Abstract
As the prevalence of post-traumatic stress disorder (PTSD) among children discharged from pediatric intensive care unit (PICU) continues to rise, corresponding research efforts have also increased. This scoping review aimed to review the PTSD prevalence, influencing factors, and tools used for PTSD measurements in children discharged from the PICU. This review employed the five-stage framework proposed by Arksey and O’Malley. The data sources included PubMed, Web of Science, Ovid, ScienceDirect, Springer, Scopus, CNKI, and WANFANG. Studies in English or Chinese published up to September 2023 were eligible for inclusion. The search yielded a total of 3536 results, with 31 articles meeting the inclusion criteria. The included studies reported that the prevalence of PTSD ranged from a minimum of 13% to a maximum of 84.6%. Risk factors for PTSD included medical interventions, child-related factors, and family environment. A total of 17 assessment tools for PTSD in PICU patients were reported. Given the significance of PTSD in this pediatric population, further attention, research, and intervention are warranted to help alleviate the burden of PTSD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The pediatric intensive care unit (PICU) is a specialized ward in a hospital, offering critical medical care at the highest level to children with severe illnesses or injuries [1]. With advancements in medical treatment and technology in recent years, the survival rate of PICU patients has increased significantly [2]. However, the number of PICU patients continues to grow, with 1.5 million children annually admitted to the PICU in the United States [2]. Many of these pediatric survivors experience ongoing post-traumatic stress disorder (PTSD) following discharge from the PICU, underscoring the importance of addressing psychological issues [2, 3].
PTSD is a psychological disorder in individuals experiencing or witnessing severe traumatic events such as war, sexual assault, accidents, or natural disasters, leading to prolonged and persistent psychological and emotional distress [4]. In the context of PICU, PTSD manifests in children undergoing treatment who exhibit re-experience, avoidance, and hypervigilance of traumatic experiences following severe illness, surgery, or other significant medical interventions [2, 5]. For instance, Als et al. examined 88 children discharged from the PICU after 5 months and found that 20% of the children exhibited symptoms of PTSD such as excessive arousal, restlessness, hyperactivity, and behavioral issues [6]. Compared with healthy peers, 7–12% of children discharged from the PICU experience more depressive emotions and social difficulties, indicative of PTSD avoidance behaviors [7]. Traumatic memories, including delusional recollections, flashbacks, and hallucinations, have been reported in children after discharge from the PICU [8], posing adverse effects not only on their quality of life but also on their learning abilities and social skills [9,10,11].
De Pellegars et al. conducted a systematic literature review of factors influencing PTSD in PICU patients and included English and French literature published between January 1, 2004, and January 31, 2022 [12]. The present study extended this search to Chinese and English articles published until September 2023, not only aiming to summarize the impact of PTSD in PICU patients following discharge, but also providing an overview of the incidence of PICU-related PTSD and presenting a review of commonly used assessment tools for PTSD in pediatric patients to establish the foundation for clinical practice and future research in the PICU.
Aims
We aimed to determine the incidence of PTSD in patients discharged from the PICU, identify the factors influencing the development of PTSD in these patients, and evaluate the available assessment tools for measuring PTSD in patients post-PICU discharge.
Methods
Trustworthiness and rigor
This scoping review followed Arksey and O’Malley’s [13] five-stage framework, which adopts a rigorous and transparent process, increasing the reliability of research outcomes. This five-stage scoping review model includes the following: (i) Defining the research query; (ii) Pinpointing pertinent research; (iii) Selecting research articles; (iv) Visualizing data; and (v) Summarizing and presenting findings [13].
Defining the research question
The central question guiding this scoping review was as follows: What is the prevalence of PTSD in children after discharge from the PICU, and what are the associated risk factors and tools used to measure it?
Keywords used for searching
Expert input from the field of child psychology was sought to refine the search terms and identify the most appropriate databases for obtaining the desired search results. Various search techniques, including the use of PTSD descriptors and Boolean operators, such as “and,” “or,” and “not” or “and not” were employed to refine, expand, and combine literature searches. Table 1 contains a descriptive list of the key search terms devised to direct the exploration.
Eligibility criteria
Inclusion and exclusion criteria were established by the research team to ensure that the scope aligned with the research objectives and maximized relevance to the research query. Table 2 presents a comprehensive list of the inclusion and exclusion criteria.
Search methods
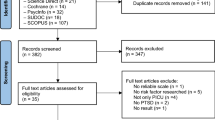
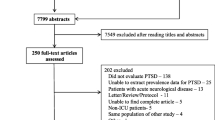
The scoping review protocol was registered on INPLASY (No. INPLASY2023110 068) and adhered to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines. Using key search descriptors, we searched the PubMed, Web of Science, Ovid, ScienceDirect, Springer, Scopus, CNKI, and WANFANG databases. An example keyword search strategy from PubMed is presented in Table 3.
