Abstract
Accurately monitoring peri-operative core temperature is a cornerstone of good practice. Relatively invasive devices such as oesophageal temperature probes and pulmonary artery catheters facilitate this, but are inappropriate for many patients. There remains a need for accurate monitors of core temperature that can be used in awake patients. This study compared the accuracy of two core temperature thermometers that can be used for this purpose: the 3M Bair Hugger™ Temperature Monitoring System Zero Flux Thermometer and the CorTempR™ Wireless Ingestible Temperature Sensor. Readings were compared with the oesophageal probe, the current intraoperative standard. Thirty patients undergoing elective surgical procedures under general anaesthesia were recruited. The ingestible sensor was ingested prior to induction of anaethesia, and post induction, the zero-flux electrode attached above the right eyebrow and oesophageal probe inserted. During surgery, the temperature on each device was recorded every minute. Measurements were compared using Bland–Altman analysis. The ingestible sensor experienced interference from use of diathermy and fluoroscopy in the operating theatre, rendering 39% of its readings unusable. These were removed from analysis. With remaining readings the bias compared with oesophageal probe was + 0.42 °C, with 95% limits of agreement − 2.4 °C to 3.2 °C. 75.4% of readings were within ± 0.5 °C of the OTP reading. The bias for the zero flux electrode compared to oesophageal probe was + 0.02 °C with 95% limits of agreement − 0.5 °C to 0.5 °C. 97.7% of readings were within ± 0.5 °C of the oesophageal probe. The study findings suggest the zero-flux thermometer is sufficiently accurate for clinical use, whereas the ingestible sensor is not.
Trial registration The study was registered at http://www.clinicaltrials.gov, NCT Number: NCT02121574.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The importance of good peri-operative temperature management in optimising patient outcomes is well established [1,2,3]. In 2008, the National Institute for Health and Care Excellence (NICE) published Clinical Guideline 65 (CG65): “Hypothermia: prevention and management in adults having surgery” [4]. This was a landmark in recognising the benefits of keeping patients normothermic in the perioperative period and was updated in 2016 to include thermometry. Of note, zero heat-flux was included as an acceptable direct estimate of core temperature to within 0.5 °C, although there was no mention of intraluminal gastrointestinal thermometry.
The absence of a practical, non-invasive means of measuring core temperature that is accurate and consistent enough to distinguish the 0.5 °C differences that are accepted as significantly affecting patient outcomes [5], has been recognised for some time [6].
Urinary bladder and oesophageal temperatures are sufficiently accurate [5] but are unsuitable for the many patients undergoing surgery including those that are awake, have oesophageal disease, or have no existing urinary catheter. Although non-invasive and relatively cheap means of measuring temperature such as aural canal probes and infrared scanners exist, they are neither accurate nor consistent enough to distinguish 0.5 °C differences [5].
In this study we planned to determine whether two methods of core temperature measurement that can be used in awake patients were sufficiently accurate for use perioperatively.
The first is the 3M Bair Hugger™ Temperature Monitoring System Zero Flux Thermometer (ZFT) (3M Europe N.V./S.A., Hermeslaan 7, B-1831 Diegem, Belgium). Initially described in 1973 [7], zero flux thermometry is a non-invasive process whereby an adhesive pad is placed on the forehead. The pad insulates the skin underneath it from external heat sources, and contains a heater which warms the underlying skin until it has equilibrated with the patient’s core temperature, this point being determined by the absence of any detectable heat flux from the core to the skin through an isothermal tunnel [8].
The second is the CorTemp™ wireless ingestible temperature monitoring system (ITS) (HQInc 210 9th Street Dr. West Palmetto, FL 34221, USA). This consists of an ingestible pill and an external receiver. The silicone coated sensor contains a micro battery, quartz crystal, communication coil and circuit board, encapsulated in medical grade epoxy. Once ingested, the crystal sensor vibrates at a frequency relative to the body’s internal temperature, produces a magnetic flux and transmits a low-frequency signal to the receiver. It is yet to be trialled in hospital patients.
