Abstract
The field of cancer genetics is evolving rapidly, and much has changed over the past ten years in the way services are being provided and by whom they are being provided. We recount here our experience with the evolution of cancer genetic services in a community setting, focusing on collaboration with non-genetics providers to offer genetic testing for hereditary cancer. This approach allows for the most effective use of genetic counselors’ expertise for challenging cases, and enables the patient to remain within their community to allow for better access to resources for long-term follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The Cancer Genetics program at St. Vincent Hospital in Indianapolis, Indiana began as many cancer genetics programs did back in the late 1990s: small and included under the umbrella of another department, with cancer genetics typically representing a small percentage of a genetic counselor’s responsibilities. At our institution, a 550-bed community-based quaternary care hospital, cancer genetics services were initiated within the Maternal Fetal Medicine and Genetics department in 1998. The first year that patients were seen, there were 6 new patients, all self-referred due to concern about family history of cancer, and all unaffected. In the year 2000, the Cancer Genetics program migrated to Pediatric Genetics, because there was a geneticist in that newly-created department, yet the patient volume remained modest (increasing from 17 new patients seen in year 2000 to 42 new patients in 2003). By 2005, there were 113 new patient contacts, largely affected individuals referred by their surgeon or oncologist. The one part-time genetic counselor could no longer provide both cancer genetic and pediatric genetic counseling services, so a new department, the Cancer Genetics Risk Assessment Program, was created in 2006. The demand for cancer genetics services and volume within the program continued to increase with 168 new patients seen in 2006 and 184 new patients in 2007. The wait time for an appointment was 5–6 weeks. The addition of a second genetic counselor and part-time administrative assistant in 2008 decreased the wait time significantly, and allowed for more patients to be seen (total of 290 new patients in 2008).
Throughout this experience, we have documented a significant patient failure rate. We defined this in our practice as being unable to contact a referred patient, a patient declining to schedule when referred, a patient not showing for an appointment, or canceling an appointment without rescheduling (often due to lack of insurance coverage for the consultation and/or testing). We began to track these patient failures, and over a period of 2 years from 2006–2008, we observed a failure rate of 33%.
Another observation that we have made over the past few years is an increase in the number of physicians who have started to offer their own genetic testing. This observation is supported in the literature, which documents as contributing factors an increase in patient requests for genetic testing and physicians’ perception of limited access to genetic services (Acheson et al. 2005; Carroll et al. 2003; Friedman et al. 2003; Sifri et al. 2003; Wideroff et al. 2003). Information about genetics tests has become increasingly available to consumers and their medical providers via the internet, direct-to-consumer marketing, the popular media and medical literature. There are other factors that may contribute to referral patterns, including perception of genetic discrimination (Lowstuter et al. 2008). Additionally, professional guidelines from several medical societies have adopted genetic testing algorithms (ASCO, NCCN, ACOG, etc), which may also have contributed to an increase in genetic testing behavior. Observations of our own program led us to surmise that an increase in physician involvement with genetic testing may have been due in part to the long wait time for a genetic counseling appointment and convenience of providing it themselves while the patient was in the office. Additionally, we postulated that patient failures were a factor, particularly for the breast surgeons as they frequently use genetic test results to make treatment decisions. As patients fail to present for genetic consultation and testing when referred, a physician may begin offer this service as a mechanism to get the information they need for management.
Recognizing this trend, we have encouraged physicians to maintain a relationship with us even when they are offering their own genetic testing. One approach to this has been through our multi-disciplinary tumor board. We have 2–3 tumor boards per year in which we present hereditary cancer cases. We attempt to focus on cases that are appropriate for physician offices to handle on their own with suggestions for performing their own genetic testing, as well as cases that demonstrate how we can be supportive and add expertise, such as the more difficult or unusual cases. Additionally, we have repeatedly emphasized the importance of referring a person who tested negative when they expected a positive result, so that we can determine if there is any other clinical testing that would be appropriate or if any research studies might be available, using cases to demonstrate.
Another mechanism to reach these offices is through their support staff; mid-level providers such as nurses and nurse practitioners. We have identified key people in those offices, and have made ourselves available by phone, e-mail, or even in-person to answer questions and assist with their testing needs. This allows more opportunities to obtain referrals that are most appropriate to our higher-level genetic counseling skills.
