Abstract
The traditional model of providing cancer predictive testing services is changing. Many genetic centres are now offering a choice to patients in how they receive their results instead of the typical face-to-face disclosure. In view of this shift in practice and the increasing demand on the ROI cancer predictive testing service, a 2 year retrospective study on patient preference in how to receive a Breast Cancer (BRCA) predictive result was carried out. Results showed that 71.7 % of respondents would have liked to have the option of obtaining their results by telephone or by letter. However, when asked about their actual experience of BRCA predictive results disclosure 40.6 % did still value the face-to-face contact, while 44.9 % would still have preferred to receive results by either post or telephone. No significant difference was found between males and females (p > 0.05) and those who tested negative or positive for the BRCA mutation (p > 0.05) in wanting a choice in how their results were disclosed. While the majority expressed a wish to have a choice in how to receive their results, it is important not to underestimate the value of a face-to-face encounter in these circumstances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genetic testing for individuals at a predisposed high risk of harboring a BRCA1/2 mutation has traditionally been carried out by means of two face-to-face or in person genetic counseling session, pre and post test. This is in keeping with published guidelines for cancer genetic counselling by the National Society of Genetic Counsellors (NSGC) (Berliner and Fay 2007). These guidelines have been modeled on the Huntington Disease (HD) testing protocol in order to provide the appropriate psychological support for those going through testing and in receiving results. NSGC recommends that post-test counseling should optimally be carried out in person. The reason for this is that results disclosure also includes a discussion on the impact of test results, medical management decisions, informing other relatives, encouragement of future contact, access to support services, all of which may be difficult to provide over the telephone or by letter (Trepanier et al. 2004). However, as these guidelines have been modeled on HD where no preventative measures are available and as the population prevalence of BRCA1/2 mutations is higher than HD, it is prudent to study the approach of face-to-face disclosure of results.
Many studies have examined the feasibility of changing from the traditional model of 2 face-to-face clinic appointments and patient satisfaction levels with alternative results disclosure methods. Sutphen et al. (2010) found a high degree of satisfaction from patients who received genetic counselling via the telephone. This approach was also found to be beneficial in reducing the barrier to gaining access to genetic counsellors due to a high demand on service from mounting referrals. Jenkins et al. (2007) found similar satisfaction rates for telephone versus in person BRCA1/2 predisposition results disclosure. Also, no difference in anxiety or general well-being was found between those who received results by telephone or in person. Additionally, satisfaction levels in a similar study showed that patients reported significantly higher satisfaction when given a choice of how to receive their result (Baumanis et al. 2009). In this study, most participants chose to receive their result by telephone and those who waited less time between availability of results and communication of these reported higher satisfaction. Moves towards a 1- visit model have already begun and this is evident from an online survey of genetic counselors, with 29.3 % of respondents reporting having adopted a 1-visit model (Wham et al. 2010).
Breast cancer is the most common form of cancer affecting women, with one in eight women diagnosed at some stage in their life. Current estimates are that approximately 226,870 women will be diagnosed with, and 39,510 will die of, cancer of the breast (Howlader et al. 2012). As 5–10 % of cancer has a hereditary basis and new technologies have facilitated identification of those at high risk, this has led to increasing demands on cancer genetic services resulting in prolonged delays in appointments. The aim of our study was to retrospectively evaluate a cohort of individuals previously seen for 2 visit predictive testing before implementing any changes to our service protocol.
Methods
Sample and Procedures
Patients with a known family BRCA mutation that were previously seen for predictive cancer genetic testing were identified through the genetics and laboratory databases. The target group was 339 individuals who had underwent BRCA predictive testing in 2009 and 2010. From the genetic database 33 individuals were identified who had breast cancer in this group and were excluded from the study as they did not fit the criterion for being unaffected for predictive testing. For the remaining 306 potential participants, all General Practitioners of these individuals were contacted to ensure they had not developed cancer and were living. This was done to avoid any potential upset of contacting families when the potential participant was deceased or had developed cancer. Through this 4 individuals were identified as unsuitable to be contacted. The remaining 302 potential participants, were checked for mutation status; 124 were BRCA positive and 178 were BRCA negative, and 230 were female and 72 were male. All of these individuals had in person pre- and post-test genetic counselling with results delivered at a face to face clinic appointment. 3 Genetic Counselors within the cancer genetics team were involved in providing this service with the same genetic counselor giving the pre- and post-test counseling. Questionnaires were colour coded, yellow for those who tested negative for BRCA mutations and green for BRCA positive and sent by post to unaffected patients with a known familial mutation within a 15 month time frame from August 2011 through to November 2012.