1.1 Study objectives and hypotheses
The objective of this study was to compare the accuracy of both of these techniques with the current intra-operative standard in the United Kingdom, the oesophageal temperature probe (OTP).
2 Methods
The study was reviewed and approved by the NRES Committee East of England–Norfolk, England (Ref: 14/EE/1016, Chairperson Dr R. Stone, 18th June 2014), and conducted in accordance with the Ethical Principles for Medical Research Involving Human Subjects outlined in the Declaration of Helsinki.
Written informed consent was obtained from all subjects. All aspects of patient privacy and confidentiality were observed.
Upon arrival in the anaesthetic room prior to induction, subjects ingested the ITS with 50 ml of water. Following induction of anaesthesia and intubation, the OTP (CareFusion General Purpose Temperature Probe, Disposable, 12Fr, Carefusion Finland 320 Oy, Kuortaneenkatu 200510, Helsinki, Finland) was inserted orally under direct vision with laryngoscopy. The tip was then advanced 40 cm distal to the incisors [9] and fixed in position with adhesive tape. The self adhesive ZFT electrode was attached above the right supraorbital ridge after cleaning with a 2% chlorhexidine/alcohol wipe, according to the manufacturer’s instructions. ZFT was not applied awake as the OTP comparator was not present pre induction.
After transfer to theatre a 3M™ Bair Hugger™ Model 750 forced-air warming unit and 3M™ Ranger™ inline intravenous Blood/Fluid Warming System were used according to local protocol on all patients. No warming mattresses or patient prewarming were employed. The face was left uncovered by the Bair Hugger™ to prevent possible interference, and to monitor the OTP to ensure it was still in place and not dislodged.
Recording commenced after application of warming and before the start of surgery. OTP and ITS gave readings almost instantaneously whilst the ZFT typically required a 3–5 min “warm up period”. Temperature was recorded simultaneously by each device every minute for the duration of the procedure by a dedicated anaesthetic clinical research fellow not involved in the clinical care of the patient. Upon completion of surgery and prior to wakening the OTP and ZFT were removed, with the ITS excreted by the patient over the following days.
3 Participants
3.1 Eligibility criteria
Patients eligible for inclusion were those over 18 years of age with sufficient mental capacity and command of spoken and written English to give informed, written consent.
Exclusion criteria included the inability to give informed consent, contraindication to insertion of oesophageal probe (carcinoma of the oesophagus or pharynx, previous oesophageal surgery, oesophageal stricture or varices, pharyngeal pouch), subjects undergoing open intra-abdominal surgery to remove a portion of the gastrointestinal tract, and abnormal gastrointestinal pathology that may prevent safe use of ITS.
Eligible participants were identified as those listed for elective surgery at the authors’ hospital trust, either at the Royal Sussex County Hospital, Brighton, or Princess Royal Hospital, Haywards Heath.
Patients were informed of the study at preoperative assessment clinic several weeks before surgery with recruitment posters, and were given a patient information sheet which contained contact information to allow questions to be asked.
Potential participants were identified during research fellows’ academic days, and recruited in order of scheduled surgery.
Written informed consent was sought on the morning of surgery at anaesthetic pre-assessment. The type of surgery the participants underwent is summarised in Table 1.
During data collection results from all 3 devices were available to and recorded by the study operator onto trust laptop computer. Clinical data was available to study operators, although not recorded.
3.2 Analysis
GraphPad Prism 6 was used to produce Bland–Altman plots of the ITS vs OTP and ZFT vs OTP. 95% limits of agreement were calculated taking into account the repeated measurements per patient using the method where the true value varies [10].
Levels of agreement between ITS/ZFT and OTP were further assessed by calculating agreement tolerability ratios using the method described by Malachy O. Columb [11], where ratios < 1 represent Acceptable agreement, 1–2 represent Marginal agreement and > 2 represent Unacceptable agreement. For these calculations, we defined OTP temperature ± 0.5 °C as the tolerability interval.
