Most quality of life (QOL) assessments measure patients’ emotional well-being, functional well-being, interpersonal/social well-being, and satisfaction with treatment. Little attention has been given to patients’ spirituality or religiosity. Further, studies that have examined the impact of spirituality or religiosity on QOL have not differentiated between the constructs. The purpose of this study was to examine religiosity and spirituality as separate variables, and to define their relationship to QOL for 61 persons with cancer. Regression analyses indicated that, while spirituality and religiosity are moderately intercorrelated, spirituality has a stronger relationship with QOL than religiosity. When attempting to understand a person's spiritual life and its impact on QOL, there is a need for clear distinction between and separate assessment of spirituality and religiosity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the American Cancer Society (2005), 1,372,910 new cases of cancer were expected to be diagnosed in the year 2005. For many, the diagnosis of cancer is emotionally devastating (Burish & Lyles, 1981). People worry about their mortality and the physical and emotional rigors they face. Quality of life (QOL) may decrease due to treatment effects, relationship stressors, physical changes, and emotional impact. As persons with cancer face stressors related to their illness and the reality of death, existential and spiritual issues often come to the forefront. This study will examine how spirituality and religiosity are related to the quality of life of persons with cancer.
Although over 30 different dimensions of QOL have been described (Kornblith & Holland, 1994), primary QOL domains include emotional well-being, functional well-being, interpersonal well-being, treatment satisfaction, sexuality and intimacy, and social well-being. Spirituality has never been considered a “core” dimension of QOL, although researchers have argued that it should be (Brady, Peterman, Fitchett, Mo, & Cella, 1999). Research on the importance of spiritual well-being to overall QOL is lacking.
Of the many QOL assessments available, only three include the dimension of spirituality (Ferrans, 1994; Ferrell, Dow, Leigh, Ly, & Gulasekaram, 1995; Fitchett, Peterman, & Cella, 1996). Investigators have suggested that religious, spiritual, and existential concerns need to be included in QOL assessment (Bufford, Paloutzian, & Ellison, 1991; Donovan, Sanson-Fisher, & Redman, 1989). In one study that examined the association between spirituality and QOL in cancer patients (Brady et al., 1999), spirituality was associated with QOL to the same degree as physical well-being and emotional well-being, two domains unquestioned in their importance to QOL.
A major methodological issue when using the construct of spirituality is the lack of a consensus definition. The term spirituality is often interchanged with religiosity although they have different meanings. Spirituality has been defined as a person's unique search, which may or may not be as a member of an organized religion, for what is sacred in life (Larson, Swyers, & McCullough, 1997). A definition of religion (Thoresen, 1998) is an organized system of beliefs, practices, rituals, and symbols designed to facilitate a relationship to and understanding of a deity as well as to promote understanding and harmony of a person's relationship to oneself and others. Thoresen (1998) believes the major distinction between religiosity and spirituality is the social and institutional nature of religiosity compared to the more individual thrust and experience of spirituality.
Because there is overlap between the two terms, they are often treated as one in the research literature. If researchers do make a distinction between spirituality and religiosity, it seems to be the norm that the term spirituality is used more often to be more inclusive and universal (Elkins, Hedstrom, Hughes, Leaf, & Saunders, 1988; Ley & Corless, 1988; Reed, 1987). However, the construct of spirituality is typically measured in terms of traditional religious beliefs, attitudes, or behaviors (Levin, 1994). If research is based on measures of religious practice rather than spirituality, a segment of the population who describe themselves as spiritual but not religious will be omitted (George, Larson, Koenig, & McCullough, 2000). This is a conceptual error, as research has shown that dimensions of religiosity and/or spirituality may be differentially related to both physical and mental outcomes (Musick, Koenig, Larson, & Matthews, 1998). Assessing both of these constructs could examine each of their associations with QOL, as well as their combined relationship to QOL. Therefore, the purpose of this study is to consider spirituality and religiosity as separate constructs and to examine their relationships with QOL in cancer patients.
