM use to treat any health condition (OR 4.62, 95% CI [1.72, 12.37]) than those born in the U.S. Additionally, Filipinos ≥ 65 years of age were less likely to report CAM use to treat any health condition (OR 0.29, 95% CI [0.10, 0.87]). Chinese-Americans reporting very good to excellent health were less likely to use CAM to treat any health condition (OR 0.28, 95% CI [0.12, 0.62]). Chinese who have a bachelor’s degree or higher educational attainment were more likely to report CAM use to treat any health condition was higher (OR 5.58, 95% CI [1.54, 20.18]). Asian Indians ≥ 65 years of age were more than 12 times as likely to report CAM use to treat any health condition (OR 12.68, 95% CI [3.51, 45.79]) compared to those between 18 and 39 years old.
Several sociodemographic variables were found to have significant associations with CAM use for the treatment of any health condition within the “Other Asian” subgroup, including higher odds with: female (OR 2.22, 95% CI [1.22, 4.05]) versus male; 40–64 year olds (OR 1.87, 95% CI [1.08, 3.24]) and ≥ 65 year olds (OR 2.87, 95% CI [1.50, 5.50]) versus 18–39 year olds; those who report some college to associate’s degree (OR 3.49, 95% CI [1.61, 7.59]) and those with bachelor’s degree or higher education (OR 2.8, 95% CI [1.41, 5.55]) versus those reporting a high school diploma or equivalency. “Other Asian” who had health insurance coverage were less likely to report CAM use to treat any health condition than those without (OR 0.45, 95% CI [0.23, 0.87]).
Discussion
This study looked at prevalence, patterns, and predictors of CAM use for treatment of health conditions, specifically among AAs. Our findings show Asian Indians reported the highest use of AMS (26.47%) and MBT (32.82%). Both Ayurveda, a type of AMS, and yoga, an MBT, have origins in India [7, 32], so this was expected. Interestingly, in another nationwide survey of CAM use within a U.S. Asian Indian population, only 2% reported using yoga, but 12.1% used an AMS [33]. “Other Asian” had a similar rate of AMS use as the Chinese subgroup, which may be explained by the use of variations of traditional Chinese medicine, such as acupuncture (a type of AMS) by “Other Asian” ethnicities (e.g., Japanese, Korean, and Vietnamese) [34,35,36].
Chinese had the second highest prevalence of MBT use among the four AA subgroups. Two of the three most common MBTs, tai chi and qigong, originated in China [37, 38]. Among the four AA subgroups, Filipinos had the highest rate of BBT use, including vitamins and herbal therapies, and Chinese reported the lowest. This was surprising, since the 2002 NHIS data showed Chinese having the highest rates of herbal medicine use compared to Filipinos and Asian Indians [4]. Comparison of our findings and the original study show MBT use among AAs remained the same [4].
This study was the first to investigate AAs’ patterns of CAM use for the treatment of health conditions. Only 9% of AAs indicated using CAM for such treatments, which seems low, especially since some Asian-specific CAM therapies (i.e., traditional Chinese medicine, Ayurveda) have been used by many Asian ethnicities to treat different types of illnesses for thousands of years, long before Western medicine was introduced in their countries [5,6,7,8]. Thus questions arise whether AAs, especially first-generation immigrants, underreported their use of CAM for treatment or if they abandon cultural healing practices to use Western medicine.
Around 6% of AAs used CAM to treat chronic conditions (e.g., pain, diabetes, arthritis, and cardiovascular diseases). Previous NHIS studies provided evidence that respondents reporting at least one chronic disease were more likely to use CAM [12, 39]. However, this association did not imply that the CAM they used was for the treatment of their chronic diseases. A potential explanation for AAs’ CAM use for treatment of chronic diseases could be so they could take responsibility for their health and improve their quality of life despite presence of disease [40]. It is not clear, however, how one’s culture influences their decision to use CAM for treatment, especially if AAs used Asian-specific CAM therapies.
“Other Asian” had the highest use of CAM for treatment of any health condition. Some ethnicities under this subgroup, such as Vietnamese, Hmong, Laotians, and Cambodians, may be more vulnerable to poor healthcare access due to high poverty rates, language barriers, health illiteracy, and immigrant status [41,42,43]. Better access to Western medicine may reduce their need to use CAM to treat illnesses as “Other Asian” with health insurance were less likely to report CAM use for treatment. Cultural perceptions of illness, which focus on holistic healing, may also motivate “Other Asian” to use CAM in the treatment of illness [23].
