Abstract
Caregivers of children with autism spectrum disorder (ASD) may find it difficult to feel a sense of control and to cope with the overall physical and emotional demands of caring for their child. While caregivers are able to successfully cope with a high level of stress, there are limits to their resources and abilities to cope over time. Genetic counselors working with affected families may be able to help parents more effectively manage stress related to the disorder. Few short-term interventions have been reported in genetic counseling yet implementation of evidence-based examples may be achievable. This study aimed to assess the feasibility of a coping effectiveness training (CET) intervention designed to enhance coping self-efficacy (CSE) among caregivers of children with ASD, with the eventual goal of translating this intervention into genetic counseling practice. A randomized treatment-control design was used to investigate the feasibility of an intervention using CET among caregivers of children with ASD. The primary outcome was the feasibility of the intervention; the secondary outcome was improvements in CSE in the intervention group as compared to the control group. Caregivers were recruited and randomized into the treatment (n=15) or control (n=13) groups. Of these, 22 completed the study (retention: 78.6%). The intervention was highly feasible; most caregivers found the CET helpful, practical, useful, and relatively easy to attend. The treatment group demonstrated significantly increased CSE from pre-intervention to post-intervention (p=0.02). Between group differences were not significant when comparing the pre-post changes. We provide preliminary evidence that CET may be beneficial to caregivers of children with ASD. The results of this feasibility study support development of a phase II study of this intervention in a larger cohort, aimed to be implemented into a genetic counseling setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is part of a broadly classified group of conditions referred to as neurodevelopmental disorders. Children with ASD experience deficits in social interactions and communication as well as behavioral challenges. The prevalence of children with ASD in the U.S. has increased from 1 in 150 in 2000, to 1 in 68 in 2012 (Center of Disease Control and Prevention 2016; Christensen 2016). As such, the number of caregivers of children with ASD has also increased.
Caregivers of children with ASD experience higher levels of psychological stress, psychiatric problems, and poorer overall health than caregivers of children with other disabilities and of neurotypical children (Hayes and Watson 2013; Miodrag and Hodapp 2010; Zablotsky et al. 2013). A variety of factors have been suggested to produce these higher stress levels including the diagnostic process (Crane et al. 2015), the challenging behaviors of children with ASD, and the variable prognoses (Hayes and Watson 2013). Of further concern, parental stress has been shown to reduce the effectiveness of interventions for children with ASD such as early teaching (Osborne et al. 2008).
In response to stress, individuals generally engage in a variety of coping strategies (Chesney et al. 2006; Lazarus and Folkman 1984). The cognitive theory of stress and coping describes two types of coping: problem- and emotion-focused (Lazarus and Folkman 1984). Problem-focused coping is an effort directed at changing stressful situations. Emotion-focused coping is the process of managing emotional responses to stressful situations. Appraisals and the choice of coping strategies may lead to adaptation, which has been defined by some researchers as “both the process of coming to terms with the implications of the condition and the observable outcomes of that process” (Biesecker and Erby 2008). Prior research suggests that caregivers of children with disorders across the ASD spectrum often find it difficult to cope with the overall emotional demands of caring for their child (Lee 2009; Phelps et al. 2009), and may be more likely to engage in emotion-focused coping strategies compared to parents of typically developing children (Lai et al. 2015).
Guidelines from the American College of Medical Genetics (ACMG) recommend all individuals/families with ASDs be referred for a clinical genetics evaluation, which is often facilitated within a few years of a child’s diagnosis (Schaefer et al. 2013). It is widely accepted that ASDs have a multifactorial etiology, influenced by various genetic and environmental factors. At least 15% of cases have an identifiable genetic condition, most commonly due to a single gene disorder or copy number variation. There are over 100 known genetic disorders that have features of ASD (for example Rett syndrome and Fragile X syndrome) (Betancur 2011; Carter and Scherer 2013).
The role of a genetic counselor in this process has traditionally been to obtain and interpret family and medical histories to provide an accurate risk assessment as well as to provide education regarding inheritance, genetic testing options, management, resources, and research. Moreover, genetic counselors are trained to help people not only understand but also “adapt to the medical, psychological and familial implications of genetic contributions to disease,” which involves helping these families to cope effectively with their child’s diagnosis (Resta et al. 2006). As such, the process of genetic counseling lends itself to psychosocial interventions that seek to enhance adaptation among parents of children with ASD by improving their coping efficacy.
