Abstract
There is tremendous excitement about the promise of new genomic technologies to transform medical practice and improve patient care. Although the full power of genetic diagnosis has not yet been realized, paradigms of clinical decision-making are changing. In fact, recent policy level changes to promote genetic counseling by certified genetics professionals (GP) such as genetic counselors and clinical geneticists, are occurring at both the payer and state level. However, there remain opportunities to develop policies within the United States to: 1) enhance the access to the limited workforce of GPs; 2) revise reimbursement schemes such that costs to deliver these services may be recouped by institutions with GPs; and 3) protect against the potential for discrimination based on genetic information. Although many of these issues predate advances in genomic technologies, they are exacerbated by them, with increasing access and awareness as costs of testing decrease. Consequently, evolving shifts in national policies poise GPs to serve as a hub of information and may be instrumental in facilitating new models to deliver genetics-based care through promoting academic-community partnerships and interfacing with non-GPs. As we acknowledge the potential for genomics to revolutionize medical practice, the expertise of GPs may be leveraged to facilitate incorporation of this information into mainstream medicine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the completion of the human genome project almost a decade ago, there have been tremendous advances in DNA sequencing technologies. To put this into perspective, the first human genome, completed in 2003, cost 2.7 billion dollars to sequence and took over 10 years to complete (Human Genome Sequencing 2004; National Human Genome Research Institute). However, over the last few years, the cost of sequencing a human genome has dropped to less than \$10,000 US and takes a matter of a few weeks to complete (Phimister et al. 2012). Costs are expected to drop below \$1,000 and take just days (potentially hours) to complete, recognizing this does not factor in the time and cost needed for interpretation and return of the results to the patient. As a result of these new sequencing technologies (called ‘next-generation sequencing’), the paradigm for genetic testing is expected to change (see Fig. 1). Specifically, tests through ‘gene panels’ (i.e., tests for multiple genes simultaneously through next generation sequencing) are becoming more common as costs are becoming similar to or even less than testing for just one genetic condition at a time (through use of Sanger sequencing). For example, the ruling in June 2013 by the Supreme Court of the United States, which concluded that genes could not be patented (American Civil Liberties Union 2013), changed the marketplace for inherited cancer and BRCA1 and BRCA2 (BRCA) testing virtually overnight. Prior to the ruling, Myriad Genetics, who held the patent for BRCA, was the only commercial laboratory in the United States offering the test and it was not available as part of a ‘gene panel’. On the day of the ruling, Ambry Genetics launched a new hereditary breast cancer panel containing BRCA (called “BRCAPlus” which in addition to BRCA includes PTEN, TP53, STK11 and CDH1: four high penetrance genes which predispose to breast cancer) for less than list price of BRCA testing through Myriad and added BRCA to several existing panels. The following day, the University of Washington added BRCA to their existing panel of 50 genes (called “BROCA”). Additionally, several other laboratories announced they would also offer similar tests within the year (Karow 2013). Further adding complexity to the genetic testing landscape is the increasing use of exome (i.e., the protein coding regions of the gene) and whole-genome testing. In the future, it is anticipated that ‘gene panels’ may become obsolete as sequencing costs continue to decrease and sequencing a patient’s exome or whole-genome may become a more cost-effective option.
In anticipation of these tremendous technologic advances, the American College of Medical Genetics and Genomics (ACMG) recently issued guidelines pertaining to a minimal list of actionable genes (i.e., 57 genes related to roughly 25 genetic conditions) for which testing should be reported when performing exome or genome sequencing (Green et al. 2013). These genes are associated with conditions that may be unrelated to the indication for ordering the sequencing (thus referred to as “incidental findings”), but knowledge of the abnormal sequence has medical value for patient care. Mutations in these genes have a well-recognized and causative role in the occurrence of disorders that can be prevented or effectively treated. These conditions include hereditary forms of cancer, later-onset cardiac-related syndromes, and connective tissue syndromes.
With the availability of new testing options, there will also be changes in the delivery of genetic risk assessment services. Specifically, the conventional clinical practice paradigm involves gathering information in order to generate a differential diagnosis, after which the appropriate test is ordered in a stepwise manner (i.e., the need for additional testing is determined once results are available). However, plummeting costs of testing are resulting in many genes being tested simultaneously (either through panels of genes focused on a particular cancer type or by exome/genome sequencing). As a result, the need to generate an extensive differential diagnosis and eliminate possible diagnoses using a stepwise genetic testing approach is lessening and clinical practice paradigms appear to be shifting towards a model where a patient is “tested first” (without the need to generate an extensive differential diagnosis based on clinical information) following broad consent. Once results are available, additional information is collected to help interpret the results of the testing and to put the diagnosis into proper clinical context.
