Abstract
Recently, self-care in children and adolescents with type 1 diabetes has changed with regard to both adherence to treatment and self-management. Only one diabetes self-care scale for children and adolescents is used in Japan which lacks reflection on flexible regimens. The aims of this study were to modify and subsequently test the validity of the revised diabetes self-care inventory (R-DSCI) for children and adolescents, and to construct the diabetes self-care model on the R-DSCI, HbA1c, duration of diabetes and age. Based on qualitative secondary analysis of the self-care framework for teenagers and a literature review of diabetes self-care instruments, the items concerning insulin injection and meal planning were modified from the original DSCI and new items concerning negotiation with parents and others were added. The participants in the validity testing were 122 children and adolescents with type 1 diabetes, 50.8% were girls, aged 9–18 years, mean HbA1c of 7.9%. The final version of the R-DSCI was composed of 41 items. Eight factors, which explained 40.9% of the variance, were identified using the varimax method; Cronbach’s alpha for the 41 items was 0.79. The diabetes self-care model showed a negative direct effect of “diabetes self-care practice” on HbA1c (P = 0.004), and the negative indirect effect of “support and perception of life with diabetes” on HbA1c through “diabetes self-care practice” (P = 0.002; estimated effect − 0.21). In addition, “independent self-care behavior” was directly affected by age (P < 0.001). The R-DSCI should be useful for clinicians and researchers to assess the self-management in children and adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children and adolescents with type 1 diabetes have to manage their own diabetes in daily life, and the demands of this change as they grow and develop. They must self-manage multiple routines at home, at school, and in the community, and need to become experts with regard to their own diabetes. Recently, self-care in children with type 1 diabetes has changed in terms not only of their adherence to ideal regimens, but also the self-management that flexible regimens demand [1].
In Japan, the annual incidence of type 1 diabetes for 2005–2010 in children younger than age 15 was reported to be 2.25/100,000/year [2]; this is more than one tenth lower than in Europe or North America. Japanese children and adolescents with type 1 diabetes experience various difficulties resulting from the low incidence of type 1 diabetes, for example lack of understanding from others; the insulin pump with Japanese display was not available until 2015. Nonetheless, insulin treatment has progressed significantly in Japan. The control of blood glucose in children and adolescents improving, such that the mean HbA1c of Japanese children and adolescents with type 1 diabetes is now < 8.0% [3]. The most frequent cause of death among 53 Japanese diabetic patients who were < 20 years old between 2001 and 2010 was malignancy (22; 41.5%); diabetic coma with hyperglycemia accounted for 6 (11.3%), and no deaths were caused by hypoglycemic coma [4]. However, the ‘diabetes camp’ for children with type 1 diabetes has 50 places per year, and although the training of diabetes educators has been improving, many are still not well prepared to care for children and adolescents with type 1 diabetes and their parents, especially during transition periods. Disparities in diabetes education occur alongside differences in the number of pediatric patients with type 1 diabetes and in the insulin treatment regimens used, among the hospitals and regions in Japan.
Children and adolescents with type 1 diabetes require continuous diabetes education, based on evaluation of their competence in self-care. During the past two decades, the focus of research in children and adolescents with type 1 diabetes has been shifting to the development of effective education programs for the promotion of self-management [5, 6]. Self-care scales require assessment not only of the frequency with which elements of an ideal diabetes regimen are performed, but also of the problem-solving and collaboration with parents or between health care professionals participating in flexible regimens. However, while many diabetes self-care scales for children and adolescents have been developed in other countries, only the diabetes self-care inventory (DSCI) for children and adolescents has been used in Japan [7]. The DSCI for children and adolescents was used to explore self-care behavior in relation to health habits [8], lifestyle [9], school life [10], stress coping [11], and body fatness [12]. Although the DSCI was used in nursing intervention in diabetes clinics, this scale had limited flexibility in response to changes in insulin regimens or lifestyle.
The aims of this study were to modify the existing scale and test the validity of the revised diabetes self-care inventory (R-DSCI) for children and adolescents and to construct a diabetes self-care model using subscales from the R-DSCI, HbA1c and duration of diabetes as clinical indicators, and age as a growth indicator.
