Abstract
Objective
The aim of this study was to determine whether interleukin-1 alpha (IL1α), interleukin-1 beta (IL1β), and IL1 receptor antagonist (IL1Ra) polymorphisms are implicated in invasive pulmonary aspergillosis (IPA) pathogenesis.
Materials and Methods
Subjects comprised 110 hematological patients and 148 healthy controls. Genotypic and allelic frequencies were similar between hematological patients and controls. IPA was diagnosed in 59 of the 110 patients according to consensus criteria published by the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group (EORTC/IFICG).
Results and Discussions
Individual locus analysis showed that IL1α and IL1Ra polymorphisms were not associated with the presence of IPA (p = 0.560 and p = 0.680, respectively). However, a trend towards a higher presence of IL1β - 511TT genotype (or IL1β-511T allele) in the IPA group than in the non-IPA patient group (p = 0.092 and p = 0.095, respectively) was found. Haplotype analysis revealed that VNTR2/-889C/-511T haplotype was strongly associated with susceptibility to develop IPA infection (p = 0.020). Haplotype analysis also showed an association between VNTR2/-889C/-511C haplotype and resistance to IPA infection (p = 0.028). Furthermore, patients with IL1Ra VNTR2/2 and IL1β-511T/T genotypes had a higher positive serum galactomannan percentage versus patients with other genotypes. Finally, C-reactive protein (CRP) production was significantly associated with IL1 gene cluster polymorphisms, although CRP values were similar between IPA and non-IPA groups.
Conclusion
These findings indicate a critical role of IL1 gene cluster polymorphisms in the susceptibility to IPA infection and CRP production.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Invasive pulmonary aspergillosis (IPA) is probably the most lethal fungal infection [1]. An intact host defense is important to prevent disease, and individuals with depleted immune system are highly susceptible to this opportunistic infection [2–4]. In fact, IPA is predominantly found in immunocompromised and hematopoietic stem cell transplantation (HSCT) patients [5–11]. Despite the availability of new antifungal drugs, the incidence of IPA infection is rising [5, 12, 13], and there has been a steady increase in mortality from IPA over the past decades [14]. There is therefore an urgent need to identify biomarkers that can reliably characterize susceptibility to develop IPA.
In humans, antifungal defense is based on mucosal barriers and macrophage and neutrophil functions. Resident alveolar macrophages ingest and kill resting conidia, while neutrophils attack hyphae via oxidative mechanisms [15]. There is also substantial evidence that local production of proinflammatory cytokines by macrophages and neutrophils is relevant in host resistance to IPA [16–20]. Proinflammatory cytokines such as IL1 are involved in enhancing inflammation and host defense. IL1 is encoded by two separate genes, interleukin-1 alpha (IL1α) and interleukin-1 beta (IL1β), located at chromosomal band 2q14 in a cluster that also contains the IL1 receptor antagonist (IL1Ra) [21]. These three members of the family are structurally related to one another and act by directly binding to IL-1 receptors (IL1R) on cells [22, 23]. IL1α and IL1β fold in a very similar manner and their sequence similarity is also high, ranging from 60% to 80%. IL1α and IL1β are potent agonists and recognize the same receptor, type I IL1 receptor (IL1RI) [24]. IL1Ra acts as a naturally occurring antagonist to this receptor, thereby blocking the biological effects of agonists.
These cytokines are produced by various cell types, including peripheral blood monocytes, human B cells, helper T lymphocytes, and natural killer cells [23]. The IL1α secreted by activated alveolar macrophages has profound local and systemic effects, increasing capillary permeability and the expression of different adhesion molecules, thereby inducing extravasation of activated neutrophils [24]. Moreover, IL1α induces production of acute phase protein such as C-reactive protein (CRP) that activates complement system in response to tissue injury or infection [25]. Activated alveolar macrophages also produce IL1β, which participates in the recruitment of neutrophils into acutely injured lungs. Nearly all of the cell types that produce IL1α and IL1β also produce IL1Ra. Hence, IL1 family cytokines may play a critical role in IPA pathogenesis.
Present outcome data for IPA infection are unacceptable, with an overall 1-year survival rate of around 20% [26]. Epidemiologic risk factors for IPA are increasingly understood but only explain a portion of disease risk. Many researchers have investigated a common set of genetic variations in the IL1 gene cluster and its association with an increased risk of developing rheumatoid arthritis, polyarthritis, coronary artery disease, and inflammatory bowel disease, among other conditions [27–30]. Investigators are beginning to consider the contribution of the host’s genetic background to the risk of IPA [31, 33].