It is worth considering that although broad testing without the need to generate a differential diagnosis may make it easier to order comprehensive testing, it will still require proficiency in genetics due to required familiarity with the various gene panel options, choosing the one best suited for each patient, result interpretation, putting the result in proper clinical context, and making appropriate management recommendations. Unlike many tests used in medicine, there is lack of FDA oversight for genetic testing thus test validity and clinical utility may differ substantially between labs. Therefore, there is heightened importance to understand variations in laboratory practices and the meaning of terms, such as analytical sensitivity, reported range, coverage, and variant filtering, when determining whether to perform a disease targeted gene panel, exome, or genome analysis and which laboratory to utilize. Not only will the quality of the result received by the ordering clinician be impacted by the factors outlined above (i.e., analytic sensitivity, filters used, etc.), but also on the ability to interpret the result itself. This is particularly true for conditions, such as those associated with moderate penetrance genes, where national best practices guidelines do not currently exist due to paucity of data. As such, it is anticipated that provision of care based on genetic testing results will become exponentially more complex resulting in an increased need for the involvement of GPs in patient care, an issue already recognized as part of several best practices guidelines from numerous professional guidelines (“ACOG Practice Bulletin No. 103: Hereditary breast and ovarian cancer syndrome” 2009; “National Accreditation Program for Breast Centers” 2013; National Comprehensive Cancer Network 2013; Riley et al. 2012; Robson et al. 2010; Trepanier et al. 2004).
Additionally, this paradigm shift in genetic testing practices will lead to changes in the approach to genetic counseling of patients, recognizing that the optimal approach is currently unknown (Domchek et al. 2013). One approach adopted by the Genetic Risk Assessment Service at the Moffitt Cancer Center includes a pre-test genetic counseling session during which the following is discussed: (1) a brief overview of multiple syndromes in general terms with discussion of specific conditions for which the patient may be at risk based on personal and/or family history, (2) discussion of high penetrance genes (which generally impart a 5–10 fold risk of cancer and may impact medical management, thus are often “medically actionable”) versus moderate penetrance genes (which generally impart a 2–4 fold risk of cancer, thus may not impact medical management), and (3) communication that with testing of multiple genes simultaneously, there is a higher chance that the patient will receive a variant of uncertain significance (VUS) result. A detailed discussion of specific conditions is deferred to the post-test session, during the disclosure of genetic test results. Thus, there currently remains a tremendous need to develop and refine new genetic counseling strategies to deliver genetic testing services to manage population needs particularly as use of genomic testing technologies continues to increase.
In addition to the clinical setting, other non-clinical settings which may benefit from inclusion of GPs is the laboratory setting and entities involved in formation of policies at the state or payer level. The value of genetic counselors (GCs) in the laboratory setting was illustrated through a study reported by ARUP laboratories (ARUP Laboratories 2011) where substantial cost savings of genetic testing was reported when GCs reviewed indications for testing and interfaced with ordering providers to ensure appropriate and cost-effective testing practices were followed. In fact, the GCs identified and cancelled or changed inappropriately ordered genetic tests for an average cost savings of \$36,500 per month, representing approximately 30 % of all complex genetic tests ordered. Among the most frequent mistake was an order for complete sequencing of a gene when a familial mutation was known. In addition to these contributions in the pre-test phase, GCs in the laboratory setting have the opportunity to assist with interpretation and communication of test results (particularly those that are less straightforward, such as VUS) as well as the provision of decision support for low/moderate penetrance genes.
Consequently, there are a multitude of settings in which GPs can facilitate the incorporation of genomic testing advances that impact cost-effective patient care. In fact, pertaining to the role of GCs in the formation of policies, there are examples in which GCs have influenced statewide and health insurance policies (Duquette et al. 2012) as well as through development of health insurer payer policies (as further outlined in the reimbursement section). Ultimately, there exist many system-level factors to consider when considering how policies may impact the delivery of genetic counseling and testing services by GPs, as outlined in the next section.
Overview of System-Level Factors Which Impact the Delivery of Services by GPs
There are a number of factors to consider that may impact services delivered by GPs, including: A) access to services; B) reimbursement for services rendered; and C) concerns regarding insurance discrimination based on genetic information.
-
A.
Access
National data indicates there are almost 3,200 GCs certified through the American Board of Genetic Counseling, of which 2,500 practice in the United States, translating to 8.1 genetic counselors per 1 million population (Benkendorf 2007). In contrast, as of November, 2007, there were only 1,253 board-certified clinical geneticists and the numbers have remained stagnant as young physicians are not entering the field (American College of Medical Genetics - Careers in Medical Genetics; Institute of Medicine 2009). Of these, an estimated 1,100 were actively practicing and spending on average ~45 % of their time seeing genetics patients (Benkendorf 2007). Extrapolating to full time equivalent (FTE) devoted to clinical effort, this translates to 1.8 clinical geneticists per million population, which is low in comparison to the “ideal” ratio of 4 per 1 million people proposed by the Royal College of Physicians (Benkendorf 2007; Institute of Medicine 2009). Furthermore, the shortage in the GP workforce is disproportionately distributed with rural areas facing the most severe shortages as well as in certain states, where there are wide variations in numbers (Table 1) (Acheson et al. 2005; Vig et al. 2009).