Ethical approval was sought and given by the hospital ethics committee.
Instrumentation
A detailed questionnaire (See Appendix A) was developed by the cancer genetics team. Questions included demographic details such as sex of the patient, and distance to appointments, in addition to asking about how they would have liked results to have been delivered.
Data Analysis
Statistical analysis was carried out by using the R version 3.1.2 http://cran.uk.R-project.org/ (R Development Core Team, 2012). Firstly questionnaire responses were collated in an excel data sheet and divided in male or female groups and into negative or positive for BRCA mutation. Answers were collated into groups for male versus female data and coded ‘N’ if no choice ticked for receiving a choice for results disclosure or ‘Y’ if a choice would have been preferred. If a choice was preferred male and female responses and positive or negative BRCA results were collated to determine if letter or telephone notification of results were suitable options. Descriptive analysis of data in Microsoft excel was used to display the proportion of respondents who would have liked an option and preference for telephone or letter. This approach was also used in showing the retrospective preference for results disclosure when asking participants to recall their actual experience of receiving results face-to-face in clinic.
Descriptive statistics, using R version 3.1.2, were preformed to determine if certain barriers to attend clinic for face-to-face results disclosure significantly affected whether participants wished to have a choice of results disclosure. All possible model permutations were created using the R package MuMln (Burnham and Anderson 2002). Each model was ranked based on the Akaike information criterion (AIC), a measure of how well each model explains the data (Akaike 1974). A lower AIC value indicates a more adequate model. To calculate the relative importance of each variable relative to all other variables, the sum of the Akaike weight was used; the larger the value of relative importance (which varies between 0 and 1), the more important the variable.
Contrasts between total male and female and positive versus negative respondents in wanting a choice of results disclosure were performed using a Pearson’s Chi Square test in R version 3.1.2. To determine if there was a bias to the study the same test was used to examine responders and non-responders in the context of being male or female or BRCA positive or negative.
For the qualitative data analysis, the Grounded Theory (GT) was used to thematically analyze the response to free text questions (Wolcott 1990). This method firstly, codes line by line and subsequently five dominant themes were identified by one of the Genetic Counsellor involved in providing predictive BRCA testing. The category of dominant themes were then looked at for frequency in the free text responses.
Results
Response Rate and Demographics
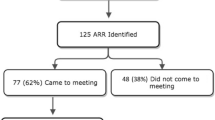
Three-hundred and two people were contacted by post and asked to anonymously complete and return the questionnaire. A total of 138 completed questionnaires had been returned (response rate of 45.7 %). The demographics of returned questionnaires are summarised in Table 1. The range of months passed from disclosure of results from the initial 2009 predictive participants to when the questionnaire was administered was 2 years to 6 months (mean = 30 months). The mean time between results disclosure and administering of questionnaire for all participants was 29 months (2 years to 5 months).
Alternative to Face to Face Results Disclosure
Participants in the survey were asked if they would have liked the option of obtaining their result by letter or by telephone instead of the obligatory face to face disclosure. It was found that 99 people wanted to have an option, 27 people did not want to have an option, and 12 people were uncertain [Fig. 1a]. Those who answered yes were then asked if they would prefer to receive the result by letter or by telephone. Of the 99 who wanted an option, 47 would prefer a letter, 43 would prefer a telephone call and nine did not answer [Fig. 1b].
