Abstract
Objective
The objectives of this study were (a) to determine the psychometric properties of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale and (b) to provide that FACIT scores behave one-dimensional to establish the mediating role of spiritual well-being in psychological distress and mental adjustment in a sample of patients with non-metastatic, resected cancer.
Method
A total of 504 consecutive patients completed the FACIT-Sp, Brief Symptom Inventory, and Mini-Mental Adjustment to Cancer scales. The dimensionality and structure of the scale were assessed by semi-confirmatory factor analysis; the reliability of the derived scale scores was evaluated using the omega coefficient, and regression analysis appraised the FACIT-Sp’s mediating role between psychological distress and mental adjustment.
Results
A clear and theoretically interpretable solution in two factors that agreed generally with solutions reported in other languages was obtained for the FACIT item scores and omega reliabilities of the derived Meaning/Peace (0.85) and Faith (0.86) scales were acceptable. The oblique solution in two factors was compatible with an essentially unidimensional solution of general well-being and associated strongly with psychological distress and mental adjustment. Spiritual well-being acted as a partial mediator between psychological distress and mental adjustment strategies, such as fighting spirit, hope, and cognitive avoidance.
Conclusions
The Spanish version of the FACIT-Sp scale is a reliable and valid clinical evaluation tool, and further highlights the potential clinical implications of spirituality for improving quality of life and adjustment to cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spirituality is the moral, mental, or cultural disposition of the person who tends to investigate and develop the characteristics of their spirit and is integrated in the process of humanization [1]. In medicine, it is interpreted as the need to find meaning, purpose, self-fulfillment, and the will to live, despite disease [2]. Spiritual well-being is a complex, multidimensional concept that arises from human beings’ deep, innermost aspiration to a vision of life and reality that integrates, connects, transcends, and gives meaning to their existence [3]. Different research has related spirituality with better adjustment to disease, helping to make difficult decisions in a context of high uncertainty [3].
Evidence suggested that one-third of newly diagnosed cancer patients experience psychological distress [4], and that spirituality is one way cancer patients manage their distress [5]. Some argue that assessing spiritual well-being is vital to understanding psychologically adjusting to cancer [6]. The influence of spirituality has been widely studied in patients with advanced or terminal cancer [7] and different authors have acknowledged that it plays a certain role in consolation, ability to remain peaceful, and happiness in contrast to inevitability, despair, and suicidal ideation [1]. However, its effect remains unknown in patients with early stage, potentially curable tumors that are becoming more and more common, thanks to the refinements in early diagnostic technologies and personalized or precision cancer treatments [8]. In this context, systemic adjuvant treatments after surgery seek to eradicate micrometastases, thereby improving long-term survival [10, 11]. These therapies have sequelae and potentially serious side effects, negatively impacting short-term quality of life in some patients [9], which complicates further the decision to recommend them or not in frail, vulnerable individuals and in patients at low risk for tumor recurrence. These kinds of choices are plagued with uncertainty and imply assuming the risk of worsening quality of life for the sake of an unsure future benefit. In these circumstances, spirituality, explained in terms of the patient’s peace, transcendence, and faith, could have a positive impact on adjusting to the disease, its prognosis, and shared decision making as to the advisability of adjuvant treatment. Spiritual well-being has been correlated with fewer anxious and depressive symptoms [10] and greater fighting spirit and hope in cancer patients [11]; consequently, it has become fundamental in caring for patients with advanced cancer [12]. However, the influence of spirituality in shared decision making between physician and patient has not scantly been explored, nor has its mediating role between patients’ psychological status and mental adjustment.
Despite the importance of spiritual well-being in patients experiencing a difficult disease, such as cancer, professionals have not always found it easy to implement spirituality within the framework of integrated patient care. This is largely due to the nature of the construct itself, which has a highly subjective, private component, and to the challenges in conceptualizing and evaluating it. One of the most widely used spirituality rating scales is the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being (FACIT-Sp) scale. To the best of our knowledge, there is no psychometric study of the Spanish version of the FACIT-Sp, although four psychometric studies of the English version have been published. The most recent one by Peterman et al. [13] suggests three factors (faith, meaning, and peace), although they indicate that both “meaning” and “peace” are highly correlated, yet empirically distinct factors. These results are consistent with recent studies using factor analyses (e.g., Canada et al. [14]; Murphy et al. [15]) and contradict the results of Peterman et al. [16], who found a component that combined meaning” and “peace.”