Study selection
All identified article references were imported into the EndNote X9 citation management software (Thomson Reuters, Philadelphia, PA, USA). Subsequently, one researcher removed duplicates and independently assessed the articles based on their titles and abstracts to gauge their relevance to the research question (Fig. 1). Then, two reviewers (T.M.T. and C.M.C.) independently screened the full-text articles strictly according to the inclusion and exclusion criteria and cross-checked the results. In cases of disagreement, the two reviewers discussed any disputes with the third reviewer (C.P.L.), who made the final decision.
Data extraction
Standardized data extraction forms were created by the research team. Two reviewers independently extracted and compared the data. The abstract information encompassed details such as author, publication year, study location, research design, assessment tools, and follow-up time.
Quality assessment
The quality of the studies included in this review was assessed using the Mixed Methods Appraisal Tool (MMAT) [14]. The MMAT serves as a valuable quality assessment instrument applicable to a range of study types, including quantitative, qualitative, and mixed-method research. Although the MMAT was employed to assess the studies’ quality in this review, no studies were excluded solely based on their scores.
Data analysis
Using descriptive synthesis, we organized the outcomes of the included articles. Initially, essential details such as authors, study design, assessment tools, and post-discharge follow-up duration were extracted from each study. Because the articles contained limited numerical data, a meta-analysis could not be conducted. The data were thematically organized and visually presented through tables to synthesize the information, and concise summaries were provided for the primary findings of each study. Finally, limitations in the literature were reflected upon, and potential future research directions were discussed.
Results
Attributes of the included studies
Following the application of the inclusion and exclusion criteria, a considerable number of articles were deemed ineligible, had inappropriate study subjects or research settings, or were abstracts or duplicates. A total of 87 papers were chosen for a thorough review. Of these, 56 publications were excluded due to inappropriate study participants, inappropriate research settings, and abstract-only publications or duplicates. Ultimately, 31 articles were included in this review. Figure 1 shows a PRISMA flow chart.
This scoping review identified 31 independent studies from 10 countries: Australia [15,16,17,18,19,20], the Netherlands [1, 21, 22], the United Kingdom (UK) [5, 6, 23,24,25,26,27,28,29,30], Canada [31, 32], the United States (US) [33,34,35,36,37], Thailand [38], France [39], Egypt [40], China [41] and India [42]. These included 20 prospective studies [1, 5, 6, 15,16,17,18,19,20,21,22,23, 26, 29, 30, 32,33,34, 39, 42], two retrospective studies [24, 38], two randomized trials [37, 41], two case–control studies [25, 28], two secondary data analyses [31, 35], and one of each of the following study types: exploratory study [27], longitudinal study [36], and comparative cross-sectional study [40]. The PICU sample sizes varied from eight [34] to 272 [19], with a mean of 72 participants. Patients’ ages ranged from 0 [1] to 18 years [24], and the study follow-up time ranged from 1 week [38] to 1 year [16]. Table 4 presents the full details of the included studies and provides insights into the attributes and outcomes of each study.
Quality of the included studies
The quality assessment results of the MMAT indicated that most of the studies fell within the moderate to good range. Among the 29 quantitative non-randomized studies, two had dropout rates exceeding 20% [20, 33], and one with a 1-year follow-up had a dropout rate exceeding 30% [39]. Of the two quantitative randomized controlled trials, one study implemented blinding for outcome assessors [37], and the other employed a random number table method [41].
PTSD in pediatric patients after discharge from the PICU
A study conducted in the Netherlands that compared child survivors (8–17 years) of a major fire incident using the Dutch Children’s Responses to Trauma Inventory (CRTI), found that more than one-third (34.5%) of these children in the PICU had subclinical PTSD [21]. Another study conducted in the PICU on Multisystem Inflammatory Syndrome in Children (MIS-C) at 3–6 months post-discharge found that among 30 children, 10 (33%) were at an increased risk of developing PTSD [1]. Boeschoten et al. [22] compared Dutch children in the PICU with those from regular wards at 5 months post-discharge, and higher scores on the PTSD questionnaire were reported among children in the PICU. Another study in the UK found that 62% of children exhibited PTSD symptoms following discharge from the PICU, with 10% displaying characteristics of acute stress disorder [23]. A study conducted in India compared a group of PICU patients to a control group with a similar number of comorbidities and comparable temperament and found that experiences of PTSD-related intrusive thoughts were significantly higher in the PICU group (43%) than in the control group (6.7%) [42]. However, a study performed in America that randomly assigned 1360 pediatric patients from the PICU to a sedation protocol group and a standard care group [37] revealed no statistically significant difference in PTSD scores 6 months after discharge [37].