Participants were also asked; to draw on their actual experience of receiving their results face to face and to respond to the preference of results disclosure by telephone, letter or face to face. Sixty-two respondents would have preferred to have received their test result by either post (n = 32) or telephone (n = 30). Fifty-six respondents did still prefer the face-to-face approach, while 16 people were unsure and four respondents gave no answer. These results are shown in Fig. 2
Variables Which Best Explain Respondents’ Preference for an Option of How They Receive Results
The most adequate model based on AIC analysis included the single variable of distance travelled. Respondents who scored distance travelled high showed a positive trend, although not significant, towards a preference for the availability of an option regarding results disclosure (Model average coefficient = 0.30494, p value = 0.138).
However, this model was not found to be more than two AIC values lower than the next best model and hence cannot be determined as the single best model. The relative importance of each explanatory term is given in Fig. 3. Distance travelled was the most important variable, with the highest relative importance value of 0.53. Parking (relative importance 0.43) and the patient’s sex (relative importance 0.31) were found to be the next two most important.
Gender as a Variable to Wanting a Choice
A total of 20 out of 25 male respondents and 69 out of 109 female respondents wished to have a choice of how to receive results. Comparative analysis between males and females who went through the BRCA predictive genetic test process and wanting a choice of result disclosure showed no significant difference [X 2 (1)=1.5626, p-value = 0.2113].
Retrospective View and Gender as a Variable on Choice of Results Disclosure
Comparative analysis between males and females when asked to retrospectively choose an alternative to face-to-face results disclosure showed no significant difference in wanting a choice [X 2 (1) = 0.7513, p-value = 0.3861].
To check for bias in the study results, comparative analysis between responders and non-responders who were male and female showed no significant difference [X 2 (1) = 3.0709, p-value = 0.07971].
Test Result as a Variable to Wanting a Choice
Comparative analysis between those who tested positive and negative for the BRCA mutation and wanting a choice of result disclosure showed no significant difference [X 2 (1) = 2.7479, p-value = 0.09738].
Retrospective View and Test Result as a Variable on Choice of Results Disclosure
Comparative analysis between BRCA positive and negative respondents when asked to retrospectively choose an alternative to face-to-face results disclosure showed no significant difference in wanting a choice [X 2 (1) = 0.1568, p-value = 0.6921].
To check for bias in the study results, comparative analysis between responders and non-responders who were BRCA positive and negative showed no statistical difference [X 2 (1) = 0.9552, p-value = 0.3284].
Negative Result and Retrospective View on Results Disclosure
A total of 18.6 % (16/86) of participants who tested negative and ticked yes to a choice of having results by telephone or letter retrospectively preferred face to face. Fifty percent (43/86) who ticked yes to choice of results by either telephone or letter also retrospectively would have preferred this option. Only 3.4 % (3/86) who were unsure about having a choice retrospectively preferred face to face and another 3.4 % (3/86) who were unsure remained unsure retrospectively. A total of 15.1 % (13/86) of participants who tested negative and selected no to a choice of results disclosure, concordantly choose face to face retrospectively.
Positive Result and Retrospective View on Results Disclosure
Similarly, for those who tested positive 9.6 % (5/52) who ticked yes to a choice of having results by telephone or letter retrospectively preferred face to face. A total of 46.1 % (24/52) who ticked yes to choice of results by either telephone or letter also retrospectively would have preferred this option. Only 5.7 % (3/52) who were unsure about having a choice retrospectively preferred face to face and another 3.8 % (2/52) who were unsure remained unsure retrospectively. Twenty-three percent (12/52) of participants who tested positive and selected no to a choice of results disclosure, concordantly chose face to face retrospectively.
Helpful Aspects of Face to Face Appointment
Participants who felt that a face to face appointment was beneficial were invited to express the aspects that they found helpful in an open text answer. Ninety-seven individuals provided a response. When responses were reviewed, five dominant themes were identified (Table 2). The benefit most widely communicated was that a face to face meeting allowed the person to ask questions and receive answers immediately (n = 54 respondents). Many respondents valued the provision of emotional support and reassurance provided (n = 20 respondents) and others felt that they were put at ease by the staff at an anxious time (n = 19 respondents). While less frequently articulated, two other interesting themes were identified. Face to face was found helpful by some because it allowed a family member or friend to be present when the result was disclosed (n = 5) and three people told us how the structure of an appointment allowed them time to prepare themselves for the impact of the test result.
