Abstract
Growing demand for and limited geographic access to genetic counseling services is increasing the need for alternative service delivery models (SDM) like telephone genetic counseling (TGC). Little research has been done on genetic counselors’ perspectives of the practice of TGC. We created an anonymous online survey to assess whether telephone genetic counselors believed the tasks identified in the ABGC (American Board of Genetic Counseling) Practice Analysis were performed similarly or differently in TGC compared to in person genetic counseling (IPGC). If there were differences noted, we sought to determine the nature of the differences and if additional training might be needed to address them. Eighty eight genetic counselors with experience in TGC completed some or all of the survey. Respondents identified differences in 13 (14.8 %) of the 88 tasks studied. The tasks identified as most different in TGC were: “establishing rapport through verbal and nonverbal interactions” (60.2 %; 50/83 respondents identified the task as different), “recognizing factors affecting the counseling interaction” (47.8 %; 32/67), “assessing client/family emotions, support, etc.” (40.1 %; 27/66) and “educating clients about basic genetic concepts” (35.6 %; 26/73). A slight majority (53.8 %; 35/65) felt additional training was needed to communicate information without visual aids and more effectively perform psychosocial assessments. In summary, although a majority of genetic counseling tasks are performed similarly between TGC and IPGC, TGC counselors recognize that specific training in the TGC model may be needed to address the key differences.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Within the last several years, there have been several important developments that have led to a potential increase in demand for genetic counseling services. The United States Preventive Task Force, for example, has recommended genetic counseling for women whose family history places them at an increased likelihood to carry a BRCA1 or BRCA2 mutation (Moyer 2014; United States Preventive Task Force 2005). As these recommendations have been classified as a “Grade B” recommendation, they are covered under the Affordable Care Act (U.S. Preventive Services Task Force 2014). Additionally, there appears to be a recent trend of insurance companies, including national provider Cigna Corporation, covering the cost of genetic counseling and requiring patients to have genetic counseling prior to providing coverage for certain genetic tests (Graf et al. 2013; Lee 2013).
Another development affecting demand for genetic counseling services is the expanded use of next generation sequencing technology in clinical genomic testing. This technology has contributed to the increasing number of genomic tests available overall (Genetests 2015). Furthermore, use of the technology brings with it potential challenges, especially in informed consent and results interpretation, and these are challenges genetic counselors are specially trained to address (Accreditation Council for Genetic Counseling 2013). The growing need for genetic counselors in the absence of significant growth in the workforce could limit appointment availability. This could lead to other providers with no specialized training in genetics taking on the responsibility of genetic testing, test interpretation and counseling. Such a situation may not be ideal since there have been several reports of adverse patient outcomes when non-genetics providers incorrectly ordered and interpreted genetic testing results and/or provided inadequate genetic counseling (Bensend et al. 2013; Bonadies et al. 2014; Brierley et al. 2010, 2012). Additionally, although there is no clear evidence that the existing genetic counseling workforce cannot meet the demand for services even with the increased availability of genetic testing, the geographic distribution of genetic counselors is limited, particularly in some rural areas of the country (National Society of Genetic Counselors 2014). As a result of all of these factors, genetic counselors are increasingly using alternative service delivery methods, such as telephone genetic counseling (TGC), to increase access to services (Cohen et al. 2013).
In order to explore access to genetic counseling services, in 2009 the National Society of Genetic Counselors (NSGC), the leading professional organization of genetic counselors in the United States, appointed a Service Delivery Model Task Force (SDMTF) to assess the status of the existing service delivery models (SDM). As part of this work, the SDMTF proposed four basic models of genetic counseling service delivery: in person genetic counseling (IPGC), TGC, group counseling (multiple non-related individuals receiving counseling for a similar indication), and telegenetics (counseling occurring remotely using video conferencing). IPGC, also known as face to face counseling, has been the traditional model for genetic counseling services and is thought to be the predominant model used in genetic counseling currently. TGC was defined as “a patient is provided genetic counseling for a new indication or concern and the session is completed entirely via telephone” and parallels an IPGC session (Cohen et al. 2012, p. 647).
Even before the NSGC recognized the importance of exploring TGC as an SDM, there had been studies investigating the provision of genetic counseling by telephone. Most of the initial studies were focused on patient outcomes related to receiving BRCA1/2 genetic test results by telephone versus in person. Overall, when comparing the two methods of receiving results, these studies found similar levels of patient satisfaction (Baumanis et al. 2009; Chen et al. 2002; Jenkins et al. 2007), retained knowledge, anxiety, and psychological well-being (Jenkins et al. 2007). As the use of TGC increased, there emerged several studies looking at patient perceptions and reactions to performing an entire genetic counseling session by telephone, rather than just results disclosures. Sangha et al. (2003) found no difference in knowledge or anxiety in patients receiving TGC for positive maternal serum screening compared to IPGC.
There have also been a few randomized trials comparing entire genetic sessions for cancer risk assessment conducted in IPGC and TGC. Similar to the studies performed on receiving genetic test results by telephone, these studies showed similar levels of patient satisfaction (Platten et al. 2012; Schwartz et al. 2014), knowledge (Schwartz et al. 2014), cancer worry (Helmes et al. 2006; Platten et al. 2012), risk perception (Helmes et al. 2006), decisional conflict (Schwartz et al. 2014), quality of life (Platten et al. 2012; Schwartz et al. 2014) and motivation to change health-related behavior (Helmes et al. 2006). In addition to showing a high level of patient satisfaction, knowledge of cancer risk, and increased motivation to change health-related behaviors, Sutphen et al. (2010) also showed that a majority of participants in their study indicated they would not have pursued genetic counseling had it not been offered by telephone, further illustrating the potential value of this SDM.
