Abstract
Objective
Immunodeficiency, centromeric instability, and facial anomalies (ICF) syndrome is a rare autosomal recessive primary immunodeficiency. Hypogammaglobulinemia is a major manifestation of ICF syndrome, but immunoglobulin replacement therapy does not seem to be effective for some ICF patients. Therefore, we aimed to reassess the immunological characteristics of this syndrome.
Methods
Eleven Japanese patients with ICF syndrome were enrolled. We performed whole-exome sequencing in four cases and homozygosity mapping using SNP analysis in two. We evaluated their clinical manifestations and immunological status.
Results
We newly diagnosed six ICF patients who had tentatively been diagnosed with common variable immunodeficiency. We identified two novel mutations in the DNMT3B gene and one novel mutation in the ZBTB24 gene. All patients showed low serum IgG and/or IgG2 levels and were treated by periodic immunoglobulin replacement therapy. Three of the six patients showed worse results of the mitogen-induced lymphocyte proliferation test. Analyses of lymphocyte subpopulations revealed that CD19+CD27+ memory B cells were low in seven of nine patients, CD3+ T cells were low in three patients, CD4/8 ratio was inverted in five patients, CD31+ recent thymic emigrant cells were low in two patients, and CD19+ B cells were low in four patients compared with those in the normal controls. ICF2 patients showed lower proportions of CD19+ B cells and CD16+56+ NK cells and significantly higher proportions of CD3+ T cells than ICF1 patients. T cell receptor excision circles were undetectable in two patients. Despite being treated by immunoglobulin replacement therapy, three patients died of influenza virus, fatal viral infection with persistent Epstein–Barr virus infection, or JC virus infection. One of three dead patients showed normal intelligence with mild facial anomaly. Two patients presented with autoimmune or inflammatory manifestations. Infectious episodes decreased in three patients who were started on trimethoprim–sulfamethoxazole and/or antifungal drugs in addition to immunoglobulin replacement therapy. These patients might have suffered from T cell immunodeficiency.
Conclusion
These results indicate that patients with ICF syndrome have a phenotype of combined immunodeficiency. Thus, to achieve a better prognosis, these patients should be treated as having combined immunodeficiency in addition to receiving immunoglobulin replacement therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunodeficiency, centromeric instability, and facial anomalies (ICF) syndrome is a rare autosomal recessive inborn error of immunity characterized by hypogammaglobulinemia, centromere instability, and facial anomalies. Patients with this syndrome are described as presenting with facial anomalies such as ocular hypertelorism, epicanthic folds, broad flat nasal bridge, low-set ears, and macroglossia [1,2,3]. They are also associated with mental retardation, including motor delay, speech delay, and intellectual disability [1,2,3]. Approximately half of patients with ICF syndrome are classified into type 1 (ICF1) with mutation in the DNMT3B gene [4, 5], whereas about 30% of patients are classified into type 2 (ICF2) with mutation in the ZBTB24 gene [6]. Recently, CDCA7 and HELLS genes were identified as causative genes for ICF3 and ICF4, respectively [7]. DNMT3B is a de novo DNA methyltransferase that acts during early cell development [7]. The function of ZBTB24 has not been definitively characterized, but it was reported to be involved in DNA methylation, particularly during B cell development [6]. CDCA7 is reported to behave as a direct c-Myc target gene and its overexpression has been found to enhance the transformation of lymphoblastoid cells. HELLS is reported to be involved in regulation of the expansion or survival of lymphoid cells and is required for efficient DNA methylation.
Immunodeficiency is characterized by severe recurrent infections such as fatal respiratory and gastrointestinal infections as a result of hypo- or α-gammaglobulinemia in the presence of B cells [1,2,3, 7]. Diverse pathogens besides bacteria were reported in ICF patients, such as viruses, fungi, and parasites [8]. Defective humoral immunity characterizes ICF syndrome, and the patients are fundamentally treated with immunoglobulin replacement therapy. Additionally, CD19+CD27+ memory B cells were shown to be absent from patients with ICF1 and ICF2 [8,9,10]. However, T cell immunodeficiency in ICF syndrome is not fully understood. T cell apoptosis, decreased CD4+ T cells, and decreased CD4+ T cells associated with autoimmune/inflammatory diseases were reported in a small number of patients with ICF syndrome [11,12,13]. Hematopoietic stem cell transplantation (HSCT) might be useful for patients with ICF syndrome [8, 14, 15], whereas immunosuppressive therapy would be required for patients with autoimmune/inflammatory manifestations [8].
In this paper, we analyze the immunological profiles including T cells in Japanese patients with ICF syndrome, and disclose the existence of T cell immunodeficiency in these patients. In addition, we describe the infectious episodes and outcomes of the patients and reveal that some infections were consistent with T cell immunodeficiency.
Material and Methods
Study Approval and Samples
Eleven Japanese patients with ICF syndrome were enrolled in this study. Detailed clinical and biological data were collected from birth until June 2018. We defined “the age at final observation” as the age at June 2018 and “the age at immunological analysis” as the age when the immunological analysis was performed. We defined normal ranges of serum levels of globulins as from 10th (or − 1.28 SD) to 90th (or + 1.28 SD) [16]. Mental status was assessed by the physicians caring for the patients. When mental retardation was suspected, the physicians evaluated the mental status using development quotient or intelligence quotient and defined mental retardation as when the score was below 70 or the patients had some difficulties attending an ordinary school or work. For 4 of the 11 patients, some clinical and biological data had previously been reported by Shirohzu et al. as Pt. 2 (Patient 3 in our study) and Pt. 3 (Patient 4 in our study) [17], and by Nitta et al. as P6 (Patient 8 in our study) and P7 (Patient 9 in our study) [10]. Written informed consent was obtained from the parents of the pediatric patients and from the adult patients, in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics board of the National Defense Medical College and Tokyo Medical and Dental University.