In August of 2007, the St. Vincent Women’s Breast Services hired a women’s health nurse practitioner to begin a Breast Risk Assessment clinic. This effort was driven by the desire to identify, educate and offer screening services to women at-risk to develop breast cancer by assessing risk factors such as estrogen exposure, obesity, alcohol intake and family history. From the outset, this program was set up as a collaborative approach, with the funds for salary support for a genetic counselor to be involved in this endeavor. We opted to use this approach so that our skill sets would be best utilized in this setting for optimal patient quality of care and professional use of time and expertise. The Cancer Genetics Risk Assessment Program has been maintained as an independent entity with evaluations provided by board-certified genetic counselors and traditional referrals from oncologists, surgeons, OB/GYNs, etc. The Breast Risk Assessment Clinic was designed to identify women whose health care provider had not recognized that they were at increased risk or had not referred them for risk assessment. Evaluations through this clinic are conducted by the nurse practitioner, with input and support from the genetic counselors.
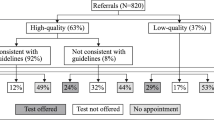
Women are initially identified as candidates to be seen in the Breast Risk Assessment Center by taking a computer survey in the mammography suite at the time of their annual screen. This survey collects medical and family history and then calculates the risk to develop breast cancer as well as the likelihood of a BRCA1/2 mutation in the family using the CancerGene program. A written set of family history criteria were developed to determine who is invited for further risk evaluation with the nurse practitioner in the Breast Risk Assessment Program, using published guidelines as a model, and have been revised based on questions that have arisen during our pilot phase. If a patient does not meet the criteria for hereditary breast and ovarian cancer risk but has a significant history of other cancers, then the patient is invited back for an evaluation with the genetic counselors in the Cancer Genetics Risk Assessment Program. The surveys are reviewed and these criteria are applied by the genetic counselors and/or nurse practitioner on a rotating basis, and a letter is mailed to the patient that they are either at average risk or that they may be at increased risk and further evaluation in either the Breast Risk Assessment or Cancer Genetics Risk Assessment Program is warranted.
Women who opt for further evaluation are seen in the Breast Risk Assessment Center by the nurse practitioner. This results in a comprehensive plan which may include genetic testing, breast MRI, clinical breast exam, and self breast exam instruction. In addition, a woman may be referred to a breast surgeon and/or prescribed chemoprevention by the nurse practitioner. The nurse practitioner discusses and offers genetic testing when appropriate, and coordinates a blood draw. Women who undergo genetic testing have results reviewed by the nurse practitioner and genetic counselor team to make further recommendations based on the outcome of the test in light of the family history assessment.
The nurse practitioner reviews any difficult or unusual cases with one of the genetic counselors. At that time, the patient may be referred to see a genetic counselor in the Cancer Genetics Risk Assessment Program instead of the nurse practitioner. Additionally, the genetic counselors are available for support in any case that the nurse practitioner feels would be helpful, often just a validation of approach by telephone. Any abnormal results are reviewed as a team to make a plan for follow-up. The nurse practitioner can order appropriate screening tests, prescribe tamoxifen or raloxifene if appropriate and perform a breast exam; the genetic counselor can address the genetic testing, risk assessment and family issues, as well as addressing any potential differential diagnoses in more difficult cases. This allows for the best use of each specialist’s skills. This collaborative approach is valued for streamlining the assessment process and utilizing the combined expertise of a nurse practitioner and genetic counselors. As a result, referrals have become more appropriately triaged and patients are adequately served.
Training and supervision of nurses to provide cancer genetic testing has been found to be as effective as utilizing genetic counselors in educating patients about genetic testing in a research setting (Bernhardt et al. 2000). Prior to the implementation of our program, the nurse practitioner took a 2-day short course on hereditary breast/ovarian cancer and spent several months reading articles on hereditary risk factors and observing genetic counseling sessions. She attended breast and genetics tumor boards and discussed cases that arose in the breast center in great detail with the genetic counselors. The possibility of obtaining an Advanced Practice Nurse in Genetics credential through the Genetic Nursing Credentialing Commission was investigated, but with such strong support from two board certified genetic counselors, it was not pursued.
This process has worked very well in our community setting. There are several factors that have contributed to this collaborative effort’s success. First, there is strong administrative support on both sides; from Cancer Services under which the genetic counselors fall, as well as Breast Services under which the nurse practitioner is housed. Second, the nurse practitioner has been very proactive in learning about cancer genetics. Though she has a comfort level to offer and order genetic testing, she also has a good recognition of her limitations. She will evaluate families for a history of breast and ovarian cancer, but will refer those families for evaluation and/or consult with a genetic counselor if other cancers appear predominant or the family does not appear to fit well within the BRCA spectrum. Finally, the openness of the genetic counselors to educating the nurse practitioner and being available to answer questions has been key to this program’s success. There have been no “turf” issues due to this open communication, regular meetings, understanding of limitations and recognition of strengths that each team member can bring to the table.