In addition to evaluating TGC using patient-related outcome measures, it is important to evaluate the SDM from the genetic counselors’ perspective as well. Only by evaluating TGC from both perspectives can we identify best practices and how to properly prepare genetic counselors for this practice. In the rationale for their planned randomized control trial comparing TGC and IPGC for BRCA1 and BRCA2 counseling, Peshkin et al. (2008) recognized this. As part of their study design, they planned to implement a Genetic Counselor Questionnaire intended to capture information from the counselor performing TGC regarding content covered in session, ability to establish rapport, perceived patient comprehension, and ability to provide patient support, answer questions and provide information. Although they have not yet published any outcome data from this questionnaire as of yet, this group recognized that there could be differences in these areas that would be important to identify in order to establish the best manner in which to provide genetic counseling by telephone. Bradbury et al. (2011) also recognized the importance of obtaining the perspectives of counselors providing TGC. In studying the opinions and experiences of genetic counselors delivering BRCA1/2 results by telephone, they found that many respondents answered that they were “uncomfortable” providing BRCA 1/2 test results by this method, particularly positive results and variants of uncertain significance. Study respondents identified lack of non-verbal cues, inability to use visual aids, and the increased difficulty of establishing rapport and providing psychosocial support as potential provider barriers to TGC (Bradbury et al. 2011).
Bradbury et al. (2011) and Peshkin et al. (2008) provided some of the initial groundwork suggesting the value of considering the genetic counselors’ perspectives of TGC to inform the development of best practices. Additionally, the Accreditation Council for Genetic Counseling (ACGC), the profession’s credentialing organization, has recently recognized the importance of preparing practicing genetic counselors for work across service delivery models. Specifically, they have established a practice based competency requiring trainees to “understand how to adapt genetic counseling skills for varied service delivery models” (ACGC 2013). As a result, more information is needed regarding whether there are true differences between the TGC and IPGC SDM’s and if so, how genetic counselors perceive and adapt to those differences. Since, thus far, there have been no systematic investigations of how conducting complete genetic counseling sessions by telephone is similar to or different from IPGC from the genetic counselor’s perspective, this is an important initial step in better characterizing TGC overall. By better characterizing the practice of TGC from the provider perspective, we may, ultimately, be better positioned to train students and genetic counselors on how to most effectively and appropriately provide the service.
Although information about what actually occurs in TGC is limited, there is information available regarding what occurs in genetic counseling practice overall. In 2008, the ABGC convened a task force to identify tasks that genetic counselors routinely perform in a typical genetic counseling session (Hampel et al. 2009). Through a survey sent to genetic counselors in the United States and Canada, a total of 143 tasks were identified as being “Quite Significant” or “Extremely Significant” to the practice of genetic counseling by at least 67 % of participants. These tasks were separated into five overarching domains: Case Preparation and History, Risk Assessment and Diagnosis, Testing, Psychosocial Assessment, and Ethical/Legal/Research/Resources, and then further divided into 15 content areas with 4 to 15 specific tasks in each content area (Hampel et al. 2009). Since this Practice Analysis is the most comprehensive description of the tasks genetic counselors routinely perform in a typical genetic counseling session, it serves as a reasonable basis for evaluating differences between IPGC and TGC services.
Purpose of the Study
The overall purpose of this study is to compare and contrast genetic counseling performed using the TGC SDM with counseling performed using the IPGC SDM. Specifically, through the use of a novel online anonymous survey, we aimed to determine whether genetic counselors providing services by telephone performed the tasks identified in the ABGC Practice Analysis differently than in IPGC (Hampel et al. 2009). For any tasks performed differently, we used qualitative methods to determine the nature of the differences. Lastly, we aimed to determine whether telephone genetic counselors believed that additional training might be needed to address any differences identified between the two models of practice. It was thought this study’s findings would contribute to the overall body of research on the provision of TGC services and provide information on how to best prepare future genetic counselors to provide these services in the most effective way possible.
Methods
Participants
For this study, participants were those members of NSGC or ABGC who performed TGC according to the definition proposed by the NSGC SDMTF (Cohen et al. 2012). Exclusion criteria for the study included any counselor who had not performed TGC according to the NSGC SDMTF definition. Once approval from the Institutional Review Board at Wayne State University was obtained, study participants were identified through e-mail recruitment from the two professional organizations, NSGC and ABGC. Both organizations were utilized for recruitment in order to capture as many counselors performing TGC as possible. An initial recruitment e-mail explaining the study and inclusion criteria that also contained a link to the online survey was sent to the NSGC’s member directory in March 2014. A follow up e-mail was sent 2 weeks later as a reminder. The initial e-mail was sent to 3011 NSGC members, and the reminder e-mail was sent to 3025 members. The same initial recruitment e-mail was also sent to diplomates of the ABGC in March 2014. Unlike NSGC, we were not able to send a follow-up reminder email for ABGC. The ABGC had 3364 diplomates at the time of the study. The survey was distributed to 3176 diplomates with working e-mail addresses registered with ABGC.
Instrumentation
We used a mixed methods study design to ascertain genetic counselors’ perceptions about differences between IPGC and TGC. We created a novel 62 question online survey, including Likert-scale, multiple choice, and open-ended questions, using the internet survey provider Survey Monkey. The survey began with an information sheet explaining the study purpose, procedures, and possible risks and benefits to the participants. The information sheet also functioned as an informed consent page. At the bottom of this page, the participants had the option to either participate or decline participation in the study. Participants had the option to skip questions or withdraw from the study at any point. The only required question, positioned directly after the information sheet, was a question involving the inclusion criteria for the study. This question was intended to ensure that only genetic counselors performing TGC according to the NSGC SDMTF’s definition completed the survey (Cohen et al. 2012). If participants answered “No” to this question, they were directed to the end of the survey. If participants answered “Yes” to this question, they were directed to the remainder of the survey. A brief introduction and instructions followed the inclusion criteria question.