Discussion
We investigated whether those who had been through the BRCA predictive genetic counseling process would have liked to have a choice in how to receive their results, instead of the compulsory face-to-face disclosure. We found that the majority of participants (71 %) would have liked to have been offered a choice of receiving their results either by telephone or letter. This could be explained by the fact that participants were contact over 1 year post-results disclosure, and many reports on psychological distress after BRCA results disclosure have shown that after several years most are not likely to experience genetic testing concerns (Beran et al. 2008; Bosch et al. 2012; Halbert et al. 2011; Hamilton et al. 2009). Our questionnaire would have been received over a year post results disclosure and so a choice may seem more reasonable to respondents at this stage. However, interestingly when respondents were asked to recall the actual experience of face to face results disclosure, 40.6 % still preferred the face-to-face disclosure while 44.9 % would have preferred telephone or letter. Fifteen percent of respondents who initially wished to have received a choice in results disclosure retrospectively preferred face-to-face. The implications of these findings are discussed with the view to implementing service level change in how the cancer predictive results disclosure is operated.
Effect of Gender on Option of How to Receive Results
Gender of the respondent did not affect the wish to have a choice of results disclosure instead of the obligatory face to face disclosure, as no statistical significance was found. Also, gender had no effect on when respondents were asked to recall the experience of face to face disclosure or on choosing an alternative option of results disclosure by letter or telephone. However, it is important to note that out of the cohort of potential participants contacted, more females responded (47.3 %) to the questionnaire then males (35 %) but no significant difference was seen between responders and non-responders in this group. So, a true value on the statistical significance of no difference between male and female responders and wanting a choice of results disclosure can be drawn. More females responding would be expected, as the amount of males coming forward for testing for BRCA would be anticipated to be less (Struewing et al. 1995). Health implications are less for men rather than women. Another explanation could be drawn from Lodder et al. (2001) which found that men having undertook BRCA predictive testing did not experience significant levels of distress or anxiety pre- or post-test. Many of the men in Lodder’s study were not concerned for their own health but more for the risk to their children, especially daughters. Similarly, Liede et al. (2000) found that the principal motivator for men in pursuing BRCA predictive testing was for their daughters. Therefore, our study’s response rate from males is not unusual in this regard, and the fact that 80 % of males wished to have a choice of how results are disclosed may also be explained by the above.
In the female group 63 % wished to have a choice of how results were disclosed. This is an important observation as the potential medical impact and management of females who go through the BRCA predictive testing process are significant. Many studies have looked at the female experience with BRCA predictive testing and the psychological impact of results. In one study, Halbert et al. (2011) looked at the long-term effects of BRCA testing in women and found that the majority of women did not experience distress about their result at least 1 year after receiving the information. Additionally, this study did observe a short term rise in anxiety and sadness in female mutation positive carriers compared to those who tested negative, but this reduced within the year of results disclosure. Hamilton et al. (2009) obtained similar findings when looking at emotional distress after BRCA testing. As our cohort were contacted at least 1 year post-test disclosure, this may explain why the majority of females felt it would be reasonable to offer a choice in how to receive results. These results would suggest that it is acceptable to males and females who have been through the BRCA predictive testing to be offered a choice in how to receive their results instead of the obligatory face to face disclosure.