Traditionally, intervention studies involving caregivers of children with ASD focused on strengthening parenting skills and facilitating better outcomes for the child with ASD (McConachie and Diggle 2007; Rogers and Vismara 2008). More recently, focus has broadened to include developing interventions that reduce parental stress. However, these interventions are often lengthy and/or group administered, such as 10 weekly sessions, which can be problematic for caregivers of children with ASD who often have busy schedules (Hastings and Beck 2004). Addionally, lengthy interventions would not be practical to implement within a pediatric genetics setting, where there are often time constraints (Schaefer et al. 2013). One previous intervention study found an association between increased coping abilities in parents of children with ASD and a reduction in clinically significant parenting stress (Feinberg et al. 2014). Though of note, this study did not include an active control condition to account for non-specific effects of contact with a healthcare provider. In a different but related context, a review of eleven studies involving parents of children with cancer identified improvements in parental mental health outcomes as a result of coping interventions (Peek and Melnyk 2010). These prior studies provide a rationale for further exploration of enhancing coping skills as an effective intervention among parents of children with ASD.
Coping effectiveness training (CET), based on the aforementioned cognitive theory of stress and coping, has been effective at enhancing coping efficacy. CET utilizes problem-focused coping strategies such as problem-solving and negotiation and emotion-focused coping strategies such as stress-reduction techniques (Chesney et al. 2003; Chesney and Folkman 1994; Chesney et al. 1996). CET consists of two phases: training and maintenance (Chesney and Folkman 1994). Participants receive training regarding appraisal of the controllability of stressful situations, problem- and emotion-focused coping, their fit with stressful situations and examples of coping strategies. CET has been effective in populations such as in men living with HIV (Chesney et al. 2003) and individuals with spinal cord injuries (Kennedy et al. 2003), though it has not been studied in parents of children with developmental challenges, including caregivers of children with ASD.
To measure the effectiveness of CET, the coping self-efficacy (CSE) scale has been used to measure coping self-efficacy as a primary outcome in prior CET intervention studies (Chesney et al. 2003; Chesney et al. 2006). Coping self-efficacy describes the confidence in one’s ability to choose effective coping strategies. Coping self-efficacy can be enhanced by helping caregivers make more deliberate choices about their coping strategies, as CET aims to do. While there has been a growing interest in recent years in developing interventions targeted at factors involved in the adaptation process, there has been limited research examining interventions targeting variables that theoretically affect adaptation, such as CSE.
This study aimed to examine whether a modified, individualized version of the CET intervention was feasible to implement among caregivers of children with ASD with the intention of downstream clinical use such as a genetic counseling session. We further aimed to measure changes in CSE in intervention participants as compared to controls, recognizing the limitations of a small sample size.
Methods
Recruitment and Sample
Participants were recruited from the greater Baltimore, Maryland area in the US. Flyers were displayed at four clinics within the Kennedy Krieger Institute (an institute for children and adolescents with neurodevelopmental disorders). Autism support groups distributed flyers and emails to members. One investigator (CH) conducted in-person recruitment at support group meetings and waiting areas of clinics. Through in-person recruitment at four clinics and support group meetings, potential participants were provided with study information, a consent form and the pre-intervention questionnaire. For those who did not have access to the paper version, they were asked to contact CH by phone or email and a paper survey was then mailed to the participant.
Eligibility criteria were: (a) primary caregiver of a child with ASD (established by caregiver report); (b) at least 18 years of age; (c) child has no known syndromic disorder that included co-morbid features that could influence parental responses (including but not limited to Rett Syndrome, Tuberous Sclerosis Complex, Fragile X Syndrome, Neurofibromatosis, Prader-Willi Syndrome and Angelman Syndrome); and (d) able to read, write and speak English. Children with genetic diagnoses were not included to generate a more homogeneous sample. Only caregivers whose children lived with them were eligible, and only one caregiver per household was included in the study. Recruitment began early July of 2010 and continued for 12 weeks.
Study Design
Genetic Counselor Training
The genetic counselor (CHS) underwent training in perceptions of controllability, emotion and problem-focused coping strategies and implementation of the CET (Kennedy et al. 2003; McInerney-Leo et al. 2004). Based on the training, a brief didactic presentation and three interactive worksheets were developed to guide the intervention. Six members of the study team reviewed the materials for the intervention and minor revisions were made accordingly. The genetic counselor role-played administering the intervention with a number of scenarios that could arise with participants and developed standardized responses. The genetic counselor rehearsed the final intervention with the principal investigator (BBB) to ensure fidelity. All sessions were audio-recorded and transcribed.