During data collection it was observed that the ITS temporarily ceased to function during use of both diathermy and fluoroscopic imaging, giving no value or one that was invalid.
All measured values were recorded, along with whether diathermy or fluoroscopy were in use at the time of each individual measurement.
Indeterminate readings from the ZFD or ITS were removed from final analysis, and their incidence recorded. Indeterminate readings from the OTP, as the index test, resulted in readings from all three thermometers being removed. Missing data was handled in the same manner. ITS and ZFD were not compared to each other as Bland Altman analysis requires an accepted comparator.
Sample size was set at 30 patients, an accepted number to estimate mean and standard deviation [12], and confirmed with one of the authors of the Bland–Altman method (Prof D Altman, personal communication, 11th April 2014).
4 Results
30 patients were recruited to the study, with 29 completing it (see Fig. 1). One participant was excluded due to dislodgement of the OTP, which could not be resited due to the nature of surgery. Mean ± SD duration per subject was 84 ± 46 min, with a total of 2511 measurements made with each individual device over the study duration. Patient characteristics are presented in Table 2.
4.1 Zero flux thermometer
The ZFT experienced one temporary malfunction for a 29 min period during a mastectomy, which was thought to be due to the close proximity (approximately 30 cm) of surgical diathermy. This affected 1.2% of all readings taken. The device functioned normally for the other breast surgery case, a lumpectomy.
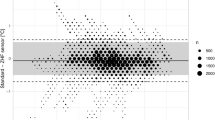
The bias for the ZFT compared to OTP was + 0.02 °C (95% limits of agreement − 0.5 °C to 0.5 °C). 97.7% of readings were within ± 0.5 °C of the OTP reading. Bland–Altman analysis found good agreement between the ZFT and OTP (Fig. 2).
The agreement tolerability ratio for the ZFD device was within acceptable limits at 0.99.
4.2 ITS
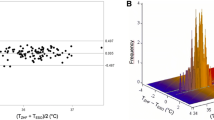
To allow analysis of unaffected data, all 983 (39%) of ITS readings recorded during interference were dropped.
With invalid readings removed, the bias for the ITS when compared with the OTP was + 0.42 °C (95% limits of agreement − 2.4 °C to 3.2 °C). 75.4% of readings were within ± 0.5 °C of the OTP reading (Fig. 3).
The agreement tolerability ratio for the ITS device was unacceptable at 5.6.
5 Discussion
The ZFD has shown to be a practical and reliable substitute for OTP, providing continuous, accurate real time readings after a typical 3–5 min “warm up period”, requiring no further user input. The ZFT functioned reliably for almost 99% of measurement duration.
Our data for the ZFT appears to show comparable accuracy to that of the published literature. A small proof of concept trial was published in 1980 [13], which compared accuracy of zero flux thermometry against a calibrated pulmonary artery catheter in 10 anaesthetised patients, found it to be comparable to oesophageal thermometry.
A preclinical trial [14] and a study in cardiac surgical patients [15] showed good performance of the ZFT. One study found accurate correlation with nasopharyngeal and sublingual temperatures in gynaecological and trauma surgery [16] and in another to pulmonary artery catheters and oesophageal probes down to 34 °C and nasopharyngeal temperatures down to 32 °C, although agreement was poor below this latter value during cardiopulmonary bypass [17].
Other studies have also found insufficient accuracy of zero flux thermometry in cardiac surgical patients, with a different zero flux device in one study having a mean bias of − 0.2 ± 0.5 °C (95% limits of agreement of ± 1.16) compared to pulmonary artery catheters [18], whilst another study comparing zero flux thermometry to pulmonary artery catheters in 105 patients having non emergent cardiac surgery found an average intraoperative temperature difference of − 0.08 °C (95% limits of agreement of ± 0.88) [19].