Genetic Analysis
We performed whole-exome sequencing using the samples of patients, parents, and/or siblings by HiSeq 1500 (Illumina, San Diego, CA, USA) and identified DNMT3B mutations in three cases (Patients 5, 6, and 11) and ZBTB24 in one case (Patient 10). In two patients (Patients 1 and 7), we performed homozygosity mapping using SNP analysis by Human610-Quad (Illumina, San Diego, CA, USA) or Affymetrix CytoScan HD array (Thermo Fisher Scientific, Waltham, MA, USA). All mutations were ascertained to be homozygous (hemizygous) in the patients and heterozygous in the parents and/or siblings by Sanger sequencing with Applied Biosystems 3130xl Genetic Analyzer or Applied Biosystems 3500 Genetic Analyzer (Thermo Fisher Scientific, Waltham, MA, USA).
Centromeric Instability
G-banding chromosome analysis was performed with the stimulation of phytohemagglutinin (PHA) in five patients (Patients 1, 5–7, and 11). Four cases (Patients 3, 4, 8, and 9) had previously been reported to show typical chromosomal anomalies at 1qh and/or 16qh. PHA (J-chemical, Tokyo, Japan)-stimulated heparinized whole blood was cultured at 37 °C with 5% CO2 for 72 h in RPMI1640 with 10% FBS and 1% penicillin/streptomycin. During the last hour of culture, cells were exposed to colcemid (KaryoMAX Colcemid; Thermo Fisher Scientific, Waltham, MA, USA) at a final concentration of 0.05 μg/ml. Hypotonic treatment was performed with 0.075 M KCL at 37 °C for 15 min, followed by fixation with Carnoy’s fixative (acetic acid:methanol, 1:3). The metaphase chromosomes were treated with trypsin at 30 °C for 4 min and stained with 5% Giemsa stain for 7 min. At least 30 metaphases were analyzed. In three cases (Patients 1, 7, and 8), we reanalyzed the second G-banding chromosome analysis, with an increase in the examination time from 24 to 72 h after stimulation and an increase in analyses of metaphases to more than 30 cells.
Mitogen-Induced Lymphocyte Proliferation Tests
Tests of lymphocyte proliferation induced by mitogens (PHA and concanavalin A: Con A) were performed in five patients (Patients 1 and 6–9) and with PHA alone in one patient (Patient 10). Peripheral blood mononuclear cells were isolated from whole blood using Lymphosepar (Immuno-Biological Laboratories, Fujioka, Japan) density gradient centrifugation, in accordance with the manufacturer’s instructions. The cells (1 × 105) were cultured with PHA (7 μg/ml; J-chemical, Tokyo, Japan) or Con A (7 μg/ml, L1104-50; EY Laboratories, San Mateo, CA, USA) in 200 μl of RPMI 1640 medium with 10% FBS at 37 °C with 10% CO2 for 72 h. 3H-thymidine was added. The cells were harvested using Filter Mate Cell Harvester (Perkin Elmer, Waltham, MA, USA) and counted by TopCount NXT (Perkin Elmer, Waltham, MA, USA).
Flow Cytometric Analysis
Peripheral blood samples of eight patients with ICF syndrome (ICF1, n = 6 and ICF2, n = 2) were analyzed in our study. Two patients were analyzed before this study [10]. Four patients (Patients 1, 3, 4, and 7) were analyzed by a FACS Calibur system (BD Biosciences, Franklin Lakes, NJ, USA) using anti-human monoclonal antibodies (mAbs): in a first tube, CD45RA (FITC, clone L48; BD Biosciences), CD31 (PE, clone WM59; BD Biosciences), CD4 (PerCP, clone SK3; BD Biosciences), and CD3 (APC, clone UCHT1; Beckman Coulter, Brea, CA, USA); in a second tube, CD3 (FITC, clone SK7; eBioscience, Waltham, MA, USA), CD16 (PE, clone B73.1; BD Biosciences), CD56 (PE-Cy5, clone N901; Beckman Coulter), and CD19 (APC, clone J3-119; Beckman Coulter); and in a third tube, IgD (FITC, clone IA6-2; BD Biosciences), CD27 (PE, clone 1A4CD27; Beckman Coulter), IgM (PE-Cy5, clone G20-127; BD Biosciences), and CD19 (APC, clone J3-119; Beckman Coulter). The data were analyzed by single platform analysis using Cell Quest (BD Biosciences). Four patients (Patients 5, 6, 10, and 11) were analyzed by the LSR-Fortessa system (BD Biosciences, Franklin Lakes, NJ, USA), as reported previously [18]. The data were analyzed using FlowJo flow cytometry analysis software (FlowJo LLC, Ashland, OR, USA).
The normal percentages of control data were taken from a previous report [18], as were the normal absolute counts of control data [19]. We defined normal ranges of control data as from 10th (or − 1.28 SD) to 90th (or + 1.28 SD) [18, 19].