Risk factors for PTSD
The development of PTSD is a complex process influenced by many factors that interact with each other [16, 19, 26]. Colville et al. [5] conducted a study on 102 children in the PICU using the Impact of Event Scale (IES), and they found that the duration of opioid/benzodiazepine use was associated with PTSD-related intrusive memories at 3 months after discharge (odds ratio, 4.98; 95% confidence interval [CI], 1.3–20.0; P < 0.023). In a study involving two PICUs in Australia, Long et al. [16] found that intubation, PICU length of stay, and use of midazolam, propofol, and morphine were significantly associated with PTSD 1 month after discharge [16]. Dow et al. [20] found that treating pediatric patients with ketamine in the PICU had a significant impact on PTSD at 6 months post-discharge.
Three studies investigated the relationship between PTSD and cortisol [25, 26, 34]. One study examined the baseline cortisol levels of 47 children in the PICU, revealing a significant positive correlation between PTSD and nighttime cortisol concentrations (p = 0.004) [25]. Another UK-based study that collected saliva samples from pediatric patients with sepsis in the PICU found that the use of corticosteroids may be associated with fewer PTSD symptoms and lower nighttime cortisol levels [26]. A study conducted in the US involving eight PICUs found that the severity of PTSD symptoms increased over time, while salivary cortisol levels decreased at 2 weeks and 3 months post-discharge [34]. Besides cortisol research, a study involving 71 pediatric patients from two PICUs found a significant positive correlation between IES-8 scores and high C-reactive protein levels (r = 0.823; p = 0.006, n = 11) during follow-up [27].
Rennick et al. [31] conducted a study involving 60 PICU patients in Canada and found that children exposed to a high number of invasive surgeries had higher PTSD scores at 6 weeks after discharge. Through a follow-up study of 120 PICU patients, they also found that individuals who underwent more invasive surgeries exhibited significantly greater medical phobia and sustained traumatic stress reactions at 6 months post-discharge [32]. However, Tippayawong et al. [38] demonstrated a negative correlation between mechanical ventilation and PTSD. Le Brocque et al. [19] conducted a study in Australia and found that the length of stay in the PICU for children aged 2–16 years was a potential risk factor for PTSD 12 months after discharge. Als et al. [6] extracted data from 88 PICU patients and compared them with 100 healthy individuals; they found that the length of stay in the PICU was a predictive factor for PTSD [6].
Five studies found cognitive and emotional factors to be associated with PTSD [17, 20, 28, 36, 39]. Among them, Dow et al. [17] conducted research on 95 PICU patients aged 6–16 and found that cognitive/emotional factors were related to PTSD at 3 weeks after discharge. In another study, cognitive processing and traumatic memory significantly and independently influenced PTSD in children 6 months post-discharge [20]. Elison et al. [28] compared a group of PICU patients to a control group and found a significant correlation between PTSD and emotional/behavioral scores in the PICU group. Another study discovered that anxiety and depression symptoms might also be independent factors affecting PTSD in PICU patients [39]. Stowman et al. [36] found that anxiety, negative emotions, and hospital-related fear among adolescents in the PICU mediated initial acute stress disorder symptoms and later PTSD symptoms in youths.
Three studies found an association between the age of PICU patients and PTSD [17, 19, 32]. Dow et al. [17] conducted an investigation of 95 children in the PICU, Le Brocque et al. [19] conducted a study of Australian children in the PICU, and Rennick et al. [32] performed a study comparing 120 PICU children with children in regular wards; they all found that younger age was associated with greater distress and PTSD.
Le Brocque et al. [19] found that pre-illness functioning, the mothers’ perception of threat to life, and the mothers’ acute distress had an impact on PTSD in pediatric patients in the PICU. Additionally, Bronner et al. [21] found that maternal PTSD was the strongest predictive factor for PTSD in children in the PICU. Furthermore, Rennick et al. [32] discovered that children with more severe medical conditions were more susceptible to developing PTSD.
Assessment tools for measuring PTSD
This scoping review included 17 distinct assessment tools [43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] related to PTSD which are listed in Table 5.
Discussion
The long-term psychological and life consequences for PTSD-affected children constitute a complex and extensive issue. These enduring effects encompass a spectrum of challenges, including anxiety, depression, traumatic memories, and emotional distress [29]. Moreover, PTSD may have adverse effects on academic performance, disrupt social relationships, and even lead to a breakdown of family dynamics for children [60].