The first section of the survey contained Likert-type questions used to determine differences between how counselors perform the various tasks identified by the ABGC Practice Analysis in TGC and IPGC (Hampel et al. 2009). The Likert scale had five answer choices: “Exactly the same,” “Almost the same,” “Somewhat different,” “Mostly different,” and “Completely different.” Participants also had the option to label a task as “Cannot assess.” We used 13 of the 15 different content areas from the practice analysis to create our survey questions: Case Preparatory Work, Contracting, Medical History, Pedigree and Family History, Risk Assessment, Diagnosis/Natural History Discussion, Inheritance/Risk Counseling, Testing Options, Test Interpretations/Results Discussion, Psychosocial Assessment, Psychosocial Support/Counseling, Resources and Follow Up, and Ethical/Legal. The content areas of Research/Study Coordination and Education/Policy were excluded from the study since tasks in these areas do not relate to direct patient counseling. For each of the 13 content areas used, each task included under the content area was listed separately so that study participants could compare their use during TGC to IPGC. Open-ended questions followed each Likert-type question asking the participant to identify key differences in the content area, why these differences exist, and any other differences between TGC and IPGC in the particular content area that were not already addressed.
Following the Likert-type section, there were two general open-ended questions. These questions asked participants to identify any other differences they believed existed between TGC and IPGC that were not addressed previously in the survey, and to identify additional skills, if any, the participants believed genetic counselors would need to effectively perform TGC. The survey ended with demographic questions collecting information regarding the participants’ genetic counseling career: typical patient type counseled by telephone, years of experience in each SDM, NSGC region affiliation, practice setting in each SDM, amount of time spent counseling per patient in each SDM, and under what circumstances they have performed TGC.
An initial draft of the survey was created by the authors and reviewed with staff from the Wayne State University Center for Urban Studies who have expertise in survey design. The revised survey was then piloted on three genetic counselors with experience in TGC. The first step in the pilot included a review of the survey by each of the counselors separately with the authors. Changes to the survey were made based on comments provided by the pilot participants. The survey instrument was then redistributed to the pilot participants for a final pilot review. No additional changes were suggested at that time. We did not perform any formal reliability or validity studies on our study instrument.
Procedures
To increase participation, our survey was sent to email addresses available through both the NSGC and the ABGC. Since many genetic counselors are members of both organizations, many individuals would likely have received more than one recruitment email inviting participation. Survey Monkey automatically collects Internet Protocol (IP) addresses for all respondents to surveys. These IP addresses were analyzed to ensure there were no duplicate responses. There were no duplicate responses detected among those individuals that agreed to complete the study and met the inclusion criteria for participation. Once this audit was performed, the IP addresses were separated from the survey results prior to any additional data analysis. Although this may not completely rule out the possibility of an individual completing the survey more than once on more than one computer, this method significantly reduces that possibility of duplicate results.
Data Analysis
Quantitative data were analyzed using IBM’s Statistical Product and Service Solutions Statistics (SPSS), Version 22 software to generate descriptive statistics. These included frequencies for the Likert-type questions, and ranges, mean values and standard deviations for the demographic variables. To better identify differences, the Likert-type responses for each practice analysis task were reorganized into three categories: “Same” “Different,” and “Cannot Assess.” The “Same” category included the responses “Exactly the same” and “Almost the same.” The “Different” category included the responses “Somewhat different,” “Mostly different,” and “Completely different.” The category “Cannot Assess” was excluded from analysis. We could not identify any previous studies or statistical methods for establishing what threshold to use when trying to highlight which tasks were identified as different most often. We decided, given the exploratory nature of this study, to highlight those tasks in which at least 25 % of respondents answered they performed a task differently.
Open ended questions were analyzed using conventional content analysis (Hsieh and Shannon 2005). The data were analyzed by the first author who identified and established codes for emerging themes and subthemes. The data was then analyzed independently by the other two authors who coded each response using the themes and subthemes identified by the first author. Any inconsistencies in coding were discussed until coding agreement was reached. All authors agreed on all of the main identified themes.
Results
Demographics
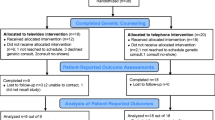
One hundred seventy-seven individuals consented to take the survey. A total of 173 of these participants answered the required inclusion/exclusion criteria question. Sixty of these 173 participants did not meet the study inclusion criteria and were directed to the end of the survey. A total of 113 participants answered the first question indicating they met the study inclusion criteria. However, only 88 participants continued on to answer at least some part of the survey (aside from the first question), with 60 participants completing the entire survey. Therefore, the study sample completing at least a portion of our survey represents 2.61 % of the 3364 genetic counselors certified by the ABGC at the time of the study. The NSGC SDMTF found that in 2010, approximately 8.0 % of 2316 genetic counselors utilized TGC often or always (Cohen et al. 2013). If we use 8.0 % as an estimate of the percentage of genetic counselors utilizing TGC, in our study, an estimated 269 genetic counselors out of 3364 ABGC certified genetic counselors would be expected to use TGC often or always. Therefore, the study population completing at least some part of the survey would represent approximately 32.7 % (88/269) of the genetic counseling population performing TGC.
Participant demographic information is outlined in Table 1. The mean years of overall genetic counseling experience was 11.08, with 10.04 years for IPGC, and 4.85 years for TGC. The majority of the participants were located in NSGC regions 2 and 4, with 38.33 % (23/60) and 21.67 % (13/60), respectively. This is an over-representation of counselors from these regions when compared to the percentage of individuals (49 %) in these two regions found in the NSGC Professional Status Survey (National Society of Genetic Counselors 2014). Three participants out of 63 (4.76 %) had performed IPGC during training only, while a majority 80.9 % (51/63) practiced IPGC prior to and/or concurrently with TGC. Telephone genetic counselors most commonly practiced in commercial diagnostic laboratories (30.1 %; 19/63) or university medical centers (27.0 %; 17/63). They primarily provided reproductive (46.2 %; 30/65), cancer (43.2 %; 28/65) and/or carrier screening services (35.5 %; 23/65). Additionally, 26.2 % (17/65) of participants selected the “other” patient indication category. Participants were not given the opportunity to provide additional information about the “other” category. Respondents reported spending an average of 47.2 min (SD = 18.14; median = 45.00 min), in an IPGC versus an average of 37.3 min (SD = 18.69, median = 35 min) in a TGC session, and this difference was statistically significant, [t(61) = 4.76, p < .001].