“Other Asian” women may have unique barriers to healthcare utilization, causing them to turn to CAM for treatment of health conditions. Previous studies have shown some “Other Asian” women prefer their physicians to be female, especially for ‘intimate’ health issues. Some only visited physicians with pregnancy [42, 44].
Middle-aged and elderly “Other Asian” were more likely to report CAM use for treatment. These age groups capture the Southeast Asian refugee population who continued to use traditional medicine once living in and exposed to U.S. healthcare system [43, 45, 46]. Also, a previous study showed Japanese-American middle-aged and elderly populations in California were more likely to use CAM [1].
Other considerations regarding CAM use were found among Asian Indians, Filipinos, and Chinese. Elderly Asian Indians had higher odds of reporting CAM use for treatment, while the Filipino elderly were less likely to do so. Some studies suggest that older Asian Indians use yoga as a daily routine and cultural practice and Asian Indians < 35 years of age view yoga as a way to keep fit physically and mentally [47, 48]. A possible reason Filipino reported less CAM use for treatment may be related to higher compliance with advice and treatment regimens provided by their physicians, whom they view as experts [49, 50].
Also, foreign-born Filipinos were more than four times as likely to use CAM as U.S.-born Filipinos. First-generation immigrants may still hold more traditional and holistic views on health and illness, like CAM, while U.S.-born Filipinos may have always relied more heavily on Western medicine. Lastly, Chinese with higher education levels were more likely to use CAM for treatment. This preference is not well understood, but one possible explanation is that higher education leads to employment, higher income, and the ability to afford the mostly out-of-pocket expense of CAM treatments [51].
Limitations
There are several limitations to our study. First, not all states participated in the 2012 NHIS [9]. It was unclear exactly where (i.e., which state/U.S. region) AA respondents were surveyed. Nevertheless, our findings may not be pertinent to those AAs living in states which did not participate in the NHIS. Second, the NHIS is a cross-sectional survey and findings are only applicable to a specific time. Thus, future studies should focus on trend analysis of CAM use for treatment among AA populations. Third, the NHIS only collected data from non-institutionalized populations, meaning persons who were hospitalized or institutionalized were not in the sample. Therefore, the sample may be biased towards healthier and younger populations [12]. Lastly, our study only looked at CAM use for treatment as a type of medical pluralism. The 2012 NHIS does not provide data to analyze whether respondents CAM use preceded, succeeded, or were concurrently combined with Western medicine. Patterns of combination use of CAM and Western medicine should be explored in future studies.
Conclusion and Recommendations for Future Studies
This study provides insight into AAs’ use of CAM for treatment and gaps in knowledge of potential medical pluralism among AAs. Our findings suggest only 9% of AAs use CAM for treatment, possibly as a type of medical pluralism. Due to low prevalence, questions arise as to whether AAs’ CAM use for treatment was underreported. Our findings also show AAs use CAM more for treatment of chronic illnesses than acute/other conditions. This may be a means to take responsibility for their health or other cultural influences may be involved. Lastly, sociodemographic characteristics had an impact on AA subgroups’ use of CAM for treatment, yet some predictors to CAM use for treatment are still not fully understood.
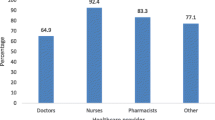
Healthcare personnel should screen for simultaneous or preferential CAM use among their AA patients to improve understanding of cultural preferences, address potential healthcare access issues, and develop health education on potential health risks due to interaction between CAM and Western medicine. Healthcare personnel should be educated on Asian-specific CAM therapies to evaluate how these can be safely integrated with Western health approaches.
Further research on medical pluralism among AAs and in the general population is needed. A nationwide AA CAM use survey may be helpful in bridging current gaps in knowledge, such as underreporting of CAM use, the schedule of CAM use for treatment purposes (e.g., subsequent or simultaneous use), whether cultural influences impact decisions to use CAM for treatment, and how CAM use for treatment impacts health. Furthermore, a broader comparison of CAM use for treatment among different races/ethnicities in the U.S. is warranted to fully comprehend medical pluralism.