In this scoping review, the included studies reported the prevalence of PTSD, ranging from a minimum of 13% [33] to a maximum of 84.6% [40]. The lowest incidence was reported by Nelson et al., who found that among 69 PICU patients aged 8–17 years in California, 13% were found to have PTSD at 3 months after discharge [33]. The highest incidence was reported by Rady et al., who investigated 130 PICU children aged 6–13 years in Egypt. In comparison to the general ward group, the PICU group exhibited a significantly higher prevalence of PTSD after discharge (84.6% and 6.2%, respectively; p < 0.001) [40]. This variation may be attributed to several factors, including differences in study design, sample characteristics, cultural variations, PTSD measurement time, and the assessment tools used [21, 23, 33, 36]. In a substantial number of studies, the prevalence of PTSD fell within the range of 20–40%, suggesting that out of every 100 PICU patients, 20–40 may experience PTSD or exhibit PTSD symptoms [29, 36, 39]. This highlights a significant proportion of PICU patients experiencing PTSD, emphasizing the need for further exploration into the factors influencing PTSD and the development of tailored interventions. These findings also underscore the necessity of addressing psychological issues in PICU patients to foster their recovery and holistic development.
This scoping review summarizes PTSD risk factors, encompassing medical interventions (medication use, invasive surgeries, and mechanical ventilation) [5, 31, 38], child-related factors (age, cortisol levels, and cognitive and emotional factors) [19, 32], and family environment (maternal psychological status and the presence of maternal PTSD) [19].
For medical interventions, the studies suggested that commonly used medications in the PICU, including opioids, benzodiazepines, and midazolam, are associated with PTSD in children [5, 16, 20]. This may be because prolonged or excessive use of opioids and benzodiazepines can lead to tolerance and dependency, with withdrawal symptoms upon discontinuation, potentially affecting psychological well-being [5]. The use of midazolam may be linked to the processing of memories and emotions related to trauma. These substances enhance the action of the neurotransmitter gamma-aminobutyric acid, producing inhibitory effects. In certain situations, this influence may interfere with the normal processing of trauma [16]. A strong association was found between treatments in the PICU, particularly invasive procedures such as intubation, surgery, blood draws, and catheter placement, and PTSD in pediatric patients [31, 32]. This might be because invasive procedures are often accompanied by pain and physiological discomfort, especially for pediatric patients. They may feel fear, anxiety, or helplessness, feeling a loss of control over their own situation [31]. These memories may leave a profound impression on the child’s psyche, becoming potentially triggering factors for PTSD.
In this scoping review, we included a diverse range of assessment tools for PTSD measurements in pediatric patients discharged from the PICU. These tools demonstrated varying degrees of reliability and validity, making them suitable for research and clinical applications related to PTSD. Notably, the Trauma Symptom Checklist for Young Children, developed for the assessment of trauma-related symptoms in children ages 3–12, exhibited strong internal consistency across its various subscales [43]. The Children’s Revised Impact of Event Scale (CRIES), designed for use with children aged 8 years and above who are able to read independently, showed high internal consistency and was effective in measuring intrusion, avoidance, and arousal symptoms. [45]. Other versions, such as CRIES-8 and CRIES-13, displayed acceptable psychometric properties and were useful in distinguishing children with and without PTSD symptoms [45, 46]. The IES demonstrated good internal consistency and was moderately correlated with depression and self-esteem measures, and it is validated for use in children aged 8 and older [47]. The Clinician-Administered Post-Traumatic Stress Disorder Scale for Children (CAPS-C) showed strong interrater reliability, enhancing its clinical utility for younger children; information from parents is used to assess symptoms using the CAPS-C [48]. The CRTI exhibited excellent internal consistency and strong convergent validity with the CRIES, and is used for children aged eight to 18 [50]. These tools offer valuable options for assessing PTSD in pediatric patients post-PICU discharge, with the choice depending on research or clinical needs. The diversity of these tools underscores the complexity of evaluating PTSD in this population; research goals, age groups, cultural sensitivity, and psychometrics should be considered when selecting an assessment tool. Future research and clinical work should choose suitable tools to improve accuracy in diagnosing and treating PTSD in children discharged from the PICU.
Limitations
This scoping review has some limitations. First, it was confined to the availability of accessible published literature containing defined or related terms. Second, the scoping review only included articles written in English and Chinese; thus, articles in other languages may have provided additional evidence. Third, with regard to the quality assessment of the literature, some entries of the MMAT lacked objective evaluation criteria, and the assessment of the results may have involved some degree of subjectivity. Finally, some of the included studies used assessment tools beyond their intended age range, which could have potentially affected the results.