Comparison of TGC Versus IPGC
Tasks Performed Differently
Of the 88 genetic counseling tasks analyzed in the survey, 13 (14.8 %) were determined to be performed differently in TGC when compared to IPGC by at least 25 % of respondents (See Table 2). The tasks which the greatest percentages of participants indicated as different included: establishing rapport through verbal and nonverbal interactions (60.2 %; 50/83) and establishing rapport through interpreters (50.0 %; 23/46), both in the Contracting Domain; recognizing factors affecting the counseling interaction (47.8 %; 32/67), assessing client/family emotions, support, etc. (40.9 %; 27/66), and assessing clients’ psychosocial needs and recognizing the need for referral (38.8 %; 26/67), in the Psychosocial Assessment Domain; facilitating genetic testing (40.9 %; 27/66) in the Testing Options Domain; and educating clients about basic genetic concepts (35.6 %; 26/73) in the Inheritance/Risk Counseling Domain. There were no differences identified by at least 25 % of respondents in the following domains: Medical History, Risk Assessment, Test Interpretation/Results Discussion, Psychosocial Support/Counseling, Resources and Follow-up, and Ethical/Legal.
What are the Key Differences and Why do the Differences Exist?
Through open ended questions, we asked the participants to identify what they perceived were the key differences between TGC and IPGC for each domain. If differences were noted, we asked open ended questions to identify why they believed the differences existed. When analyzing the qualitative data from these two questions, three main themes emerged: nonverbal cues, other visual information, and logistical differences.
Theme 1: Nonverbal Cues
Nonverbal communication was identified as a key difference for many of the ABGC Practice Analysis tasks, especially in the domains of Contracting, Pedigree and Family History, Diagnosis and Natural History, Inheritance/Risk Counseling, Testing Options, Test Interpretation, Psychosocial Assessment, and Psychosocial Support and Counseling. Specifically, the participants pointed to the inability to read the patient’s body language and assess nonverbal cues as factors that adversely impacted their ability to build rapport, assess understanding, and make psychosocial assessments. Related to building rapport, one participant stated:
It is a little harder to establish rapport when you can’t see the patient, probably because of the lack of nonverbal cues.
While another, in reference to assessing understanding, said:
I think it’s more difficult to assess the client’s understanding when you can’t see them. I find it easier to do this in person. For chattier clients this isn’t a problem, but for those who are more quiet, I find it tricky.
Another participant noted that it is the psychosocial assessment that is harder, but once the assessment is made, the psychosocial support and counseling are similar.
I feel like the harder part of phone counseling is knowing there IS an emotion going on. When it’s obvious on the phone, I address it almost the same as in person with a couple of exceptions.
Additionally, some individuals commented that the difficulties due to a lack of nonverbal cues were even more apparent when an interpreter was used in a telephone session. To this point, a few participants stated that they did not offer TGC with an interpreter given the inherent barriers to effective communication.
Although most individuals spoke of the lack of verbal cues as impacting the counseling session negatively, a few individuals felt the opposite. For example, one individual commented that some patients may be more open in a TGC session due to an increased feeling of anonymity.
However, other patients are more talkative over the phone and will discuss about more personal issues as it can be seen as an “anonymous” call (men more often than women).
Another noted that speaking to a patient on the telephone might give important clues about the patient’s home life that can be used in a psychosocial assessment.
Sometimes the assessment seems better by phone..... I can hear how much chaos is in the patient’s life. I can hear if there is a person who is saying things in the background that they might not say in the office.
Although we did not specifically ask participants how they addressed any key differences between TGC and IPGC, some provided this information. For instance, several people who identified the absence of nonverbal cues as a difference associated with TGC, described how they modified their counseling approach accordingly. With regard to establishing rapport in the absence of nonverbals, one participant stated:
At the beginning of the conversation I usually explain to the patient that since we are not in the same room I cannot read their non-verbal cues and need them to speak up if they have questions or get confused. I am almost never this blunt during in-person discussions.
To overcome the difficulties in assessing patient understanding without nonverbal cues, another participant stated:
As mentioned previously, counseling when not in person requires much more verbal checking in to ensure and confirm understanding.
While another said:
Evaluating a client’s risk perception and response and modifying counseling requires closer attention to verbal cues in telephone counseling since facial expressions and body language cannot be assessed.
Another, in reference to assessing psychosocial needs, stated:
I have actually said to people “I know this is an emotional topic, and since I can’t see you, I may miss a sign that the information is upsetting to you. This can be helpful information to me, so that we can address your concerns, so please feel free to stop me and tell me if something is upsetting to you.
Other ways counselors modified their counseling included increased recognition of the significance of nonverbal cues (such as long pauses, tone of voice and rate of speech), and utilizing those cues in their assessments. Others indicated they truly listened to their patients’ words rather than making assumptions based on visual cues and used more direct questioning in TGC than they would typically use in an IPGC. One participant illustrated this well by stating:
When there is a silence on the end of the line I have no visual cues to guide me as to why. I have to be more direct and I cannot verify my best guesses with visual corroboration…
Another highlighted that rapport building and patient assessments are possible with increased awareness of the inherent limitations of the TGC model.
The non-verbal communication between the patient and the genetic counselor is certainly different because you rely more on intonation rather than facial expressions or body language. This can be ok, but it is absolutely critical to be aware of this when speaking with a patient on the phone.
Theme 2: Other Visual Information
Aside from the absence of nonverbal cues provided by the patient, there were other differences noted due to the lack of other types of visual cues/information both from the patient and the counselor. Many counselors discussed the difficulty of providing complex information without the use of visual aids such as those traditionally used in IPGC sessions; therefore, several differences were noted among the tasks involving information giving. Specifically, these differences were noted most often in the domains of Diagnosis and Natural History and Inheritance/Risk Counseling. For example, one participant noted how explaining the concept of how genetic disorders can be inherited is more difficult without using visual aids:
…communication is more difficult without being able to use diagrams to explain biological and genetic concepts, so that I can show (i.e. transmission of mutations, hypertrophic heart) and where (a) patient can point out parts of the concepts not understood. It is more difficult to evaluate client perception and comprehension without visual clues and therefore to respond with clarifications or corrections.