Quantification of TREC and KREC by Real-time PCR
Quantification of T cell receptor excision circles (TREC) and kappa-deleting recombination excision circles (KREC) was performed by TaqMan-based real-time quantitative polymerase chain reaction (PCR), as previously described [20, 21], using samples of gDNA from nine patients with ICF syndrome (ICF1, n = 6 and ICF2, n = 3). Copy numbers of TREC and KREC were evaluated as the levels per microgram of DNA, and copy numbers of less than 100 copies/μg of DNA were defined as “undetectable.”
Statistical Analysis
We conducted all statistical analyses by using GraphPad Prism software (GraphPad Software, San Diego, CA, USA). When we needed to compare two groups, we used the unpaired t test with Welch’s correction and considered a p value of < 0.05 as significant.
Results
Clinical Findings
Seven patients had ICF1 (Fig. 1, upper panel) and four patients had ICF2 (Fig. 1, lower panel). Four males and seven females were included. Six patients from four families (Patients 1–4, 9, and 11) were born to consanguineous parents (Fig. 1 and Table 1). The age at final observation and the age at immunological analysis did not differ between ICF1 and ICF2 [final observation age; ICF1, 23 ± 4 (range, 4–35 years) and ICF2, 22 ± 8 (range, 7–41 years), p = 0.93] [immunological analysis age; ICF1, 20 ± 4 (range, 4–33 years) and ICF2, 19 ± 8 (range, 5–39 years), p = 0.92].
Family pedigrees of the ICF1 or ICF2 patients. Upper panels (Families A–C and H) and lower panels (Families D–G) indicate family pedigrees of the ICF1 and ICF2 patients, respectively. Square symbols represent males and circular symbols represent females. Filled symbols show the patients and open symbols with a dot show the heterozygous mutated parents and/or siblings. Double line indicates consanguineous parents. wt, wild type; NA, not available
Infectious Episodes and Inflammatory Manifestations
A 28-year-old female (Patient 1) and her twin sister (Patient 2) contracted recurrent pneumonia and sinusitis. Patient 2 had suffered from arthritis and mild hepatitis without detectable autoantibodies since the age of 17 years (Table 1). A 15-year-old girl (Patient 3) and her 13-year-old brother (Patient 4) contracted recurrent pneumonia and otitis media (Table 1). A 33-year-old female (Patient 5) and her 29-year-old sister (Patient 6) contracted recurrent pneumonia and otitis media. Additionally, Patient 5 suffered from myositis without detectable antibodies. Patient 6 suffered from bronchiectasis with middle lobe syndrome. A 5-year-old girl (Patient 7) suffered from recurrent pneumonia (Table 1). In addition, a 5-year-old boy (Patient 8) suffered from pneumococcemia, recurrent pneumonia, recurrent cytomegalovirus (CMV) viremia, and persistent Epstein–Barr virus (EBV) infection with refractory diarrhea. Moreover, a 39-year-old man (Patient 9) suffered from recurrent pneumonia, recurrent sinusitis, and progressive multifocal leukoencephalopathy (PML) due to JC virus (Table 1). A 27-year-old man (Patient 10) suffered from recurrent pneumonia and bronchitis. Finally, a 4-year-old girl (Patient 11) suffered from recurrent otitis media and contracted sepsis suspected of being caused by Pseudomonas aeruginosa with neutropenia (Table 1).
Treatment and Outcome
All 11 patients had been treated with intravenous or subcutaneous immunoglobulin replacement therapy. We analyzed the period of immunoglobulin replacement therapy, for which there was no significant difference between ICF1 and ICF2 [ICF1, 20.4 ± 4.0 (range, 0.9–33) and ICF2, 10.0 ± 5.9 (range, 2–27) years, p = 0.20] or surviving or deceased patients [surviving, 20.2 ± 3.9 (range, 0.9–33) and deceased, 7.0 ± 5.0 (range, 2–17) years, p = 0.10]. Four patients (Patients 1, 7, 8, and 11) received trimethoprim–sulfamethoxazole (TMP/SMX) and one patient (Patient 7) received antifungal drug, whereas Patient 9 was administered cytarabine against PML. Four of the eight surviving patients who were not using TMP/SMX had been suffering from recurrent infection, but hospitalization was unnecessary in most cases. That is, Patient 3 suffered from bronchitis and pneumonia, Patient 4 pneumonia, Patient 5 urosepsis, and Patient 10 pneumonia. Infectious episodes decreased in two patients (Patients 1 and 11) who started TMP/SMX and one patient (Patient 7) who started TMP/SMX and antifungal drugs (Table 1). Patient 1 had suffered from recurrent bronchitis and sinusitis even after the replacement of immunoglobulin, but the frequency of fever decreased after starting TMP/SMX.
Three patients (Patients 2, 8, and 9) died despite sufficient immunoglobulin replacement therapy. Patient 2 died during recovery from influenza virus type B infection at the age of 18 (Table 1). In Patient 8, at the age of 5, Epstein–Barr virus was detected from blood and skin, with a copy number in blood of 1.4 × 106 copies/μg DNA. The infected cells in blood were confirmed to be T cells, not B cells. He died of fatal infection with persistent EBV infection at the age of 7 [10] (Table 1). Patient 9 died of progressive PML due to JC virus at the age of 41 [10] (Table 1).