Practice implications
This review reports a wide prevalence range for PTSD in children discharged from PICUs, ranging from 13 to 84.6%. It also sheds light on the multitude of risk factors associated with the development of PTSD in children discharged from PICUs, including medical procedures, child characteristics, and the family environment. This review serves as a valuable resource for healthcare professionals, equipping them with the knowledge needed to identify high-risk individuals and administer appropriate care. By considering the risk factors, doctors, nurses, and psychologists can tailor treatment plans effectively, ultimately mitigating psychological distress in children. The review also highlights 17 assessment tools that can be utilized in clinical settings, offering guidance on selecting the most suitable methods for different patient groups. This serves to enhance the precision and efficacy of diagnosis, thereby improving overall patient care.
Conclusions
In summary, PTSD in pediatric patients following PICU hospitalization presents a complex issue with profound effects on children. Variability in the incidence rates and the diversity of influencing factors make the identification of PTSD and subsequent intervention challenging. Future research should focus on in-depth investigations of neuroscience, biology, assessment tools, and cross-cultural factors to facilitate early identification of potential traumatic events in PICU patients, along with providing psychological support, education, and appropriate treatment, which can mitigate or prevent the development of PTSD.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Otten MH, Buysse CMP, Buddingh EP, Terheggen-Lagro SWJ, von Asmuth EGJ, de Sonnaville ESV, Ketharanathan N, Bunker-Wiersma HE, Haverman L, Hogenbirk K, de Hoog M, Humblet M, Joosten KFM, Kneyber MCJ, Krabben G, Lemson J, Maas NM, Maebe S, Roeleveld PP, van Schooneveld M, Timmers-Raaijmaakers B, van Waardenburg D, Walker JC, Wassenberg R, van Woensel JBM, de Wit E, Wolthuis DW, van Zwol A, Oostrom KJ, Knoester H, Dulfer K (2023) Neurocognitive, psychosocial, and quality of life outcomes after multisystem inflammatory syndrome in children admitted to the PICU. Pediatr Crit Care Med 24:289–300. https://doi.org/10.1097/PCC.0000000000003180
Talat H (2023) Pediatric Intensive Care Unit (PICU): Providing Critical Care for Children. Linkedin, in www.linkedin.com/pulse/pediatric-intensive-care-unit-picu-providing-critical-heba-talat/
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ, Brady SL, Brodsky MB, Denehy L, Elliott D, Flatley C, Harabin AL, Jones C, Louis D, Meltzer W, Muldoon SR, Palmer JB, Perme C, Robinson M, Schmidt DM, Scruth E, Spill GR, Storey CP, Render M, Votto J, Harvey MA (2012) Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med 40:502–509. https://doi.org/10.1097/CCM.0b013e318232da75
Aupperle RL, Melrose AJ, Stein MB, Paulus MP (2012) Executive function and PTSD: disengaging from trauma. Neuropharmacology 62:686–694. https://doi.org/10.1016/j.neuropharm.2011.02.008
Colville G, Kerry S, Pierce C (2008) Children’s factual and delusional memories of intensive care. Am J Respir Crit Care Med 177:976–982. https://doi.org/10.1164/rccm.200706-857OC
Als LC, Picouto MD, Hau SM, Nadel S, Cooper M, Pierce CM, Kramer T, Garralda ME (2015) Mental and physical well-being following admission to pediatric intensive care. Pediatr Crit Care Med 16:e141–e149. https://doi.org/10.1097/PCC.0000000000000424
Davydow DS, Richardson LP, Zatzick DF, Katon WJ (2010) Psychiatric morbidity in pediatric critical illness survivors: a comprehensive review of the literature. Arch Pediatr Adolesc Med 164:377–385. https://doi.org/10.1001/archpediatrics.2010.10
Rennick JE, Rashotte J (2009) Psychological outcomes in children following pediatric intensive care unit hospitalization: a systematic review of the research. J Child Health Care 13:128–149. https://doi.org/10.1177/1367493509102472
De Young AC, Landolt MA (2018) PTSD in children below the age of 6 years. Curr Psychiatry Rep 20:97. https://doi.org/10.1007/s11920-018-0966-z
Frem T (2013) PTSD in preschool children: a review and synthesis of research on the need for a separate DSM category. Concept 36