Design and Randomization
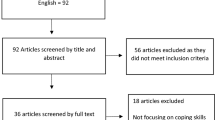
This study used a treatment-control pilot design. The control sample was included to allow assessment of preliminary intervention effects. Following completion of a pre-intervention questionnaire, caregivers were randomized to either control or treatment group (Fig. 1). Participants received two individualized sessions, delivered one-on-one between the genetic counselor and the caregiver. The first session was 90 min and the second was 60 min, held one month apart. Post-intervention questionnaires were completed approximately one month after the second session. Non-responders received a reminder email or phone call. Participants who completed all study aspects received a $50 gift certificate to a department store.
Randomization was performed using a stratified randomized block design with block sizes of four. Participants were stratified by the caregiver’s perception of severity of the child’s condition. Prior research shows that severity impacts caregiver stress with higher levels of stress seen among parents of children with more severe disability, in particular, more problematic behavior (McStay et al. 2013; Plant and Sanders 2007). In the pre-intervention questionnaire, caregivers indicated seriousness of their child’s condition compared to other children with ASD on a 9 point Likert scale (1 = less severe and 9 = more severe with responses 1–5 categorized as “not severely affected” and 6–9 categorized as “severely affected”). In the treatment group six (40%) children were severely affected, in the control group, four children were severely affected (31%), differences across groups were not statistically significant p = 0.3.
Participants were also stratified by recruitment source in an attempt to obtain equal balance in demographic variables between treatment and control groups. Participants were told that they would be randomized before consenting to be in the study, providing them an opportunity to opt out if they were not willing to be randomized.
Intervention
Treatment Condition
We developed an intervention for this study based on CET interventions developed for use with HIV positive men (Chesney et al. 2003; Chesney et al. 1996). We also drew from a brief cognitive-behavioral intervention used in the genetic counseling setting, which was effective at enhancing psychological well-being in families with hereditary breast and ovarian cancer (McInerney-Leo et al. 2004), as the ultimate goal of our intervention was incorporation into a clinical setting such as a genetic counseling session. Margaret A. Chesney, PhD, who pioneered the CET intervention, gave permission for us to use the intervention and CSE scale. Following development, the intervention was piloted with four parents of children with ASD.
In the first session, participants engaged in a 30-min discussion about aspects of their child’s condition they feel they can and cannot control. The latter 60 min consisted of a psychoeducational discussion about stress, appraisals, coping, and the match between appraisals and coping. Participants were guided through three worksheets (supporting information: file A1) to direct their thinking about how they appraise and cope with stressful situations. Specifically, the interventionist (CH) helped participants match problem-solving strategies to stressors appraised as controllable and emotion-focused coping strategies to stressors appraised as uncontrollable. At the end of the session, participants were given a homework assignment to complete the same three worksheets in relation to stressors that arose before the second session.
During the second session, participants discussed stressful situations that arose during the time since the first session with the interventionist. The psychoeducational discussion was revisited, alongside the worksheets and the homework assignment as they applied to the shared examples.
Control Condition
The control sessions were administered by the same interventionist as in the intervention arm (CH). During both sessions in the control arm, participants were asked to share information about their child’s diagnosis and care, similar to a client-centered discussion that might be facilitated during a traditional genetic counseling session. In the first session, participants were asked to discuss their child’s current resources, stressful aspects of their child’s condition, and hopes for their child. They were asked to think about these hopes between the first and second sessions. During the second session, participants were asked to discuss events that occurred since the first session related to their child’s condition and any stressors related to these events. The interventionist actively listened and reflected back to the clients’ what they chose to share. Sessions were guided by client issues devoid of components of the CET intervention including the worksheets. The control condition was standardized by administration of the same questions to each control participant. In addition, the interventionist used a similar client-centered technique with each participant.
Measures
Pre-Intervention Questionnaire
Participant characteristics measured included caregiver’s relationship to child, number of children, number of children with ASD, age of the child, child’s diagnosis, age at child’s diagnosis, age at child’s first symptom, child’s gender, marital status, level of education, income, racial/ethnic background, and age.
The coping self-efficacy (CSE) scale was used to assess caregivers’ perceived self-efficacy for coping with challenges and threats (Chesney et al. 2006). This scale was designed for use in the original CET intervention from which our intervention was based. The CSE scale has been reported to have good concurrent and predictive validity with measures of psychological distress and well-being, ways of coping, and social support (Chesney et al. 2006). Cronbach alpha scores for the pre- and post-survey were 0.94 and 0.97 respectively. Participants were asked to rate the extent to which they believed they can perform various tasks important to adaptive coping on an 11-point scale where 0 represents ‘cannot do at all’ and 11 is ‘certain can do’. Ratings were summed for an overall score with higher scores indicating greater CSE. An example item is: “when things aren’t going well for you, or when you’re having problems, how confident or certain are you that you can do the following…Break an upsetting problem down into smaller parts?” CSE measures were administered to both groups in a post-intervention questionnaire.
