Abstract
This study describes the development and psychometric evaluation of an adolescent self-report version of the Pediatric Diabetes Routines Questionnaire (PDRQ:A), a measure of diabetes-specific routines for youth with type 1 diabetes, and further validation of the parent-version (PDRQ:P) in an adolescent sample. Participants included 120 parent–adolescent dyads (ages 12–17) and an additional 24 parents who completed measures of diabetes-specific adolescent routines, general adolescent routines, diabetes self-care, and family support of youth diabetes care. The PDRQ:P/A demonstrated good internal consistency, test–retest reliability, and parent–child agreement, and adequate validity coefficients. Confirmatory factor analysis supported a one-factor model. Promising results were obtained. The PDRQ:P/A is a clinically feasible parent- and self-report measure that can provide valuable information regarding how frequently adolescents engage in their diabetes management tasks in a consistent manner. Addition of an adolescent report format will enhance the utility of the measure for clinical and research use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Management of type 1 diabetes (T1D) to prevent the development of acute- and long-term complications requires a demanding regimen, including careful blood glucose monitoring, insulin administration, and dietary and exercise management (American Diabetes Association [ADA], 2017). Routine self-management of T1D is therefore critical for achievement of optimal T1D outcomes (i.e., adherence, glycemic control, and quality of life). For adolescents with T1D, however, normative developmental tasks (e.g., puberty, increased independence and autonomy, incomplete executive functioning development) may significantly interfere with T1D management routines (Markowitz, Garvey, & Laffel, 2015; Rausch et al., 2012; Wasserman, Hilliard, Schwartz & Anderson, 2015; Wysocki, 1993).
There is a growing body of literature highlighting the importance of general child and family routines in daily chronic illness management (see Crespo et al., 2013 for a review). Findings indicate that higher levels of family routines buffer against disordered eating behaviors in adolescent girls with T1D (Mellin, Neumark-Sztainer, Patterson, & Sockalosky, 2004), as well as anxiety (Markson & Fiese, 2000) and decreased inflammatory markers (Schreier & Chen 2010) in youth with asthma. Greening, Stoppelbein, Konishi, Jordan, and Moll (2007) found that general child routines mediate the relation between behavior problems and regimen adherence in youth with T1D (Greening et al., 2007). With the exception of Fiese, Wamboldt, and Anbar (2005) and Fiese, Winter, Anbar, Howell, and Poltrock (2008), who found a positive association between asthma-specific routine burden and asthma severity (Fiese et al., 2005, 2008), few researchers have examined routines that are specific to individual chronic illness regimens. Yet, well-validated, disease-specific measures are important because they are more responsive to change and clinically useful than general measures (Wiebe, Guyatt, Weaver, Matijevic, & Sidwell, 2003).
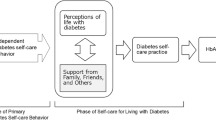
Disease-specific routines are “observable, repetitive behaviors, in relation to self-care behaviors of disease management, which occur with predictable regularity in the daily and/or weekly life of the individual with the illness” (Pierce & Jordan, 2012). For diabetes, self-care/adherence is defined as the “daily regimen tasks that the individual performs to manage their disease” (Weinger, Butler, Welch, & La Greca, 2005), whereas diabetes-specific routines occur when specific self-care tasks are performed at a consistent time, order, and/or manner. A common diabetes-specific routine for the self-care task “treatment of hypoglycemia” is the “15 min rule” [i.e., check blood glucose, eat 15 g of fast acting carbohydrates, wait 15 min, check again (ADA and Hypoglycemia, n.d.)]. An example of a more individualized diabetes-specific routine for the self-care task “refilling prescriptions” might be “Adolescent tells parent each time she opens her last insulin pen or test strip bottle.”
Recent development of the Pediatric Diabetes Routines Questionnaire (PDRQ) provided a psychometrically sound mechanism for studying diabetes-specific routines in youth (Pierce & Jordan, 2012). The PDRQ is a 21-item parent-report measure of the frequency of routines specific to the diabetes regimen in youth with T1D between ages 5 and 17. Factor analysis of the PDRQ revealed two components, Daily Regimen Routines (DRR) and Technical/Situational Routines (TSR), which sum to form a total score (Pierce & Jordan, 2012). The DRR component (12 items) includes items measuring the extent to which youth engage in everyday regimen tasks at about the same time or in the same order or way. The TSR component (9 items) measures the extent to which routines are followed in intermittent situations (e.g., while exercising) and for technical aspects of the regimen (e.g., rotating sites and calculating doses). Psychometric properties of the PDRQ are discussed in the “Methods” section.