Hamblen J, Barnett E (2016) PTSD in children and adolescents. National Center for PTSD. http://www.georgiadisaster.info/Schools/fs%207%20school/PTSD%20in%20Children%20&%20Adolescents.pdf
De Pellegars A, Cariou C, Le Floch M, Duverger P, Boussicault G, Riquin E (2023) Risk factors of post-traumatic stress disorder after hospitalization in a pediatric intensive care unit: a systematic literature review. Eur Child Adolesc Psychiatry. https://doi.org/10.1007/s00787-023-02141-8Epub ahead of print
Arksey H, O’Malley J (2005) Scoping reviews: towards a methodological framework. Int J Soc Res Methodol 8:19–32. https://doi.org/10.1080/1364557032000119616
Souto RQ, Khanassov V, Hong QN, Bush PL, Vedel I, Pluye P (2015) Systematic mixed studies reviews: updating results on the reliability and efficiency of the mixed methods Appraisal Tool. Int J Nurs Stud 52:500–501. https://doi.org/10.1016/j.ijnurstu.2014.08.010
Dow BL, Kenardy JA, Le Brocque RM, Long DA (2013) The diagnosis of posttraumatic stress disorder in school-aged children and adolescents following pediatric intensive care unit admission. J Child Adolesc Psychopharmacol 23:614–619. https://doi.org/10.1089/cap.2013.0044
Long D, Gibbons K, Le Brocque R, Schults JA, Kenardy J, Dow B (2022) Midazolam exposure in the paediatric intensive care unit predicts acute post-traumatic stress symptoms in children. Aust Crit Care 35:408–414. https://doi.org/10.1016/j.aucc.2021.06.004
Dow BL, Kenardy JA, Long DA, Le Brocque RM (2019) Cognitive/affective factors are associated with children’s acute posttraumatic stress following pediatric intensive care. Psychol Trauma 11:55–63. https://doi.org/10.1037/tra0000349
Dow BL, Kenardy JA, Le Brocque RM, Long DA (2012) The utility of the children’s revised impact of event scale in screening for concurrent PTSD following admission to intensive care. J Trauma Stress 25:602–605. https://doi.org/10.1002/jts.21742
Le Brocque RM, Dow BL, McMahon H, Crothers AL, Kenardy JA, Williams TJ, Long DA (2020) The course of posttraumatic stress in children: examination of symptom trajectories and predictive factors following admission to pediatric intensive care. Pediatr Crit Care Med 21:e399–e406. https://doi.org/10.1097/PCC.0000000000002316
Dow BL, Kenardy JA, Le Brocque RM, Long DA (2023) Cognitive predictors of posttraumatic stress in children 6 months after Paediatric Intensive Care unit admission. Trauma Care 3:82–92. https://doi.org/10.3390/traumacare3020009
Bronner MB, Knoester H, Bos AP, Last BF, Grootenhuis MA (2008) Posttraumatic stress disorder (PTSD) in children after paediatric intensive care treatment compared to children who survived a major fire disaster. Child Adolesc Psychiatry Ment Health 2:9. https://doi.org/10.1186/1753-2000-2-9
Boeschoten SA, Dulfer K, Boehmer ALM, Merkus PJFM, van Rosmalen J, de Jongste JC, de Hoog M, Buysse CMP, Dutch collaborative PICU research network (SKIC) (2020) Quality of life and psychosocial outcomes in children with severe acute asthma and their parents. Pediatr Pulmonol 55:2883–2892. https://doi.org/10.1002/ppul.25034
Judge D, Nadel S, Vergnaud S, Garralda ME (2002) Psychiatric adjustment following meningococcal disease treated on a PICU. Intensive Care Med 28:648–650. https://doi.org/10.1007/s00134-002-1237-2
Rees G, Gledhill J, Garralda ME, Nadel S (2004) Psychiatric outcome following paediatric intensive care unit (PICU) admission: a cohort study. Intensive Care Med 30:1607–1614. https://doi.org/10.1007/s00134-004-2310-9
Als LC, Picouto MD, O’Donnell KJ, Nadel S, Cooper M, Pierce CM, Kramer T, Glover VAS, Garralda ME (2017) Stress hormones and posttraumatic stress symptoms following paediatric critical illness: an exploratory study. Eur Child Adolesc Psychiatry 26:511–519. https://doi.org/10.1007/s00787-016-0933-3
Corbet Burcher G, Picouto MD, Als LC, Cooper M, Pierce CM, Nadel S, Garralda ME (2018) Post-traumatic stress after PICU and corticosteroid use. Arch Dis Child 103:887–889. https://doi.org/10.1136/archdischild-2017-314157
Caspani G, Corbet Burcher GC, Garralda ME, Cooper M, Pierce CM, Als LC, Nadel S (2018) Inflammation and psychopathology in children following PICU admission: an exploratory study. Evid Based Ment Health 21:139–144. https://doi.org/10.1136/ebmental-2018-300027
Elison S, Shears D, Nadel S, Sahakian B, Garralda ME (2008) Neuropsychological function in children following admission to paediatric intensive care: a pilot investigation. Intensive Care Med 34:1289–1293. https://doi.org/10.1007/s00134-008-1093-9