Effect of Positive or Negative BRCA Result on Option of How to Receive Results
Our study showed that there was no difference in those who tested positive for BRCA mutations and those who tested negative in initially preferring a choice regarding how to receive their result and in retrospectively recalling their actual experience of face to face disclosure and preferring an alternative to this. Forty-one percent of respondents were positive and 48 % where negative for BRCA mutation, and no significant difference was seen between responders and non-responders in these groups. Therefore, a true value on the statistical significance of no difference between positive and negative responders and wanting a choice in results disclosure can be drawn. Sixty-three percent of those who tested positive and 77 % of those who tested negative for BRCA wished to have a choice in how their results were delivered. It would seem that those who tested both positive and negative having been through the BRCA predictive testing process would deem it reasonable to be offered a choice in results delivery. This would be in keeping with research indicating that general and cancer specific distress is reduced overtime in those who go through BRCA testing. Beran et al. (2008) and Hamilton et al. (2009) showed that general distress due to testing positive for BRCA mutations remitted by 1 year after genetic results disclosure and that there was only a difference in cancer specific distress at this time frame between those who tested positive and negative. This may reflect certainty about mutation status and cancer risk and understanding of management and screening options. Again our group were surveyed at least 1 year post results disclosure, and the majority would have liked a choice in results delivery.
Other Variables Affecting Option of Results Disclosure
We also asked about numerous factors that may make it difficult for respondents to attend genetics appointments. Overall, taking all variables into account, logistical issues of distance and parking appear to be the highest ranking variables in respondents showing a positive trend in wanting a choice in results disclosure. However, these were not found to be statistically significant in influencing whether a choice of result disclosure was wanted. It is important to note that the clinic service provided would require patients to travel considerable distance, and it is of no surprise that this was noted as the most frequent variable in making it difficult to attend for a genetics appointment. Other studies have noted that access to genetic services can be improved by telecommunications (Bradbury et al. 2011; Zilliacus et al. 2010) and in view of lack of genetic counselling resources in The Republic of Ireland, this could also be an option to be considered.
Face to Face Results disclosure
In view of the impact of changing our protocol from the face to face model of results disclosure we felt it was important to draw on participants’ actual experience of receiving their results in this way and thinking of the alternative mode by letter or telephone. Approximately 45 % felt that telephone or letter would have been preferred, and 40.6 % did still prefer face to face disclosure. This is in contrast to the resounding response of respondents initially wanting a choice in how to receive results instead of the obligatory face to face without an option. Also, 18 % of those who tested negative and 10 % of those who tested positive who initially wanted a choice in results disclosure, retrospectively preferred face to face instead of the alternative letter and telephone option. This reflects that it is important not to undervalue the face-to-face results disclosure but to consider an alternative by telephone and letter as a reasonable mode of results delivery. The most evaluated alternative method to face to face result disclosure is genetic counselling by telephone (Baumanis et al. 2009; Sangha et al. 2003). These studies found that the use of a telephone is not significantly inferior to face to face meetings. However, it is important to consider both the benefits and disadvantages of giving results by telephone compared to over face to face appointments. Possible advantages of phone counselling include avoidance of the stress, expense and time commitment of a clinic visit and a reduction in barriers to service by increasing accessibility for patients (Tsu et al., 2002). Another advantage is that a telephone call allows for a more timely response rate to the patient from the time the test result becomes available to the genetic counsellor (Klemp et al. 2005). There are several disadvantages to giving results by telephone that include the loss of rapport building between the counselor and patient, less immediate re-assurance compared with face-face results disclosure, and diminished attention to support needs of the patient at that time (Sangha et al. 2003).
Other studies have looked at the support needs at results disclosure. Aktan-Collan et al. (2000) found that 46 % of patients reported the need for support being the greatest at the results disclosure stage for hereditary non-polyposis colorectal cancer (HNPCC). Our study also showed that just under half of respondents did value the face-to-face disclosure for three main reasons: having the opportunity to ask questions and receive immediate answers, to be put at ease and alleviate anxiety, and provision of emotional support and reassurance. As 40.6 % of respondents did value the face-to-face disclosure, it would seem that moving away from this completely by offering only results by letter or telephone would not be appropriate. Doughty Rice et al. (2009) found that 90 % of those who tested positive for BRCA mutations attended for follow up appointments in the genetic clinic after receiving their result by telephone, in comparison to only 10.5 % of those who tested negative. However, it is important to note that there was no difference in satisfaction levels in those who received their results by telephone or face to face in this study, as is reported in many other studies (Baumanis et al. 2009; & Helmes et al. 2006; Jenkins et al. 2007; Klemp et al. 2005). Therefore, the face to face contact is important in the context of positive results and there is need for additional support and information after telephone results disclosure.