The first aim of this study was to analyze the psychometric properties of the FACIT-Sp Spanish version scale (dimensionality, structure, and reliability of the derived scores). The second aim was to establish the mediating effect of spiritual well-being on psychological distress and mental adjustment, in patients with non-metastatic, resected cancer consulting with a medical oncologist for the first time to make decisions about adjuvant therapy.
Material and methods
Subjects
Between June 2015 and December 2016, patients coming for the first time to the Medical Oncology Department of 14 hospitals to decide on adjuvant chemotherapy with or without radiotherapy were recruited. Candidates for inclusion were adults (≥ 18 years) who had a histologically confirmed, non-advanced, solid tumor treated with surgery for which international clinical guidelines consider adjuvant chemotherapy to be an option. Patients were excluded if they had metastatic disease, if they were treated with preoperative radiotherapy or chemotherapy, if the “standard” indication consisted solely of adjuvant hormonal therapy or radiotherapy, or if tumor resection was incomplete. Patients with physical conditions, comorbidities, and/or ages that comprised an absolute contraindication to chemotherapy and those with personal, psychological, family, sociological, geographical, and/or an underlying medical condition that could, in the investigator’s opinion, hamper the patient’s ability to participate were likewise excluded.
The selected population comprised patients that had undergone radical surgery in the previous month, who were free of disease, and for whom the focus of oncological consultation was to decide whether adjuvant chemotherapy was appropriated.
Study design and procedure
NEOcoping is a prospective, multicenter, observational study without intervention and patients were recruited consecutively. The ethics review board at each of the participating institutions approved the study, and the procedures were in accordance with the Helsinki Declaration. Data collection processes were similar at all hospitals. Subsequent to a full explanation of the study objectives and procedures, patients were invited to participate. All subjects signed informed consent prior to commencing. Study participation was voluntary and anonymous. Consent could be withdrawn at any time. Data were collected from the patients and clinical records and questionnaires were obtained individually during a 1-h session. Data were collected through the centralized web platform: www.neocoping.es.
Instruments
Functional Assessment of Chronic Illness-Spiritual Well-Being (FACIT-Sp) scale
The FACIT-Sp [3] consists of 12 items on a five-point Likert-type scale ranging from “not at all” (0) to “very much” (4) and three subdomains, which allows the components of Spiritual Well-Being (meaning, peace, and faith). The English version of the FACIT-Sp has also been translated and linguistically validated in Spanish and other languages (see www.facit.org). Internal consistency reliability coefficients range from 0.81 to 0.88 [13].
Brief Symptom Inventory
The Brief Symptom Inventory (BSI-18) includes 18 symptoms to assess the degree of distress on a five-point scale ranging from “total absence of symptom” (1) to “full presence of symptom” (5) [17]. The scale provides three groups of symptoms (somatization, depression, and anxiety) and a total score, known as the global severity index (GSI), which compiles the interviewee’s psychological distress. Cronbach’s alpha ranged from 0.81 to 0.90 [17].
Mini-Mental Adjustment to Cancer
The Mini-Mental Adjustment to Cancer (Mini-MAC) scale is amply used to evaluate adjustment to cancer [18]. The 29-item mini-MAC is a self-rating questionnaire using a four-point Likert scale that includes the following five coping responses: fighting spirit, helplessness-hopelessness, anxious preoccupation, fatalism, and cognitive avoidance. High scores indicate that coping styles are used more often. Reliability for scales ranged from 0.52 to 0.88 [19].
Shared Decision-Making Questionnaire
The Shared Decision-Making Questionnaire (SDM-Q-9) is a brief, valid, and reliable questionnaire that rates the SDM procedure from the patient’s point of view [20]. It was adapted to Spanish by De las Cuevas et al. [21]. The questionnaire comprises nine items, on a six-point Likert scale varying from “completely disagree” (0) to “completely agree” (5). SDM-Q-9 has shown a high Cronbach alpha in Spanish samples (0.88) [21].
Demographic data
The following medical and demographic data were obtained: gender, age, marital status, educational level, occupational field, tumor site, stage, and time between diagnosis and the first visit with a medical oncologist.