Post-Intervention Questionnaire and Feasibility Assessment
The treatment group was asked specific questions about the sessions/worksheets to assess the feasibility of the CET intervention. This was done through open- and closed-ended questions. Closed-ended questions assessed the extent to which the in-person sessions met participant expectations and needs, the usefulness of the worksheets, how often the participant had used the coping strategies in the time since the intervention, whether they would return to the program, and whether they would recommend the program to a friend. Results from the quantitative feasibility assessments were ranked using a 7-point scale (1 = low; 7 = high). To help interpret quantitative feasibility data, open-ended questions explored what participants found helpful and what improvements were needed.
Additional parameters to assess feasibility included: number of eligible caregivers; exploration of recruitment approaches; ease of delivery and acceptability of the intervention; follow-up, questionnaire response and adherence rates; time needed to collect and analyze data.
Sample Size Estimation
As a feasibility study, we were not powered to detect differences. Using prior measures of CSE we calculated that to detect a small effect in CSE after the intervention with 80% power, an alpha level set at 0.05, and a correlation of 0.2 between the pre- and post-survey, the minimum sample size needed was 194 participants. The effect size was chosen because effect sizes for changes in coping as a result of psychosocial interventions range from 0.2 to 0.8 (Chesney et al. 2006). Thus, an effect of 0.2 or greater is a statistically meaningful effect size. This sample size estimation applies to future studies of the CSE.
Data Analysis
Primary outcome measures (feasibility data) were analyzed using descriptive statistics and content analysis. Secondary outcome variables were analyzed using signed-rank tests and rank-sum tests. Nonparametric tests were used to compare data from the treatment and control groups due to the small sample size and discreteness of the data. Wilcoxon-sign-rank and Wilcoxon-Mann-Whitney tests were used to test whether CSE had changed over time, and examine differences between pre- and post-intervention measurements between treatment and control groups, respectively. Fisher’s exact tests were used to assess whether withdrawals differed from non-withdrawals.
Data were analyzed using PASW Statistics 18.0 (SPSS Inc., Hong Kong).
This study was approved by the National Human Genome Research Institute IRB.
Results
Response Rate and Retention
Thirty participants completed the pre-intervention questionnaire. Two were ineligible. Of the 28 randomized caregivers (15 treatment, 13 control), 24 completed the first session and 22 completed the second session. All 22 individuals completed the final questionnaire and were included in the final analysis (78.6% retention). (Figure 1)
Attrition rates did not vary between groups: three treatment and three control participants withdrew. Comparing those who withdrew to those who remained in the study, a greater percentage of those who withdrew had less than a college education (83%, n = 5 vs. 32%, n = 7; p = 0.04). Those who withdrew had more children than those who did not withdraw (mean 2.8 vs. 2.2 p = 0.01).
Participant Characteristics
Mean age of caregivers was 38.2 years (SD: 7.4) and ranged from 24 to 54. Children’s mean age was 5.4 years (SD: 2.4). On average, children were diagnosed with ASD at 3.03 years (SD: 1.5). Participants were predominantly biological mothers (81.8%), married (63.6%), Caucasian (68.2%), and had a post-graduate education (45.5%). Most had an annual household income over $70,000 (50%). The majority of caregivers had only one affected child (90.1%). Most of the children in this sample were male (68.2%) and diagnosed with either autism (77.3%) or PDD-not otherwise specified (PDD-NOS; 18.2%). Most (61.9%) were recruited from the Kennedy Krieger Institute.
Annual household income was the only demographic variable that was significantly different between treatment and control groups with more individuals in the treatment group reporting a household income above $70,000. (Table 1)
Intervention Feasibility
Data were collected and analyzed over a six-month period.