Genetic Analysis
A total of 6 of 11 patients (Patients 1, 5–7, 10, and 11) were tentatively diagnosed as having common variable immunodeficiency. In 2 patients (Patients 1 and 7), we identified loss-of-heterozygosity regions containing the DNMT3B and ZBTB24 genes, respectively. c.1988G>T (p.G663V) mutation seen in Patient 11 was previously reported by others, whereas c.2189A>C (p.H730P) (Patient 1) and c.2384G>T (p.G795V) (Patients 5 and 6) were novel mutations in the DNMT3B gene (Fig. 2, upper panel). c.1369C>T (p.R457X) mutation seen in Patient 7 was previously reported by others, whereas c.1108_1109insA (p.S370fs) (Patient 10) was a novel mutation in the ZBTB24 gene (Fig. 2, lower panel). The mutations of four patients (Patients 3, 4, 8, and 9) had previously been reported (Fig. 2 and Table 1) [10, 17]. Four patients (Patients 5–8) from three families (Families C–E) had homozygous and/or hemizygous mutations, even though they were from nonconsanguineous families (Fig. 1).
Distributions of DNMT3B and ZBTB24 mutations in patients with ICF syndrome. A schematic shows the protein structures associated with the DNMT3B (upper panel) and ZBTB24 (lower panel) genes. Locations of the mutations identified in this study are shown by arrows. PWWP, PWWP domain; ADD, ADD domain; catalytic, catalytic domain; BTB, BTB domain; A-T, AT-hook; C2H2 zinc fingers, zinc finger domains
Centromeric Instability
All nine cases (Patients 1, 3–9, and 11) showed typical chromosomal anomalies at 1qh and/or 16qh (Table 1). Patients 1, 7, and 8 were ascertained to have centromeric instability in the second G-banding chromosome analysis and an increasing examination time of 72 h after stimulation.
Facial Anomalies
Facial anomalies were typical in six patients but were mild in five patients. Ocular hypertelorism was observed in six patients but was mild in five patients (Patients 1, 2, 5, 6, and 10). Epicanthic folds, broad flat nasal bridge, low-set ears, macroglossia, and micrognathia were observed in 7, 8, 5, 2, and 1 of 11 patients, respectively (Table 1).
Mental Status
Marked mental retardation was observed in three patients (one patient with ICF1 and two patients with ICF2) (Table 1). Eight patients (Patients 1–6, 8, and 10) showed normal intelligence levels, and five of them (Patients 1, 4–6, and 10) were able to attend an ordinary school or work without difficulty (Table 1).
Fertility
Two of six adult ICF patients (two ICF1 patients; Patient 5 and Patient 6) suffered from amenorrhea and one ICF2 patient (Patient 7) had no sign of secondary sexual characteristics at the age of 12. On the other hand, three of six adult ICF patients (two ICF1 and one ICF2; Patients 1, 2, and 10) showed normal gonadal function and one male ICF2 patient (Patient 10) had a child.
Immunological Analysis
A total of 9 of 11 patients with ICF syndrome showed low IgG levels [ICF1, 412 ± 145 (range, 138–1160) and ICF2, 513 ± 208 (range, 108–1088) mg/dL, p = 0.71] (Table 2, Fig. S1). Intriguingly, two patients with normal IgG levels (Patient 5, 1160 mg/dL and Patient 8, 1088 mg/dL) showed low IgG2 levels (Patient 5, 33 mg/dL and Patient 8, 41 mg/dL). Serum IgG2 was low in all five patients (Patients 5–9) (Table 2, Fig. S1B). Serum IgA levels were low in all patients [ICF1, 2 ± 1 (range, 0–7) and ICF2, 31 ± 14 (range, 0–69) mg/dL, p = 0.13], and IgA levels in patients with ICF1 were significantly lower than those in patients with ICF2 (Table 2, Fig. S1C). Serum IgM levels were variable in seven patients with ICF1; three patients showed low levels, one patient showed a normal level (Patient 6, 72 mg/dL), and two patients showed high levels (Patient 2, 300 mg/dL and Patient 11, 950 mg/dL). One patient (Patient 5) showed a high IgM level (265 mg/dL) at the age of 26, but this declined to a normal level (74 mg/dL) at the age of 33. In contrast, all patients with ICF2 showed significantly lower IgM levels [ICF1, 202 ± 131 (range, 4–950) and ICF2, 18 ± 8 (range, 0–40) mg/dL, p = 0.21] (Table 2, Fig. S1D).
Lymphocyte proliferation tests with PHA and Con A stimuli were performed in six patients with ICF syndrome (both in Patients 1, 5, and 7–9 and PHA only in Patient 10). Two of six patients showed low responses with PHA (Patient 9, 3150 cpm and Patient 10, 7910 cpm) [ICF1, 28,100 ± 7300 (range, 20,800–35,400) and ICF2, 21,640 ± 11,079 (range, 3150–52,300) cpm, p = 0.66] (Table 2) and two of five patients showed low responses with Con A (Patient 8, 10,400 cpm and Patient 9, 103 cpm) [ICF1, 31,101 ± 3910 (range, 27,200–35,002) and ICF2, 22,034 ± 17,044 (range, 103–55,600) cpm, p = 0.66] (Table 2).