We hope to foster more relationships in this manner. Recently, the Cancer Genetics Risk Assessment Program was approached by a community hospital within our health network, but 60 miles away, to provide genetic counseling services on-site for them. The hospital personnel had minimal training to offer genetic testing, and indicated they were not completely comfortable offering this service themselves. They had been encouraged to incorporate our services by an oncologist who practices in both hospitals and was currently referring patients to the Cancer Genetics Risk Assessment Program. Additionally, staff at this hospital had experienced a few challenging cases that had highlighted for them the need to have a more highly-trained genetics professional involved.
We offered to meet with them to evaluate their needs. They had two nurses who were interested in genetic testing and learning more about the process. We invited them to observe some genetic counseling sessions in our office and offered to share the software that we use to identify high risk patients. Since our hospitals are on the same computer network, they could potentially use the risk assessment software locally. The data collected at their local hospital would be stored on the common server, allowing us to review cases and make recommendations about the need to invite patients for follow up at their local hospital versus a more in-depth evaluation within our program. We are in the process of setting up a more formal relationship where we can support the identified nurses in providing genetic testing for their straightforward cases, in a manner very similar to the relationship we have with the nurse practitioner in our Breast Risk Assessment Center. We will likely attend their tumor board monthly or bi-monthly, at which time we can review cases in person and see patients that require a higher level genetics skill. We also remain available for patients to come to us on a referral basis, as they did previously.
We believe that streamlining the process of genetic testing and keeping it local when possible best utilizes resources and the skills of highly-trained genetic counselors. This should decrease the failure rate for patients who refuse or cannot travel outside their local area and for those being treated for cancer who may be overwhelmed by a complicated and busy treatment schedule. Additionally, local genetic testing allows for patients to more easily access and coordinate the appropriate follow-up they may need, such as referrals to breast surgeons and screening services such as MRI, since those who arrange genetic testing will likely be more familiar with resources available locally.
In summary, we have found that when genetic evaluation and testing is offered in this collaborative, supportive manner, the patients are well-served to receive genetic testing within their local environment. This approach has not negatively influenced our patient volume, as evidenced by our continued growth. In fact, it has likely contributed to the increase in patient volume, as physicians are willing to refer when they have an established relationship and open communication with a genetic counselor. They are more likely to recognize the complexity of genetic testing as the positive interactions regarding their patients increase, and the support we provide them is valuable and desired.
References
Acheson, L., Stange, K. C., & Zyzanski, S. (2005). Clinical genetics issues encountered by family physicians. Genetics in Medicine, 7(7), 501–508.
Bernhardt, B. A., Geller, G., Doksum, T., & Metz, S. A. (2000). Evaluation of nurses and genetic counselors as providers of education about breast cancer susceptibility testing. Oncology Nursing Forum, 27(1), 33–39.
Carroll, J. C., Brown, J. B., Blaine, S., Glendon, G., Pugh, P., & Medved, W. (2003). Genetic susceptibility to cancer: family physicians’ experience. Canadian Family Physician, 49, 45–52.
Friedman, L. C., Cooper, H. P., Webb, J. A., Weinberg, A. D., & Plon, S. E. (2003). Primary care physicians’ attitudes and practices regarding cancer genetics: a comparison of 2001 with 1996 survey results. Journal of Cancer Education, 18(2), 91–94.
Lowstuter, K. J., Sand, S., Blazer, K. R., MacDonald, D. J., Banks, K. C., Lee, C. A., et al. (2008). Influence of genetic discrimination perceptions and knowledge on cancer genetics referral practice among clinicians. Genetics in Medicine, 10(9), 691–698.
Sifri, R., Myers, R., Hyslop, T., Turner, B., Cocroft, J., Rothermel, T., et al. (2003). Use of cancer susceptibility testing among primary care physicians. Clinical Genetics, 64, 355–360.
Wideroff, L., Freddman, A. N., Olson, L., Klabunde, C. N., Davis, W., Srinath, K. P., et al. (2003). Physician use of genetic testing for cancer susceptibility: results of a national survey. Cancer Epidemiology, 12, 295–303.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cohen, S.A., McIlvried, D. & Schnieders, J. A Collaborative Approach to Genetic Testing: A Community Hospital’s Experience. J Genet Counsel 18, 530–533 (2009). https://doi.org/10.1007/s10897-009-9243-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-009-9243-y