Variables relating to participants’ assessment of the CET indicated that the intervention met participants’ expectations (mean, 5.75; SD, 1.22) and needs (mean, 6.08; SD, 1.31). Participants noted that the intervention helped them to learn new information (mean, 6.08; SD, 1.08), identify controllable aspects of their child’s condition (mean, 6.00; SD, 1.35), and think of new ways to manage stressful situations (mean, 5.92; SD, 1.00). (Table 2)
Participants found the intervention practical and useful: the intervention influenced how participants felt in stressful situations (mean, 4.83; SD, 1.64) and helped them to feel more control (mean, 4.67; SD, 1.83). Participants reported a range of responses about the ability the worksheets helped them to manage stress more effectively (mean, 3.5; SD, 2.02; modes of 1, 4, and 6). Participants also indicated that on average, they would be relatively likely to attend a similar intervention again (mean, 5.33; SD, 1.92) and would recommend the intervention to a friend (mean, 5.75; SD, 1.91). (Table 2)
Most treatment participants (66.7%, n = 8) indicated they had thought about the intervention worksheets and used them in a situation at least ‘a few times’. The same number of participants stated they had reviewed the worksheets ‘a few times’. Many of the caregivers also indicated they used the coping strategies either ‘sometimes’ (33.3%, n = 4) or ‘regularly’ (41.7%, n = 5). (Table 2)
Caregivers in the treatment group provided open responses about their experiences with the intervention. Most responses were short and readily interpreted literally. They described helpful aspects of the intervention including a discussion of stressful issues, being able to gain new perspectives and problem solving. For example, one caregiver stated, “[the intervention sessions were helpful in] making me see things through a difference perspective, such as things I can or cannot change or have no control over”. Caregivers also noted the intervention sessions helped them recognize the importance of self-care: “that I need to become less stressed and take care of myself and not just my children”.
Most participants noted no unhelpful aspects of the intervention, but the few who did mentioned the limitation of the practicality of applying coping strategies in everyday situations, with some noting they already had effective coping mechanisms: “[I] already had good coping strategies, discussing this wasn’t as helpful.”
Participants offered suggestions of ways the intervention could be improved including additional follow-up meetings and more convenient meeting locations. Of the six participants who withdrew, data were available from three, all of who gave scheduling difficulties as the primary reason for withdrawal: “[I] have four kids; two in football and one autistic. [I was] unable to arrange childcare and scheduling in order to get to discussion.”
Coping Self-Efficacy (CSE)
Caregivers’ CSE was measured using the CSE scale. There were no statistically significant differences in the means and medians of CSE between the groups at pre-intervention (all p > 0.79).
In the post-intervention analysis, there were statistically significant increases in CSE from pre-test to post-test in in the treatment group (p = 0.02), but not in the control group (p = 0.17). On average, the total scores on the CSE scale in the treatment group increased by 34.6 points (p = 0.02). However, in examining the between-group differences in CSE, there was not a statistically significant difference (all p > 0.41). (Table 3)
Discussion
The findings of our study suggest that CET may be feasible for a genetic counselor to implement among caregivers of children with ASD, providing a rationale for investigation of this intervention using a larger phase II study design. The observed improvement in CSE as a result of our intervention adds further justification, though it is important to note that treatment effects were not statistically significant.
In recent years, the use of problem-solving and other coping strategies in parents of children with ASD has emerged, evidenced by two prior reports of these techniques developed for use in this population (Feinberg et al. 2014; Nguyen et al. 2016). Unique to these two prior studies, our study used CET with the addition of emotion-focused coping training, matching appraisals to coping approach. Development of an intervention should draw on these two previous studies in addition to our intervention. A benefit of our study, omitted from the two previous problem-solving intervention studies, was the control condition that received the same number and length of sessions as the intervention group. This was an effort to control for confounding effects, such as the potential for a lengthy individual session with a caring health care provider to influence outcome measures. A further advantage of our intervention is the brief, individualized nature which enables downstream translation to a clinical genetic counseling setting.
The feasibility of our trial is evidenced by results that most caregivers in the treatment group reported positive experiences with the CET; reporting that it was helpful, practical, useful, and relatively easy to attend. Importantly, participants benefited from problem-solving techniques in the intervention (i.e. talking through stressful situations, breaking down stressors into manageable parts, and coming up with specific solutions). These concrete, structured, and goal-directed conversations may have helped caregivers to better cope with their child’s condition.
Prior research has shown that among caregivers of children with ASD, problem-focused coping was associated with increased levels of adaptation more so than emotion-focused coping (Lewis 2008; Smith et al. 2008). This may be explained by including caregivers of younger children with more recent diagnoses, which was the case in our study. Previous research has found that parents of children with ASD shift away from problem-focused toward emotion-focused coping over time (Gray 2006). This may be because shortly after diagnoses, there are many active tasks caregivers can perform such as seeking out therapies or providers, whereas these active tasks reduce with time, in part due to the scarcity of resources available for older children and adults (Gray 2006).