References
Hsiao AF, et al. Complementary and alternative medicine use among Asian-American subgroups: prevalence, predictors, and lack of relationship to acculturation and access to conventional health care. J Altern Complement Med. 2006;12:1003–10.
Keith VM, et al. Assessing the effects of race and ethnicity on use of complementary and alternative therapies in the USA. Ethn Health. 2005;10:19–32.
Mackenzie ER, et al. Ethnic minority use of complementary and alternative medicine (CAM): a national probability survey of CAM utilizers. Altern Ther Health Med. 2003;9:50–7.
Mehta DH, et al. Use of complementary and alternative therapies by Asian Americans. Results from the National Health Interview Survey. J Gen Intern Med. 2007;22:762–7. https://doi.org/10.1007/s11606-007-0166-8.
Lu A, et al. An integrative approach of linking traditional Chinese medicine pattern classification and biomedicine diagnosis. J Ethnopharmacol. 2012;141:549–56.
Mukherjee PK, et al. Development of Ayurveda—tradition to trend. J Ethnopharmacol. 2017;197:10–24.
Mukherjee PK, et al. Changing scenario for promotion and development of Ayurveda—way forward. J Ethnopharmacol. 2012;143:424–34.
Xue CCL, et al. Traditional Chinese medicine: an update on clinical evidence. J Altern Complement Med. 2010;16:301–12.
National Health Interview Survey (NHIS) public use data release: NHIS survey description. National Center for Health Statistics. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2012/srvydesc.pdf. Accessed 15 Apr 2018.
Bromfield SG, McGwin G Jr. Use of complementary and alternative medicine for eye-related diseases and conditions. Curr Eye Res. 2013;38:1283–7.
Dossett ML, et al. Complementary and alternative medicine use by US adults with gastrointestinal conditions: results from the 2012 National Health Interview Survey. Am J Gastroenterol. 2014;109:1705–11.
Falci L, Shi Z, Greenlee H. Multiple chronic conditions and use of complementary and alternative medicine among US adults: results from the 2012 National Health Interview Survey. Prev Chronic Dis. 2016. https://doi.org/10.5888/pcd13.150501.
Garrow D, Egede LE. National patterns and correlates of complementary and alternative medicine use in adults with diabetes. J Altern Complement Med. 2006;12:895–902.
Hoerster KD, et al. Use of conventional care and complementary/alternative medicine among US adults with arthritis. Prev Med. 2012;54(1):13–7.
Nahin RL, et al. Disease severity is associated with the use of complementary medicine to treat or manage type-2 diabetes: data from the 2002 and 2007 National Health Interview Survey. BMC Complement Altern Med. 2012;12:193. https://doi.org/10.1186/1472-6882-12-193.
Upchurch DM, Rainisch BW. The importance of wellness among users of complementary and alternative medicine: findings from the 2007 National Health Interview Survey. BMC Complement Altern Med. 2015;15(1):362.
Ghildayal N, et al. Complementary and alternative medicine use in the US adult low back pain population. Glob Adv Health Med. 2016;5(1):69–78.
Bertisch SM, et al. Use of relaxation techniques and complementary and alternative medicine by American adults with insomnia symptoms: results from a national survey. J Clin Sleep Med. 2012;8:681–91.
Griffith LG. Medical pluralism: what health behaviors do people have and why does it matter? University of Birmingham Institute of Research into Superdiversity. https://www.birmingham.ac.uk/Documents/college-social-sciences/social-policy/iris/2015/presentations/medical-pluralism-LG.pdf. Accessed 2 May 2018.
Nissen N, Manderson L. Researching alternative and complementary therapies: mapping the field. Med Anthropol. 2013;32:1–7.
Kaptchuk TJ, Eisenberg DM. Varieties of healing. 1: medical pluralism in the United States. Ann Intern Med. 2001;135(3):189–95.
Lupton D. Medicine as culture: illness, disease and the body. 3rd ed. Thousand Oaks: Sage; 2012.
Wade C, et al. Medical pluralism of Chinese women living in the United States. J Immigr Minor Health. 2007;9:255–67.
Wade C, et al. Medical pluralism among American women: results of a national survey. J Women’s Health. 2008;17(5):829–40.