Study Limitations and Research Recommendations
One of the limitations of the study was asking regarding waiting times for the initial appointment in the genetic clinic as 6 months was included two options in the response categories. This would make it difficult to ascertain individuals who waited only 6 months to those who waited more than 6 months. For this reason we did not include this data in the study. Recommendations from our study would be that offering a choice of results disclosure to individuals going through the BRCA predictive process would be a reasonable option without undervaluing the current protocol of obligatory face to face results disclosure. It would be important to use clinical judgment in cases where alternatives to face to face results disclosure may cause distress and to always offer a follow up appointment for additional information and support, especially in the case of mutation positive families.
Conclusion
Changing protocol from long standing practice is never easy from a counsellor or patient perspective. Also, it is important to keep in mind the serious implications of BRCA1/2 results disclosure for those that test positive. Information on medical management, screening and support is important for those who test positive. Therefore, for future practice it would be important to audit patients’ experience of an alternative to face to face results disclosure when a protocol change is implemented based on this retrospective study.
References
Akaike, H. (1974). A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19(6), 716–723.
Aktan-Collan, K., Mecklin, J. P., de la Chapelle, A., Peltomaki, P., Uutela, A., & Kaariainen, H. (2000). Evaluation of a counselling protocol for predicitive genetic testing for hereditary non-polyposis colorectal cancer. Journal of Medical Genetics, 37, 108–13.
Baumanis, L., Evans, J. P., Callanan, N., & Susswein, L. R. (2009). Telephoned BRCA1/2 genetic test results: prevalence, practice, and patient satisfaction. Journal of Genetic Couselling, 18, 447–463.
Beran, T. M., Stanton, A. L., Kwan, L., Seldon, J., Bower, J. E., Vodermaier, A., & Ganz, P. A. (2008). The trajectory of psychological impact in BRCA ½ genetic testing: does time heal? Annals of Behaviour Medicine, 36, 107–16.
Berliner, J. L., & Fay, A. M. (2007). Risk assessment and genetic counselling for hereditary breast and ovarian cancer: recommendations of the national society of genetic counselors. Journal of Genetic Counselling, 16, 241–260.
Bosch, N., Junyent, N., Gadea, N., Brunet, J., Ramon Cajal, T., Torres, A., Grana, B., Velasco, A., Darder, E., Mensa, I., & Balmana, J. (2012). Breast, 21, 755–60.
Bradbury, A. R., Patrick-Miller, L., Fetzer, D., Egleston, B., Cummings, S. A., Forman, A., Bealin, L., Peterson, C., Corbman, M., O’Connell, J., & Daly, M. B. (2011). Genetic counselor opinions of and experiences with telephone communication of BRCA1/2 test results. Clinical Genetics, 79(2), 125–31.
Burnham, K. P., & Anderson, D. R. (2002). Model selection and multimodel inference: A practical information-theoretic approach (2nd ed.). New York: Springer-Velag.
Halbert, C. H., Stopfer, J. E., McDonald, J., Weathers, B., Collier, A., Troxel, A. B., & Domchek, S. (2011). Long term reactions to genetic testing for BRCA 1 & 2 mutations: does time heal women’s concerns? Journal of Clinical Oncology, 29, 4302–4306.
Hamilton, J. G., Lobel, M., & Moyer, A. (2009). Emotional distress following genetic testing for hereditary breast and ovarian cancer: a meta analytic review. Health Psychology, 28, 510–518.
Helmes, A. W., Culver, J. O., & Bowen, D. J. (2006). Results of a randomized study of telephone versus in-person breast cancer risk counselling. Patient Education and Counselling, 64, 96–103.
Howlader N., Noone A.M., Krapcho M., et al. (eds). (2012). SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations), National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2009_pops09/, based on November 2011 SEER data submission, posted to the SEER web site, April 2012.