Statistical analysis
Descriptive statistics and frequencies were used to characterize the sample and assess the distribution of the item scores. To evaluate the factorial structure of the scale, the sample was randomly split into two groups and exploratory factor analysis (EFA) was performed on the first split-half sample. The adequacy of the inter-item correlation matrix to be factor analyzed was assessed using the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy. Next, solutions with different numbers of factors were fitted by using robust, unweighted least squares estimation with mean-and-variance corrected fit statistics as implemented in the FACTOR program [22]. Given that EFA provided a clearly interpretable solution that approached a simple structure, a semi-confirmatory factor analysis (SCFA) solution based on a specified target was next fitted to the entire sample using FACTOR also with robust, weighted least squares estimation with mean-and-variance corrected fit statistics. In both EFA and SCFA solutions, the goodness-of-fit indices used to assess model appropriateness were the following: (a) RMSEA, with its 90% confidence interval (CI); (b) goodness-of fit-index (GFI); (c) the root mean square of the standardized residuals (z-RMSR); and (d) the comparative fit index (CFI), as a relative measure of fit with respect to the null independence model. We followed the usual rules in deciding model appropriateness [23,24,25]. Once the FACIT dimensionality and structure had been established, scores based on the chosen solution adopted were obtained and their reliability was assessed. Because well-defined subscales were obtained, we considered in principle raw scores obtained as the simple sums of the scores on the items that define the corresponding factor. The corresponding reliabilities of these scores were estimated by using the omega coefficient [26]. Finally, because we intended to use global well-being scores as the mediating variable, the closeness to unidimensionality of the FACIT solution was appraised by using the explained common variance (ECV) index [27], and the reliability of the global scores was assessed with the omega coefficient. Multiple hierarchical regressions were conducted to probe the link between spiritual well-being and psychological distress and mental adjustment, and MedGraph-I version 3.0 [28] software was used to analyze mediation [29]. Following Baron and Kenny’s recommendation, mediation analysis was not performed with the total SDM-Q-9 score, as there was no correlation with the Spiritual Well-Being scale [29]. Psychological distress (BSI-GSI) was the predictive variable; mental-adjustment evaluated with the Mini-MAC was the variable criterion, and the mediating variable was spiritual well-being, as per FACIT-Sp. The study used a stepwise selection method and statistical analyses were run on the IBM-SPSS 23.0 statistical software package (SPSS, INC., Chicago, III) for Windows PC.
Results
Sample characteristics
Of the 573 patients screened, 59 were not eligible (17 did not meet inclusion criteria, 33 met exclusion criteria, and 19 had incomplete data). A total of 504 patients with non-metastatic, resected cancer, aged 25–84 years, were recruited. Mean age was 58.6 years (SD = 12.1) and 61.5% were female. The majority were married or partnered (77.2%), had a primary level of education (57.5%), and the most usual employment status was retired (59.7%). The most common cancer was colon (40.5%), followed by breast (33.7%). Of the tumors, 41.9% were stage III, whereas the rest were stage I-II. See Table 1.
Psychometric properties of FACIT-Sp
In general, FACIT-Sp item scores were distributed asymmetrically (negatively skewed). Furthermore, given that the test is not very long and the sample was reasonably large, we considered that the best choice was to use the underlying-variables approach, and fit the FA models (both exploratory and confirmatory) to the inter-item polychoric correlation matrix (more details in [30]). Finally, the KMO index (0.822) suggested that the inter-item relations were consistent enough to be fitted by the FA model.
Exploratory factor analyses
Given the clear results obtained with the SCFA in the entire sample, only a summary of the previous EFA results will be provided here. The oblique two-factor model fits better than the one-factor or three-factor model, with one factor labeled meaning/peace defined by items 1 to 8 such as “My life has been productive,” and the other factor labeled faith defined by items 9 to 12 such as “I find strength in my faith or spiritual beliefs,” a structure similar to the one initially found by Peterman et al. [16].