As a means to improve access to GPs, the ACMG has focused efforts to increase information about the profession through development of informational material (American College of Medical Genetics - Careers in Medical Genetics). Similarly, to accommodate increasing demand for GPs, the number of genetic counseling training programs in North America has increased from 18 accredited programs in 1993 to 32 current programs in 2013 with full accreditation and another 3 provisional programs (which are new thus have not yet graduated any students) (Accreditation Council for Genetic Counseling; Institute of Medicine 2009). Together these programs graduate about 3,000 students each year (American Board of Genetic Counseling). The profession is growing rapidly with the number of certified genetic counselors increasing over 400 % since the early 1990s (Association of Genetic Counseling Program Directors). Another means by which access of patients to a certified GC may be enhanced is the existence of title protection, without which anyone in that state can refer to themselves as a GC, including those who have not graduated from a training program accredited by the Accreditation Council for Genetic counseling (Accreditation Council for Genetic Counseling; American Board of Genetic Counseling). Thus, a healthcare provider could unknowingly refer a patient to a provider without graduate training in genetic counseling who calls themselves a GC. In fact, licensure for GCs continues to be adopted by an increasing number of states (National Society of Genetic Counselors) and all fifteen states that currently have licensure for GCs provide title protection.
The issue of access is significant as the demand for genetic testing continues to rise due to an increased number of conditions for which a genetic cause is identified coupled with plummeting costs made possible by next-generation sequencing technologies. Moreover, the awareness of and requests for testing for BRCA mutations has been on the rise in part due to numerous celebrities disclosing they carry a mutation, most notably the recent disclosure of Angelina Jolie that she carries a BRCA mutation having worldwide impact (Jolie 2013). As such, GPs are ideally poised to help lead the integration of new genetic and genomic knowledge and skills into clinical practice. Thus, expansion in access to genetics expertise will be a key component to realizing the benefits of genetics and genomics innovations.
-
B.
Reimbursement
Another strategy that could help increase the GP workforce is to revise reimbursement schemes. Most Cancer Genetic Risk Assessment (CGRA) services cost more to administer than the direct revenue they generate (McPherson et al. 2008) as most GCs cannot typically bill insurers independently for services rendered. This recognition of the lack of reimbursement for genetic services delivered by GCs coupled with data to suggest that provision of genetic counseling through a trained genetics professional can lead to increased cost effectiveness and enhance quality of care (ARUP Laboratories 2011; Pal et al. 2013a, b; Plon et al. 2011; Senter et al. 2013) is beginning to influence policy shifts at the state and payer level. In fact, one of the most successful models to influence policy within the state has been through the Michigan Cancer Genomics Program. This program includes multiple partners representing national organizations, state government and state comprehensive cancer control, state and local cancer registrars, clinical cancer genetics providers, payers, community partners and others. This integrated effort is led by GCs based in the Michigan Department of Health who have brought together a diverse group of stakeholders to provide education and awareness and influence policy-level changes. In fact, despite the great challenges posed by the US healthcare system due to multiple unconnected payer and provider networks, this program was successfully able to increase the number of health plans with a written policy aligned with the USPSTF Grade B BRCA Recommendation from 4 to 11 within a 3 year period (2008–2011) (Duquette et al. 2012). This was accomplished through multiple methods including surveillance, education, federal and state policies, partnerships, and dissemination of information. In fact, one facet of the Michigan Cancer Genomics program that enhanced access to GPs was a policy adopted by a Michigan-based insurer, Priority Health.
Priority Health was one of the first insurers to require genetic counseling by a certified GP either in person (through traditional “face-to-face” appointments) or by telephone before genetic testing for inherited cancer predisposition may be ordered. This policy was implemented to: 1) enhance identification of members at high risk for familial cancer syndromes; 2) ensure education and adequate informed consent for clients; and 3) ensure appropriate testing and follow-up. Through telephone counseling, access to GPs is increased as there is no need to travel for an in-person appointment, regardless of distance to the closest in-person option to access a GP. Part of the policy change at Priority Health included the recognition and addition of the CPT code, 96040, to the provider fee schedule. This code was designated for use by certified GCs (based at institutions across the state) to bill for in-person and telephone genetic counseling services based on length of time of the counseling, and was reimbursed regardless of distance to the closest in-person GP. These genetic counseling code fees are comparable to other ancillary healthcare providers such as Physical/Occupational/Speech/Respiratory therapies. The cost associated with payment of this code was deemed to be insignificant in comparison to the expected benefits associated with the counseling such as decreases in inappropriate testing, reduction of patient anxiety, and referral to appropriate screening for early detection and, in some cases, significant reduction of cancer incidence when prophylactic surgeries are chosen by members. This policy also demonstrates the expanding role of GCs as it was developed by a board-certified genetic counselor who develops this payer’s policies on all emerging technologies (K.L, co-author). Interestingly, the Michigan program has demonstrated that increased reimbursement and increased access has led to an increased use of cancer genetic counseling services with an increase from 8 CGRA clinics staffed by GPs in 2011 to 17 in 2013 (Duquette et al. 2012).