Colville G, Pierce C (2012) Patterns of post-traumatic stress symptoms in families after paediatric intensive care. Intensive Care Med 38:1523–1531. https://doi.org/10.1007/s00134-012-2612-2
Colville GA, Pierce CM (2013) Children’s self-reported quality of life after intensive care treatment. Pediatr Crit Care Med 14:e85–e92. https://doi.org/10.1097/PCC.0b013e3182712997
Rennick JE, Morin I, Kim D, Johnston CC, Dougherty G, Platt R (2004) Identifying children at high risk for psychological sequelae after pediatric intensive care unit hospitalization. Pediatr Crit Care Med 5:358–363. https://doi.org/10.1097/01.pcc.0000128603.20501.0d
Rennick JE, Johnston CC, Dougherty G, Platt R, Ritchie JA (2002) Children’s psychological responses after critical illness and exposure to invasive technology. J Dev Behav Pediatr 23:133–144. https://doi.org/10.1097/00004703-200206000-00002
Nelson LP, Lachman SE, Li SW, Gold JI (2019) The effects of family functioning on the development of posttraumatic stress in children and their parents following admission to the PICU. Pediatr Crit Care Med 20:e208–e215. https://doi.org/10.1097/PCC.0000000000001894
Board R, Dai J (2011) Effects of five parent-and-child risk factors on salivary cortisol levels and symptoms of posttraumatic stress disorder in school-age, critically ill children: pilot study. Heart Lung 40:236–246. https://doi.org/10.1016/j.hrtlng.2010.05.051
Olszewski AE, Dervan LA, Smith MB, Asaro LA, Wypij D, Curley MAQ, Watson RS (2023) Risk factors for positive post-traumatic stress disorder screening and associated outcomes in children surviving acute respiratory failure: a secondary analysis of the randomized evaluation of sedation titration for respiratory failure clinical trial. Pediatr Crit Care Med 24:222–232. https://doi.org/10.1097/PCC.0000000000003150
Stowman S, Kearney CA, Daphtary K (2015) Mediators of initial acute and later posttraumatic stress in youth in a PICU. Pediatr Crit Care Med 16:e113–e118. https://doi.org/10.1097/PCC.0b013e31822f1916
Watson RS, Asaro LA, Hertzog JH, Sorce LR, Kachmar AG, Dervan LA, Angus DC, Wypij D, Curley MAQ, RESTORE Study Investigators, the Pediatric Acute Lung Injury and Sepsis Investigators (2018) Long-term outcomes after Protocolized Sedation versus Usual Care in Ventilated Pediatric patients. Am J Respir Crit Care Med 197:1457–1467. https://doi.org/10.1164/rccm.201708-1768OC
Tippayawong P, Chaiyakulsil C (2022) Incidence and associated factors of pediatric post-intensive care syndrome using the VSCAREMD model. Acute Crit Care 37:627–635. https://doi.org/10.4266/acc.2022.00234
Fergé JL, Banydeen R, Le Terrier C, Fize H, Miguel M, Kentish-Barnes N, Jehel L, Moroy A, Valentino R, Mehdaoui H (2021) Mental health of adolescent relatives of intensive care patients: benefits of an open visitation policy. Am J Crit Care 30:72–76. https://doi.org/10.4037/ajcc2021799
Rady HI, Ismail OR, Abdelkader MS, Abdelgalil AA (2020) Increased psychiatric risk in children after pediatric Intensive Care Unit admission. J Nerv Ment Dis 208:147–151. https://doi.org/10.1097/NMD.0000000000001123
Mingming G, Yingying L, Dong M, Linxi H (2020) Application of psychological nursing intervention based on stress system theory in post-traumatic stress disorder of children in major traffic accidents. Chin J Mod Nurs 26:5
Muranjan MN, Birajdar SB, Shah HR, Sundaraman P, Tullu MS (2008) Psychological consequences in pediatric intensive care unit survivors: the neglected outcome. Indian Pediatr 45:99–103
Briere J, Johnson K, Bissada A, Damon L, Crouch J, Gil E, Hanson R, Ernst V (2001) The trauma symptom checklist for young children (TSCYC): reliability and association with abuse exposure in a multi-site study. Child Abuse Negl 25:1001–1014. https://doi.org/10.1016/s0145-2134(01)00253-8
Giannopoulou I, Smith P, Ecker C, Strouthos M, Dikaiakou A, Yule W (2006) Factor structure of the children’s revised impact of event scale (CRIES) with children exposed to earthquake. Pers Individ Dif 40:1027–1037. https://doi.org/10.1016/j.paid.2005.11.002
Deeba F, Rapee RM, Prvan T (2014) Psychometric properties of the children’s revised impact of events scale (CRIES) with Bangladeshi children and adolescents. PeerJ 2:e536. https://doi.org/10.7717/peerj.536