Methodology
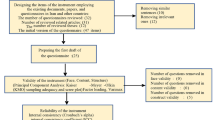
Development of the R-DSCI for children and adolescents
The original DSCI for children and adolescents was developed by Kanematsu in 1997 and contained 30 items to be self-reported, on a three-point Likert scale. The DSCI assesses multidimensional self-care behaviors: nutrition, insulin injection, self-monitoring of blood glucose, coping with hypoglycemia, exercise, and daily life. Each self-care behavior comprises three domains: skill and knowledge, independence, and feelings. The DSCI is composed of five subscales: F1: Self-care behavior through collaboration with parents (6 items), F2: Self-care behavior initiated by the patient alone (11 items), F3: Feelings toward self-care behavior (5 items), F4: Independent self-care behavior (5 items), and F5: Evaluation of blood glucose control (3 items). Cronbach’s alpha for the DSCI is 0.76. The limitation of the original scale is a lack of flexibility with regard to the incorporation of new technologies in diabetes care. Therefore, a qualitative secondary analysis of the self-care framework for teenagers living with diabetes [13] and a literature review of diabetes self-care instruments [14] were conducted to facilitate modification of the DSCI.
Qualitative secondary analysis The framework focuses on the accumulated experiences of teenagers since being diagnosed with type 1 diabetes, to identify potential new items for inclusion and to modify existing items in the instrument. Consequently, a self-care framework was constructed consisting of the following two phases: “primary diabetes self-care behavior” and “living with diabetes”. The first phase “primary diabetes self-care behavior” is a learning process leading to the mastering of diabetes self-care behavior. The second phase “living with diabetes” is a learning process in which children acquire appropriate self-care skills in many situations, and learn to cope with diabetes in their daily life. Perceptions of life with diabetes and support from family, friends, and others were important components in the second phase. Positive perceptions, seeking support, negotiation, and sufficient support lead them to perform appropriate diabetes self-care in their daily life. The self-care framework for teenagers with type 1 diabetes is shown in Fig. 1.
Literature review of diabetes self-care instruments A search for studies of diabetes self-care instruments for children and adolescents was conducted using CINAHL, MEDLINE, Academic Search Premier, and PsycINFO. Eighteen diabetes self-care instruments were identified, some of which focused on assessing the frequency with which elements of an ideal diabetes regimen were performed [15,16,17]. Many of these instruments were developed before 1999, while other instruments focusing on the essential components of continuous appropriate self-management [18,19,20,21] were developed after 2000.
From these analyses, 17 items were identified for inclusion in the Revised DSCI (R-DSCI), and eight items regarding insulin pump use and flexible dietary management using carbohydrate counting were modified. The relevance and clarity of these additional and modified items were assessed and proofed by a panel of experts consisting of six Japanese pediatric diabetes researchers and one certified diabetes educator.
The modified items were insulin injection (five items; nos. 26, 27, 28, 29, 30) and meal planning (three items; nos. 22, 23, 25). The added items were negotiation with parents, medical staff, and school teachers (five items; nos. 9, 13, 14, 16, 17), support from friends (three items; nos. 10, 12, 15), perception of diabetes and diabetic complications (four items; nos. 5, 7, 43, 44), daily life habits (two items; nos. 3, 4), and three other items (nos. 6, 24, 46). The first revised version of the DSCI (R-DSCI) was composed of 47 items that could be rated on a three-point Likert scale. The score range is thus 47–141, with higher scores indicating better self-care.
Participants
Participants were recruited from diabetes outpatient clinics and peer support groups. The inclusion criteria were children in grades 3–12, aged 9–18, who had been diagnosed with type 1 diabetes ≥ 6 months previously. The exclusion criteria were having cognitive or perceptual difficulties in completing the questionnaire, or other chronic conditions that could impact the individual’s diabetes self-care.
Procedures
Participants were recruited from three diabetes outpatient clinics and five peer support groups from six prefectures in Japan. Measurements were made by researchers. When attending routine clinics or peer support group events, the children and adolescents who fulfilled the inclusion criteria were invited to participate in the study. Informed consent was obtained from both children or adolescents and parents. This study was approved by the ethics committee of Chiba University Graduate School of Nursing (13 Oct 2015, nos. 27–59).
All participants completed demographic and clinical reports, which included their age, gender, duration of diabetes, insulin pump use, and HbA1c; and the R-DSCI. They were asked to return the reports and R-DSCI to the researchers using paid return envelopes. A subset of 28 participants was asked to complete a second R-DSCI 4 weeks later, to evaluate test–retest reliability, but only six participants (21.4%) completed this.