METHOD
Participants
Participants were patients reporting for a medical appointment in a specialized hematologic malignancy clinic of a midwestern NIH-designated Comprehensive Cancer Center. Hematologic malignancies include lymphoma, leukemia, myelodysplastic syndrome, multiple myeloma, myeleoproliferative non-Hodgkin's lymphoma, and Hodgkin's disease.
Patients who were at least 18 years of age, and diagnosed with a hematologic malignancy, were given a letter by their physician describing the study and were then approached by the first author who provided more information to interested patients. Seventy-five patients were asked to take part in the study, and 61 patients agreed. Refusal reasons included lack of time, interest, and/or energy, and scheduling conflicts.
Measures
Quality of life
The Functional Assessment of Cancer Therapy Scale — General (FACT-G; Cella et al., 1993) is a widely used 27-item questionnaire that measures participants’ global quality of life in the domains of physical, functional, social, and emotional well being. The FACT-G has high internal reliability (Cronbach α's from 0.72 to 0.85), and has been well-validated (Cella et al., 1993). Convergent validity was evaluated by examining scores on the FACT-G with the Functional Living Index-Cancer (FLIC), a measure of QOL (Schipper, Clinch, McMurray, & Leavitt, 1984); a shortened version of the Profile of Mood States (POMS) (Cella et al., 1987); and the Marlowe-Crowne Social Desirability Scale (M-CSDS) (Strahan & Gerbasi, 1972). The Pearson correlation with the FLIC was high (0.79). Correlations with mood distress on the POMS were high (−0.58 to −0.65). Correlation with social desirability, as measured by the M-CSDS, was low (r = 0.22), supporting divergent validity.
Spirituality
The Functional Assessment of Chronic Illness Therapy—Spiritual Well-Being (FACIT-Sp; Peterman, Fitchett, Brady, Hernandez, & Cella, 2002) was used to measure spirituality. The FACIT-Sp was developed with the collaboration of cancer patients, psychotherapists, and religious/spiritual experts. This 12-item scale covers aspects of spirituality, such as a sense of meaning in one's life, harmony, peacefulness, and a sense of strength and comfort. Examples of items are “I feel a sense of purpose in my life” and “I find comfort in my faith or spiritual beliefs.” This scale differs from other measures due to its emphasis on the existential and intrapersonal aspects of spirituality.
A report containing two separate studies supports the psychometric properties of the FACIT-Sp (Peterman et al., 2002). The first study utilized an ethnically diverse sample of 1,617 patients with chronic disease (cancer or HIV) and demonstrated adequate internal consistency reliability (Cronbach's α = .81–.88). Factor analysis of the FACIT-Sp produced two meaningful factors, one that measured the importance of faith and one that measured a sense of meaningfulness and purpose in life. FACIT-Sp scores were also significantly and positively associated with QOL measured by the FACT-G (physical well-being, r = 0.25; emotional well-being, r = 0.55) as well as total QOL scores (r = 0.58). The second study further validated the FACIT-Sp by examining its relationship to existing measures of religion and spirituality. The authors proposed that moderate correlations above .30 between the FACIT-Sp and other religion measures would support convergent validity whereas correlations above .80 would suggest duplication of an existing measure. The FACIT-Sp total score was significantly correlated with spiritual beliefs (r = .48), organizational religiousness (r = .34), nonorganizational religiousness (r = .31), and intrinsic religiousness (r = .41).
Religiosity
The Duke Religion Index (DUREL; Koenig, Parkerson, & Meador, 1997) was used to assess religiosity. This index contains five items. The first two items measure organizational and nonorganizational dimensions of religious practice and were taken from large community and clinical studies. The final three items were extracted from Hoge's 10-item intrinsic religiosity scale (Hoge, 1972). Principal component factor analysis of the original 10-item scale revealed an intrinsic and extrinsic factor. Three items were chosen on the basis of their high loading on the intrinsic factor, correlation with total score, and relationship with health outcomes. The 3-item subscale had a Cronbach's alpha of 0.75; it was strongly correlated with the original 10-item scale (r = 0.85), and correlated with the first two items assessing organizational (r = 0.40) and nonorganizational (r = 0.42) dimensions of religiosity. The total of the five items was used as the measure of religiosity for this study to encompass organizational and nonorganizational extrinsic aspects of religiosity as well as intrinsic aspects of religiosity.