We originally envisaged that the ITS could be utilised both during surgery and in clinical areas outside the operating theatres. However, it was immediately apparent that the interference from diathermy and fluoroscopy would mean that its utility intraoperatively would be severely limited. Discussion between the clinicians and statisticians led to the exclusion of data from the periods of interference (which had been recorded during data collection). The capsule functioned during periods without interference, therefore these timepoints were analysed in order to determine whether it could be used to provide continuous, accurate readings of core temperature during other parts of the patient pathway.
Bland–Altman plots (Fig. 3) suggest that when functioning correctly, the ITS has a reasonable level of accuracy around a normal body temperature of 37 °C, although it tends to overread above this level and underread below it. The device produced no meaningful results when diathermy or fluoroscopy were in use, representing, in this study, almost 40% of operative time. When functioning, we could not explain the difference between the OTP and the ITS. This could be due to bias and inaccuracy of the ITS. The intermediate blood supply of the intestine, along with the presence of intraluminal food debris, faeces and air may also be partly responsible. Finally the exposure of intact bowel during laparoscopic abdominal surgery in some cases may have also affected the accuracy of the device.
For continuous monitoring of intraoperative temperatures the ITS also proved to be impractical due to the requirement of close proximity between the capsule and the external monitor used to capture the reading (approximately 60 cm or less). This was exacerbated by the seemingly rapid gastrointestinal transit time.
The most convenient solution was to rest the device on the patient’s shoulder, with the operator reaching over the patient under the surgical drapes to press the read button to obtain a temperature. The degree of involvement required by this device in its current format would render it impractical for a lone anaesthetist to measure temperature every minute for the duration of surgery. In everyday practice, every 30 min in accordance with current guidelines may be workable, although the method employed may be unacceptable to many clinicians.
The ITS has been tested over several days in laboratory protocols to a high degree of accuracy [20], and in various sports to look for both hypothermia and hyperthermia [21, 22].
While the device’s ability to log temperatures and accompany the patient throughout the hospital pathway may still prove useful for research purposes preoperatively, it does not appear to be a satisfactory intraoperative monitor in the theatre environment.
A comparison of both devices to the pulmonary artery catheter, the gold standard of core temperature measure, would have been impractical and unethical due to its difficult insertion and association with complications [23].
While we were able to analyse a large number of data pairs, more subjects would have improved the accuracy as temperatures within patients did not vary widely.
Whilst the measurements for the study were undertaken in anaesthetised patients, both methods of temperature measurement can, and have, been used in awake patients. However, future studies which compare them to reference standard measures in patients undergoing regional or local anaesthesia would be of benefit.
6 Conclusions
The ZFT appears to be a reliable, practical and accurate continuous measure of core temperature during elective surgery that could potentially be used for awake patients. As such it represents a significant step forwards for perioperative temperature management.
The ITS presented logistical issues and was not accurate enough to be used for routine surgery.
References
Harper CM, Andrzejowski JC, Alexander R. NICE and warm. Br J Anaesth. 2008;101(3):293–95. https://doi.org/10.1093/bja/aen233.
Harper CM, McNicholas T, Gowrie-Mohan S. Maintaining perioperative normothermia. Brit Med J. 2003;326(7392):721–2.
Sessler DI. Perioperative heat balance. Anesthesiology. 2000;92(2):578–96.
NICE. Hypothermia: prevention and management in adults having surgery. NICE clinical guideline 65. London: National Institute for Health and Clinical Excellence; 2008 (updated 2016).
Sessler D. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109(2):318–38.
Harper CM. The need for an accurate noninvasive thermometer. Anesth Analg. 2009;109(1):288.
Fox RH, Solman AJ, Isaacs R, et al. A new method for monitoring deep body temperature from the skin surface. Clin Sci. 1973;44:81–6.
Teunissen LP, Klewer J, de Haan A, et al. Noninvasive continuous core temperature measurement by zero heat flux. Physiol Meas. 2011;32:559–70.