Statistical analysis
Analysis was conducted using the IBM Statistical Package for Social Science (SPSS) version 21. Missing data were estimated using the missing value analysis of SPSS. Item-level missing data ranged from 0 to 5 (0.0–4.1%). Correlation of items with the total R-DSCI scale, and the item mean and standard deviation were calculated.
Data analysis was conducted in three phases, according to the objective of the study. The first phase of the analysis, that of construct validity, was conducted by explanatory factor analysis using the varimax rotation method. An iterative process of repeated factor analysis was conducted to identify the most suitable factor structure, with factor loadings > 0.3 given to factors with eigenvalues of > 1.0 and good alpha reliabilities. The reliability of the R-DSCI was determined using Cronbach’s alpha. Correlations of items with subscales were also calculated. In addition, test–retest reliability was evaluated using a subset of the original group. The second phase of the analysis sought to correlate study variables and compare these with insulin regimens (MDI vs. CSII) and genders (male vs. female). Total and subscale scores on the R-DSCI were correlated with metabolic control (HbA1c), age, and duration of diabetes, using Pearson’s method. Total and subscale scores on the R-DSCI were compared according to insulin regimen and gender using unpaired two tailed t tests. The third phase of the analysis involved construction of a diabetes self-care model, using subscales of the R-DSCI, HbA1c, and duration of diabetes as clinical indicators, and age as a growth indicator, by covariance structure analysis using AMOS 21 software.
Results
Sample characteristics
Of the 212 potential participants who were approached, data were collected from 123 children and adolescents (response rate 58.0%). The most frequent reason for non-participation was that potential participants did not come to outpatient clinics or peer support group events during the study. One individual was excluded because this case was in grade 2. All cases completed at least 43 items on the R-DSCI (≥ 90%); therefore, n = 122 for analysis. The demographic characteristics of the participants were: 50.8% girls, age 13.1 ± 2.7 years old, duration of diabetes 6.8 ± 4.2 years, and HbA1c 7.9 ± 0.9% (Table 1).
Validity of the R-DSCI
Each item-to-total correlation was above 0.3 (P < 0.05). All 47 items were included in an explanatory factor analysis. Six items “Have you been admitted to hospital for hypoglycemia or ketosis within the past year? (no. 6)”, “Do you have close friends who have diabetes? (no. 12)”, “Do your teachers at school pay attention to you and help you? (no. 13)”, “Do you eat too much in secret without your parents’ knowledge? (no. 24)”, “Do you have ways of making sure you don’t forget your insulin injections or bolus? (no. 30)”, “When you go out, do you take a snack with you to prevent hypoglycemia? (no. 41)” were eliminated, because each item’s factor loading was low. There were nine factors with eigenvalues of > 1.0. A scree plot display of the eigenvalues indicated that the data could be summarized using eight factors. The final version was composed of 41 items and eight factors: F1: Support from family and attitude toward diabetes self-care (8 items), F2: Regularity of snacks and insulin injection (6 items), F3: Support at school and perception of life with diabetes (8 items), F4: Self-monitoring of blood glucose and daily life (5 items), F5: Independent self-care behavior (4 items), F6: Physical activity (3 items), F7: Nutrition and goal of blood glucose control (5 items), and F8: Discussions with medical staff/teachers (2 items). The eight factors explained 40.86% of the variance. The item loading range was 0.30–0.72 (Table 2). A histogram of R-DSCI total score indicated that it was normally distributed. The mean R-DSCI score was 97.5 ± 8.7, with a range of 74–121, skewness − .14, and kurtosis 0.01.
Reliability of the R-DSCI
The Cronbach’s alpha for the 41 items was 0.79 and for the subscales was 0.53–0.75. Correlations between item-to-subscale scores were 0.41–0.84 (P < 0.01). The correlation between F5 and total score was 0.20 (P < 0.05), and those between other subscales and total score were 0.37–0.70 (P < 0.01). Item numbers, means (SDs), and Cronbach’s alpha coefficients for the eight factors in the R-DSCI are shown in Table 2. Test–retest reliability for the R-DSCI was estimated using a subset (n = 6) of the 122 cases and found to be stable (r = 0.87, P < 0.05) in this small sample.