Demographics
A demographic measure collected information about patients’ current living arrangement, religious affiliation, and religion in which one was raised (if any), occupation, education, relationship status, ethnicity, and income.
In addition to the measures completed by the patients, age, diagnosis, date of diagnosis, stage of disease, and current therapy were obtained from the patients’ charts. The attending physician completed a measure of patients’ performance status on the day they took part in the study using the Eastern Cooperative Oncology Group performance status rating system (PS) (Zubrod et al., 1960). In this instrument, 0 = normal activity, 1 = some symptoms, but no bedrest during daytime, 2 = bedrest less than 50% of daytime, 3 = bedrest more than 50% of daytime, and 4 = unable to get out of bed.
RESULTS
Sample Characteristics
Fifty-six percent of the sample was male, and 44% was female. The difference in gender may be explained by the tendency for more hematolgic malignancies to be diagnosed in men than in women (Greenlee, Hill-Harmon, Murray, & Thun, 2001). Table I presents further demographic information on the sample used.
The performance status (PS) of the sample revealed that participants in this study were healthy. Nearly 80% of the study participants reported no need for bedrest during the day. The remaining 20% of the sample reported daily bedrest. None of the participants who took part in the study were completely unable to get out of bed.
Spirituality and Religiosity
Responses to the FACIT-SP indicated that respondents rated themselves moderately high on this dimension (M/SD = 36.51/10.18 of a possible 48.00). A T-test revealed that the scores of the sample used in this study do not differ at the 0.05 level from the sample reported by Fitchett and colleagues (1996). FACIT-Sp scores were significantly and positively associated with overall QOL measured by the FACT-G (r = 0.72), a finding that replicated the work of Peterman et al. (2002).
The FACIT-Sp scores in this study displayed a high level of internal consistency (α = 0.92). FACIT-Sp scores were not significantly associated with gender, marital status, or ethnicity; they were significantly associated with current religious practice (r = 0.50, p = < .001). FACIT-Sp scores were not significantly associated with demographic variables of education, employment status, income, or current living arrangements. Previous data has indicated a significant relationship between total FACIT-Sp score and age, gender, marital status, ethnicity, and type of disease (Peterman et al., 2002). The lack of association in the current study may be due to the homogeneity of the sample used.
Nearly 97% of the subjects were raised in the Protestant or Catholic religion; 1.6% reported not being raised in any religion. 82% of the sample reported that they still practiced a religion. Scores of the first two DUREL items revealed that usual attendance at church or other religious meetings was reported as follows: at least once a week (33%), a few times a month (21%), a few times a year (5%), once a year or less (31%), and never (10%). Over half of the subjects reported that they spend time in private religious activities, such as prayer, meditation, or Bible study at least once a week, 31% stated they participate in such activities a few times a month, and 12% never take part in such activities.
Intrinsic religiosity of the sample measured by the last three items of the DUREL, revealed a mean score of 11.79 (SD = 2.68) out of a possible score of 15. A T-test comparing the mean score for intrinsic religiosity of the sample to the norms provided by the DUREL revealed that the study sample showed significantly lower intrinsic religiosity than the normative sample (M = 13.3) (t[2, 60] = −4.41, p < 0.001). Internal consistency for the final three items of the DUREL was high (α = 0.78). This is similar to the internal consistency measurement for the normative sample (α = 0.75).
Means, standard deviations, and correlations are presented in Table II. Preliminary bivariate correlations were computed to explore whether any of the demographic variables should be taken into account when examining the contributions of religiosity and spirituality to QOL. The PS, a measure of performance status rated by the patient's physician, was significantly and negatively correlated with QOL. Age was significantly correlated with PS. Therefore, both age and PS were included in the regression equations as demographic variables.
Regression Analyses
Results of the regression analyses are contained in Table III. In the first hierarchical multiple regression, PS and age accounted for 22% of the variance in QOL. In the second step of the regression model, religiosity added an additional 8% in the variance of QOL. Adding spirituality in the third step of the regression significantly augmented the equation, explaining an additional 29% in the variance. Age, performance status, religiosity, and spirituality accounted for 59% of the total variance in QOL, full model F(4, 53) = 20.86, p < 0.001.