Although the PDRQ allows for assessment of diabetes-specific routines, its usefulness with the adolescent T1D population is limited due to its sole parent-report format. Achieving independence from family members is a key developmental task during adolescence and, for many adolescents with T1D, this aligns with the transfer of responsibility for T1D management from parent to adolescent (Markowitz et al., 2015). Development of an adolescent self-report version of the PDRQ would provide a means to obtain more accurate information directly from adolescents (Markowitz et al., 2015), thereby increasing confidence in the data.
The primary goal of this study was to develop and validate an adolescent self-report version of the PDRQ, the PDRQ: Adolescent (PDRQ:A) and to further validate the parent-report version (renamed PDRQ: Parent [PDRQ:P]) in a large sample of adolescents with T1D and their parents. The aims of this study are as follows: (1) to evaluate the factor structure of the PDRQ:P/A through confirmatory factor analysis (CFA); (2) to replicate previous research supporting the internal consistency of the PDRQ:P and to evaluate the internal consistency of the PDRQ:A; (3) to examine the convergent validity of the PDRQ:P/A with measures of general adolescent routines, diabetes-specific family conflict, diabetes-specific parent support, and diabetes adherence; (4) to examine the degree of parent–adolescent agreement on the PDRQ; and (5) to examine demographic differences on the PDRQ:P/A.
Methods
Participants
The PDRQ:P/A was administered to 120 adolescents with T1D and their primary caregiver (subsequently called parent). An additional 24 parents completed the PDRQ:P whose adolescents did not complete the PDRQ:A. Adolescents were eligible if they had diagnosis of T1D for at least 6 months, and were between 12 and 17 years old, English speaking, and not diagnosed with a comorbid chronic illness, intellectual disability, and/or autism spectrum disorder. Parents were eligible if they were English speaking and had an adolescent meeting eligibility criteria. Participants were recruited through the mailing lists of two diabetes organizations and through the upcoming patient appointment list at a children’s hospital.
Measures Under Evaluation
Demographic Form
Demographic and clinical information including adolescent age, gender, race, insulin regimen, and duration of diabetes and parent marital status, education level, employment status, and annual family income were collected through parent report.
Pediatric Diabetes Routines Questionnaire: Parent (PDRQ:P)
Initial analyses of the PDRQ:P (originally PDRQ) in 198 parents of youth ages 5–17 with T1D (Pierce & Jordan, 2012) suggested promising psychometrics, including internal consistency (α = .88), test–retest reliability (r = .81), and construct validity through positive relations with general child routines, family rituals, diabetes treatment adherence, and supportive diabetes-specific family behaviors and through a negative correlation with nonsupportive diabetes-specific family behaviors (Pierce & Jordan, 2012). Item frequency is measured on a 5-point Likert scale ranging from 1 “never” to 5 “everyday.” A N/A “cannot rate this item/not applicable” response is also available.
For the current study, the content of the original 21 items remained identical, but the referee in the items was changed from “My child…” to “My adolescent.” After conducting a literature review on adolescent development (e.g., Betz & Redclay, 2005), five new items were added to the PDRQ:P to assure developmental appropriateness, all beginning with “My adolescent follows a routine for managing diabetes while…” “…on a date”; “…engaging in extracurricular activities (e.g., sports, clubs, etc.)”; “…spending time with friends at our house”; “…spending time with friends away from home”; and “…at work.” It was expected that all new items would fall within the TSR domain because they occur in specific situations and are unique to the individual adolescent. The modified PDRQ:P is shown in Fig. 1.
Pediatric Diabetes Routines Questionnaire: Adolescent (PDRQ:A)
The PDRQ:A (Fig. 2) was developed for the current study. It included the 21 items that were reworded to first person (i.e., “I” instead of “My child”) from the original PDRQ, as well as the same five new developmentally relevant items that were added to the PDRQ:P.
Validation Measures
The following measures were administered for construct validation of the PDRQ:P/A. Item content is identical between the parent- and child-report versions on all measures.
Adolescent Routines Questionnaire: Parent and Self-Report (ARQ:P/S)
The ARQ (Meyer, 2008) is a 33-item measure of adolescent routines ages 12–17 in five domains: Daily Living Routines, School/Discipline Routines, Household Routines, Extracurricular Activities, and Social Routines, which sum to form a Total score. Item frequency is rated on a 5-point Likert scale: 0 “almost never” to 4 “nearly always.” Total ARQ:P/S scores, obtained by summing all item ratings, can range from 0 to 132 with higher values indicating more frequent routines. The ARQ:P/S demonstrated adequate test–retest reliability (r’s = .74 and .67), parent–child agreement (r = .65) , and construct validity in its initial development study (Meyer, 2008). Coefficient alpha in the present sample was .91 and .86 for the ARQ:P/S.