Flow cytometric analyses were performed in 10 patients with ICF syndrome. Three of six patients, who were all adults, showed low percentages of CD3+ T cells compared with the normal control (Patient 1, 54.3%; Patient 5, 43.8%; and Patient 6, 54.4%). All patients with ICF2 showed significantly higher percentages of CD3+ T cells than the patients with ICF1 [ICF1, 61.8 ± 5.5% (range, 43.8–81.0%) and ICF2, 93.3 ± 1.9% (range, 90.0–97.0%), p = 0.0016] (Table 2, Fig. S2A). The CD4/8 ratio was inverted in two of six patients with ICF1 (Patient 1, 0.88 and Patient 3, 0.63) and three of four patients with ICF2 (Patient 7, 0.75; Patient 9, 0.32; and Patient 10, 0.54) [ICF1, 1.4 ± 0.4 (range, 0.6–3.0) and ICF2, 1.2 ± 0.6 (range, 0.3–3.0), p = 0.80] (Table 2, Fig. S2B). The level of CD31+ recent thymic emigrant cells (RTE) among CD3+CD4+CD45RA+ cells was low in one of six patients with ICF1 (Patient 3, 63.3%) and one of two patients with ICF2 compared with that in the normal control (Patient 10, 21.9%) (Table 2, Fig. S2C).
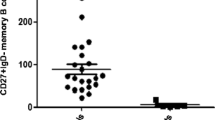
As for CD19+ B cells, two of six patients with ICF1 (Patient 6, 3.3% and Patient 11, 6.3%) and three of four patients with ICF2 (Patient 8, 3.0%; Patient 9, 1.0%; and Patient 10, 0.7%) showed low percentages of CD19+ B cells compared with the normal control. Three of six patients with ICF1 (Patient 1, 29.4%; Patient 3, 21.2%; and Patient 4, 25.0%) showed high percentages of CD19+ B cells compared with the normal control. Mean percentages of CD19+ B cells in patients with ICF2 were lower than those in patients with ICF1 [ICF1, 15.3 ± 4.6% (range, 3.3–29.4%) and ICF2, 3.0 ± 1.6% (range, 0.7–7.5%), p = 0.069] (Table 2, Fig. S2D). The percentages of CD27+ memory B cells were low in seven of nine patients with ICF compared with that in the normal control. One patient with ICF1 (Patient 11, 7.7%) and one patient with ICF2 (Patient 10, 8.7%) showed normal percentages of CD27+ memory B cells [ICF1, 3.7 ± 1.3% (range, 0.5–7.7%) and ICF2, 4.1 ± 2.4% (range, 0.3–8.7%), p = 0.88] (Table 2, Fig. S2E). The percentages of IgM+ memory B cells (CD27+IgM+IgD+) were low in 4 of 6 ICF1 patients and all 3 ICF2 patients compared with that in the normal control [ICF1, 3.08 ± 1.30% (range, 0.29–7.36%) and ICF2, 2.52 ± 1.52% (range, 0.34–5.45%), p = 0.79] (Table 2). The percentages of switched memory B cells (CD27+IgM+IgD−) were low in all nine patients compared with that in the normal control [ICF1, 0.58 ± 0.16% (range, 0.07–1.10%) and ICF2, 1.61 ± 0.93% (range, 0.00–3.22%), p = 0.39] (Table 2).
As for CD16+56+ NK cells, two of six patients with ICF1 (Patient 5, 21.8%; Patient 6, 23.5%) showed high percentages, while one of three patients with ICF2 (Patient 10, 0.68%) showed low percentages of CD16+56+ NK cells compared with the normal control. Mean percentages of CD16+56+ NK cells in patients with ICF2 were lower than those in patients with ICF1 [ICF1, 11.3 ± 3.7% (range, 3.3–23.5%) and ICF2, 2.2 ± 1.4 (range, 0.7–5.0%), p = 0.06] (Table 2, Fig. S2E).
TREC and KREC were analyzed in nine patients with ICF syndrome. TREC were undetectable in two patients with ICF1 (Patients 5 and 6), who had been positive for them 7 years earlier. There was no significant difference in TREC between ICF1 and ICF2 [ICF1, 10.9 ± 10.6 (range, < 0.1–64.0) × 103; ICF2, 2.00 ± 0.63 (range, 0.73–2.80) × 103 copies/μg of DNA, p = 0.44]. KREC were positive in all patients [ICF1, 11.9 ± 5.73 (range, 1.63–39.00) × 103; ICF2, 2.3 ± 0.93 (range, 1.37–4.2) × 103 copies/μg of DNA, p = 0.16] (Fig. 3).
TREC and KREC levels of patients with ICF syndrome. Copy numbers of TREC and KREC in six ICF1 patients (Patients 1, 3–6, and 11) and three ICF2 patients (Patients 7, 8, and 10) are shown. The age in parentheses indicates the age at the time of analysis of TREC and KREC. Copy numbers less than 100 copies/μg of DNA were defined as “undetectable.” TREC, T cell receptor excision circles; KREC, kappa-deleting recombination excision circles
Discussion
In this study, we newly diagnosed six ICF patients who had tentatively been diagnosed as having common variable immunodeficiency. Furthermore, we identified three novel mutations of c.2189A>C (p.H730P) (Patient 1) and c.2384G>T (p.G795V) (Patients 5 and 6) in the DNMT3B gene and c.1108_1109insA (p.S370fs) (Patient 10) in the ZBTB24 gene. In three families (Families C–E), we identified homozygous mutations even though they were nonconsanguineous families. The novel mutations found in DNMT3B (Patients 1, 5, and 6) were missense mutations in the catalytic domain, as previously reported [3], whereas the novel mutation found in ZBTB 24 (Patient 10) was also a nonsense mutation presented in zinc fingers, as previously reported [3]. We diagnosed two ICF patients by the presence of memory B cells. Although memory B cells were present in Patient 10, IgA deficiency was observed and NK cells were also few in number; thus, we suspected ICF syndrome and performed diagnosis using whole-exome sequencing. Although memory B cells were present and extremely high levels of IgM were seen in Patient 11, we suspected ICF based on facial anomalies and mental retardation and performed diagnosis with G-banding chromosome analysis and genetic analysis.