A subset of our caregivers found the emotion-focused strategies useful. These caregivers reported that the intervention helped them recognize the importance of self-care, an emotion-focused technique that may be useful in managing uncontrollable aspects of situations, such as a child’s long-term course (Lazarus and Folkman 1984; Lewis 2008). Many participants indicated that they had little time for themselves amidst their daily caregiving responsibilities.
Retention rates of our study were relatively high, potentially due to the individualized short-term nature of the intervention. In contrast, one study implemented a group psychosocial intervention in women with metastatic breast cancer, and found the group aspect had a significant negative effect on feasibility (Goodwin et al. 2000): a large proportion of participants were lost due to scheduling difficulties and the study’s inability to maintain adequately-sized groups, which prolonged the recruitment timeframe. Similarly, Chesney et al. (2003) reported that higher levels of participation may have been maintained in their trial using CET in HIV patients if their intervention was delivered individually, instead of in a group (Chesney et al. 2003).
The study described here recruited a modest number of individuals (N = 28) over a 12-week period. A larger study of this intervention should consider an enhanced recruitment process. Recruitment through local schools could be considered in future studies. The difficulty of recruiting parents of children with autism for randomized trials was shown in a previous study investigating problem-solving education for mothers of children with autism. The investigators recruited for a period considerably longer than our study, close to three years; however, their final cohort consisted of a mere 122 mothers (Feinberg et al. 2014). Many of the participants in our study had scheduling difficulties and this, not surprisingly, was the most cited reason for withdrawal. Future studies could consider resources for respite care, as was suggested by caregivers in our study.
We observed an increase in CSE in the treatment group at post-intervention, though not significantly different from the change observed in the control group. This finding is consistent with published results from the study of CET in men with HIV (Chesney et al. 2003) and offers some evidence that CET may influence CSE. There is prior evidence that the effects of CET persist after 12 months (Chesney et al. 2003). This also suggests that those in the treatment group felt more confidence in their ability to cope with the stressful nature of caring for their child, which may result in less adverse psychological outcomes (Lazarus and Folkman 1984). If caregivers are given new resources to choose more effective coping strategies, they may be able to better adapt to their child’s condition over time.
Practice Implications
When referred to a pediatric genetics clinic, families typically meet with a clinical geneticist who performs the diagnostic evaluation and may recommend more specific genetic testing to identify a specific underlying etiology. The role of the genetic counselor in this process is to assist parents and families with decision-making regarding genetic testing options, understand the implications of possible results, anticipate the risks to other family members, and ultimately to help them to cope with and adapt to the condition affecting their child. Efforts to enhance coping may be done during the initial visit, during telephone conversations, and subsequent visits to review genetic test results, and additional genetic testing options, such as exome sequencing (Schaefer et al. 2013). This brief, individualized intervention uniquely lends itself to be incorporated into these genetic counseling sessions, which in turn would provide opportunities for expanded roles for genetic counselors (Baty et al. 2016). Previous randomized control trials using interventions have been successfully carried out in the context of cancer genetic counseling (Athens et al. 2017). For example, Eijzenga et al. observed significantly lower levels of cancer worry and distress after administering an intervention that used a questionnaire to facilitate communication about psychological problems during a genetic counseling session (Eijzenga et al. 2014). Beyond the genetic counselling context, the intervention we have designed may be deployed by a range of healthcare providers. As the intervention involves extended visits, it would be optimally used by healthcare providers able to provide extended visits, for example social workers, behavioral healthcare providers, psychologists and psychiatrists.
Study Limitations
This study had limitations. Although there was some variation among our participants, the majority were Caucasian, married, and highly educated. As such, findings cannot be generalized to the population of ASD caregivers. Further, data regarding the ability of single-parent families, and families of other races and ethnicities to participate in this intervention are needed. Given that recruitment took place at clinics and support groups, the caregivers in our study were already taking advantage of certain resources which may have left them more receptive to the intervention. Interpretation of our results may be further limited due to social desirability, which may have influenced how participants responded to surveys. Annual household income was significantly different between treatment and control groups. Potentially the treatment group responded differently because of their access to different resources, with more individuals in the treatment group reporting a household income above $70,000. Lastly, we did not gather detailed information about the child’s condition that may interact with the coping needs of the parent such as IQ, presence of aggressive or disruptive behaviors and whether the child is verbal or non-verbal. Future studies should consider the added value of these data.
Conclusion
We provide evidence that a CET intervention was feasible to implement within our study population. In the treatment group, there were statistically significant increases in CSE from pre-intervention to post-intervention. This result suggests that individuals who underwent CET felt more confident in their ability to cope, leading to more effective coping and reducing caregiver distress. This finding must be interpreted in light of the absence of significant treatment effects. Future studies, specifically a phase II trial, should seek to follow-up with a larger investigation powered to detect statistically significant effects in CSE to provide sufficient evidence that would inform a downstream clinical trial.