Diabetes Family Behavior Checklist: Parent- and Child-Rated (DFBC:P/C)
The DFBC (Lewin et al., 2005; Schafer, Glasgow, McCaul, & Dreher, 1983; Schafer, McCaul, & Glasgow, 1986) is a 16-item measure of supportive and nonsupportive family behaviors related to the diabetes self-care regimen in youth ages 8–18. Frequencies of nonsupportive (7 items) and supportive (9 items) behaviors are rated on a 5-point Likert scale: 1 “never” to 5 “at least once a day.” Nonsupportive and supportive family behavior subtypes are calculated separately and higher values indicate greater frequencies of behavior (range is 7–35 for nonsupportive and 9–45 for supportive). In the present study, coefficient alpha for the DFBC:P/C Supportive scale was .67 and .76, and for the DFBC:P/C Nonsupportive scale was .72 and .69.
Diabetes Family Conflict Scale: Parent and Child Versions (DFCS:P/C)
The DFCS (Hood, Butler, Anderson, & Laffel, 2007) is a 19-item measure of diabetes-specific family conflict in two domains: Direct Management Tasks and Indirect Management Tasks. Frequencies of conflict are rated on a 3-point Likert scale from 1 “almost never” to 3 “almost always.” Total DFCS:P/C scores, obtained by summing all item ratings, can range from 19 to 57 with higher values indicating more frequent conflict. Moderate parent–child agreement (r = .26) and concurrent and predictive validity have been reported (Hood et al., 2007). Coefficient alpha in the present sample was .95 and .97 for the DFCS:P/C.
Self-Care Inventory: Parent and Adolescent Versions (SCI:P/A)
The SCI (Lewin et al., 2009) is a 14-item measure of respondents’ perceptions of their adherence to diabetes self-care recommendations rated on a 5-point Likert scale: 1 “never do it” to 5 “always do this as recommended without fail;” “Not Applicable” is provided as a response option. Total SCI:P/A scores are obtained by summing all item ratings and dividing by the total number of items (subtracting the number of missing items and items marked “Not Applicable” from the dominator); values are then multiplied by 10 to provide a more conventional metric (Lewin et al., 2009). Higher scores indicate more optimal adherence. Lewin et al. examined the psychometric properties of the SCI in a sample of youth on more recent, intensive regimens and their parents. Strong test–retest reliability coefficients were reported (r = .86 and .91). Parent–child agreement was moderate (r = .47), and convergent validity was supported (Lewin et al., 2009). Coefficient alpha in the present sample was .75 and .77 for the SCI:P/A.
Procedure
Following Institutional Review Board approval, participants were recruited through a national diabetes organization, state diabetes organization, or a university-based children’s hospital. Two different methods of data collection were utilized: online and mail-out. All parent–adolescent dyads were offered an opportunity to be entered into a lottery for one of four $25 gift cards to a discount retailer if both the parent and adolescent completed all questionnaires. At the end of the study, eligible dyads were entered into one of four lotteries in the order in which they enrolled in the study (i.e., the first 40 eligible participants were entered into the first drawing). One dyad was randomly selected from each lottery and was mailed a gift card.
Online participants (n = 118 parents, 81.9%; n = 94 adolescents, 78.3%) completed study measures via a secure survey website. For online recruitment through diabetes organizations (n = 90 parents, 62.5%; n = 66 adolescents, 55.0%), a parent hyperlink (electronic consent/parental permission form, demographic form, and parent versions of study measures) was distributed to members by the organization director via email or listserv/e-newsletter. Within one week of measure completion, the parent was emailed an adolescent hyperlink (electronic assent form and adolescent versions of study measures) and instructed to forward it to their adolescent with T1D. For online recruitment through the children’s hospital (n = 28 parents and adolescents, 19.4%), parents who did not opt out via an initial mail-out were emailed the parent and the adolescent hyperlinks together and instructed to forward the adolescent hyperlink to their adolescent with T1D. Parents who did not complete measures within one week were emailed up to three weekly reminders. For both online groups, all adolescent surveys were completed within one month of parent completion. If adolescents did not respond within one week of parent completion, up to three weekly reminder emails were sent to parents. Twenty-four parents completed the parent surveys, but their adolescent did not. χ2 and t tests revealed no significant differences on demographic or clinical variables between parent participants whose adolescent did and did not complete the PDRQ:A.
The state diabetes organization did not have email addresses on file for all members, so in an effort to recruit a socioeconomically diverse sample, a mail-out was also conducted (n = 26 parents and adolescents, 18.1% of total sample). Paper packets including the consent and assent form, demographic form, and study measures were provided to the state organization director, who then mailed packets to all parents without email addresses.
Test–retest data were collected for 35.8% (n = 43) of adolescents. Two weeks after submission of their initial measures, all online adolescent participants were invited to complete the electronic PDRQ:A a second time via an email sent to their parents and forwarded. Mail-out participants did not participate in the test–retest sample. Retest surveys were included in analyses if they were completed within five weeks of the initial PDRQ:A. No incentives were provided for participating in the test–retest sample.