More recently, shifts in payer policies are continuing as more insurers reimburse for genetic counseling when provided by a certified GC or geneticist. As of September 16, 2013, Cigna became the first major U.S. insurer to require customers who were eligible for some types of genetic testing (hereditary breast and ovarian cancer, Hereditary colorectal cancer, and Long QT syndrome, a genetic arrhythmia) to be counseled by a board-certified GC or clinical geneticist unaffiliated with Cigna prior to undergoing testing. Recognizing that an estimated 20 % of BRCA tests are ordered inappropriately, coupled with the realization that genetic counseling costs substantially less than many genetic tests, Cigna developed this policy to reduce inappropriate utilization and limit some of the anxiety and physical harm that may occur when a patient receives inappropriate genetic testing (Lee 2013). Although this policy provides reimbursement for in person genetic counseling by a certified genetic counselor, it differs from the approach taken by Priority Health. Specifically, telephone counseling currently appears to only be reimbursed by Cigna when it is conducted by one commercial company (InformedDNA) (Cigna) through an exclusive agreement, thus may represent a monopoly in the provision of telephone counseling services. Thus, this policy may limit Cigna’s goals to minimize conflict of interest between GPs and the genetic testing laboratory through requirement of the involvement of an independent genetics professional (Cigna). Additionally, the individual providing the telephone counseling at this commercial company may not be familiar with support and medical resources available in the member’s community, which may impact follow-up and ongoing care for patients.
Other approaches to reform public and private healthcare policy and coverage to address gaps in insurance coverage for genetic/genomic analyses is their inclusion as a component of preventive care, which may improve reimbursement relative to the time required to provide adequate CGRA services. There has been some shifts in policy in this area, but it has been limited. For example, under the Affordable Care Act (ACA), otherwise known as healthcare reform, most insurance companies now must cover genetic counseling and testing for BRCA for women at higher risk (as defined by the United States Preventive Services Taskforce (USPSTF)) (“Genetic Risk Assessment and BRCA Mutation Testing for Breast and Ovarian Cancer Susceptibility” 2013), at no cost to patients (Centers for Medicare and Medicaid Services 2013). However, even this policy has its barriers, as genetic counseling for other hereditary cancer syndromes is not included in the act. Additionally, this coverage only applies to a limited population; for example, men do not fall under this provision of the ACA as the USPSTF has not recommended testing for them (due to a lack of studies focused on these men which is required to generate evidence-based recommendations). Such mandates that require coverage of genetic testing are rare.
Additional policy-level approaches include the incorporation of genetic counseling as an essential health benefit within state health plans which will lead to increased reimbursement. As part of the ACA, states are responsible for determining their essential health benefits (National Conference of State Legislatures 2012). Most states have chosen a benchmark plan that serves as the standard of what benefits must be covered, however many states have created supplemental mandates, such as mental health coverage. Therefore, individuals have the ability to communicate with their elected representatives to express their preferences for mandates in the law. Thus, it is very important that stakeholders (which include GPs) be familiar with development of health benefits in their state and to inform policy makers on the reasons coverage of these services is important.
-
C.
Discrimination based on Genetic Test Results
Fear of discrimination has previously been cited as a factor which may hinder patients from seeking genetic testing through a GP (National Partnership for Women and Families on behalf of the Coalition for Genetic Fairness 2004). However in 2008, Congress passed the Genetic Information Non-Discrimination Act (GINA) to help alleviate public fears of discrimination. GINA protects against discrimination based on genetic information in individual and group health insurance as well as in certain workplaces (Leib et al. 2008). However, there remains limited public awareness about this law as evidenced by a 2010 phone survey of Michigan adults, in which only 13.3 % were aware of GINA (McClosky et al. 2011). Therefore, there is a need to increase awareness of existing laws that provide protection against discrimination in order to encourage more patients to seek out information from GPs.
While educational efforts regarding legal protections against genetic discrimination are an essential piece of increasing use of GPs, gaps in existing law must also be addressed in order to help alleviate fear of individuals considering genetic testing. GINA protects against many forms of health insurance discrimination, but does not cover Tricare (healthcare for the military), the Indian Health Service, and the Federal Employees Health Benefits Plans. Furthermore, protection of employees by GINA is limited to state and local governments and private employers with 15 or more employees. Moreover, GINA covers only some federal employees (Baruch and Hudson 2008). Additionally, GINA only provides protections in health insurance and employment and does not cover life insurance, disability insurance, long-term care, or other supplemental insurances which are not strongly regulated by the states. States are increasingly passing legislation to address life and disability insurance protections (Vorhaus 2011), but no such protections are in place at the national level. Without adequately addressing these fears, individuals may still opt to not seek out a GP or genetic testing for fear of losing access to these supplemental insurances. Currently, 24 states have laws that regulate life, long-term care, or disability insurances. However, most of these state laws only regulate how genetic information is used by the companies, but they do not ban the use overall.
The most comprehensive legislation to date was passed in California in 2012 (Senate Bill No. 559, referred to as CalGINA (California Genetic Information Nondiscrimination Act)). By adding genetic information as a protected class under the Unruh Civil Rights Act, this law bans certain forms of discrimination based on genetic information in all businesses whatsoever (Wagner 2011). Other states are also moving to pass more comprehensive laws regarding genetic privacy. However, these laws currently create only a patchwork of protections across the states. This is especially concerning because genetic information is inherently familial. If an individual living in one state has different privacy and anti-discrimination rights than his relative in another state, this minimizes the effect of state laws. Thus, patients seeking genetic testing continue to face risks of discrimination in certain circumstances.