The inability to use visual aids also impacted the domain of Family History and Pedigree in this way:
I like to involve the patient in the pedigree taking process and show them what I’m doing, what the symbols mean, etc. For me I feel like this helps engage the patients more in the family history taking and hopefully will elicit more honest and accurate responses. I lose this ability in a telephone consult.
Although most individuals who identified the lack of visual aids as a difference felt it had a negative impact, one individual suggested that perhaps genetic counselors may rely too much on visual aids in their explanations of genetic concepts. This participant stated:
Reliance of [sic] visual aids is a useful tool when available, but not essential and may even be a crutch.
While another spoke of the importance of evaluating how information was delivered in a TGC session.
I worked with a health literacy expert who helped me focus the counseling provided on what really matters to a patient’s decision making.
There were other differences identified in the domain of Family History and Pedigree due to the lack of visual information as well. Specifically, counselors spoke of the need to modify questioning due to the inability to make any kind of visual assessment of ethnicity. One participant spoke about the difficulty of assessing ethnicity over the phone in this way:
Ethnicity can be easier to determine when you can see the patient/client; you may phrase the ethnicity question differently in these cases, such as “would you consider yourself to be African American?” versus just blatantly asking. It may be more difficult to draw these conclusions from telephone counseling, so the question may be more pointed.
Additionally, several counselors spoke of the inability to observe family dynamics in TGC, including one that noted:
In phone counseling you cannot see family members together so rarely have the opportunity to observe family dynamics.
A few others spoke about the limitations of detecting pertinent dysmorphic or other physical features that may inform the differential diagnosis.
Theme 3: Logistical Differences
In addition to the differences between TGC and IPGC as a result of the inability for the patient and counselor to see each other, there were also some other differences due to the actual physical distance between the counselor and patient. Most of these differences seemed to be logistical in nature and involved the domains of Case Preparatory Work, Natural History/Diagnosis, Testing Options, and Resources and Follow Up. More explicitly, these logistical differences included: genetic testing coordination, making support referrals, making management/diagnostic referrals, billing and obtaining records. One participant spoke of the difficulty in creating a management plan and finding local providers for patients that may not be located in an area near themselves:
Development of the management plan varies, as patients who I worked with via phone couns(e)ling may or may not already be in our healthcare system, and so I may not know specific specialists to refer a patient to in his or her area. Typically, I just spoke generally - contact your PCP to help you find an urologist, etc.
Another participant noted the difference in the logistics of genetic testing for TGC patients:
Facilitation of genetic testing is very different with phone counseling because of logistics needed in getting paperwork to the lab for a blood draw and coordinating specimen collection with the patient at another time and usually different location. During in person counseling, I am able to provide/coordinate all of those services at that meeting.
In regards to the domain of Resources and Follow Up, a participant noted the difficulties in making referrals for patients in many different geographical locations:
Referrals and resources are harder when dealing with an expansive geographical network. My patients can be anywhere in the world so I do not know of supports and other providers in many of these areas.
Participants often indicated differences in regards to arranging genetic testing for TGC patients. Some counselors felt less of a direct role in the genetic testing process in TGC because they have to work to arrange genetic testing to occur at a location in the patient’s area rather than in the counselor’s workplace. One participant discussed how this can also add time to follow up with a patient:
Because of distance, have to arrange for blood draw close to home and send kit and prescription - adds more time to follow up.
Additional Skills in TGC
When asked if genetic counselors should be taught additional skills to effectively perform TGC, 53.8 % (35/65) of participants answering this question said “yes.” Participants were then asked to expand on this if they answered “yes.” The majority of answers fell into four different themes: no new specific skills, more exposure to or practice with the TGC SDM in training, more training on performing a psychosocial assessment and building rapport for the TGC SDM specifically, and additional training on explaining concepts without the use of visual aids. Many responses fell into the “no new specific skills” theme due to the participants discussing skills that they felt genetic counselors already had, but needed to utilize in a different way when performing TGC. For example, one participant said:
It’s an enhancement of the same basic skills set. You just have to ask people where they are, who they are with and sometimes how they are feeling (which you might do in person as well).
Participants identified the benefit of having more exposure to TGC during training, such as having a rotation that allowed a trainee to utilize the TGC SDM. One participant noted how this may help trainees better identify the differences between TGC and IPGC:
If possible they should be given the opportunity to do phone counseling in training, so they see if there’s any difference and how to address it.
As discussed previously, performing a psychosocial assessment was identified as being different and it was an area where participants felt genetic counselors could improve these skills for more effective TGC. For example, one participant stated:
Additional training in psychosocial techniques to elicit more verbal engagement is useful for phone GC.
Being able to explain complex genetic concepts by telephone without the availability of visual aids was another common skill participants noted to be unique to TGC compared with IPGC. As one participant suggested:
…train students to develop verbal analogies for genetic concepts rather than just utilizing images.
Discussion
This study investigated perspectives of genetic counselors performing TGC regarding whether there are differences between TGC and IPGC, and if so, why the differences exist. Participants were also asked whether the differences have any implications for training. Of the 88 tasks from the ABGC Practice Analysis addressed in the survey, 13 (14.8 %) were determined to be different based on our criterion (at least 25 % of respondents indicated a task was different). This indicates that overall, the majority of the tasks are perceived as being performed similarly in TGC and IPGC. The tasks that were most different were “establishing rapport through verbal and nonverbal interactions” and “establishing rapport through interpreters” both in the Contracting Domain; “recognizing factors affecting the counseling interaction”, “assessing client/family emotions, support, etc.” and “assessing clients’ psychosocial needs and recognizing the need for referral”, all in the Psychosocial Assessment Domain; “facilitating genetic testing” in the Testing Options Domain; and “educating clients about basic genetic concepts” in the Inheritance/Risk Counseling Domain. The domain with the most differences was Psychosocial Assessment with all four tasks within this domain classified as “Different.”