Semi-confirmatory factor analysis
On the basis of the EFA results summarized above, a SCFA solution was fitted to the data with the following specifications: factor 1 was defined by items 1 to 8 and factor 2, by items 9 to 12; items 9 and 12 were considered to be factorially complex and were allowed to load on both factors. Goodness-of-fit results for a two-factor SCFA solution were the following: GFI 0.938, Z-RMSR 0.067, and CFI 0.970, demonstrating that the fit can be considered acceptable.
The rotated oblique SCFA pattern is illustrated in Table 2. Because two items are factorially complex, the solution does not have an independent-cluster structure. However, it is quite clear: Bentler’s simplicity index is 0.997 and so the factors are well defined. As for interpretation, they may both reflect the sources of meaning in important relationships in patients’ life such as life relationships of family or children [31], and also the role of religion in generating meaning following a traumatic event [32]. Finally, the estimated inter-factor correlation was 0.42, positive and substantial as can be theoretically expected.
Scoring, reliability, and essential unidimensionality
The Meaning/Peace and Faith scales defined from the factor solution in Table 3 had omega reliability estimates of 0.850 and 0.861, which are acceptable even for individual assessment. With regard to essential unidimensionality, the ECV estimate was 0.70, which means that 70% of the common variance can be explained by a general well-being factor. This value is already enough to consider the total FACIT scores as measuring a broad, general dimension of well-being [3] made up of two correlated components or facets of Meaning/Peace and Faith. The omega reliability estimate corresponding to the full-scale scores was 0.874. Overall, these results provide support for the usage of the total FACIT scores as a mediating variable in the analyses that follow.
Mediation analysis
Mediation analyses were conducted to describe the mediating role of spiritual well-being between psychological distress and adjustment to cancer. Spiritual well-being correlates significantly and negatively to psychological distress (r = − 0.335, p < 0.001); significantly and positively to fighting spirit, hope, resignation, and cognitive avoidance (all p < 0.001); and significantly and negatively to anxious preoccupation (r = − 0.238, p < 0.001). As spiritual well-being increases, psychological symptomatology and anxious preoccupation decrease, and the use of coping strategies such as fighting spirit, hope, resignation, and cognitive avoidance increases (see Table 3).
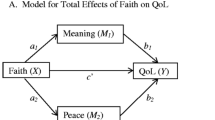
The results of the mediation analysis illustrate that psychological distress has a significant association with spiritual well-being: ß = − 0.33, p < 0.001, such that patients suffering greater psychological distress have less spiritual well-being. Furthermore, psychological distress also influences adjustment to cancer: specifically, fighting spirit, ß = − 0.23; hope, ß = − 0.31; cognitive avoidance, ß = 0.20; and anxious preoccupation, ß = 0.62. This means that the greater the psychological distress, the less use of adaptive coping strategies and the greater anxious preoccupation. Likewise, the independent linear regression analysis reveals a significant correlation between spiritual well-being and the coping strategies of fighting spirit, ß = 0.41; hope, ß = 0.23; and cognitive avoidance, ß = 0.15. In contrast, it showed no correlation with anxious preoccupation, ß = − 0.26. Similarly, distress is seen to lose its effect in part on fighting spirit, ß = − 0.10; hopelessness, ß = −0.27; and cognitive avoidance, ß = 0.28, when spiritual well-being is introduced; whereas spiritual well-being losses all of its mediating effect on anxious preoccupation, ß = 0.61, see Fig. 1.
Therefore, the mediation analysis reveals that spirituality partially mediates between psychological distress and adjustment to cancer, such as fighting spirit (Sobel z value = −5.875, p < 0.001), hopelessness (Sobel z value = − 2.903, p < 0.003), and cognitive avoidance (Sobel z value = −4.462, p < 0.001), but not between psychological distress and anxious preoccupation (Sobel z value = 0.558, p = 0.576).
Discussion
Owing to renewed interest in the spiritual domain and how it relates to health, the results of current research suggest that, among people with cancer, spiritual well-being has a positive association with adjustment to the disease [33]. A first aim of this study was to analyze the psychometric properties of the FACIT-Sp in a sample of individuals with resected, non-metastatic cancer. The results were generally favorable. The FACIT item scores were compatible with a clear and theoretically interpretable solution in two factors that agreed generally with solutions reported in other languages [34, 35]. The reliabilities of the derived Meaning/Peace and Faith scales were acceptable. Finally, the oblique solution in two factors was compatible with an essentially unidimensional solution of general well-being, and the reliability estimate for the total scale scores can be considered adequate. However, in the two-factor model, items 8 and 12 were considered to be factorially complex and load on both factors. This may be because both items could be related to emotional and affective aspects linked to spirituality that should be object of future investigations. Another possible explanation is the difficulty for Spanish patients in answering negatively worded questions such as item 8, perhaps it could be replaced with a positively worded item as suggested others researchers [15, 36].