Ultimately, despite some progress towards protecting against genetic discrimination, there remains a need to address this issue more comprehensively. As it currently stands across most of the country, a life, disability, or long-term care insurer can deny an individual insurance if the company can show actuarial justification (i.e., the demonstration that premiums collected are reasonable and proportional to the distribution of their expected costs among policy holders) or risk of increased cost based on genetic information. Thus, some patients embarking on genetic testing continue to face risks of discrimination in certain circumstances, and discussion about this issue prior to testing is required to obtain informed consent. As we anticipate the increasing use of genetic testing across the population due to decreasing costs and increasing awareness, there is a need to address the deficiencies in existing laws that protect against discrimination based on genetic testing through federal legislation.
Solutions to Enhance the Reach of GPs
While recognizing that the physician referral model works well in settings with access to trained GPs, there are many rural areas where such professionals are not readily available (Acheson et al. 2005; MacDonald et al. 2010; Vig et al. 2009). Furthermore, there remain great fluctuations in the access to GPs across states, as illustrated in Table 1 which shows the wide variations in numbers of GPs per 1 million population across the ten most populous states. However, innovative approaches to delivering quality genetics services to an increasing number of patients in community settings have been demonstrated through establishing academic-community partnerships that focus on collaboration with non-genetics providers to offer genetic testing for hereditary cancers (Cohen et al. 2009; MacDonald et al. 2010). These collaborative partnerships increase the reach of GPs and enhance the delivery of GCRA services through leveraging the expertise of GPs for challenging cases yet enabling patients to remain in their community, allowing them better access to resources for long-term follow-up care. In fact, a recent study conducted through a community hospital in Indianapolis, Indiana, reported that collaboration between GPs and non-GPs to provide genetic risk assessment resulted in a 4-fold increase in the number of patients who accessed genetic counseling as compared to the prior year (Cohen and McIlvried 2013). Thus, a possible efficient solution to further increasing access to care may be expanding such models to include reimbursable, telephone counseling conducted by the GPs familiar with the community and its resources. As the genetic counseling and testing landscape continues to evolve, it will be important to assess how insurance policies which reimburse for telephonic counseling (such as Priority Health and Cigna) may promote these types of partnerships.
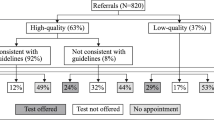
Another example of this type of partnership is the Florida-based Inherited Cancer Research Initiative (ICARE) through which an infrastructure to support research, education, and outreach initiatives focused on BRCA genetic counseling and testing was initiated in 2010, funded through an external peer-reviewed grant. Recognizing the limited number of GPs statewide (as illustrated in Table 1), a network of providers (including both GPs and non-GPs, called ‘ICARE Partners’) was developed who offer BRCA testing services across the state. Education and outreach about inherited cancer predisposition is provided to ICARE Partners by the ICARE study team with the overarching goal of enhancing the provision of genetic services across the state. In fact, contact has been established with 121 healthcare providers since 2010, with dissemination of over 10,000 brochures to date. In addition to educational and outreach efforts, ICARE Partners refer high risk patients to the research registry to provide the research link. This referral mechanism, in turn, has contributed to the tremendous growth of the registry since initiation of the grant in summer 2010 with over 800 BRCA carriers recruited to date.
Specific educational resources available to ICARE Partners include access to:
-
1)
Bi-Monthly Case Conferences: 1 h web-based teleconferences led by a board-certified clinical geneticist and genetic counselors (who are part of the ICARE team) during which brief educational updates are provided in the first 15 min, after which 3–4 clinical cases are presented, including reason for referral, review of the pedigree including differential diagnosis, risk assessment, testing options, and management plan. Each case includes discussion items and a take home message. As shown in Fig. 2, there has been a steady increase in attendance at case conference from unique sites since 2010.
-
2)
Resource Guide to facilitate delivery of CGCT services: A booklet was developed to consolidate specific items that providers might find helpful when offering genetic testing services, informed by questions consistently posed to GPs by outside non-GP healthcare providers. The booklet has 4 sections as follows: I. Guidelines for service delivery; II. Available training opportunities in inherited cancer predisposition; III. Materials to facilitate service delivery; and IV. Insurance-related concerns. This booklet was developed in response to needs voiced by local community-based providers who requested assistance and shadowing experiences through the Moffitt-based Genetic Risk Assessment Service in order to increase their familiarity with genetic testing for hereditary cancer predisposition. Its purpose is to provide an overview of the aspects with which providers should be familiar, when delivering these specialized services as well as to provide guidance about cases in which it may be valuable to draw upon the expertise of a GP.