In order to clarify the separate contribution of spirituality and religiosity to QOL, separate hierarchical regression analyses were conducted. The second regression analysis entered the variable of spirituality first, followed by religiosity. The analysis indicated that spirituality alone accounted for 51% of the variance, F(1, 59) = 64.33, p < 0.0001. Adding religiosity to the model did not significantly account for additional variance in QOL.
The third regression entered the variable of religiosity first, followed by spirituality. Religiosity accounted for 13% of the variance, F(1, 59) = 9.69, p < 0.003. Adding spirituality to the model accounted for an additional 38% of the variance. Spirituality accounts for a significant increment in the variance of QOL when religion is already in the model. When both spirituality and religiosity were in the model, 51% of the variance in QOL was accounted for.
DISCUSSION
This study attempted to clarify the separate contributions of spirituality and religiosity to quality of life among cancer patients. Data from patients diagnosed with a hematologic malignancy revealed that spirituality and religiosity were both related to quality of life. Spirituality accounted for more of variance in QOL than did religiosity; spiritual constructs such as feelings of peace and harmony, a sense of purpose, and spiritual beliefs more powerfully predict quality of life than constructs such as church attendance, time in religious activities, and religious beliefs.
While study participants had high levels of spirituality, only 33% of them attended a religious service weekly. Additionally, while nearly all participants were raised in religious homes, 15% of the sample no longer practiced any religion, despite high levels of spirituality. It seems spirituality is a personal practice that can develop regardless of one's exposure to religious activities while growing up. These findings support the idea that spirituality exists independent of membership in an organized religious body (Jenkins & Pargament, 1995; Simoni, Martone, & Kerwin, 2002).
In addition to the current study, two other studies have measured religiosity and spirituality as separate constructs in their relation to QOL in cancer patients. Borman and Nicholas (1999) measured quality of life, spirituality, and religiosity of 75 cancer patients within their first year of diagnosis. They found spirituality and stage of cancer to predict QOL, but not religiosity. Cotton, Levine, Fitzpatrick, Dold, and Targ (1999) measured the relationship between QOL and spirituality and religiosity in 130 women with breast cancer. They used two measures of spirituality, the FACIT-Sp, and the Principles of Living Survey (PLS; Thoresen et al., 1995). While the FACIT-Sp primarily focuses on spirituality, the PLS measures both religious and spiritual beliefs. Cotton and colleagues found a stronger association between the FACIT-Sp and QOL than between the PLS and QOL. It was suggested by the authors that the FACIT-Sp measures more internally-based constructs such as meaning, purpose, and strength, while the PLS focuses more on external factors such as religious practice, forgiveness, and connection to others and nature. The studies by Borman and Nicholas (1999) and Cotton et al. (1999) both revealed that spirituality is a better predictor of QOL than is religiosity.
The National Institute for Healthcare Research (NIHR) attempted to better clarify the relationship between spirituality and health by bringing together a group of well-respected researchers and scholars to discuss religion and spirituality as they relate to clinical health status. This group met during a series of three conferences and made detailed recommendations in a consensus report (Larson et al., 1997). The panel discussed the distinction and overlaps between religion and spirituality, and stated that attempts to measure spirituality as a separate construct from religion are difficult. They advocated against conceptualizing the terms as incompatible opposites, and labeling either term as good or bad. For instance, taking the stance that the individuality of spirituality is good, while the institutional nature of religion is bad should be avoided. The panel strongly indicated that these two phenomena are not independent of one another. The panel also suggested that neither religiosity nor spirituality can be measured by a single item measure, and recommended that many domains of religiousness/spirituality be measured.
Several limitations of the current study must be noted. Although attempts were made to clearly define the constructs of religiosity and spirituality, and to measure them separately, the current conceptualization and measurement of religiosity and spirituality may be limited or biased. The assessment tools may be restricted in their ability to wholly measure each construct.