Insofar, as the second objective of this study, our results show that spiritual well-being associated negatively with psychological distress and positively with adjustment to cancer, so that as spiritual well-being increases, psychological symptomatology and anxious preoccupation decrease, and the use of coping strategies such as fighting spirit, hope, resignation, and cognitive avoidance improve. These results were similar to those of previous studies which found that during the course of their disease, people with cancer can find greater meaning in their lives and relationships and are stronger in coping with their illness [17]. In our study, spiritual well-being not only correlated with psychological distress and adjustment to cancer, but also revealed itself to be a partial mediator between both, such that as psychological distress increases, spiritual well-being decreases, leading, in turn, to worse adjustment to the disease.
In contrast, we expected to detect a strong association between spiritual well-being and satisfaction with SDM; however, this has not been the case. The vast majority of patients in our sample reported feeling very satisfied with the information that the medical oncologist provided them and the low variability of responses on the SDM-Q-9 would explain the low correlation between both scales. It is possible that spirituality and adjustment to cancer are truly detached from satisfaction with making serious medical decisions, as in this case. However, the Anglo-Saxon literature suggests that most patients feel less involved in the SDM process than they would like [37]. If this were so, one might think that the patients are not so satisfied as they claim to be, but prefer not to express it and that filling in the questionnaires immediately after the visit with the oncologist may have increased the bias toward social desirability [38]. On the other hand, there are studies that suggest that patients can overestimate the special attention received by participating in a research project, feeling that they are more involved in decisions about their treatment [38] and avoiding the cognitive dissonance between wanting to participate in the SDM process and the fact of not being involved. Likewise, these results can be influenced by factors such as the sample’s age and characteristics, by reason of most patients included in this study were relatively older (mean, 59 years). It is well known that older persons tend to be more complacent with their physicians [39] and suffering a life-threatening disease can make them feel more vulnerable and dependent on the care of their doctor.
Overall, the results suggest the need to raise professionals’ awareness to the commitment to offer integral care to cancer patients, affording them strategies to cope with this kind of demand.
This type of request is usually presented during the visit as the patient’s search for meaning in their experience to fit it into their life story, which can help them to regulate their emotional states and to better cope with the adjuvant treatment.
There are several limitations to this study. First of all, though our sample size is larger than that of other series in the literature, it was comprised of patients with a localized tumor who had undergone surgery and were candidates for adjuvant chemotherapy. In the future, we would advise expanding the sample to include other tumor stages and types with the aim of confirming these results, as well as to compare different clinical-pathological and social variables. Secondly, the FACIT-Sp self-report subjective measures may not accurately reflect patients’ sense of meaning, peace, and faith, having limitations such as response bias (social enchantment, imprecise memory, etc.) and their difficulty in fully comprehending the spiritual well-being process. Finally, another limitation has to do with the data collection procedure. Several authors have stated that time sequence is relevant in the mediation of the variables involved. Subsequent studies could present successive measures of the variables so that the change between them over time can be contemplated.
Implications for practice
The Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) Spanish version is a valid and reliable scale to assess spiritual well-being in patients with non-metastatic cancer. Spiritual well-being can serve to soften the impact of the disease and aid in adjusting to cancer, with potential clinical implications for improving quality of life in cancer patients receiving adjuvant treatment.