-
3)
Inherited Cancer Registry newsletter: This is a bi-annual 4-page newsletter that briefly outlines recent clinical and research updates pertaining to risk assessment, testing options and management of those with inherited cancer predisposition. Also included within the newsletter is a section on statewide clinical trials for those with inherited cancer, as personalized treatments based on germline mutations are often only available at a small number of study sites. The newsletter is a means by which updated information is disseminated to healthcare providers and patients who participate in the research registry (Newsletters are available at the ICARE website, which can be accessed through: https://doi.org/www.inheritedcancer.net).
-
4)
Access to ICARE-based experts for inquiries: A dedicated telephone line and e-mail address have been established to provide centralized access to healthcare providers requesting information about our services. This infrastructure has facilitated access for providers across the state to seek input from GPs, when faced with complicated patients. This service is provided by a board-certified GC whose specific role is to give a description of resources available through our efforts as well as general guidance pertaining to hereditary cancer predisposition to ICARE partners.
Conclusions
Within the oncology care setting, there is great excitement as advances in genomic medicine lead to personalized cancer treatment (Dancey et al. 2012). These advances serve as an example of how genomics could impact all disciplines and contribute to the transformation of healthcare as it becomes part of mainstream medicine. As a result of these exciting advances in conjunction with data that consistently demonstrate that most healthcare providers have limited knowledge and inadequate training to make appropriate use of genomic advances (Baars et al. 2005; Giardiello et al. 1997; Grosse and Khoury 2006; Wideroff et al. 2005; Wilkins-Haug et al. 2000), GPs are poised to serve as a hub of information. Yet, there remain several barriers to expanding their role and reach, including: 1) a limited workforce of GPs; 2) gaps in reimbursement schemes with resulting inability to recoup direct costs for services rendered; and 3) consumers fears of genetic discrimination due to limited awareness of GINA coupled with gaps in anti-discrimination laws. As such, the roles of both clinical and nonclinical GPs must continue to evolve to meet provider and societal needs.
Clinically, GPs are poised to expand their role by serving as part of a multi-disciplinary team, expanding their reach through electronic media and becoming increasingly available for provider guidance and consultation. Nonclinically, GC role expansion is similar but involves positions at laboratories and entities involved in policy formation, roles which are essential if the services offered by their clinical colleagues’ skills are to be optimized, both in terms of cost effective practices and delivery of high quality gene-based care. Regardless of the work setting, GPs may act as a hub of genetic knowledge, providing information and guidance to consumers, providers, and policy makers to ultimately reduce barriers and increase access to genetic services.
References
American College of Obstetricians and Gynecologists; ACOG Committee on Practice Bulletins--Gynecology; ACOG Committee on Genetics; Society of Gynecologic Oncologists (2009). ACOG Practice Bulletin No. 103: hereditary breast and ovarian cancer syndrome. Obstetrics and Gynecology, 113(4), 957–966.
Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility. (2013). U.S. Preventive Services Task Force. https://doi.org/www.uspreventiveservicestaskforce.org/uspstf/uspsbrgen.htm. Accessed 18 July 2013.
Accreditation Council for Genetic Counseling. Genetic counseling programs. https://doi.org/gceducation.org/Pages/Accredited-Programs.aspx. Accessed 16 Sept 2013.
Acheson, L. S., Stange, K. C., & Zyzanski, S. (2005). Clinical genetics issues encountered by family physicians. Genetics in Medicine, 7(7), 501–508.
American Board of Genetic Counseling. How do I train to become a certified genetic counselor? https://doi.org/www.abgc.net/Certification/become_a_genetic_counselor.asp. Accessed 25 June 2013.
American Board of Genetic Counseling. https://doi.org/www.abgc.net/ABGC/AmericanBoardofGeneticCounselors.asp. Accessed 4 Sept 2013.
American Civil Liberties Union. (2013). BRCA FAQs. https://doi.org/www.aclu.org/free-speech/brca-faqs. Accessed 29 Sept 2013.
American College of Medical Genetics. Careers in medical genetics. https://doi.org/www.acmg.net/ACMG/Education/Careers_in_Genetics/ACMG/Education/Careers_in_Genetics.aspx?hkey=547e8cff-b2c9-4157-84b4-eae56e56120b. Accessed 4 Sept 2013.
ARUP Laboratories. (2011). Value of genetic counselors in the laboratory. https://doi.org/www.aruplab.com/files/resources/genetics/White-paper-1-value-of-GCs-in-lab.pdf. Accessed 10 Jan 2013.
Association of Genetic Counseling Program Directors. Who…are genetic counselors. https://doi.org/www.nsgc.org/portals/0/program%20directors/genetic%20counselors%20v3.pdf. Accessed 16 Sept 2013.
Baars, M. J., Henneman, L., & Ten Kate, L. P. (2005). Deficiency of knowledge of genetics and genetic tests among general practitioners, gynecologists, and pediatricians: a global problem. Genetics in Medicine, 7(9), 605–610.
Baruch, S., & Hudson, K. (2008). Civilian and military genetics: nondiscrimination policy in a post-GINA world. American Journal of Human Genetics, 83(4), 435–444.
Benkendorf, J. (2007). The medical genetics workforce: Getting to where we need to be from here. https://doi.org/oba.od.nih.gov/oba/SACGHS/meetings/Nov2007/benkendorf.pdf. Accessed 4 Sept 2013.