Both the quantitative data and the qualitative data suggest that many of the tasks identified as different were related to nonverbal communication. Specifically, in the qualitative data, the participants pointed to the limitations in nonverbal communication in a TGC setting impairing the counselor’s ability to perform a psychosocial assessment. Without being able to see patient facial expressions and body language, participants felt that they may miss their patients’ emotional responses. This may result in missed opportunities to perform appropriate short-term client-centered, psychosocial counseling. Building rapport was also commonly described as being more difficult to establish in TGC than IPGC as a result of lack of nonverbal communication. This may result in more impersonal counseling interactions and possibly impact the overall connection the counselor and patient have.
These findings linking nonverbal communication to difficulties making psychosocial assessments and establishing rapport are similar to those identified by genetic counselors performing telephone results disclosures in the Bradbury et al. (2011) study. In that study, genetic counselors were asked to list the perceived disadvantages of results disclosures by telephone. Those genetic counselors listed “more difficult to assess/respond to patient emotions” as a disadvantage for genetic counselors, as well as “less emotional support from genetic counselor” as a perceived disadvantage for patients (Bradbury et al. 2011, p. 129). Other studies, however, have shown that patients report equivalent satisfaction between TGC and IPGC, including in terms of psychological counseling (Baumanis et al. 2009; Platten et al. 2012; Schwartz et al. 2014). This discrepancy may suggest that psychosocial counseling by telephone may just be a perceived disadvantage from the counselor’s point of view and not something the patients feel is lacking in the TGC SDM. Further research on patient psychosocial outcomes in TGC could help to clarify this discrepancy.
In addition to psychosocial assessments and rapport building, participants also identified difficulties assessing client understanding as a result of a lack of nonverbal cues. In the open-ended responses, participants noted often that it is more difficult to assess a patient’s understanding by telephone compared to in person due to the inability to see nonverbal cues indicating confusion or lack of understanding, such as a furrowed brow in a patient’s expression. They felt that this might cause genetic counselors to miss opportunities to provide clarification of complex concepts leading to decreased understanding in the patient. Patient misunderstanding was a patient disadvantage noted by genetic counselors in the Bradbury et al. (2011) study as well. However, two studies, one in cancer genetic counseling and one in prenatal genetic counseling, have not found a difference in patient knowledge between IPGC and TGC (Sangha et al. 2003; Schwartz et al. 2014). This again may suggest that the differences perceived by genetic counselors are more related to their discomfort with the lack of visual cues available in TGC rather than true patient misunderstanding.
Unlike most other tasks, the task “assess client understanding and response” occurs in more than one domain in the ABGC Practice Analysis including specifically Diagnosis/Natural History, Testing Options, and Test Interpretation/Results Discussion. For these tasks, participants noted at least some differences in all domains where they appear. The difference between TGC and IPGC was found to be greatest in the Diagnosis/Natural History domain with 30.2 % feeling the task is performed differently (therefore, meeting our criterion to be defined as “Different”) versus 22 % in the Testing Options domain and 20.6 % in the Test Interpretation/Results Discussion domain. Since we could not analyze any statistical differences between these percentages, it is difficult to interpret these data. However, we might speculate that assessing client understanding (or possibly a counselor’s concerns about patient misunderstanding) during TGC may be dependent on the type of information the counselor is presenting. Further research is needed evaluating a variety of measures of patient knowledge in a variety of clinical indications in a TGC setting to determine if there is really increased patient misunderstanding in TGC or if this is only the genetic counselor’s perception.
Not being able to use visual aids when counseling by telephone was another common theme that emerged in relation to communicating information to patients. Many study participants cited the lack of visual aid use in telephone counseling as making it more difficult to counsel patients by telephone compared to in person. This correlates with the Bradbury et al. (2011) study which showed that the lack of visual aids was perceived as a disadvantage in TGC, as well as with Peshkin et al. (2008) who provided specially designed visual aids to be sent to TGC patients ahead of their appointments. Interestingly, a few participants in the current study stated that not being able to use visual aids in TGC was not a disadvantage necessarily for the patient, but rather, a disadvantage for the counselor in the sense that visual aids may be used more for the counselor’s benefit than for the patient’s. One participant even mentioned that visual aid use may be a “crutch” used by counselors for their own benefit in providing counseling.
Logistical issues were also an area where counselors identified differences in our study. Several counselors specifically identified genetic testing coordination as an area that differed between TGC and IPGC. They spoke of the challenge of not being directly involved in the coordination process and not being able to draw blood at the time of the counseling session. Although none of the counselors in our study spoke specifically of the impact or influence of these logistical issues on their patients, two randomized trials comparing TGC and IPGC have shown lower rates of uptake of genetic testing in patients counseled by telephone (Butrick et al. 2014; Kinney et al. 2014). Butrick et al. (2014), in their discussion of this finding, thought that the disparity might be related to logistical issues since their patients had to follow-up with a phlebotomy clinic or provider in order to have genetic testing performed. Kinney et al. (2014), on the other hand, did not feel that the logistical issues were a large barrier to testing as their patients were allowed to submit buccal samples, which they then sent themselves by mail. Since the counselors in our study did note differences in genetic testing coordination, and there is evidence that the genetic testing uptake rate is affected by TGC, it is important to continue studying this finding in more detail and develop processes that decrease barriers to genetic testing for patients utilizing TGC.
Even though the majority of tasks were identified as similar between the two SDMs, many participants felt that genetic counselors needed to be taught additional skills or how to use their existing skills differently to provide effective TGC SDM. Specifically, many participants suggested tailoring training in psychosocial assessment skills to include asking more direct questions and identifying different nonverbal patient cues (like inflection, pauses or sighing) to determine a patient’s emotional status. Peshkin et al. (2008) took these factors into consideration when designing their randomized non-inferiority trial on TGC. Specifically, they developed genetic counseling “probes” regarding risk perception, test interpretation, medical decision making and family communication that were to be used by the counselor during TGC sessions to elicit information more easily, given the lack of non-verbal cues. Additionally, participants felt that it would be helpful to teach students how to explain complex genetic concepts without the use of visual aids. Finally, many participants felt that providing opportunities to practice using the TGC SDM during training, such as a rotation in a clinic using TGC, would be an effective way to prepare trainees to be able to utilize their skills in this model.