References
Bovero A, Leombruni P, Miniotti M et al (2016) Spirituality, quality of life, psychological adjustment in terminal cancer patients in hospice. Eur J Cancer Care (Engl) 25(6):961–969. https://doi.org/10.1111/ecc.12360
Scott-Ladd B, Chan CCA (2004) Emotional intelligence and participation in decision-making: strategies for promoting organizational learning and change. Strateg Chang 13(2):95–105. https://doi.org/10.1002/jsc.668
Peterman AH, Fitchett G, Brady MJ et al (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy— Well-being Scale (FACIT-Sp). Ann Behav Med 24(1):49–58. https://doi.org/10.1207/S15324796ABM2401_06
Mitchell AJ, Chan M, Bhatti H et al (2011) Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol 12(2):160–174. https://doi.org/10.1016/S1470-2045(11)70002-X
Munoz AR, Salsman JM, Stein KD, Cella D (2015) Reference values of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being: a report from the American Cancer Society’s studies of cancer survivors. Cancer 121(11):1838–1844. https://doi.org/10.1002/cncr.29286
Nejat N, Whitehead L, Crowe M (2017) The use of spirituality and religiosity in coping with colorectal cancer. Contemp Nurse 53(1):48–59. https://doi.org/10.1080/10376178.2016.1276401
Schnipper LE, Davidson NE, Wollins DS et al (2015) American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol 33(23):2563–2577. https://doi.org/10.1200/JCO.2015.61.6706
Bai M, Lazenby M (2015) A systematic review of associations between spiritual well-being and quality of life at the scale and factor levels in studies among patients with cancer. J Palliat Med 18(3):286–298. https://doi.org/10.1089/jpm.2014.0189
McDermott DF, Regan MM, Clark JI et al (2005) Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol 23(1):133–141. https://doi.org/10.1200/JCO.2005.03.206
Yeung NCY, Lu Q (2014) Affect as a mediator between self-efficacy and quality of life among Chinese cancer survivors in China. Eur J Cancer Care (Engl) 23(1):149–155. https://doi.org/10.1111/ecc.12123
Whitford HS, Olver IN (2012) The multidimensionality of spiritual wellbeing: peace, meaning, and faith and their association with quality of life and coping in oncology. Psycho-Oncology 21(6):602–610. https://doi.org/10.1002/pon.1937
Koenig HG (2009) Research on religion, spirituality, and mental health: a review. Can J Psychiatr 54(5):283–291. https://doi.org/10.1177/070674370905400502
Peterman AH, Reeve CL, Winford EC et al (2014) Measuring meaning and peace with the FACIT–Spiritual Well-Being Scale: distinction without a difference? Psychol Assess 26(1):127–137. https://doi.org/10.1037/a0034805
Canada AL, Murphy PE, Fitchett G et al (2008) A 3-factor model for the FACIT-Sp. Psychooncology 17(9):908–916. https://doi.org/10.1002/pon.1307
Murphy PE, Canada AL, Fitchett G et al (2010) An examination of the 3-factor model and structural invariance across racial/ethnic groups for the FACIT-Sp: a report from the American Cancer Society’s Study of Cancer Survivors-II (SCS-II). Psychooncology 19(3):264–272. https://doi.org/10.1002/pon.1559
Peterman AH, Fitchett G, Brady MJ et al (2002) Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 24(1):49–58. https://doi.org/10.1207/S15324796ABM2401_06
Derogatis LR (2001) BSI 18, Brief Symptom Inventory 18: administration, scoring and procedures manual. NCS Pearson, Incorporated
Watson M, Law MG, Santos MD et al (1994) The Mini-MAC: further development of the mental adjustment to cancer scale. J Psychosoc Oncol 12(3):33–46. https://doi.org/10.1300/J077V12N03_03
Bredal IS (2010) The Norwegian version of the Mini-Mental Adjustment to Cancer Scale: factor structure and psychometric properties. Psycho-Oncology 19(2):216–221. https://doi.org/10.1002/pon.1564
Kriston L, Scholl I, Hölzel L et al (2010) The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns 80(1):94–99. https://doi.org/10.1016/j.pec.2009.09.034
De las Cuevas C, Perestelo-Perez L, Rivero-Santana A et al (2015) Validation of the Spanish version of the 9-item Shared Decision-Making Questionnaire. Health Expect 18(6):2143–2153. https://doi.org/10.1111/hex.12183
Lorenzo-Seva U, Ferrando PJ (2013) FACTOR 9.2: a comprehensive program for fitting exploratory and semiconfirmatory factor analysis and IRT models. Appl Psychol Meas 37(6):497–498. https://doi.org/10.1177/0146621613487794