Centers for Medicare & Medicaid Services. (2013). Affordable care act implementation FAQ - Set 12. https://doi.org/www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/aca_implementation_faqs12.html. Accessed 16 Sept 2013.
Cigna. Genetic Testing and Counseling Program. https://doi.org/www.cigna.com/healthcare-professionals/resources-for-health-care-professionals/genetic-testing-and-counseling-program. Accessed 29 Sept 2013.
Cohen, S. A., & McIlvried, D. E. (2013). Improving access with a collaborative approach to cancer genetic counseling services: a pilot study. Community Oncology, 10(8), 227–234.
Cohen, S. A., McIlvried, D., & Schnieders, J. (2009). A collaborative approach to genetic testing: a community hospital’s experience. Journal of Genetic Counseling, 18(6), 530–533.
Dancey, J. E., Bedard, P. L., Onetto, N., & Hudson, T. J. (2012). The genetic basis for cancer treatment decisions. Cell, 148(3), 409–420.
Domchek, S. M., Bradbury, A., Garber, J. E., Offit, K., & Robson, M. E. (2013). Multiplex genetic testing for cancer susceptibility: out on the high wire without a net? Journal of Clinical Oncology, 31(10), 1267–1270. doi:https://doi.org/10.1200/jco.2012.46.9403.
Duquette, D., Lewis, K., McLosky, J., & Bach, J. (2012). Using core public health functions to promote BRCA best practices among health plans. Public Health Genomics, 15(2), 92–97. doi:https://doi.org/10.1159/000334267.
Giardiello, F. M., Brensinger, J. D., Petersen, G. M., Luce, M. C., Hylind, L. M., Bacon, J. A., et al. (1997). The use and interpretation of commercial APC gene testing for familial adenomatous polyposis. New England Journal of Medicine, 336(12), 823–827.
Green, R. C., Berg, J. S., Grody, W. W., Kalia, S. S., Korf, B. R., Martin, C. L., et al. (2013). ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genetics in Medicine, 15(7):565–574.
Grosse, S. D., & Khoury, M. J. (2006). What is the clinical utility of genetic testing? Genetics in Medicine, 8(7), 448–450.
Human Genome Sequencing, C. (2004). Finishing the euchromatic sequence of the human genome. Nature, 431(7011), 931–945. https://doi.org/www.nature.com/nature/journal/v431/n7011/suppinfo/nature03001_S1.html.
Institute of Medicine. (2009). Innovations in service delivery in the age of genomics: Workshop summary. Washing, D.C.: The National Academies Press.
Jolie, A. (2013). My medical choice. https://doi.org/www.nytimes.com/2013/05/14/opinion/my-medical-choice.html?_r=0. Accessed 18 July 2013.
Karow, J. (2013). Competition for Myriad heats up as US testing labs launch BRCA tests, hereditary cancer panels. https://doi.org/www.genomeweb.com/sequencing/competition-myriad-heats-us-testing-labs-launch-brca-tests-hereditary-cancer-pan. Accessed 18 July 2013.
Lee, J. (2013). Cigna to require counseling prior to some genetic tests. https://doi.org/www.modernhealthcare.com/article/20130725/NEWS/307259958/cigna-to-require-counseling-prior-to-some-genetic-tests. Accessed 26 July 2013.
Leib, J. R., Hoodfar, E., Haidle, J. L., & Nagy, R. (2008). The new genetic privacy law. Community Oncology, 5(6), 124–127.
MacDonald, D. J., Blazer, K. R., & Weitzel, J. N. (2010). Extending comprehensive cancer center expertise in clinical cancer genetics and genomics to diverse communities: the power of partnership. Journal of the National Comprehensive Cancer Network, 8(5), 615–624.
McClosky, J., Anderson, B., & Fussman, C. (2011). Genetic testing and the genetic non-discrimination act. Michigan BRFSS surveillance brief https://doi.org/www.michigan.gov/documents/mdch/MIBRFSS_Surveillance_Brief_Sept_2011_Vol5No4_FINAL_365644_7.pdf. Accessed 19 June 2013.
McPherson, E., Zaleski, C., Benishek, K., McCarty, C. A., Giampietro, P. F., Reynolds, K., et al. (2008). Clinical genetics provider real-time workflow study. Genetics in Medicine, 10(9), 699–706.
National Accreditation Program for Breast Centers. (2013). Genetic evaluation and management (page 48). Retrieved June 15, 2013.
National Comprehensive Cancer Network. (2013). Genetic/familial high-risk assessment: Breast and ovarian V.2.2013. https://doi.org/www.nccn.org/professionals/physician_gls/recently_updated.asp. Accessed 26 Apr 2013.
National Conference of State Legislatures. (2012). State health insurance mandates and the PPACA esential benefits provisions. Retrieved June 19, 2013, from https://doi.org/www.ncsl.org/issues-research/health/state-ins-mandates-and-aca-essential-benefits.aspx.
National Human Genome Research Institute. The human genome project completion: Frequently asked questions. https://doi.org/www.genome.gov/11006943. Accessed 6 Sept 2013.