References
Athens, B. A., Caldwell, S. L., Umstead, K. L., Connors, P. D., Brenna, E., & Biesecker, B. B. (2017). A systematic review of randomized controlled trials to assess outcomes of genetic counseling. Journal of Genetic Counseling, 1–32. https://doi.org/10.1007/s10897-017-0082-y
Baty, B. J., Trepanier, A., Bennett, R. L., Davis, C., Erby, L., Hippman, C., et al. (2016). Developing a model of advanced training to promote career advancement for certified genetic counselors: An investigation of expanded skills, advanced training paths, and professional opportunities. Journal of Genetic Counseling, 25(4), 625–634.
Betancur, C. (2011). Etiological heterogeneity in autism spectrum disorders: More than 100 genetic and genomic disorders and still counting. Brain Research, 1380, 42–77.
Biesecker, B., & Erby, L. (2008). Adaptation to living with a genetic condition or risk: A mini-review. Clinical Genetics, 74(5), 401–407.
Carter, M., & Scherer, S. (2013). Autism spectrum disorder in the genetics clinic: A review. Clinical Genetics, 83(5), 399–407.
Center of Disease Control and Prevention. (2016). Autism spectrum disorder data and statistics. Retrieved from http://www.cdc.gov/ncbddd/autism/data.html.
Chesney, M., & Folkman, S. (1994). Psychological impact of HIV disease and implications for intervention. The Psychiatric Clinics of North America, 17(1), 163–182.
Chesney, M., Folkman, S., & Chambers, D. (1996). Coping effectiveness training for men living with HIV: Preliminary findings. International Journal of STD & AIDS, 7(suppl 2), 75–82.
Chesney, M., Chambers, D., Taylor, J., Johnson, L., & Folkman, S. (2003). Coping effectiveness training for men living with HIV: Results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine, 65(6), 1038–1046.
Chesney, M., Neilands, T., Chambers, D., Taylor, J., & Folkman, S. (2006). A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology, 11(3), 421–437.
Christensen, D. L. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveillance Summaries, 65, 1–23.
Crane, L., Chester, J. W., Goddard, L., Henry, L. A., & Hill, E. (2015). Experiences of autism diagnosis: A survey of over 1000 parents in the United Kingdom. Autism, 20(2), 153–162.
Eijzenga, W., Aaronson, N. K., Hahn, D. E., Sidharta, G. N., van der Kolk, L. E., Velthuizen, M. E., et al. (2014). Effect of routine assessment of specific psychosocial problems on personalized communication, counselors' awareness, and distress levels in cancer genetic counseling practice: A randomized controlled trial. Journal of Clinical Oncology, 32(27), 2998–3004.
Feinberg, E., Augustyn, M., Fitzgerald, E., Sandler, J., Ferreira-Cesar Suarez, Z., Chen, N., et al. (2014). Improving maternal mental health after a child's diagnosis of autism spectrum disorder: Results from a randomized clinical trial. JAMA Pediatrics, 168(1), 40–46. https://doi.org/10.1001/jamapediatrics.2013.3445.
Goodwin, P. J., Leszcz, M., Quirt, G., Koopmans, J., Arnold, A., Dohan, E., et al. (2000). Lessons learned from enrollment in the BEST study—A multicenter, randomized trial of group psychosocial support in metastatic breast cancer. Journal of Chinese Entrepreneurship, 53(1), 47–55.
Gray, D. E. (2006). Coping over time: The parents of children with autism. Journal of Intellectual Disability Research, 50(12), 970–976.
Hastings, R., & Beck, A. (2004). Practitioner review: Stress intervention for parents of children with intellectual disabilities. Journal of Child Psychology and Psychiatry, 45(8), 1338–1349.
Hayes, S. A., & Watson, S. L. (2013). The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(3), 629–642. https://doi.org/10.1007/s10803-012-1604-y.
Kennedy, P., Duff, J., Evans, M., & Beedie, A. (2003). Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. The British Journal of Clinical Psychology, 42(1), 41–52.
Lai, W. W., Goh, T. J., Oei, T. P. S., & Sung, M. (2015). Coping and well-being in parents of children with autism Spectrum disorders (ASD). Journal of Autism and Developmental Disorders, 45(8), 2582–2593. https://doi.org/10.1007/s10803-015-2430-9.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer Publishing Company, Inc.