Echevarria-Guanilo ME, Dantas RAS, Farina JA, Alonso J, Rajmil LA, Rossi LA (2011) Reliability and validity of the impact of event scale (IES): version for Brazilian burn victims. J Clin Nurs 20:1588–1597. https://doi.org/10.1111/j.1365-2702.2010.03607.x
Stallard P, Salter E, Velleman R (2004) Posttraumatic stress disorder following road traffic accidents — a second prospective study. Eur Child Adolesc Psychiatry 13:172–178. https://doi.org/10.1007/s00787-004-0399-6
John PB, Russell PSS (2007) Validation of a measure to assess post-traumatic stress disorder: a, sinhalese version of impact of event scale. Clin Pract Epidemiol Ment Health 3:4. https://doi.org/10.1186/1745-0179-3-4
Alisic E (2008) In: Vermetten E, Kleber RJ, van der Hart O (eds) Psychological assessment for children: questionnaires. [Utrecht: de tijdstroom uitgeverij]. Handboek Posttraumatische Stressstoornissen [Handbook of posttraumatic stress disorders]
Bertrand O, Philippe B, Eric B, Charlotte A, Alain B, Isabelle C, de Gauzy JS, Grandjean H, Raynaud JP (2014) Validation of the French version of the child post-traumatic stress reaction index: psychometric properties in French speaking schoolaged children. PLoS ONE 9:1–17. https://doi.org/10.1371/journal.pone.0112603
Koran LM (1975) The reliability of clinical methods, data, and judgments (first of two parts). N Engl J Med 293:642–646. https://doi.org/10.1056/NEJM197509252931307
Koran LM (1975) The reliability of clinical methods, data, and judgments (second of two parts). N Engl J Med 293:695–701. https://doi.org/10.1056/NEJM197510022931405
Stinchfield R, McCready J, Turner NE, Jimenez-Murcia S, Petry NM, Grant J, Welte J, Chapman H, Winters KC (2016) Reliability, validity, and classification accuracy of the DSM-5 diagnostic criteria for gambling disorder and comparison to DSM-IV. J Gambl Stud 32:905–922. https://doi.org/10.1007/s10899-015-9573-7
Yasik AE, Saigh PA, Oberfield RA, Green B, Halamandaris P, McHugh M (2001) The validity of the children’s PTSD inventory. J Trauma Stress 14:81–94. https://doi.org/10.1023/A:1007887615685
Foa EB, Johnson KM, Feeny NC, Treadwell KRH (2001) The child PTSD symptom scale: a preliminary examination of its psychometric properties. J Clin Child Psychol 30:376–384. https://doi.org/10.1207/S15374424JCCP3003_9
Sveen J, Low A, Dyster-Aas J, Ekselius L, Willebrand M, Gerdin B (2010) Validation of a Swedish version of the impact of event scale-revised (IES-R) in patients with burns. J Anxiety Disord 24:618–622. https://doi.org/10.1016/j.janxdis.2010.03.021
Brunet A, St-Hilaire A, Jehel L, King S (2003) Validation of a French version of the impact of event scale-revised. Can J Psychiatry 48:56–61. https://doi.org/10.1177/070674370304800111
Conybeare D, Behar E, Solomon A, Newman MG, Borkovec TD (2012) The PTSD checklist—civilian version: reliability, validity, and factor structure in a nonclinical sample. J Clin Psychol 68:699–713. https://doi.org/10.1002/jclp.21845
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosom Med 41:209–218. https://doi.org/10.1097/00006842-197905000-00004
Ekim A (2020) The post-intensive care syndrome in children. Compr Child Adolesc Nurs 43:15–21. https://doi.org/10.1080/24694193.2018.1520323
Acknowledgements
The authors extend their gratitude to the reviewers for dedicating their time and expertise to the thorough review of our manuscript.
Funding
This work was supported by the Medical Science and Technology Project of the Sichuan Health Committee (grant no. 21PJ055).
Author information
Authors and Affiliations
Contributions
Conceptualization: T.M.T., C.P.L., and C.M.C. Literature search and screening: T.M.T and L.X.L. Literature review and summarization: T.M.T and L.X.L. Writing the original draft, reviewing, and editing: T.M.T., C.P.L., and C.M.C. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent for participate
Not applicable.
Competing interests
The authors declare no competing interests.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tang, M., Chui, P.L., Chong, M.C. et al. Post-traumatic stress disorder in children after discharge from the pediatric intensive care unit: a scoping review. Eur Child Adolesc Psychiatry (2024). https://doi.org/10.1007/s00787-024-02505-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00787-024-02505-8