For CFA, missing items and not applicable responses on the PDRQ:P/A were interpolated using bootstrapping, which occurred for less than 0.05% of PDRQ:P and PDRQ:A responses. For demographic, reliability, and validity analyses, missing items and not applicable responses on the PDRQ:P/A for the initial sample and the PDRQ:A retest sample were replaced with the average item score, which occurred for less than 0.03% of PDRQ:P and PDRQ:A responses. Questionnaires with more than four items missing were not included in the analyses.
Results
Sample Characteristics
In the overall sample, mean age of adolescents (N = 120) was 13.9 years (SD = 1.61; range 12–17 years); 52.5% were female; 85.0% were White and 8.3% were Black. More than half (58.3%) used an insulin pump. Mean duration of T1D was 5.42 years (SD = 3.98; range 6 months–15 years). Mean parent report of adolescent Hemoglobin A1C was 8.06 (SD = 1.47). Most parents were mothers (85.5%) and co-parenting (81.4% married or living with someone); 17.9% were single (living alone, divorced, widowed, or separated). Socioeconomic status computed using Hollingshead’s (1975) four-factor index indicated a median value corresponding to major business and professionals (M = 52.63, SD = 10.17; range 22.0–67.5) (Hollingshead, 1975). Demographic and clinical differences between the initial and test–retest samples are reported below.
χ2 and t tests were examined to determine if demographic variables differed between participants who completed surveys online versus mail-out and who completed surveys online via the diabetes organizations versus the children’s hospital. The online group (M = 53.69, SD = 9.32) reported a significantly higher SES level than the mail-out group (M = 47.43, SD = 12.59), t (128) = 2.21, p < .05. There was a higher percentage of pump users in the diabetes organization online group than the children’s hospital online group, χ2 (1, N = 115) = 9.32, p < .01. To maximize power given the small proportion of the sample belonging to the mail-out group (18.1%) and the children’s hospital online group (19.4%), the samples were combined for subsequent analyses. The implications of these differences are discussed below.
Item Reduction
The five new developmentally relevant items were considered for elimination based on the following criteria: (a) item mean of 2.00 or less, indicating the average rating for the routine was “sometimes” or less; (b) item-total correlation coefficient below .30 with the PDRQ:P/A total score; and/or (c) item endorsement of greater than 50% “Not Applicable,” indicating that the item is not representative of the majority of participants.
All five items had means greater than 2.00 and item-total correlations greater than .30 for the PDRQ:P/A, with the exception of the new PDRQ:P item “…on a date” (r = .273). Two new items (…on a date; …at work) also had high percentages of “Not Applicable” responses by parents (68.1 and 79.9%, respectively) and adolescents (51.7 and 69.7%, respectively). These two items were not representative of the majority of participants and inclusion in the CFA would have prohibitively restricted the sample size. They were eliminated from subsequent analyses.
Confirmatory Factor Analysis
Mplus Version 6.11 (Muthén & Muthén, 2007) was used to conduct a CFA to determine if the two factors (DRR and TSR) obtained in the original study were maintained in the current sample. Weighted least squares mean and variance was specified as the CFA estimator. Two goodness-of-fit indices were evaluated on the 24 observed variables to assess the degree of fit between the model and sample: Comparative Fit Index (CFI; ≥ .95 satisfactory) and Root Mean Square Error of Approximation (RMSEA; ≤ .08 satisfactory) (Brown, 2006; Hu & Bentler, 1999). The two-factor model provided a good fit to the data for the PDRQ:P: χ2 (251, N = 119) = 467.91, p < .001; CFI = .97; and RMSEA = .08 and PDRQ:A: χ2 (251, N = 112) = 362.68, p < .001; CFI = .95; and RMSEA = .06. The inter-factor correlation between the two subscales on the PDRQ:P was r = .95, p < .001 and on the PDRQ:A was r = .93, p < .001, suggesting that items likely cross-loaded between factors. Thus, a one-factor model was tested and provided a good fit for the PDRQ:P: χ2 (252, N = 118) = 486.16, p < .001; CFI = .97; and RMSEA = .08 and the PDRQ:A: χ2 (252, N = 111) = 369.85, p < .001; CFI = .95; and RMSEA = .06.
Given the goodness-of-fit for both models, the one-factor solution was selected for further analyses because it offers a more parsimonious fit to the data. The single-factor loadings for each item of the PDRQ:P/A are reported in Table 1. For the PDRQ:A, all items significantly loaded onto the latent factor. For the PDRQ:P, only Item 4 (“My adolescent is routinely supervised when s/he has a low blood sugar at school.”) did not load significantly, p = .26. Given the significant item loading on the PDRQ:A, and the item’s positive performance in the initial development study, this item was retained on the PDRQ:P. The possible score range for the 24-item PDRQ:P/A is 24–120 and distributions are provided in Table 2.