Lee, G. K. (2009). Parents of children with high functioning autism: How well do they cope and adjust? Journal of Developmental and Physical Disabilities, 21(2), 93–114.
Lewis, K. (2008). Caregiver adaptation to pervasive developmental disorders. JHU/NHGRI Genetic Counseling Program Master's Thesis.
McConachie, H., & Diggle, T. (2007). Parent implemented early intervention for young children with autism spectrum disorder: A systematic review. Journal of Evaluation in Clinical Practice, 13(1), 120–129.
McInerney-Leo, A., Biesecker, B. B., Hadley, D. W., Kase, R. G., Giambarresi, T. R., Johnson, E., et al. (2004). BRCA1/2 testing in hereditary breast and ovarian cancer families: Effectiveness of problem-solving training as a counseling intervention. American Journal of Medical Genetics Part A, 130(3), 221–227.
McStay, R. L., Dissanayake, C., Scheeren, A., Koot, H. M., & Begeer, S. (2013). Parenting stress and autism: The role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism, 18(5), 502–510.
Miodrag, N., & Hodapp, R. M. (2010). Chronic stress and health among parents of children with intellectual and developmental disabilities. Current Opinion in Psychiatry, 23(5), 407–411.
Nguyen, C. T., Fairclough, D. L., & Noll, R. B. (2016). Problem-solving skills training for mothers of children recently diagnosed with autism spectrum disorder: A pilot feasibility study. Autism, 20(1), 55–64. https://doi.org/10.1177/1362361314567134.
Osborne, L. A., McHugh, L., Saunders, J., & Reed, P. (2008). Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders, 38(6), 1092–1103.
Peek, G., & Melnyk, B. M. (2010). Coping interventions for parents of children newly diagnosed with cancer: An evidence review with implications for clinical practice and future research. Pediatric Nursing, 36(6), 306.
Phelps, K. W., Hodgson, J. L., McCammon, S. L., & Lamson, A. L. (2009). Caring for an individual with autism disorder: A qualitative analysis. Journal of Intellectual and Developmental Disability, 34(1), 27–35.
Plant, K. M., & Sanders, M. R. (2007). Predictors of care-giver stress in families of preschool-aged children with developmental disabilities. Journal of Intellectual Disability Research, 51(2), 109–124.
Resta, R., Biesecker, B. B., Bennett, R. L., Blum, S., Estabrooks Hahn, S., Strecker, M. N., et al. (2006). A new definition of genetic counseling: National Society of genetic counselors’ task force report. Journal of Genetic Counseling, 15(2), 77–83.
Rogers, S. J., & Vismara, L. A. (2008). Evidence-based comprehensive treatments for early autism. Journal of Clinical Child & Adolescent Psychology, 37(1), 8–38.
Schaefer, G. B., Mendelsohn, N. J., Practice, P., & Committee, G. (2013). Clinical genetics evaluation in identifying the etiology of autism spectrum disorders: 2013 guideline revisions. Genetics in Medicine, 15(5), 399–407.
Smith, L. E., Seltzer, M. M., Tager-Flusberg, H., Greenberg, J. S., & Carter, A. S. (2008). A comparative analysis of well-being and coping among mothers of toddlers and mothers of adolescents with ASD. Journal of Autism and Developmental Disorders, 38(5), 876.
Zablotsky, B., Bradshaw, C. P., & Stuart, E. A. (2013). The association between mental health, stress, and coping supports in mothers of children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(6), 1380–1393. https://doi.org/10.1007/s10803-012-1693-7.
Acknowledgements
We thank the participants in this feasibility study who gave of their time and provided detailed feedback on the intervention. We also thank Trish Magyari for helping to train Christy Haakonsen Smith in the intervention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial Disclosures
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health.
Conflict of Interest
Author Haakonsen Smith C, Author Turbitt E, Author Muschelli J, Author Leonard L, Author Lewis KL, Author Freedman B, Author Muratori M, and Author Biesecker declare that they have no conflict of interest.
Human Studies and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Animal Subjects
No animal studies were carried out by the authors for this article.
Electronic supplementary material
ESM 1
(PDF 63 kb)
Rights and permissions
About this article
Cite this article
Haakonsen Smith, C., Turbitt, E., Muschelli, J. et al. Feasibility of Coping Effectiveness Training for Caregivers of Children with Autism Spectrum Disorder: a Genetic Counseling Intervention. J Genet Counsel 27, 252–262 (2018). https://doi.org/10.1007/s10897-017-0144-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-017-0144-1