Serum IgG, IgG2, and IgA levels were all low in patients with ICF syndrome (ICF1 and ICF2), as reported previously [1,2,3]. Although serum IgM levels were reported to be low to normal in patients with both ICF1 and ICF2 [3], three patients with ICF1 were found to have increased levels of serum IgM. Notably, two of them (Patients 2 and 5) suffered from inflammatory manifestations. Although autoantibodies were not detected from both patients, these manifestations could be due to autoimmunity as a result of T cell immunodeficiency. CD19+ B percentages were low in one of six patients with ICF1 and three of four patients with ICF2. Lack of CD19+CD27+ memory B cells was observed in 9 of 11 patients, as previously reported [8]. Two patients showed normal percentages of CD19+CD27+ memory B cells (Patient 10, 8.7% and Patient 11, 7.7%). However, they both had decreased numbers of B cells (Patient 10, 11/μL and Patient 11, 317/μL) and also decreased absolute numbers of CD19+CD27+ memory B cells.
One patient (Patient 8) suffered from recurrent CMV viremia and persistent EB infection, and another (Patient 9) developed PML caused by JC virus infection. In addition, one patient (Patient 2) died during the recovery from influenza virus infection. These vulnerabilities to viral infection suggest the existence of T cell immunodeficiency in patients with ICF syndrome. Consistent with these observations, three patients (Patients 8–10) showed remarkably reduced responses in mitogen-induced lymphocyte proliferation tests. Three patients (Patients 1, 5, and 6) showed low percentages of CD3+ T cells, five patients (Patients 1, 3, 7, 9, and 10) showed an inverted CD4/CD8 ratio, and two patients showed decreased RTE (Patients 3 and 10). TREC progressively decreased over years in two patients (Patients 5 and 6), indicating poor T cell neogenesis [22]. Moreover, infectious episodes decreased in three patients who started taking TMP/SMX and/or antifungal drugs in addition to immunoglobulin replacement therapy. T cell abnormalities such as T cell apoptosis and a reduction of CD4+ T cells with aging had been reported in ICF syndrome [11,12,13]. It has been reported that three patients developed pneumocystis pneumonia and six patients did persistent candida stomatitis [2]. Three patients with ICF syndrome required HSCT because of the complications of persistent small round structured virus and candida infection, Pneumocystis jirovecii infection, and persistent enteritis with unknown cause [14]. In addition, one patient with ICF1 underwent HSCT because of P. jirovecii infection [15]. Previous reports were of individual cases showing T cell immunodeficiency in ICF syndrome. In this study, we used multiple methods such as clinical course analysis, lymphocyte proliferation test, lymphocyte subset analysis, and TREC and demonstrated T cell immunodeficiency in ICF syndrome. Therefore, patients with ICF syndrome should be treated as having T cell immunodeficiency in addition to receiving immunoglobulin replacement therapy.
Two patients with ICF1 (Patients 2 and 5) presented autoimmune or inflammatory manifestations that are uncommon in ICF syndrome. Patient 5 exhibited a decreased number of CD3+ T cells and undetectable TREC. One patient with ICF2 who suffered from autoimmune or inflammatory features also had decreased CD4+ T cells as a combined immunodeficiency [13]. It has been reported that two patients with ICF1 who were associated with autoimmune/inflammatory manifestations had a poor outcome, for whom the need for additional immunosuppressive treatment was proposed [8]. Patient 2 died during the recovery from influenza virus infection at the age of 18. These findings suggest that T cell disorders occur in ICF syndrome, especially in cases with autoimmune/inflammatory manifestations.
ICF syndrome is well known to be associated with facial anomaly. Regarding mental status, Weemaes et al. [3] reported mental retardation in all 13 ICF2 patients, but reported that mental retardation was not observed in almost half of the ICF1 patients. Sterlin et al. [8] reported marked mental retardation in one ICF2 patient, although intelligence was almost normal in ICF1 and ICF3 patients. In our study, 5 of 11 patients (four ICF: Patients 1, 2, 5, and 6; one ICF2: Patient 10) showed mild facial anomaly and normal intelligence (Table 1). Notably, four patients (Patients 1, 5, 6, and 10) are able to work without difficulty. All five patients were associated with typical immunodeficiency and/or immune dysregulation. That is, all five patients showed hypogammaglobulinemia. In total, one patient with ICF2 (Patient 10) showed a decreased mitogen-induced lymphocyte proliferation test result, three patients with ICF1 (Patients 1, 5, and 6) showed low percentages of CD3+ T cells, two patients (Patients 1 and 10) showed an inverted CD4/8 ratio, one patient with ICF2 (Patient 10) showed a low percentage of RTE, and two patients with ICF1 (Patients 5 and 6) showed undetectable TREC. Patient 2 with mild facial anomaly and normal intelligence died of viral infection. Therefore, immunodeficiency might not be closely related to facial anomaly and mental retardation in ICF syndrome.