Reliability
The 24-item PDRQ:P/A demonstrated coefficient alphas of .939 and .901, respectively. Item-total correlations ranged from .104 (Item 4) to .817 (Item 25) for the PDRQ:P and from .229 (Item 4) to .698 (Item 25) for the PDRQ:A (Table 1).
χ2 and t tests were used to analyze differences between participants that provided and did not provide test–retest data; there were no significant differences on most variables suggesting that completers of the test–retest data did not differ from the overall sample on age, race, insulin regimen type, SES, and duration of T1D. However, there was a significantly lower percentage of female adolescents (41.9%), χ2 (1, N = 117) = 3.93, p = .047, and single parents (9.3%), χ2 (1, N = 118) = 3.89, p = .049, in the retest sample than in the overall sample. The bivariate correlation between the PDRQ:A initial test and retest demonstrated good temporal reliability, r (38) = .761, p < .001. A t test revealed that the means between administration time-points were not significantly different, t (38) = − 1.56 p = .13, indicating that PDRQ:A scores from time one to time two administration were consistent.
To examine consistency between parent and adolescent report on the PDRQ:P/A, the bivariate correlation was calculated between the two versions, r (109) = .611, p < .001. The means between the PDRQ:P/A were not significantly different, t (109) = − .635, p = .53, indicating that routine scores were consistent between versions.
Construct Validity
Bivariate correlations between the PDRQ:P/A and scores on measures theoretically hypothesized to be related to diabetes-specific routines were examined. Moderate to strong correlations in the predicted direction were found between the PDRQ:P/A and all construct validity measures with the exception of the PDRQ:P and DFBC:P Supportive Scale and the PDRQ:A and DFCS:A, although the latter relation approached significance, r (99) = − .19, p = .057 (Table 2). Bivariate correlations between the PDRQ:P/A and validation measures and the distribution of scores of all measures can be found in Table 2.
Relations with Demographic and Clinical Characteristics
Correlations and t tests were examined between the PDRQ:P/A and demographic and clinical variables (Table 3). Race was dichotomized as White and racial/ethnic minority and marital status was dichotomized as single parenting (single living alone, divorced, widowed, or separated) or co-parenting (married or living with someone). Adolescent age was negatively correlated with the PDRQ:P/A, r = − .226, p < .01 and r = − .230, p < .05, respectively. Duration of T1D diagnosis was also negatively correlated with the PDRQ:A, r = − .192, p < .05 but not the PDRQ:P. On the PDRQ:P, greater frequency of diabetes-specific routines was reported by parents who identified their adolescent as White (M = 76.61, SD = 14.65; n = 120) than as an ethnic/racial minority (M = 67.66, SD = 18.92; n = 19), t (137) = 2.37, p = .02. On the PDRQ:P, parents who co-parented (M = 76.97, SD = 14.16; n = 115) reported significantly more frequent diabetes-specific routines than single parents (M = 68.62, SD = 19.01; n = 26), t (31.56) = 2.11, p = .04. Neither adolescent race nor parental marital status were significantly correlated with the PDRQ:A.
Discussion
Overall, findings support the PDRQ:P/A as a psychometrically sound instrument for measuring the consistency and regularity with which adolescents perform T1D management tasks. Two of the five new developmentally relevant items (i.e., following routines while at work or on a date) were eliminated prior to analyses. Because the sample included adolescents between ages 12 and 17, the “work” item was probably not appropriate for the younger portion of the sample. Indeed, the U.S. Department of Labor does not report employment statistics for youth younger than 16 years old (Bureau of Labor Statistics, 2017). The same explanation is likely for the “dating” item as well.
Item 4, “I/My adolescent is routinely supervised when I/he/she has a low blood sugar at school” did not load significantly onto the expected latent factor solution for the PDRQ:P, although it did for the PDRQ:A. The pattern coefficients and item-total correlations were also low for both informants, suggesting the item is measuring something different than other items on the scale. Since treating low blood sugars is something that can be done relatively easily and independently at school, supervision is likely something that is not relevant to adolescents with T1D and differentiates Item 4 from the other school-related items (Items 19 and 20), both of which had moderate to high pattern coefficients and item-total coefficients. Nevertheless, Item 4 was retained on the PDRQ:P to maintain consistency between versions of the PDRQ and across studies. However, future PDRQ development studies should continue to monitor and evaluate the properties of Item 4, particularly on the adolescent version.