Comparisons between genders, insulin regimens and correlations among study variables
Total and subscale scores on the R-DSCI were compared according to gender using unpaired t tests (Table 3). Only one subscale, F5: Physical activity score of boys, was significantly higher than that of girls (t = 2.39, P < 0.05). Total and subscale scores on the R-DSCI were compared according to insulin regimen using unpaired t tests (Table 4). Only one subscale, F4: Self-monitoring of blood glucose and daily life, the score of CSII was significantly higher than that of MDI (t = − 2.44, P < 0.05).
Table 5 shows the correlations between total or subscale scores on the R-DSCI and HbA1c, age, or duration of diabetes. The total score (r = −0.24, P < 0.05) and three subscale scores, F2: Regularity of snacks and insulin injection (r = −0.27, P < 0.01), F4: Self-monitoring of blood glucose and daily life (r = −0.21, P < 0.05), and F7: Nutrition and goal of blood glucose control (r = −0.23, P < 0.05), were significantly negatively correlated with HbA1c. Appropriate self-care was associated with good blood metabolic control. The total score (r = −0.24, P < 0.05) and four subscale scores were significantly negatively correlated with age. F5: Independent self-care behavior was significantly correlated with age (r = 0.48, P < 0.01). The total score (r = −0.22, P < 0.05) and one subscale score were significantly negatively correlated with duration of diabetes.
The diabetes self-care model created using subscales of the R-DSCI, and clinical and growth indicators
Based on the correlations between subscales of the R-DSCI and study variables, a hypothetical model was tested repeatedly. The three subscales F1, F3, and F8, were used as composite indicators for a latent “support and perception of life with diabetes” construct. The four subscales F2, F4, F6, and F7, were used as composite indicators for a latent “diabetes self-care practice” construct. Because subscale F5 was a factor that was not significantly correlated with other subscales, it was included in the model as a possible confounder. HbA1c, age, and duration of diabetes were found to be associated with some of the subscales of the R-DSCI; therefore, these were included in the model. The final model had a good fit, with χ2 = 52.99, df = 40, P = 0.08, χ2(52.99)/df(40) = 1.32, CFI 0.91, RMESA 0.05, and AIC 126.99 (Fig. 2). This model shows a negative direct effect of “diabetes self-care practice” on HbA1c (P = 0.004) and a negative indirect effect of “support and perception of life with diabetes” on HbA1c through “diabetes self-care practice” (P = 0.002; estimated effect − 0.21). The model shows a negative direct effect of age on “diabetes self-care practice” (P = 0.001) and a positive direct effect of age on F5: Independent self-care behavior (P < 0.001). In addition, the model shows a negative direct effect of duration of diabetes on “support and perception of life with diabetes” (P = 0.03).
Discussion
Two principal conclusions can be drawn from this study. First, only one diabetes self-care scale for children and adolescents has been used in Japan, and this has been modified to improve its flexibility and to add items to reflect the self-care framework. Of the items on the R-DSCI, 41 self-reported measures were shown to have acceptable scale and subscale reliability (α = 0.79 and 0.53–0.74, respectively). Cronbach’s alpha of F8: Discussions with medical staff/teachers was a little lower (α = 0.53), but this factor contained only two items. Test–retest reliability for the R-DSCI was stable (r = 0.87, P < 0.05) in a small sample, a histogram of the R-DSCI total score indicated that it was normally distributed, and the R-DSCI revealed few gender differences. The R-DSCI thus reflected the flexible regimens currently used in diabetes care. It was then compared with the original DSCI factor structures. Two new factors, F3: Support at school and perception of life with diabetes and F8: Discussions with medical staff/teachers, were included in the R-DSCI. These two factors consist of the added items negotiation with others, support from friends, and perception of diabetes and diabetic complications. Our findings suggest that experience in daily school life influences the perception of life with diabetes in children and adolescents and, indeed, experiential learning was found to be key for adolescents to develop self-management skills and independence [22].
Second, a diabetes self-care model for children and adolescents was constructed using subscales of the R-DSCI, HbA1c, and duration of diabetes as clinical indicators, and age as a growth indicator. The model shows a positive direct effect of age on F5: Independent self-care behavior, but a negative direct effect of age on “diabetes self-care practice”. Although teenagers have sufficient cognitive maturity and problem-solving abilities to manage their disease, many adolescents show poor adherence to treatment regimens, because there is conflict between the needs of diabetes management and their social development and peer activities [23]. In addition, this model shows a direct effect of “diabetes self-care practice” on HbA1c, and an indirect effect of “support and perception of life with diabetes” on HbA1c through “diabetes self-care practice”. Support from parents and others, and children’s perception of life with diabetes were indirect factors that were important for good metabolic control. The subscale F5: Independent self-care behavior was a factor that did not significantly correlate with other subscales, and age alone had a positive direct effect on F5; therefore, it was only included in the phase “primary diabetes self-care behavior” of the self-care framework. This diabetes self-care model, which was constructed using subscales of R-DSCI, HbA1c, duration of diabetes, and age, validated the self-care framework.