Polymorphisms in genes modulating immune response are likely to be determinants of host susceptibility to fungal infections and may become critically important during periods of immunosuppression. Our understanding of the host’s genetic contribution to IPA risk and/or progression will be improved by the detection of genetic polymorphisms that regulate susceptibility to this infection. In fact, genetic association studies using polymorphic markers in candidate genes have successfully identified a number of genes associated with susceptibility to IPA infection. These include immune system genes such as IL10 [31, 32] and tumor necrosis factor receptor 2 (TNFR2) [33]. Elucidation of the genetic susceptibility profile may allow implementation of specific prophylaxis strategies in high-risk patients and the development of potentially novel therapies.
The capacity of the host to mount an IL1α driven response is influenced by sequence variants in the IL1/IL1Ra cluster. All IL1 family genes are polymorphic, and several of their polymorphisms have been associated with a wide number of clinical conditions, including susceptibility to sepsis [34, 35], increased risk of death due to sepsis [36], increased risk of febrile seizures [37, 38], and susceptibility to tuberculosis [39, 40], malaria [41], or periodontitis [42].
Because an individual’s capability to synthesize these cytokines can be altered by the presence of variant alleles [43–46], genetic polymorphisms of IL1 family genes are potential candidate genes of susceptibility to infectious diseases. Therefore, the aim of this study was to identify whether certain genetic variants of IL1α, IL1β, or IL1Ra genes confer susceptibility or resistance to IPA infection. A search of the literature revealed no previous study of these relationships.
Materials and Methods
Study Subjects and Study Design
All determinations and genetic analyses in hematological patients and healthy controls were performed with fully informed written consent, and anonymity of the data was guaranteed. The study was approved by the ethics review board of our hospital.
The population included 110 hematological patients admitted to our Department of Haematology between January 2004 and June 2007. All hematological patients in this study received a prolonged chemotherapy treatment and were therefore considered susceptible to develop IPA. One hundred forty-eight age-matched controls were also enrolled from among blood donors with no history of hematological disease or evidence of IPA infection. Patients and healthy controls were of Spanish origin (Caucasian).
A candidate gene-association approach was used to address the role of IL1 cluster genes in the pathogenesis of IPA. Hematological patients were classified into two categories (IPA and non-IPA patients) according to criteria recently published by the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group (EORTC/IFICG) [47]. The diagnosis was assigned by physician investigators in a blinded fashion.
The following single nucleotide polymorphisms (SNPs) were selected for the study: IL1α-889 (C/T) (rs1800587) and IL1β-511 (C/T) (rs1143627) [48, 49]. An 86-bp variable number of tandem repeats (VNTR) in second intron of IL1Ra gene (rs380092) was also investigated [50]. The effect of the three polymorphisms on IPA risk was investigated by using a retrospective cohort study.
Clinical Parameters
Clinical data were obtained by a detailed review of hospital records. IPA diagnosis was established on the basis of clinical, radiological, and microbiological data according to consensus criteria [47]. Underlying disease and bone marrow transplantation were correlated with the following types of criteria: host factor criteria (severe neutropenia for >10 days, persistent fever for >96 h refractory to appropriate broad-spectrum antibacterial treatment in high-risk patients, signs and symptoms indicating graft-versus-host disease, corticoid therapy in previous 60 days, and invasive fungal infection during a previous episode of neutropenia), microbiological criteria (positive result for Aspergillus antigen in ≥2 blood samples), and clinical criteria of lower respiratory tract infection (major criteria, any of the following new infiltrates on computed tomography (CT) imaging: halo sign, air-crescent sign, or cavity within area of consolidation; Minor criteria, cough, thoracic pain, hemoptysis, pathologic pulmonary sound, and radiological evidence suggestive of invasive infection).