Another limitation is that the sample may be unrepresentative of the population of those with cancer. The current sample tended to be older, White married individuals. Past research has shown that demographic variables of ethnicity, age, gender, marital status, education, and income have all been related to QOL and/or levels of religiosity/spirituality (Cotton et al., 1999; Holland et al., 1999; Kaczorowski, 1989; Mickley, Soeken, & Belcher, 1992; Peterman et al., 2002). However, no such significant relationships were found in the current study, possibly due to the homogeneity of the sample. The unrepresentative sample limits the generalizability of this study to mainly older, White males and females.
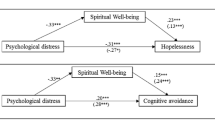
Future research needs include further clarification of the commonalities and distinctions of religiosity and spirituality. Longitudinal research with rigorous methodologies could determine if the relationship between religiosity and spirituality and quality of life is consistent over time, or consistent throughout specific disease processes. The use of more rigorous statistical analyses such as structural equation modeling could be helpful in exploring direct and indirect relationships among these variables.
In conclusion, spirituality and religiosity are both salient in the context of confronting a life-threatening illness such as cancer. Spiritual and/or religious beliefs may increase QOL by providing support for coping, developing a deeper understanding of life's meaning or purpose, and enhancing the will to live. Most important, the separate roles of spirituality and religiosity should be considered in evaluating for or intervening to improve cancer patients’ QOL.
REFERENCES
American Cancer Society. (2005). Statistics. [Online]. Available: http://www.cancer.org [2005, April].
Borman, P. D., & Nicholas, D. R. (1999, August). Spirituality, religiosity, and the quality of life of oncology patients. Paper presented at the Meeting of the American Psychological Association, Boston, MA.
Brady, M. J., Peterman, A. H., Fitchett, G., Mo, M., & Cella, D. (1999). A case for including spirituality in quality of life measurement in oncology. Psycho-Oncology, 8, 417–428.
Bufford, R. K., Paloutzian, R. F., & Ellison, C. W. (1991). Norms for the spiritual well-being scale. Journal of Psychology and Theology, 19, 56–70.
Burish, T. G., & Lyles, J. N. (1981). Effectiveness of relaxation training in reducing adverse reactions to cancer chemotherapy. Journal of Behavioral Medicine, 4, 65–78.
Cella, D. F., Jacobsen, P. B., Orav, E. J., Holland, J. C., Silberfarb, P. M., & Rafla, S. (1987). A brief POMS measure of distress for cancer patients. Journal of Chronic Disease, 40, 939–942.
Cella, D. F., Tulsky, D. S., Gray, G., Sarafian, B., Linn, E., Bonomi, A., et al. (1993). The functional assessment of cancer therapy scale: Development and validation of the general measure. Journal of Clinical Oncology, 11, 1–10.
Cotton, S. P., Levine, E. G., Fitzpatrick, C. M., Dold, K. H., & Targ, E. (1999). Exploring the relationships among spiritual well-being, quality of life, and psychological adjustment in women with breast cancer. Psycho-Oncology, 8, 429–438.
Donovan, K., Sanson-Fisher, R. W., & Redman, S. (1989). Measuring quality of life in cancer patients. Journal of Clinical Oncology, 7, 959–968.
Elkins, D. N., Hedstrom, L. J., Hughes, L. L., Leaf, J. A., & Saunders, C. (1988). Toward a humanistic phenomenological spirituality. Journal of Humanistic Psychology, 28, 5–18.
Ferrans, C. E. (1994). Quality of life through the eyes of survivors of breast cancer. Oncology Nursing Forum, 21, 1645–1651.
Ferrell, B. R., Dow, K. H., Leigh, S., Ly, J., & Gulasekaram, P. (1995). Quality of life in long-term cancer survivors. Oncology Nursing Forum, 22, 915–922.
Fitchett, G., Peterman, A., & Cella, D. F. (1996). Spiritual beliefs and quality of life in cancer and HIV patients. Paper presented at the Society for Scientific Study of Religion, Nashville, TN.