Regarding the differences in clinical findings between ICF1 and ICF2, it was reported that intellectual impairment was mild in ICF1 and severe in all ICF2 patients [3] [8]. In our study, two ICF2 patients with normal mental intelligence were reported and one patient (Patient 10) was working without difficulty. We reported two ICF1 patients with autoimmune/inflammatory manifestations, which was the same as previously reported [8]. As a feature that had not been reported previously, we reported hypogonadism for the first time in two ICF1 patients and suspicion of this in one ICF2 patient. Regarding the differences of immunological findings between the two ICF subtypes, it was reported that the humoral immunodeficiency of ICF1 was more prominent than ICF2 [3]. As in a previous report, agammaglobulinemia and hypogammaglobulinemia were more prominent in ICF1, but three ICF1 patients showed extremely high levels of IgM and were also found to have autoimmune/inflammatory manifestations. Regarding the results of the mitogen-induced lymphocyte proliferation test, they were reported to worsen in some ICF cases (subtype unknown) [2], while normal results were also reported in both ICF1 and ICF2 types [8]. Our study showed that this test result worsened in half (3 out of 6 patients) of the cases examined, all of which were ICF2 patients. In this study, we newly discovered that ICF2 patients show lower percentages of CD19+ B cells and CD16+56+ NK cells and significantly higher percentages of CD3+ T cells than ICF1 patients. In addition, although normal TREC results were reported in a single ICF1 patient [12], we newly discovered that TREC declined and became undetectable in two ICF1 patients (Patients 5 and 6).
Our results suggest that a poor prognosis of ICF syndrome might be caused by the associated T cell immunodeficiency. We propose that ICF syndrome should be managed and treated as a combined immunodeficiency, in addition to the administration of immunoglobulin replacement therapy (i.e., antibacterial drugs including trimethoprim–sulfamethoxazole, antiviral drugs, and/or HSCT). The number of patients examined was limited in this study, and further studies are necessary to clarify the detail of the T cell immunodeficiency in ICF syndrome and what types of treatments are needed for particular kinds of ICF patients.
Abbreviations
- CDCA7:
-
Cell division cycle-associated protein 7
- Con A:
-
Concanavalin A
- DNMT3B:
-
DNA methyltransferase 3B gene
- HELLS:
-
Helicase, lymphoid-specific
- HSCT:
-
Hematopoietic stem cell transplantation
- ICF:
-
Immunodeficiency, centromeric instability, and facial anomalies
- KREC:
-
Kappa-deleting recombination excision circles
- NGS:
-
Next-generation sequencing
- PCR:
-
Polymerase chain reaction
- PHA:
-
Phytohemagglutinin
- PML:
-
Progressive multifocal leukoencephalopathy
- RTE:
-
Recent thymic emigrant cells
- TREC:
-
T cell receptor excision circles
- ZBTB24:
-
Zinc finger and BTB domain-containing 24 gene
References
Ehrlich M, Jackson K, Weemaes C. Immunodeficiency, centromeric region instability, facial anomalies syndrome (ICF). Orphanet J Rare Dis. 2006;1:2.
Hagleitner MM, Lankester A, Maraschio P, Hultén M, Fryns JP, Schuetz C, et al. Clinical spectrum of immunodeficiency, centromeric instability and facial dysmorphism (ICF syndrome). J Med Genet. 2008;45:93–9.
Weemaes CM, van Tol MJ, Wang J, et al. Heterogeneous clinical presentation in ICF syndrome: correlation with underlying gene defects. Eur J Hum Genet. 2013;21:1219–25.
Xu GL, Bestor TH, Bourc’his D, Hsieh CL, Tommerup N, Bugge M, et al. Chromosome instability and immunodeficiency syndrome caused by mutations in a DNA methyltransferase gene. Nature. 1999;402:187–91.
Hansen RS, Wijmenga C, Luo P, Stanek AM, Canfield TK, Weemaes CMR, et al. The DNMT3B DNA methyltransferase gene is mutated in the ICF immunodeficiency syndrome. Proc Natl Acad Sci U S A. 1999;96:14412–7.
de Greef JC, Wang J, Balog J, den Dunnen J, Frants RR, Straasheijm KR, et al. Mutations in ZBTB24 are associated with immunodeficiency, centromeric instability, and facial anomalies syndrome type 2. Am J Hum Genet. 2011;88:796–804.
Thijssen PE, Ito Y, Grillo G, Wang J, Velasco G, Nitta H, et al. Mutations in CDCA7 and HELLS cause immunodeficiency-centromeric instability-facial anomalies syndrome. Nat Commun. 2015;6:7870.
Sterlin D, Velasco G, Moshous D, Touzot F, Mahlaoui N, Fischer A, et al. Genetic, cellular and clinical features of ICF syndrome: a French national survey. J Clin Immunol. 2016;36:149–59.
Blanco-Betancourt CE, Moncla A, Milili M, Jiang YL, Viegas-Péquignot EM, Roquelaure B, et al. Defective B-cell-negative selection and terminal differentiation in the ICF syndrome. Blood. 2004;103:2683–90.
Nitta H, Unoki M, Ichiyanagi K, Kosho T, Shigemura T, Takahashi H, et al. Three novel ZBTB24 mutations identified in Japanese and Cape Verdean type 2 ICF syndrome patients. J Hum Genet. 2013;58:455–60.
Pezzolo A, Prigione I, Facchetti P, Castellano E, Viale M, Gimelli G, et al. T-cell apoptosis in ICF syndrome. J Allergy Clin Immunol. 2001;108:310–2.
Rechavi E, Lev A, Eyal E, Barel O, Kol N, Barhom SF, et al. A novel mutation in a critical region for the methyl donor binding in DNMT3B causes immunodeficiency, centromeric instability, and facial anomalies syndrome (ICF). J Clin Immunol. 2016;36:801–9.
von Bernuth H, Ravindran E, Du H, et al. Combined immunodeficiency develops with age in immunodeficiency-centromeric instability-facial anomalies syndrome 2 (ICF2). Orphanet J Rare Dis. 2014;9:116.