Study Limitations
Our study was designed and intended to be exploratory since thus far, there has been limited information available on how genetic counselors perceive TGC. Our survey instrument has not been validated and much of the data obtained were qualitative. Additionally, there is limited information on the true number of genetic counselors performing TGC. All of these factors make it difficult to generalize the results of this study to all genetic counselors providing TGC. Also, as with any content analysis, there is the possibility of bias when identifying emerging themes in the responses since the process is somewhat subjective. To lessen this effect, all three authors analyzed the data independently and all agreed on the major themes identified. Of note, the themes identified were similar to those previously identified and anticipated by other groups (Bradbury et al. 2011; Peshkin et al. 2008).
Another potential limitation is that although our survey was designed to only include those genetic counselors performing TGC based on the NSGC SDM definition, we cannot say for certain that this occurred. While none of the participants stated explicitly that they were only providing post-test results disclosures by telephone rather than conducting an entire session telephonically, there were some qualitative responses that seemed to infer that this might have been the case. Additionally, the choices provided for the Likert-type questions included three that could be defined as “different” and two that could be defined as “same”. Since participants were given more “different” choices in these questions, this may have led to a skewing of answers towards identifying tasks as “different”. Despite this possibility, the majority of tasks performed in TGC were still identified as being performed the same in IPGC. Therefore, this suggests that the impact of this survey design element may have been minimal. A further limitation is that the length of the survey resulted in participant drop out. Eighty-eight participants answered the first Likert-type question regarding tasks in the Case Preparatory Work domain, while only 66 participants answered the Likert-type question regarding the Ethical/Legal domain (the last domain in our study). Additionally, the length of the survey and the number of open ended questions overall could have affected the quality of the open ended responses received as the survey progressed. The instructions accompanying the survey requested that participants consider differences between TGC and IPGC in general rather than based on differences related to specific patient factors or referral indications. However, given some of the open-ended responses, there appeared to be some counselors that were triaging cases between IPGC and TGC based on indication. These responses suggest that patients with more straightforward and less complicated indications may be preferentially seen more frequently for TGC with the more complicated indications reserved for IPGC. This suggests that some of the differences identified in this study may be due to complexity or type of patient indications rather than true differences between TGC and IPGC. Performing additional research that compares TGC to IPGC for the same patient indication could provide some clarity in this area.
Conclusions
In summary, the majority of ABGC Practice Analysis tasks were identified as being performed similarly in the TGC SDM when compared to the IPGC SDM. We found the majority of the differences between TGC and IPGC fell into the domains of Contracting, Psychosocial Assessment, Testing Options and Inheritance/Risk Counseling. Based on this research, it does not appear that, in general, additional skills are necessary for performing TGC, but that it may be necessary to apply some of the core skills of genetic counseling in different ways to perform effective TGC. From this observation, it appears that the skills taught in genetic counseling training may be sufficient to perform TGC, however, there may be a need for additional training on how to modify these skills to best navigate the limitations inherent to the TGC SDM.
Although other groups (Bradbury et al. 2011; Peshkin et al. 2008) have anticipated and identified genetic counseling needs and practice barriers in TGC previously, this is one of the first studies directly investigating the experiences and perceptions of genetic counselors working in TGC. As TGC practice from the provider’s perspective has not been studied extensively, additional research is necessary to continue exploring this SDM. It would be important to look at the possible factors influencing the counselors’ perceptions of the differences identified in this study including counseling indication, experience in the TGC model, overall clinical experience and TGC practice setting, to name a few. Additional research is also needed to evaluate how these factors and other counselor attributes influence patient outcome measures including knowledge, psychological well-being and satisfaction in the TGC setting. By identifying both patient factors and counselor factors that influence the provision of TGC, we can focus training efforts on improving TGC services for the benefit of the patient receiving these services.
References
Accreditation Council for Genetic Counseling. (2013). Practice-based competencies for genetic counselors. Retrieved from http://www.GCeducation.org/Documents/ACGCPracticeBasedCompetencies_13-Final-Web.pdf. Accessed 29 Apr 2014.
Baumanis, L., Evans, J. P., Callanan, N., & Susswein, L. R. (2009). Telephoned BRCA1/2 genetic test results: prevalence, practice, and patient satisfaction. Journal of Genetic Counseling, 18(5), 447–463. doi:10.1007/s10897-009-9238-8.
Bensend, T. A., McCarthy Veach, P., & Niendorf, K. B. (2013). What’s the harm? Genetic counselors’ perceptions of adverse effects of genetics service provision by non-genetics professionals. Journal of Genetic Counseling, 23, 48–63. doi:10.1007/s10897-013-9605-3.
Bonadies, D., Brierley, K. L., Barnett, R. E., Baxter, M. D., Donenberg, T., Ducaine, W. L., et al. (2014). Adverse events in cancer genetic testing: the third case series. Cancer Journal, 20(4), 246–253. doi:10.1097/PPO.0000000000000057.
Bradbury, A. R., Patrick-Miller, L., Fetzer, D., Egleston, B., Cummings, S. A., Forman, A., et al. (2011). Genetic counselor opinions of, and experiences with telephone communication of BRCA1/2 test results. Clinical Genetics, 79(2), 125–131. doi:10.1111/j.1399-0004.2010.01540.x.
Brierley, K. L., Campfield, D., Ducaine, W., Dohany, L., Donenberg, T., Shannon, K., et al. (2010). Errors in delivery of cancer genetics services: implications for practice. Connecticut Medicine, 4(7), 413–423.
Brierley, K. L., Blouch, E., Cogswell, W., Homer, J. P., Pencarinha, D., Stanislaw, C. L., et al. (2012). Adverse events in cancer genetic testing medical, ethical, legal, and financial implications. Cancer Journal, 18(4), 303–309. doi:10.1097/PPO.0b013e3182609490.
Butrick, M., Kelly, S., Peshkin, B. N., Luta, G., Nusbaum, R., Hooker, G. W., et al. (2014). Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genetics in Medicine. doi:10.1038/gim.2014.125. Advance online publication.