CFA was conducted to examine the factorial validity of the PDRQ:P/A. The two-factor model resulted in a good fit for the PDRQ:P/A, but the high inter-factor correlation between the factors suggests that there was a considerable degree of overlap such they were not measuring distinct types of routines. A one-factor model was tested post hoc and provided a good fit for the PDRQ:P/A, offering a more parsimonious fit. Although diabetes-specific routines can theoretically be understood in terms of two factors, there is no presumption that the underlying component constructs are distinct, orthogonal, or differentially predictive. Given the difference in factor structures between the initial PDRQ, which was validated in parents of youth ages 5–17 (Pierce & Jordan, 2012), and the PDRQ:P/A (i.e., two-factor structure and one-factor structure, respectively), future research should focus on further examination of the factor structures of the PDRQ and PDRQ:P/A in children and adolescents. Until additional psychometric data and scoring guidelines are published, we recommend using the initial PDRQ and corresponding two-factor structure for parents of children ages 5–11 and the PDRQ:P/A and corresponding one-factor structure for adolescent ages 12–17 and their parents. Results of the current study indicate that use of a single factor for the PDRQ self- and parent-report in adolescents appears to be theoretically and statistically sound for measurement of the diabetes-specific routine construct.
Findings revealed good reliability for the PDRQ:P/A. The measure is internally consistent and demonstrated good parent–child agreement and temporal stability. Construct validity of the PDRQ:P/A was supported by appropriate correlations with measures of general child routines and diabetes treatment adherence. However, not all predicted relationships between diabetes-specific routines and diabetes-specific family support and conflict were supported. While a negative relation between parent- and adolescent-report of diabetes-specific routines and nonsupportive diabetes-specific family behaviors was found, only adolescents revealed a positive relation between diabetes-specific routines and supportive diabetes-specific family behaviors. The nonsignificant relation in parents was surprising given the positive correlations found between the same variables in the PDRQ development study (Pierce & Jordan, 2012), but may be reflective of increasing autonomy and responsibility for T1D management during adolescence (Markowitz et al., 2015). Future PDRQ:P/A validation studies should incorporate the use of the Diabetes Family Responsibility Questionnaire to assess whether increasing adolescent autonomy is related to more frequent routines (Anderson, Auslander, Jung, Miller, & Santiago, 1990; Vesco et al., 2010). On another measure of family functioning, it was expected that higher family conflict surrounding diabetes tasks would be related to a lower frequency of diabetes-specific routines. This relation was supported in parents, but only approached significance (p = .057) in adolescents, indicating that with more power (i.e., a larger sample size) the relation may have reached significance.
Due to differences in sampling methods, demographic variables were evaluated for differences by method. The online group reporting a significantly higher SES level than the mail-out group. This underscores the critical importance of including mechanisms to reach a broad range of SES in order to obtain representative samples of adolescents with diabetes and their parents. Additionally, there were a significantly higher percentage of pump users in the diabetes organization online group than the children’s hospital group. The children’s hospital group was substantially smaller than the diabetes organization online group, and drawn from a single outpatient clinic, so likely less representative of the underlying population of adolescents with T1D than the diabetes organization group, which was larger and recruited nationally. This finding may be an artifact of these sampling differences.
In examining demographic differences on the PDRQ;P/A, adolescent age was negatively correlated with frequency of diabetes-specific routines, indicating that older adolescents had less frequent diabetes-specific routines. Adolescent age was also negatively correlated with the SCI:P/S (r = − .22, p = .01 and r = − .19, p = .05, respectively) indicating that older adolescents had lower diabetes regimen adherence. While the cross-sectional nature of this study precludes conclusions regarding directionality or cause of these relations, the fact that both adherence and routines are negatively correlated with age is consistent with prior literature suggesting changes in diabetes management responsibility throughout adolescence (Markowitz et al., 2015) and that older adolescent age is predictive of poorer T1D management and control (Hilliard, Wu, Rausch, Dolan, & Hood, 2013). Longitudinal research is needed to document the developmental trajectory and psychosocial correlates of diabetes-specific routines across adolescent and young adult age groups and also to examine the PDRQ’s predictive validity.
Further examination of demographic differences and parent report of diabetes-specific routines revealed more frequent diabetes routines among White adolescents and those with more than one parent. These results are consistent with previous research indicating that racial/ethnic minorities and single-parent family composition are risk factors for poor T1D adjustment and health outcomes (Agarwal, Jawad, & Miller, 2015; Lord et al., 2015). Given that the majority of adolescents in the current sample were White, above average SES, and from intact families, and that there were demographic differences between the test and retest samples, future studies should focus on examination of the psychometric properties of the PDRQ:P/A in a more demographically representative sample in order to address its limited generalizability.
Several additional methodological limitations are noteworthy. The sample was recruited online and via mail, so we did not have direct contact with participants and are unable to report the total number families approached or reasons for decline. Moreover, it is not known why 24 adolescents did not complete the PDRQ:A (i.e., whether they declined or never received the email from their parents). This method also precluded obtaining estimates of Hemoglobin A1C via laboratory or point of care analyses. Future research should examine relations between glycemic control and diabetes-specific routines. Finally, test–retest data should be interpreted with caution given that only online participants were recruited, 35.5% of the sample participated, and there were demographic differences between the retest and overall samples.