A diabetes education program focusing on the accumulated experiences of children and adolescents since being diagnosed with type 1 diabetes is required during the transition to the next life stage. The diabetes self-care model facilitates the development of such a diabetes education program, and the R-DSCI makes it possible to evaluate diabetes education programs in Japan. Clinicians and researchers should thus make use of the R-DSCI for the assessment of self-management by children and adolescents. Children and adolescents were able to reflect on their own self-care behaviors while completing the R-DSCI. The result shows that the F4: Self-monitoring of blood glucose and daily life score of CSII was significantly higher than that of MDI. CSII may reduce the sense of burden of daily diabetes management, especially in a school setting for children and adolescents. Recently, new blood glucose monitoring devices such as sensor-augmented pump and Flash Glucose Monitoring have become available in Japan. Several reports suggested that Flash Glucose Monitoring may improve mental well-being among individuals in Japan with type 1 diabetes [24]. Continued investigation is required to explore the effects these new blood glucose monitoring devices have on diabetes self-care of children and adolescents.
Limitations of the present study include relatively small sample sizes, especially for test–retest reliability, and Cronbach’s alpha for F8 was low. Although sample size is an inevitable problem because of the low incidence of type 1 diabetes in Japan, further studies should evaluate the reliability of the R-DSCI using larger sample sizes. In addition, self-care by younger children with type 1 diabetes and the support given for self-care by their parents require further investigation.
References
Hanas R. Type 1 diabetes in children, adolescents and young adults. 4th ed. London: Class Publishing; 2010.
Onda Y, Sugihara S, Ogata T, Yokoya S, Yokoyama T, Tajima N. Incidence and prevalence of childhood-onset Type 1 diabetes in Japan: the T1D study. Diabet Med. 2017;34(7):909–15.
Mochizuki M, Kikuchi T, Urakami T, Kikuchi N, Kawamura T, Yokomichi H, Hoshino T, Matsuura N, Sasaki N, Sugihara S, Amemiya S. Japanese Study Group of Insulin Therapy for Childhood Adolescent Diabetes (JSGIT). Improvement in glycemic control through changes in insulin regimens: findings from a Japanese cohort of children and adolescents with type 1 diabetes. Pediatr Diabetes. 2017;18(6):435–42.
Nakamura J, Kamiya H, Haneda M, Inagaki N, Tanizawa Y, Araki E, Ueki K, Nakayama T. Causes of death in Japanese patients with diabetes based on the results of a survey of 45,708 cases during 2001-2010: report of the committee on causes of death in diabetes mellitus. J Diabetes Investig. 2017;8(3):397–410.
Lange K, Swift P, Pankowska E, Danne T. ISPAD Clinical Practice Consensus Guidelines 2014. Diabetes education in children and adolescents. Pediatr Diabetes. 2014;15(Suppl. 20):77–85.
Martin D, Lange K, Sima A, Kownatka D, Skovlund S, Danne T, Robert J. Recommendations for age-appropriate education of children and adolescents with diabetes and their parents in the European Union. Pediatr Diabetes. 2012;13(Suppl. 16):20–8.
Kanematsu Y, Nakamura N, Uchida M. Construction and validation of diabetic self-care behaviors Questionnaire for children and adolescents. J School Nurs Chiba Univ. 1997;19:71–8.
Kanematsu Y, Nakamura N, Uchida M, Tani H, Miyamoto S, Sugihara S, Konda S, Sasaki N, Nihmi H. Self-care behaviors and health behaviors of children with diabetes mellitus. J Child Health. 1997;56(6):777–83.
Nakamura N, Kanematsu Y, Takeda J, Maru M, Matsuoka M, Uchida M, Ninomiya K, Konno M, Tani H. Health habits and self-care behaviors of children with insulin-dependent diabetes mellitus in relation to lifestyle of their parents. J Jpn Acad Nurs Sci. 1999;19(3):74–82.