National Partnership for Women and Families on behalf of the Coalition for Genetic Fairness. (2004). Faces of genetic discrimination: How genetic discrimination affects real people. https://doi.org/www.nationalpartnership.org/site/DocServer/FacesofGeneticDiscrimination.pdf. Accessed 19 June 2013.
National Society of Genetic Counselors. States issuing licenses for genetic counselors. https://doi.org/www.nsgc.org/Advocacy/StatesIssuingLicensesforGeneticCounselors/tabid/347/Default.aspx. Accessed 15 June 2012.
Pal, T., Cragun, D., Lewis, C., Doty, A., Rodriguez, M., Radford, C., et al. (2013a). A statewide survey of practitioners to assess knowledge and clinical practices regarding hereditary breast and ovarian cancer. Genetic Testing and Molecular Biomarkers. doi:https://doi.org/10.1089/gtmb.2012.0381.
Pal, T., Lee, J. H., Besharat, A., Thompson, Z., Monteiro, A. N., Phelan, C., et al. (2013b). Modes of delivery of genetic testing services and the uptake of cancer risk management strategies in BRCA1 and BRCA2 carriers. Clinical Genetics. doi:https://doi.org/10.1111/cge.12130.
Phimister, E. G., Feero, W. G., & Guttmacher, A. E. (2012). Realizing genomic medicine. New England Journal of Medicine, 366(8), 757–759. doi:https://doi.org/10.1056/NEJMe1200749.
Plon, S. E., Cooper, H. P., Parks, B., Dhar, S. U., Kelly, P. A., Weinberg, A. D., et al. (2011). Genetic testing and cancer risk management recommendations by physicians for at-risk relatives. Genetics in Medicine, 13(2), 148–154. doi:https://doi.org/10.1097/GIM.0b013e318207f564.
Riley, B. D., Culver, J. O., Skrzynia, C., Senter, L. A., Peters, J. A., Costalas, J. W., et al. (2012). Essential elements of genetic cancer risk assessment, counseling, and testing: updated recommendations of the National Society of Genetic Counselors. Journal of Genetic Counseling, 21(2), 151–161. doi:https://doi.org/10.1007/s10897-011-9462-x.
Robson, M. E., Storm, C. D., Weitzel, J., Wollins, D. S., & Offit, K. (2010). American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. Journal of Clinical Oncology, 28(5), 893–901. doi:https://doi.org/10.1200/jco.2009.27.0660.
Senter, L., O’Connor, M., Oriyo, F., Sweet, K., & Toland, A. (2013). Linking distant relatives with BRCA gene mutations: potential for cost savings. Clinical Genetics. doi:https://doi.org/10.1111/cge.12211.
Trepanier, A., Ahrens, M., McKinnon, W., Peters, J., Stopfer, J., Grumet, S. C., et al. (2004). Genetic cancer risk assessment and counseling: recommendations of the national society of genetic counselors. Journal of Genetic Counseling, 13(2), 83–114.
Vig, H. S., Armstrong, J., Egleston, B. L., Mazar, C., Toscano, M., Bradbury, A. R., et al. (2009). Cancer genetic risk assessment and referral patterns in primary care. Genetic Testing and Molecular Biomarkers, 13(6), 735–741.
Vorhaus, D. (2011). Considering the impact of yet another proposal for genetic legislation. Retrieved June 19, 2013, from https://doi.org/www.genomicslawreport.com/index.php/2011/03/23/ca-proposal-for-genetic-legislation/.
Wagner, J. K. (2011). A new law to raise GINA’s floor in California. https://doi.org/www.genomicslawreport.com/index.php/2011/12/07/a-new-law-to-raise-ginas-floor-in-california/. Accessed 19 June 2013.
Wideroff, L., Vadaparampil, S. T., Greene, M. H., Taplin, S., Olson, L., & Freedman, A. N. (2005). Hereditary breast/ovarian and colorectal cancer genetics knowledge in a national sample of US physicians. Journal of Medical Genetics, 42(10), 749–755.
Wilkins-Haug, L., Erickson, K., Hill, L., Power, M., Holzman, G. B., & Schulkin, J. (2000). Obstetrician-gynecologists’ opinions and attitudes on the role of genetics in women’s health. Journal of Women’s Health & Gender-Based Medicine, 9(8), 873–879.
Acknowledgments
Sincere appreciation is expressed to Debra Duquette, MS, CGC, Michigan Department of Community Health, Lansing, MI for her input and guidance. This work was supported in part by an external peer-reviewed research grant through Florida Biomedical (IBG09-34198).
Disclosures of interest
Cristi Radford is a full-time employee of the commercial laboratory Ambry genetics. Karen Lewis is a full-time employee of the Michigan-based health insurer, Priority Health. Anya Prince and Tuya Pal declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Radford, C., Prince, A., Lewis, K. et al. Factors Which Impact the Delivery of Genetic Risk Assessment Services Focused on Inherited Cancer Genomics: Expanding the Role and Reach of Certified Genetics Professionals. J Genet Counsel 23, 522–530 (2014). https://doi.org/10.1007/s10897-013-9668-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-013-9668-1