Gennery AR, Slatter MA, Bredius RG, Hagleitner MM, Weemaes C, Cant AJ, et al. Hematopoietic stem cell transplantation corrects the immunologic abnormalities associated with immunodeficiency-centromeric instability-facial dysmorphism syndrome. Pediatrics. 2007;120:e1341–4.
Gössling KL, Schipp C, Fischer U, Babor F, Koch G, Schuster FR, et al. Hematopoietic stem cell transplantation in an infant with immunodeficiency, centromeric instability, and facial anomaly syndrome. Front Immunol. 2017;8:773.
Stiehm ER, Fudenberg HH. Serum levels of immune globulins in health and disease: a survey. Pediatrics. 1966;37:715–27.
Shirohzu H, Kubota T, Kumazawa A, Sado T, Chijiwa T, Inagaki K, et al. Three novel DNMT3B mutations in Japanese patients with ICF syndrome. Am J Med Genet. 2002;112:31–7.
Takashima T, Okamura M, Yeh TW, Okano T, Yamashita M, Tanaka K, et al. Multicolor flow cytometry for the diagnosis of primary immunodeficiency diseases. J Clin Immunol. 2017;37:486–95.
Shearer WT, Rosenblatt HM, Gelman RS, Oyomopito R, Plaeger S, Stiehm ER, et al. Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol. 2003;112:973–80.
Morinishi Y, Imai K, Nakagawa N, Sato H, Horiuchi K, Ohtsuka Y, et al. Identification of severe combined immunodeficiency by T-cell receptor excision circles quantification using neonatal Guthrie cards. J Pediatr. 2009;155:829–33.
Nakagawa N, Imai K, Kanegane H, Sato H, Yamada M, Kondoh K, et al. Quantification of κ-deleting recombination excision circles in Guthrie cards for the identification of early B-cell maturation defects. J Allergy Clin Immunol. 2011;128:223–5.e2.
Kamae C, Nakagawa N, Sato H Honma K, Mitsuiki N, Ohara O, Kanegane H, Pasic S, Pan-Hammarström Q, van Zelm MC, Morio T, Imai K, Nonoyama S. Common variable immunodeficiency classification by quantifying T-cell receptor and immunoglobulin κ-deleting recombination excision circles. J Allergy Clin Immunol 2013; 131: 1437–40.e5.
Acknowledgments
We thank Dr. Takehiro Takashima, Dr. Koichi Inagaki, Dr. Naomi Terada, Ms. Kaori Tomita, and Ms. Kimiko Gasa for their excellent technical assistance. We are grateful to the patients and their families for their participation in this study.
Authorship Contributions
C.K., K.I., H.K., and S.N. designed the study and wrote the manuscript. T.K., K.H., N.N., and T-W.Y. performed the flow cytometric analysis and collected the data. T.O., E.N., and O.O. performed the gene analysis. A.O., T.S., H.T., S.T., M.H., A.H., S.W., and T.S. cared for the patients. H.S., T.K., and T.M. contributed to the critical discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent was obtained from the parents of the pediatric patients and from the adult patients, in accordance with the Declaration of Helsinki. The study protocol was approved by the ethics board of the National Defense Medical College and Tokyo Medical and Dental University.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Electronic Supplementary Material
Figure S1
Immunoglobulin levels of ICF patients. Serum immunoglobulin levels of patients with ICF1 (white circle) and ICF2 (black circle) are shown. (A) Serum levels of IgG. (B) Serum levels of IgG2. (C) Serum levels of IgA. (D) Serum levels of IgM. Each immunoglobulin value is expressed separately for the ICF subtypes (ICF1 or ICF2) and each age group (7–12 months old, 3–5 years old, and adult). The horizontal bars in the figures show the average value of each age group. (PPTX 90 kb). The normal values of serum level globulins were taken from Stiehm et al. [16]. We defined normal ranges of serum levels of globulins as from 10th (or − 1.28 SD) to 90th (or + 1.28 SD) [16] as shown by vertical bars.
Figure S2
Lymphocyte subpopulations of patients with ICF syndrome. Lymphocyte subpopulations of patients with ICF1 (white circle) and ICF2 (black circle) are shown. (A) Percentages of CD3+ T cells. (B) The ratios of CD4+ to CD8+ T cell lymphocytes. (C) Percentages of CD31+ recent thymic emigrant cells (RTE) among CD3+CD4+CD45RA+ cells. (D) Percentages of CD19+ B cells. (E) Percentages of CD19+CD27+ memory B cells. (F) Percentages of CD16+56+ NK cells. Each lymphocyte subpopulation is expressed separately for the ICF subtypes (ICF1 or ICF2) and each age group (2–6 years old, 7–19 years old, and adult). The horizontal bars in the figures show the average value of each age group. The normal percentages of control data were taken from the work of Takashima et al. [18]. Vertical bars indicate the range from − 1.28 standard deviations (10th) to + 1.28 standard deviations (90th) of normal controls of each age group (PPTX 121 kb)
Rights and permissions
About this article
Cite this article
Kamae, C., Imai, K., Kato, T. et al. Clinical and Immunological Characterization of ICF Syndrome in Japan. J Clin Immunol 38, 927–937 (2018). https://doi.org/10.1007/s10875-018-0559-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-018-0559-y