Chen, W. Y., Garber, J. E., Higham, S., Schneider, K. A., Davis, K. B., Deffenbaugh, A. M., et al. (2002). BRCA1/2 genetic testing in the community setting. Journal of Clinical Oncology, 20(22), 4485–4492. doi:10.1200/JCO.2002.08.147.
Cohen, S. A., Gustafson, S. L., Marvin, M. L., Riley, B. D., Uhlmann, W. R., Liebers, S. B., & Rousseau, J. A. (2012). Report from the National Society of Genetic Counselors service delivery model task force: a proposal to define models, components, and modes of referral. Journal of Genetic Counseling, 21(5), 645–651. doi:10.1007/s10897-012-9505-y.
Cohen, S. A., Marvin, M. L., Riley, B. D., Vig, H. S., Rousseau, J. A., & Gustafson, S. L. (2013). Identification of genetic counseling service delivery models in practice: a report from the NSGC service delivery model task force. Journal of Genetic Counseling, 22(4), 411–421. doi:10.1007/s10897-013-9588-0.
Genetests. (2015). Disorders for which genetic tests are available and laboratories offering tests, 1993–2015. Retrieved from https://www.genetests.org/img/content/chart1.png. Accessed 2 Apr 2015.
Graf, M. D., Needham, D. F., Teed, N., & Brown, T. (2013). Genetic testing insurance coverage trends: a review of publicly available policies from the largest US payers. Personalized Medicine, 10(3), 235–243. doi:10.2217/pme.13.9.
Hampel, H., Grubs, R. E., Walton, C. S., Nguyen, E., Breidenbach, D. H., Nettles, S., et al. (2009). Genetic counseling practice analysis. Journal of Genetic Counseling, 18(3), 205–216. doi:10.1007/s10897-009-9216-1.
Helmes, A. W., Culver, J. O., & Bowen, D. J. (2006). Results of a randomized study of telephone versus in-person breast cancer risk counseling. Patient Education and Counseling, 64(1–3), 96–103. doi:10.1016/j.pec.2005.12.002.
Hsieh, H. F., & Shannon, S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi:10.1177/1049732305276687.
Jenkins, J., Calzone, K. A., Dimond, E., Liewehr, D. J., Steinberg, S. M., Jourkiv, O., et al. (2007). Randomized comparison of phone versus in-person BRCA1/2 predisposition genetic test result disclosure counseling. Genetics in Medicine, 9(8), 487–495. doi: 10.1097GIM.0b013e31812e6220.
Kinney, A. Y., Butler, K. M., Schwartz, M. D., Mandelblatt, J. S., Boucher, K. M., & Pappas, L. M. (2014). Expanding access to BRCA1/2 genetic counseling with telephone delivery: a cluster randomized trial. Journal of the National Cancer Institute, 106(12), dju328. doi:10.1093/jnci/dju328.
Lee, J. (2013). Cigna requires genetic counseling. New policy aims to reduce inappropriate testing of at-risk patients. Modern Healthcare, 43(30), 4.
Moyer, V. A. (2014). Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: U.S. preventive services task force recommendation statement. Annals of Internal Medicine, 160(4), 271–281. doi:10.7326/M13-2747.
National Society of Genetic Counselors. (2014). 2014 professional status survey executive summary. Retrieved from http://nsgc.org/p/do/sd/sid=2475&type=0. Accessed 9 Oct 2014.
Peshkin, B. N., DeMarco, T. A., Graves, K. D., Brown, K., Nusbaum, R. H., Moglia, D., et al. (2008). Telephone genetic counseling for high-risk women undergoing BRCA1 and BRCA2 testing: rationale and development of a randomized controlled trial. Genetic Testing, 12(1), 37–52. doi: 10.1089=gte.2006.0525.
Platten, U., Rantala, J., Lindblom, A., Brandberg, Y., Lindgren, G., & Arver, B. (2012). The use of telephone in genetic counseling versus in-person counseling: a randomized study on counselees’ outcome. Familial Cancer, 11(3), 371–379. doi:10.1007/s10689-012-9522-x.
Sangha, K., Dircks, A., & Langlois, S. (2003). Assessment of the effectiveness of genetic counseling by telephone compared to a clinic visit. Journal of Genetic Counseling, 12(2), 171–184.
Schwartz, M. D., Valdimarsdottir, H. B., Peshkin, B. N., Mandelblatt, J., Nusbaum, R., Huang, A. T., et al. (2014). Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. Journal of Clinical Oncology, 32(31), 618–626. doi:10.1200/jco.2013.51.3226.
Sutphen, R., Davila, B., Shappell, H., Holtje, T., Vadaparampil, S., Friedman, S., et al. (2010). Real world experience with cancer genetic counseling via telephone. Familial Cancer, 9(4), 681–689. doi:10.1007/s10689-010-9369-y.
U.S. Preventive Services Task Force. (2005). Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Annals of Internal Medicine, 143(5), 355–361. doi:10.7326/0003-4819-143-5-200509060-00011.
U.S. Preventive Services Task Force. (2014). USPSTF A and B recommendations by date. Retrieved from http://www.uspreventiveservicestaskforce.org/uspstf/uspsdaterecs.htm. Accessed 31 Mar 2014.
Acknowledgments
We would like to thank Rawan Awwad, Whitney Ducaine and Kristen Rauch for their assistance with piloting this survey. We would also like to thank all the genetic counselors that took the time to complete our survey.
Conflict of Interest
Kelly R. Burgess and Angela Trepanier declare that they have no conflict of interest.
Erin P. Carmany has stock options and is a contractor for Informed Medical Decisions, Inc., a provider of telephone genetic counseling services.
Human Studies and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Animal Studies
No animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burgess, K.R., Carmany, E.P. & Trepanier, A.M. A Comparison of Telephone Genetic Counseling and In-Person Genetic Counseling from the Genetic Counselor’s Perspective. J Genet Counsel 25, 112–126 (2016). https://doi.org/10.1007/s10897-015-9848-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-015-9848-2