Galactomannan Detection
Serum galactomannan (GM) detection has been shown to be a useful test for the early diagnosis and follow-up of IPA and is now included in IPA diagnosis criteria [47]. Sandwich enzyme-linked immunosorbent assay (ELISA) has proven to offer good sensitivity to detect GM [51–54], and GM concentration was found to correlate with the fungal tissue burden [54–57]. In the present study, serum GM antigen was determined twice weekly during the hospital stay and at each outpatient visit until the end of their immunosuppressant or chemotherapeutic treatment. Serum GM concentrations were determined by Platelia Aspergillus ELISA (Bio-Rad, Marnes-la-Coquette, France), which uses a rat monoclonal antibody directed against the (1–3)-β-d-galactofuranoside side chains of the GM molecule. This antibody, produced by immunizing rats with a mycelial extract of Aspergillus fumigatus, serves as both capture and detection antibody in the assay, which can detect as little as 1.0 ng/ml of circulating GM. ELISA was carried out according to the manufacturer’s instructions. A test sample was classified as positive when the optical density ratio was >0.5 and two successive positive samples indicated presence of GM in serum, a sign of IPA. A careful review of concomitant treatments (piperacillin-tazobactam or amoxicillin-clavulonic acid) in each patient was necessary to avoid false-positive GM results. Likewise, tests were performed on the same day to avoid sample contamination and ensure accuracy of results.
Plasma IL1α and IL1β Levels
Plasma samples were obtained by centrifugation of ethylenediaminetetraacetic acid blood at 1,800 rpm for 15 min and stored at −20°C until required. Plasma IL1α and IL1β levels were determined in both IPA and non-IPA groups. Plasma samples of patients with IPA infection were analysed after detection of positive GM. IL1α and IL1β levels were quantified using both human IL1α and IL1β ELISA kits (BLK Diagnostics, Barcelona, Spain) according to the manufacturer’s instructions.
C-reactive Protein Levels
CRP data were available in 101 patients. CRP values were determined by Synchron LX®I 725 Ingegrated Chemistry/Immunoassay System (Beckman Coulter). Serum sample for CRP analysis was collected at appearance of respiratory symptoms. CRP values were collected restrospectively by review of clinical records.
Polymorphism Analysis
IL1α, IL1β, and IL1Ra polymorphisms were detected in samples from hematological patients and controls by polymerase chain reaction (PCR) using previously reported primers [48–50] that amplified a short fragment of DNA containing the polymorphism (Table I). PCR amplifications were carried out in a total volume of 50 μl using an identical reaction mixture containing approximately 50 ng genomic DNA, 1 U GoTaq Flexi DNA polymerase (Promega, Madison, WI, USA), 0.5 μM of each primer (Genotek, Bonsai Technologies Group, Madrid, Spain), 5× green buffer (Promega), 1.5 mM MgCl2 (Promega), 200 μM of each deoxyribonucleotide triphosphate (GeneCraft, Münster, Germany), and H2O. Thermal cycling parameters were optimized for use with a Px2 Thermal Cycler (Thermo Electron®, Göttingen, Germany). Amplification conditions for IL1α, IL1β, and IL1Ra SNPs are also shown in Table I. The two alleles at each polymorphic site were identified by incubating the PCR product with a restriction enzyme selected to cut one of the two alleles (Table I), followed by electrophoresis on 3% agarose gel. IL1Ra VNTR alleles were also determined by identifying the number of repeats of an 86-bp sequence directly by electrophoresis on 3% agarose gel.
Statistical Analysis
Distributions of genotypes of IL1α, IL1β, and IL1Ra polymorphisms were examined to determine whether they followed the Hardy–Weinberg equilibrium, using the chi-square (χ 2) test. Results obtained for each genotype were compared with these expected data. Allele frequencies were calculated by direct gene counting. Results were analyzed by constructing contingency tables to determine differences in genotypic and allelic frequencies of studied polymorphisms among IPA patients, non-IPA patients, and controls. The IPA risk associated with the genotypes was estimated using odds ratios (OR) and 95% confidence intervals. ORs were adjusted for possible confounders (age and gender). P < 0.05 was considered significant.
The SNPStats program (Institut Català d’Oncología, Hospital Duran i Reinals, Barcelona, Spain; http://bioinfo.iconcologia.net/snpstats/start.html) was used for the data analysis [58].
Clinical characteristics were compared among groups by using the chi-square test. Clinical, radiological, and microbiological characteristics of the infection were summarized using descriptive statistics. Clinical data were compared among groups by using Tabulated Data Epidemiological Analysis (EPIDAT) 3.1 version for Windows. CRP values were analyzed and graphically represented using the System Package for Statistical Software (SPSS) 15.0 version for Windows.
LD and Haplotype Analysis
Based on the genotype data of the IL1α, IL1β, and IL1Ra polymorphisms, linkage disequilibrium (LD) analysis was performed using the SNPStats program [58]. Haplotype frequencies were implemented with SNPStats software using the expectation–maximization (EM) algorithm. This approach has a high predictive value and shows good concordance (90–98%) with pedigree data and simulated sample set analysis [59, 60].