Jenkins, J., Calzone, K. A., Dimond, E., Liewehr, D. J., Steinberg, S. M., Jourkiv, O., Klein, P., Soballe, P. W., Prindiville, S. A., & Kirsch, I. R. (2007). Randomizes comparison of phone versus in-person BRCA1/2 predisposition genetic test result disclosure counselling. Genetics in Medicine, 9, 487–495.
Klemp, J. R., O’Dea, A., Chamberlain, C., & Fabian, C. J. (2005). Patient satisfaction of BRCA ½ genetic testing by women at high risk for breast cancer participating in a prevention trial. Familial Cancer, 4, 279–284.
Liede, A., Metcalfe, K., Hanna, D., Hoodfar, E., Snyder, C., Durham, C., Lynch, H. T., & Narod, A. (2000). Evaluation of the needs of male carriers of mutations in BRCA 1 or BRCA 2 who have undergone genetic counselling. American Journal of Human Genetics, 67, 1494–1504.
Lodder, L., Frets, P. G., Trijsburg, R. W., Tibben, A., Meijers-Heijboer, E. J., Duivenvoorden, H. J., Wagner, A., van der Meer, C. A., Devilee, P., Cornelisse, C. J., & Niermeijer, M. F. (2001). Men at risk of being a mutation carrier for hereditary breast/ovarian cancer: an exploration of attitudes and psychological functioning during genetic testing. European Journal of Human Genetics, 9, 492–500.
R Development Core Team (2012). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. See http://www.R-project.org
Rice C.D., Ruschman J.G., Martin L.J., Manders J.B., Miller E. (2009). Retrospective comparison of patient outcomes after in-person and telephone results disclosure counselling for BRCA1/2 genetic testing. Familial Cancer.
Sangha, K., Dircks, A., & Langlois, S. (2003). Assessment of the effectiveness of genetic counseling by telephone compared to a clinic visit. Journal of Genetic Counseling, 12(2), 171–184.
Struewing, J. P., Lerman, C., Kase, R. G., Giambarresi, T. R., & Tucker, M. A. (1995). Anticpated uptake and impact of genetic testing in hereditary breast and ovarian cancer families. Cancer Epidemiology Biomakers and prevention, 4, 169–173.
Sutphen, R., Davila, B., Shappell, H., Holtje, T., Vadaparampil, S., Friedman, S., Toscano, M., & Armstrong, J. (2010). Real world experience with cancer genetic counselling via telephone. Familial Cancer, 9(4), 681–9.
Trepanier, A., Aherns, M., McKinnon, W., Peters, J., Stopfer, J., & Grumet, S. C. (2004). Genetic cancer risk assessment and counselling: recommendation of the national society of genetic counsellors. Journal of Genetic Counselling, 13, 83–114.
Tsu, R. C., Burm, M. L., Jennifer, A. G., & Sells, C. W. (2002). Telephone vs. face-to-face notification of HIV reults in high risk youth. Journal of Adolescent Health, 30, 154–160.
Wham, D., Vu, T., Chan-Smutko, G., Kobelka, C., Urbauer, D., & Heald, B. (2010). Assessment of clinical practices among cancer genetic counselors. Familial Cancer, 9, 459–68.
Wolcott, H. (1990). Writing up qualitative research. London: Sage.
Zilliacus, E. M., Meiser, B., Lobb, E. A., Kirk, J., Warwick, L., & Tucker, K. (2010). Women’s experience of telehealth cancer genetic counselling. Journal of Genetic Counselling, 19, 463–72.
Conflict of Interest
The authors declare that they have no conflict of interest. This article does not contain any studies with human participants or animals preformed by any of the authors.
Ethical Approval
All procedures preformed in studies involving human particiapants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed Consent
Informed consent was optained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A


Rights and permissions
About this article
Cite this article
O’Shea, R., Meany, M., Carroll, C. et al. Predictive Genetic Testing and Alternatives to Face to Face Results Disclosure: A Retrospective Review of Patients Preference for Alternative Modes of BRCA 1 and 2 Results Disclosure in the Republic of Ireland. J Genet Counsel 25, 422–431 (2016). https://doi.org/10.1007/s10897-015-9887-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-015-9887-8