Incorporation of routines into the diabetes regimen is a recognized and important focus of diabetes management, but the limited availability of measures impeded widespread evaluation of diabetes-specific routines. The present study found promising results for the PDRQ:P/A, as a multi-informant measure of the frequency of diabetes-specific routines. The PDRQ affords researchers and clinicians the ability to examine routines specific to the diabetes regimen, rather than general routines in adolescents with T1D. The availability of a valid measure of diabetes-specific routines may provide researchers and clinicians the ability to feasibly document frequency of diabetes-specific routines. For researchers, the PDRQ:P/A provides a means to establish frequencies of diabetes-specific routines in observational or intervention studies. Future research should focus on evaluation of current routines and implementation of routines-based interventions in adolescents with T1D. The PDRQ:P/A may be useful in identifying and monitoring specific targets for such interventions. Clinically, the PDRQ:P/A could provide justification for further discussion between clinicians, patients, and their caregivers regarding forming routines around their specific T1D regimen. Low scores on the PDRQ:P/A could warrant referral to behavioral or educational resources.
References
Agarwal, S., Jawad, A. F., & Miller, V. A. (2015). A multivariate model exploring the predictive value of demographic, adolescent, and family factors on glycemic control in adolescents with type 1 diabetes. Pediatric Diabetes. https://doi.org/10.1111/pedi.12331.
American Diabetes Association. (2017). Standards of medical care in diabetes—2017. Diabetes Care, 40, 386–390. https://doi.org/10.2337/dc14-S014.
American Diabetes Association. (n.d.). The diabetes advisor: Hypoglycemia. Retrieved from https://professional.diabetes.org/sites/professional.diabetes.org/files/media/hypoglycemia.pdf. Accessed 20 Mar 2018.
Anderson, B., Auslander, W. F., Jung, K. C., Miller, J. P., & Santiago, J. V. (1990). Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15(4), 477–492.
Betz, C. L., & Redclay, G. (2005). An exploratory study of future plans and extracurricular activities of transition-age youth and young adults. Issues in Comprehensive Pediatric Nursing, 28(1), 33–61. https://doi.org/10.1080/01460860590916753.
Brown, T. A. (2006). Confirmatory factor analysis for applied research. New York: Guilford Press.
Bureau of Labor Statistics. U.S. Department of Labor. (2017). Employment and unemployment among youth summary. Retrieved September 29, 2017, from https://www.bls.gov/news.release/youth.nr0.htm.
Crespo, C., Santos, S., Canavarro, M. C., Kielpikowski, M., Pryor, J., & Féres-Carneiro, T. (2013). Family routines and rituals in the context of chronic conditions: A review. International Journal of Psychology. https://doi.org/10.1080/00207594.2013.806811.
Fiese, B., Winter, M., Anbar, R., Howell, K, & Poltrock, S. (2008). Family climate of routine asthma care: Associating perceived burden and mother-child interaction patterns to child well-being. Family Process, 47(1), 63–79. https://doi.org/10.1111/j.1545-5300.2008.00239.x.
Fiese, B. H., Wamboldt, F. S., & Anbar, R. D. (2005). Family asthma management routines: Connections to medical adherence and quality of life. Journal of Pediatrics. https://doi.org/10.1016/j.jpeds.2004.08.083.
Greening, L., Stoppelbein, L., Konishi, C., Jordan, S. S., & Moll, G. (2007). Child routines and youths’ adherence to treatment for type 1 diabetes. Journal of Pediatric Psychology, 32(4), 437–447. https://doi.org/10.1093/jpepsy/jsl029.
Hilliard, M. E., Wu, Y. P., Rausch, J., Dolan, L. M., & Hood, K. K. (2013). Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. Journal of Adolescent Health, 52(1), 28–34. https://doi.org/10.1016/j.jadohealth.2012.05.009.
Hollingshead, A. B. (1975). A four-factor index of social status. New Haven, CT: Yale University Sociology Department.
Hood, K. K., Butler, D. A., Anderson, B. J., & Laffel, L. M. B. (2007). Updated and revised diabetes family conflict scale. Diabetes Care, 30(7), 1764–1769. https://doi.org/10.2337/dc06-2358.
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118.
Lewin, A. B., Geffken, G. R., Heidgerken, A. D., Duke, D. C., Novoa, W., Williams, L. B., & Storch, E. A. (2005). The diabetes family behavior checklist: A psychometric evaluation. Journal of Clinical Psychology in Medical Settings, 12(4), 315–322. https://doi.org/10.1007/s10880-005-7817-x.
Lewin, A. B., LaGreca, A. M., Geffken, G. R., Williams, L. B., Duke, D. C., Storch, E. A., & Silverstein, J. H. (2009). Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The self-care inventory (SCI). Journal of Pediatric Psychology, 34(9), 999–1007. https://doi.org/10.1093/jpepsy/jsp032.