Results
Hematological Patient and Control Populations: Clinical Characteristics
The hematological and control populations did not differ in gender or age. Hematological disorders were distributed as follow: 18 (16.36%) cases of acute lymphoid leukemia, 42 (38.18%) of acute myeloid leukemia, 10 (9.09%) of Hodgkin’s disease, 27 (24.55%) of non-Hodgkin’s lymphoma, ten (9.09%) of multiple myeloma, and three (2.73%) of aplastic anemia. There were no differences in the distribution of underlying disease between IPA and non-IPA patients. Out of the 110 patients studied, 79 (71.81%) developed neutropenic fever with a duration of ≥2 weeks. Fifty-nine patients were diagnosed with IPA infection according to EORTC/IFICG and the National Institute of Allergy and Infectious Disease Mycoses Study Group (NIAID/MSG) criteria [47], and the remaining 51 showed no evidence of IPA. Gender or age distributions were similar among IPA and non-IPA patients. Table II shows clinical comparisons between IPA and non-IPA patients. As expected, cough, pathologic pulmonary sound, and hemoptysis were significantly more frequent in IPA patients versus non-IPA patients. Thoracic pain did not significantly differ between the groups but showed a trend towards an increased frequency in IPA versus non-IPA patients. Radiological infiltrates and pathological CT imaging were significantly more frequent in IPA patients versus non-IPA patients. The main risk factors (severe neutropenia and corticoid therapy) were homogeneously distributed between IPA and non-IPA patients (Table II). There were no differences in the distribution of underlying disease between IPA and non-IPA patients.
IL1α, IL1β, and IL1Ra Polymorphisms
No deviations from Hardy–Weinberg equilibrium were observed for IL1α, IL1β, and IL1Ra polymorphisms in hematological patients or healthy controls. The distribution of IL1Ra VNTR, IL1α - 889(C/T) or IL1β-511(C/T) genotypes and the corresponding allelic frequencies of 148 healthy blood donors are summarized in Table III. These frequencies are similar to previous reports [50, 61–64]. Only four out of the possible five alleles were found in our controls. In this healthy population, IL1Ra VNTR distribution of 1/1, 1/2, 2/2, 1/4, and 1/3 genotype frequencies were 0.540, 0.324, 0.094, 0.013, and 0.020, respectively. The genotype and allele frequencies of the hematological patients are summarized in Table III. Alleles 3, 4, and 5 of IL1Ra VNTR were not represented in the hematological patient groups. The distribution of 1/1, 1/2, and 2/2 genotype frequencies were 0.536, 0.354, and 0.110, respectively. No significant differences between hematological patients and healthy controls were found in the genotype and allelic distributions of IL1Ra VNTR or IL1α-889(C/T) and IL1β-511(C/T) polymorphisms (Table III).
No significant difference in any genotype was found between the IPA and non-IPA patient groups. Similar data were obtained with recessive or dominant models. IL1α-889(C/T) distribution of C/C, C/T, and T/T genotype frequencies was 0.457, 0.407, and 0.136, respectively, in IPA patients and 0.529, 0.314, and 0.157, respectively, in non-IPA patients. Allele frequency of IL1α-889C was 0.661 in IPA patients versus 0.686 in non-IPA patients (p = 0.799, OR = 0.89, 95% CI, 0.49–1.63; Table IV). IL1β-511(C/T) distribution of C/C, C/T, and T/T genotype frequencies was 0.288, 0.559, and 0.152, respectively, in IPA patients and 0.431, 0.510, and 0.059, respectively, in non-IPA patients (p = 0.110). However, using a recessive model analysis, trend was found toward a higher presence of IL1β-511TT genotype in IPA group than in non-IPA patient group (p = 0.092). Allele frequency of IL1β-511C was 0.568 in IPA patients versus 0.686 in non-IPA patients (p = 0.095; OR = 0.60; 95% CI, 0.33–1.08; Table IV). To conclude, IL1Ra VNTR distribution of 1/1, 1/2, and 2/2 genotype frequencies was 0.508, 0.390, and 0.102, respectively, in IPA patients and 0.569, 0.314, and 0.118, respectively, in non-IPA patients. Allele frequency of IL1Ra1 was 0.703 in IPA patients versus 0.726 in non-IPA patients (p = 0.832; OR = 0.90; 95% CI 0.48–1.68; Table IV).