Wang M, Singh A, Qureshi H, et al. Optimal depth for nasopharyngeal temperature probe positioning. Anesth Analg. 2016;122(5):1434–8. https://doi.org/10.1213/ANE.0000000000001213.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82. https://doi.org/10.1080/10543400701329422.
Clinical measurement and assessing agreement. Curr Anaesth Crit Care 2008; 19 (5–6): 328–9. https://doi.org/10.1016/j.cacc.2008.07.001.
Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–12.
Lees DE, Kim YD, Macnamara TE. Noninvasive determination of core temperature during anesthesia. South Med J. 1980;73(10):1322–24.
Kimberger O, Thell R, Schuh M, et al. Accuracy and precision of a novel non-invasive core thermometer. Br J Anaesth. 2009;103(2):226–31. https://doi.org/10.1093/bja/aep134.
Eshraghi Y, Nasr V, Parra-Sanchez I, et al. An evaluation of a zero-heat-flux cutaneous thermometer in cardiac surgical patients. Anesth Analg. 2014;119(3):543–49. https://doi.org/10.1213/ane.0000000000000319.
Iden T, Horn E-P, Bein B, et al. Intraoperative temperature monitoring with zero heat flux technology (3M SpotOn sensor) in comparison with sublingual and nasopharyngeal temperature: an observational study. Eur J Anaesthesiol. 2015;32(6):387–91. https://doi.org/10.1097/eja.0000000000000232.
Mäkinen M-T, Pesonen A, Jousela I, et al. Novel zero-heat-flux deep body temperature measurement in lower extremity vascular and cardiac surgery. J Cardiothorac Vasc Anesth. 2016;30(4):973–8.
Sastre JA, Pascual MJ, López T. Evaluation of the novel non-invasive zero-heat-flux Tcore™ thermometer in cardiac surgical patients. J Clin Monit Comput. 2018. https://doi.org/10.1007/s10877-018-0143-2.
Eshraghi Y, Nasr V, Parra-Sanchez I, et al. An evaluation of a zero-heat-flux cutaneous thermometer in cardiac surgical patients. Anesth Analg. 2014;119:543–9.
Darwent D, Zhou X, Heuvel C, et al. The validity of temperature-sensitive ingestible capsules for measuring core body temperature in laboratory protocols. Chronobiol Int. 2011;28(8):719–26. https://doi.org/10.3109/07420528.2011.597530.
Byrne C, Lim CL. The ingestible telemetric body core temperature sensor: a review of validity and exercise applications. Br J Sports Med. 2007;41(3):126–33. https://doi.org/10.1136/bjsm.2006.026344.
Aughey RJ, Goodman CA, McKenna MJ. Greater chance of high core temperatures with modified pacing strategy during team sport in the heat. J Sci Med Sport. 2014;17(1):113–18. https://doi.org/10.1016/j.jsams.2013.02.013.
Hadian M, Pinsky MR. Evidence-based review of the use of the pulmonary artery catheter: impact data and complications. Crit Care. 2006;10(3):1–11. https://doi.org/10.1186/cc4834.
Acknowledgements
The authors wish to thank David Crook PhD for assistance with study design.
Funding
This study was funded by a small project grant from the Association of Anaesthetists of Great Britain and Ireland Foundation, administered by the National Institute for Academic Anaesthesia (WKR0-2013-0051).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
C.M.H. has received loans of equipment from various manufacturers of warming devices, including Inditherm, Augustine Biomedical, Arizant, 3M and Mölnlycke. He has also received expenses and honoraria for sitting on advisory boards for 3M and Mölnlycke. Other authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Jack, J.M., Ellicott, H., Jones, C.I. et al. Determining the accuracy of zero-flux and ingestible thermometers in the peri-operative setting. J Clin Monit Comput 33, 1113–1118 (2019). https://doi.org/10.1007/s10877-019-00252-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00252-9