Lord, J. H., Young, M. T., Gruhn, M. A., Grey, M., Delamater, A. M., & Jaser, S. S. (2015). Effect of race and marital status on mothers’ observed parenting and adolescent adjustment in youth with type 1 diabetes. Journal of Pediatric Psychology, 40(1), 132–143. https://doi.org/10.1093/jpepsy/jsu078.
Markowitz, J. T., Garvey, K. C., & Laffel, L. M. B. (2015). Developmental changes in the roles of patients and families in type 1 diabetes management. Current Diabetes Reviews, 11(4), 231–238.
Markson, S., & Fiese, B. (2000). Family rituals as a protective factor for children with asthma. Journal of Pediatric Psychology, 25(7), 471–479. https://doi.org/10.1093/jpepsy/25.7.471.
Mellin, A. E., Neumark-Sztainer, D., Patterson, J., & Sockalosky, J. (2004). Unhealthy weight management behavior among adolescent girls with type I diabetes mellitus: The role of familial eating patterns and weight-related concerns. Journal of Adolescent Health, 35, 278–289. https://doi.org/10.1016/j.jadohealth.2003.10.006.
Meyer, K. J. (2008). Development and validation of the Adolescent Routines Questionnaire: Parent and self-report. Unpublished doctoral dissertation, Louisiana State University, Baton Rouge. Retrieved from http://etd.lsu.edu/docs/available/etd-11062008130552/unrestricted/Meyer_diss.pdf. Accessed 20 Mar 2018.
Muthén, L. K., & Muthén, B. O. (2007). Mplus user’s guide (5th ed.). Los Angeles: Muthén & Muthén.
Pierce, J. S., & Jordan, S. S. (2012). Development and evaluation of the Pediatric Diabetes Routines Questionnaire. Children’s Health Care, 41(1), 56–77. https://doi.org/10.1080/02739615.2012.643290.
Rausch, J., Hood, K. K., Delamater, A., Shroff Pendley, J., Rohan, J. M., Reeves, G., … Drotar, D. (2012). Changes in treatment adherence and glycemic control during the transition to adolescence in type 1 diabetes. Diabetes Care, 35, 1219–1224.
Schafer, L. C., Glasgow, R. E., McCaul, K. D., & Dreher, M. (1983). Adherence to IDDM regimens: Relationship to psychosocial variables and metabolic control. Diabetes Care, 6(5), 493–498. https://doi.org/10.2337/diacare.6.5.493.
Schafer, L. C., McCaul, K. D., & Glasgow, R. E. (1986). Supportive and nonsupportive family behaviors: Relationships to adherence and metabolic control in persons with type I diabetes. Diabetes Care, 9(2), 179–185. https://doi.org/10.2337/diacare.9.2.179.
Schreier, H. M. C., & Chen, E. (2010). Longitudinal relationships between family routines and biological profiles among youth with asthma. Health Psychology, 29(1), 82–90. https://doi.org/10.1037/a0018311.
Vesco, A. T., Anderson, B., Laffel, L., Dolan, L. M., Ingerski, L. M., & Hood, K. K. (2010). Responsibility sharing between adolescents with type 1 diabetes and their caregivers: Importance of adolescent perceptions on diabetes management and control. Journal of Pediatric Psychology, 35(11), 68–1177.
Wasserman, R. M., Hilliard, M. E., Schwartz, D. D., & Anderson, B. J. (2015). Practical strategies to enhance executive functioning and strengthen diabetes management across the lifespan. Current Diabetes Reports, 15(8), 52. https://doi.org/10.1007/s11892-015-0622-5.
Weinger, K., Butler, H. A., Welch, G. W., & La Greca, A. M. (2005). Measuring diabetes self-care: A psychometric analysis of the Self-Care Inventory-revised with adults. Diabetes Care, 28(6), 1346–1352. https://doi.org/10.2337/diacare.28.6.1346.
Wiebe, S., Guyatt, G., Weaver, B., Matijevic, S., & Sidwell, C. (2003). Comparative responsiveness of generic and specific quality-of-life instruments. Journal of Clinical Epidemiology, 56(1), 52–60.
Wysocki, T. (1993). Associations among teen-parent relationships, metabolic control, and adjustment to diabetes in adolescents. Journal of Pediatric Psychology, 18(4), 441–452. https://doi.org/10.1093/jpepsy/18.4.441.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Jessica S. Pierce has received funding from National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (Grant #: 1DP3DK108198-01). Authors Sara S. Jordan and Randolph C. Arnau declare no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pierce, J.S., Jordan, S.S. & Arnau, R.C. Development and Validation of the Pediatric Diabetes Routines Questionnaire for Adolescents. J Clin Psychol Med Settings 26, 47–58 (2019). https://doi.org/10.1007/s10880-018-9563-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-018-9563-x