George, L. K., Larson, D. B., Koenig, H. G., & McCullough, M. E. (2000). Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology, 19, 102–116.
Greenlee, R. T., Hill-Harmon, M. B., Murray, T., & Thun, M. (2001). Cancer statistics, 2001. CA: A Cancer Journal for Clinicians, 51, 15–36.
Hoge, D. R. (1972). A validated intrinsic religious motivation scale. Journal for the Scientific Study of Religion, 11, 369–376.
Holland, J. C., Kash, K. M., Passik, S., Gronert, M. K., Sison, A., Lederberg, M., et al. (1999). The role of religious and spiritual beliefs in coping with malignant melanoma. Psycho-Oncology, 8, 14–26.
Jenkins, R. A., & Pargament, K. I. (1995). Religion and spirituality as resources for coping with cancer. Journal of Psychosocial Oncology, 13, 51–74.
Kaczorowski, J. W. (1989). Spiritual well-being and anxiety in adults diagnosed with cancer. Hospice Journal, 5, 105–116.
Koenig, H., Parkerson, G. R., & Meador, K. G. (1997). Religion index for psychiatric research. American Journal of Psychiatry, 153, 885–886.
Kornblith, A. B., & Holland, J. C. (Eds.). (1994). Handbook of measures of psychological, social and physical function in cancer: Vol 1. Quality of life. New York: Memorial Sloan-Kettering Cancer Center.
Larson, D., Swyers, J., & McCullough, M. (Eds.). (1997). Scientific research on spirituality and health: A consensus report. Rockville, MD: National Institute for Healthcare Research.
Levin, J. S. (1994). Religion and health: Is there an association, is it valid, and is it causal? Social Science and Medicine, 38, 1475–1482.
Ley, D. C. H., & Corless, I. B. (1988). Spirituality and hospice care. Death Studies, 12, 101–110.
Mickley, J. R., Soeken, K., & Belcher, A. (1992). Spiritual well-being, religiousness and hope among women with breast cancer. IMAGE: Journal of Nursing Scholarship, 24, 267–272.
Musick, M. A., Koenig, H. G., Larson, D. B., & Matthews, D. (1998). Religion and spiritual beliefs. In J. Holland (Ed.), Psycho-oncology (pp. 780–789). New York: Oxford University Press.
Peterman, A. H., Fitchett, G., Brady, M. J., Hernandez, L., & Cella, D. (2002). Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp). Annals of Behavioral Medicine, 24, 49–58.
Reed, P. G. (1987). Spirituality and well-being in terminally ill hospitalized adults. Research in Nursing and Health, 10, 335–344.
Schipper, H., Clinch, J., McMurray, A., & Leavitt, M. (1984). Measuring the quality of life of cancer patients: The Functional Living Index-Cancer: Development and validation. Journal of Clinical Oncology, 2, 472–483.
Simoni, J. M., Martone, M. G., & Kerwin, J. F. (2002). Spirituality and psychological adaptation among women with HIV/AIDS: Implications for counseling. Journal of Counseling Psychology, 49, 139–147.
Strahan, R., & Gerbasi, K. C. (1972). Short homogeneous versions of the Marlowe-Crowne Social Desirability Scale. Journal of Clinical Psychology, 28, 191–193.
Thoresen, C., Bowman, E., Koopman, C., Yang, P., Dubs, G., & Speigel, D. (1995). Principles of living survey. Department of Psychiatry, Stanford University.
Thoresen, C. E. (1998). Spirituality, health, and science: The coming revival? In S. Roth-Roemer, S. R. Kurpius, & C. Carmin (Eds.), The emerging role of counseling psychology in health care (pp. 409–431). New York: Norton.
Zubrod, C. G., Schneiderman, M., Frei, E., et al. (1960). Appraisal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thisphosphoramide. Journal of Chronic Diseases, 11, 7–33.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rippentrop, A.E., Altmaier, E.M. & Burns, C.P. The Relationship of Religiosity and Spirituality to Quality of Life Among Cancer Patients. J Clin Psychol Med Settings 13, 29–35 (2006). https://doi.org/10.1007/s10880-005-9000-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-005-9000-9