Hair JF, Black WC, Babin BJ (2010) RE Anderson multivariate data analysis: a global perspective
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J 6(1):1–55. https://doi.org/10.1080/10705519909540118
Schermelleh-Engel K, Moosbrugger H, Müller H (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 23–74
McDonald RP (1999) Test theory: a unified treatment. L. Erlbaum Associates, Mahwah
ten Berge JMF, Kiers HAL (1991) A numerical approach to the approximate and the exact minimum rank of a covariance matrix. Psychometrika 56(2):309–315. https://doi.org/10.1007/BF02294464
Jose PE (2003) MedGraph-I: a programme to graphically depict mediation among three variables: the internet version, version 2.0. Victoria Univesity Wellington, Wellington, New Zealand Retrieved Dec 31:2009
Baron RM, Kenny DA (1986) The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182. https://doi.org/10.1037/0022-3514.51.6.1173
Ferrando PJ, Lorenzo-Seva U (2013) Unrestricted item factor analysis and some relations with Item Response Theory. Technical Report. Department of Psychology, Universitat Rovira i Virgili, Tarragona. http://psico.fcep.urv.es/utilitats/factor
Breitbart W, Rosenfeld B, Gibson C et al (2010) Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology 19(1):21–28. https://doi.org/10.1002/pon.1556
Park CL, Chmielewski J, Blank TO (2010) Post-traumatic growth: finding positive meaning in cancer survivorship moderates the impact of intrusive thoughts on adjustment in younger adults. Psychooncology 19(11):1139–1147. https://doi.org/10.1002/pon.1680
Visser A, Garssen B, Vingerhoets A (2010) Spirituality and well-being in cancer patients: a review. Psycho-Oncology 19(6):565–572. https://doi.org/10.1002/pon.1626
Fradelos E, Tzavella F, Koukia E et al (2016) The translation, validation and cultural adaptation of functional assessment of chronic illness therapy—Spiritual Well-being 12 (facit-sp12) Scale in Greek language. Mater Socio Medica 28(3):229–234. https://doi.org/10.5455/msm.2016.28.229-234
Noguchi W, Ohno T, Morita S et al (2004) Reliability and validity of the Functional Assessment of Chronic Illness Therapy–Spiritual (FACIT–Sp) for Japanese patients with cancer. Support Care Cancer 12(4):240–245. https://doi.org/10.1007/s00520-003-0582-1
Lazenby M, Khatib J, Al-Khair F, Neamat M (2013) Psychometric properties of the Functional Assessment of Chronic Illness Therapy—Spiritual Well-being (FACIT-Sp) in an Arabic-speaking, predominantly Muslim population. Psycho-Oncology 22(1):220–227. https://doi.org/10.1002/pon.2062
Laidsaar-Powell RC, Butow PN, Bu S et al (2013) Physician-patient-companion communication and decision-making: a systematic review of triadic medical consultations. Patient Educ Couns 91(1):3–13. https://doi.org/10.1016/j.pec.2012.11.007
Scholl I, Kriston L, Dirmaier J, Härter M (2015) Comparing the nine-item Shared Decision-Making Questionnaire to the OPTION Scale—an attempt to establish convergent validity. Health Expect 18(1):137–150. https://doi.org/10.1111/hex.12022
Bench S, Day T (2010) The user experience of critical care discharge: a meta-synthesis of qualitative research. Int J Nurs Stud 47(4):487–499. https://doi.org/10.1016/j.ijnurstu.2009.11.013
Funding
This work was supported by FSEOM-Onvida for Projects on Long Survivors and Quality of Life. SEOM (Spanish Society of medical Oncology) 2015. The sponsor of this research has not participated in the collection, analysis, or interpretation of the data, in the writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors meet the appropriate authorship criteria and no author has been omitted from the list. All authors contributed to the concept and design of the manuscript, and critically reviewed and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
The study has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments. This study is an observational trial without intervention.
Informed consent statement
Signed informed consent was obtained from all patients.
Rights and permissions
About this article
Cite this article
Jimenez-Fonseca, P., Lorenzo-Seva, U., Ferrando, P.J. et al. The mediating role of spirituality (meaning, peace, faith) between psychological distress and mental adjustment in cancer patients. Support Care Cancer 26, 1411–1418 (2018). https://doi.org/10.1007/s00520-017-3969-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3969-0