Arcury TA, et al. Use of complementary therapies for health promotion among older adults. J Appl Gerontol. 2015;34:552–72.
Sivén J, Mishtal J. Yoga as entrée to complementary and alternative medicine and medically pluralistic practices. Hum Organ. 2012;2012(71):348–57.
Barnes PM, et al. Complementary and alternative medicine use among adults: United States, 2002. Semin Integr Med. 2004;2(2):54–71.
Brown CM, et al. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13(7):751–8.
Elewonibi BR, BeLue R. Prevalence of complementary and alternative medicine in immigrants. J Immigr Minor Health. 2016;18(3):600–7.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2008. http://www.R-project.org.
Lumley T. Survey: analysis of complex survey samples. R package version 3.32, 2017.
Field T. Yoga clinical research review. Complement Ther Clin Pract. 2011;17:1–8.
Misra R, et al. Complementary and alternative medicine use among Asian Indians in the United States: a national study. J Altern Complement Med. 2010;16:843–52.
Yu F, et al. Traditional Chinese medicine and Kampo: a review from the distant past for the future. J Int Med Res. 2006;34(3):231–9.
Cha WS, et al. Historical difference between traditional Korean medicine and traditional Chinese medicine. Neurol Res. 2007;29(sup1):5–9.
Bodeker G, Ong CK. WHO global atlas of traditional, complementary and alternative medicine. Geneva: World Health Organization; 2005.
Li JX, et al. Tai chi: physiological characteristics and beneficial effects on health. Br J Sports Med. 2001;35(3):148–56.
Xu J. Body, discourse, and the cultural politics of contemporary Chinese Qigong. J Asian Stud. 1999;58(4):961–91.
Mongiovi J, et al. Complementary and alternative medicine use and absenteeism among individuals with chronic disease. BMC Complement Altern Med. 2016. https://doi.org/10.1186/s12906-016-1195-9.
Thorne S, et al. Complementary/alternative medicine in chronic illness as informed self-care decision making. Int J Nurs Stud. 2002;39:671–83.
Kim W, Keefe R. Barriers to healthcare among Asian Americans. Soc Work Public Health. 2010;25:286–95.
Lee S. Barriers to health care access in 13 Asian American communities. Am J Health Behav. 2010. https://doi.org/10.5993/AJHB.34.1.3.
MacDuff S, et al. The use of complementary and alternative medicine among refugees: a systematic review. J Immigr Minor Health. 2011;13:585–99.
Jackson JC, et al. Development of a cervical cancer control intervention program for Cambodian American women. J Commun Health. 2000;25(5):359–75.
Buchwald D, et al. Use of traditional health practices by Southeast Asian refugees in a primary care clinic. West J Med. 1992;156(5):507.
Bengiamin M, et al. Understanding traditional Hmong health and prenatal care beliefs, practices, utilization, and needs. http://health-equity.lib.umd.edu/3854/1/HmongReportWEB.pdf. Accessed 8 June 2018.
Büssing A, et al. Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Altern Med. 2012. https://doi.org/10.1155/2012/165410.
Kalavar JM, Van Willigen J. Older Asian Indians resettled in America: narratives about households, culture, and generation. J Cross-Cult Gerontol. 2005;20:213–30.
De Guzman AB, et al. Developing a model of medication adherence among Filipino elderly. Educ Gerontol. 2013;39(5):298–313.
McLaughlin LA, Braun KL. Asian and Pacific Islander cultural values: considerations for health care decision making. Health Soc Work. 1998;23:116–26.
Nahin RL, et al. Costs of complementary and alternative medicine (CAM) and frequency of visit to CAM practitioners, United States, 2007. Center for Disease Control and Prevention. https://stacks.cdc.gov/view/cdc/11548 (2009). Accessed 8 June 2018.
Funding
This work was partially supported by the National Institutes of Health (NIH) under Grants U54MD007584 and U54MD007601. The content is solely the responsibility of the authors and does not necessarily represent official views of NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest was reported by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Felicilda-Reynaldo, R.F.D., Choi, S.Y., Driscoll, S.D. et al. A National Survey of Complementary and Alternative Medicine Use for Treatment Among Asian-Americans. J Immigrant Minority Health 22, 762–770 (2020). https://doi.org/10.1007/s10903-019-00936-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-019-00936-z