Kuniyoshi M, Gushiken M, Miyagi K, Gajya S. Self-care behavior of diabetic children and its practice in school life. J Jpn Acad Diabetes Educ Nurs. 2003;7(2):107–14.
Nakamura N, Kanematsu Y. Stress and coping behavior of drinking, smoking and eating with diabetic teenagers: comparison with health teenagers, and longitudinal change. J Jpn Acad Diabetes Educ Nurs. 1998;1(2):76–83.
Nakamura N, Ideno K, Tokuda T, Konno M, Kanematsu Y. Body fatness and influence factors of type 1 diabetes mellitus in children and adolescents, and self-awareness of their body weight. J Chiba Acad Nurs Sci. 2001;7(1):1–6.
Nakamura N, Ideno K, Kanamaru T, Tani H, Shirahata N, Utsumi K, Nakai A, Sato N, Kanematsu Y. An integrative review of the learning process of self-care behavior in young children with type 1 diabetes. J Chiba Acad Nurs Sci. 2012;18(1):1–9.
Nakamura N, Kanamaru T, Nakai A, Kanematsu Y. Diabetes self-care instruments for children and adolescents with type 1 diabetes: a literature review. J Jpn Acad Diabetes Educ Nurs. 2016;20(1):41–7.
Saucier CP, Clark LM. The relationship between self-care and metabolic control in children with insulin-dependent diabetes mellitus. Diabetes Educ. 1993;19(2):133–5.
Hanson CL, De Guire MJ, Schinkel AM, Kolterman OG, Goodman JP, Buckingham BA. Self-care behaviors in insulin-dependent diabetes: evaluative tools and their associations with glycemic control. J Pediatr Psychol. 1996;21(4):467–82.
Lewin AB, LaGreca AM, Geffken GR, Williams LB, Duke DC, Storch EA, Silverstein JH. Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: the self-care inventory (SCI). J Pediatr Psychol. 2009;34(9):999–1007.
Schilling LS, Dixon JK, Knafl KA, Lynn MR, Murphy K, Dumser S, Grey M. A new self-report measure of self-management of type 1 diabetes for adolescents. Nurs Res. 2009;58(4):228–36.
Ellis DA, Templin TN, Moltz K, Naar-King S, Dekelbab B, Carcone AI. Psychometric properties of the revised parental monitoring of diabetes care questionnaire in adolescents with type 1 diabetes. J Adolesc Health. 2012;50(3):289–95.
Cox ED, Fritz KA, Hansen KW, Brown RL, Rajamanickam V, Wiles KE, Fate BH, Young HN, Moreno MA. Development and validation of PRISM: a survey tool to identify diabetes self-management barriers. Diabetes Res Clin Pract. 2014;104(1):126–35.
Cooper H, Spencer J, Lancaster GA, Titman A, Johnson M, Wheeler SL, Lwin R. Development and psychometric testing of the online adolescent diabetes needs assessment tool (ADNAT). J Adv Nurs. 2014;70(2):454–68.
Spencer JE, Cooper HC, Milton B. The lived experiences of young people (13-16 years) with Type 1 diabetes mellitus and their parents–a qualitative phenomenological study. Diabet Med. 2013;30(1):e17–24.
Cameron FJ, Amin R, de Beaufort C, Codner E, Acerini CL. ISPAD clinical practice consensus guidelines 2014: diabetes in adolescence. Pediatr Diabetes. 2014;15(Suppl. 20):245–56.
Mitsuishi S, Nishimura R, Harashima SI, Kawamura T, Tsujino D, Koide K, Nishimura A, Utsunomiya K, Inagaki N, Atsumi Y. The effect of novel glucose monitoring system (flash glucose monitoring) on mental well-being and treatment satisfaction in Japanese people with diabetes. Adv Ther. 2018;35(1):72–80.
Acknowledgements
This study was funded by JSPS KAKENHI Grant number JP16K12136. The authors acknowledge the late Professor Yuriko Kanematsu who made a great contribution to our studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients before being included in the study.
Conflicts of interest
The authors declare that they have no conflicts of interests.
About this article
Cite this article
Nakamura, N., Yakushijin, Y., Kanamaru, T. et al. Development and validity testing of the revised diabetes self-care inventory for children and adolescents. Diabetol Int 10, 117–125 (2019). https://doi.org/10.1007/s13340-018-0377-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-018-0377-8