Linkage Disequilibrium Analysis and Haplotype Analysis
As expected, IL1α-889(C/T), IL1β-511(C/T), and IL1Ra polymorphisms were in LD in our hematological patients (IL-1α-889(C/T) versus IL-1β-511 (C/T): D′ = 0.2483 and r = −0.1348; IL-1α-889 (C/T) versus IL-1Ra VNTR: D′ = 0.0704 and r = 0.0639; IL-1β-511 (C/T) versus IL-1Ra VNTR: D′ = 0.2668 and r = −0.2171). Haplotype frequency estimates are shown in Table V. Eight haplotypes were identified in the hematological patients. Haplotype frequency analyses with the EM algorithm showed that the haplotype distribution significantly differed between IPA and non-IPA groups. Haplotype analysis revealed a significantly higher presence of VNTR2/-889C/-511T haplotype in the IPA group than in the non-IPA group (p = 0.020; Table V). Hence, the VNTR2/-889C/-511T haplotype was associated with IPA susceptibility. Furthermore, haplotype analysis showed a significantly higher presence of the VNTR2/-889C/-511C haplotype in the non-IPA group than in the IPA group (p = 0.028; Table V). Therefore, VNTR2/-889C/-511C haplotype was associated with resistance to IPA. The global haplotype association p value was 0.026, showing a significant global association of IL1 cluster genes with IPA susceptibility (Table V).
IL1α and IL1β Levels
IL1α levels were similar between patients with and without IPA (2.71 ± 0.82 versus 2.53 ± 0.79 pg/ml), and no differences were found as a function of genotype (data not shown). IL1β levels were similar between IPA and non-IPA groups. Plasma IL1β levels were below the assay limit in 45 of IPA patients (n = 59) and 33 of non-IPA patients (n = 51).
GM Antigen Analysis
GM levels were detected in serum at an early stage of disease, often before clinical clues and radiological features. A mean of 24.12 determinations were performed in duplicate for each IPA patient and a mean of 4.39 determinations in duplicate for each non-IPA patient. A total of 1,647 assays were performed in duplicate, and 262 (15.91%) were positive. No significant association was found between positive GM percentage distribution and IL1α-889(C/T) genotypes (Fig. 1a). However, a significantly higher positive GM percentage was observed in patients with IL1β-511(C/T) genotype TT than in those with IL1β-511 (C/T) genotypes CC or CT (p = 0.0015 and p < 0.0001, respectively; Fig. 1b). Likewise, a significantly higher positive GM percentage was observed in patients with IL1Ra genotype 2/2 than in those with IL1Ra genotype 1/1 or 1/2 (p = 0.0024 and p = 0.0266, respectively; Fig. 1c). Taken together, these results strongly suggest that both IL1β-511(C/T) and IL1Ra polymorphisms may have a relevant role in IPA susceptibility and possibly in infection disease progression.
a Distribution of positive GM percentage by IL1α genotypes. ‡Comparison of positive GM percentage in CC genotype versus CT genotype patients (p = 0.1311).*Comparison of positive GM percentage in CC genotype versus TT genotype patients (p = 0.9661). +Comparison of positive GM percentage in CT genotype versus TT genotype patients (p = 0.4201). b Distribution of positive GM percentage by IL1a genotypes. ‡Comparison of positive GM percentage in CC genotype versus CT genotype patients (p = 0.3513).*Comparison of positive GM percentage in CC genotype versus TT genotype patients (p = 0.0015). +Comparison of positive GM percentage in CT genotype versus TT genotype patients (p < 0.0001). c Distribution of positive GM percentage by IL1Ra genotypes. ‡Comparison of positive GM percentage in 1/1 genotype versus 1/2 genotype patients (p = 0.5097). *Comparison of positive GM percentage in 1/1 genotype versus 2/2 genotype patients (p = 0.0024). +Comparison of positive GM percentage in 1/2 genotype versus 2/2 genotype patients (p = 0.0266)
CRP Analysis
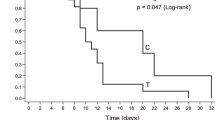
CRP values were significantly higher in patients with IL1Ra genotype 2/2 than in those with IL1Ra genotypes 1/2 or 1/1 (p < 0.0001 and p < 0.0001, respectively; Fig. 2a). CRP values were also significantly higher in patients with IL1α-889(C/T) genotype CC than in those with IL1α-889(C/T) genotypes CT or TT (p < 0.0001 and p = 0.0210, respectively; Fig. 2b). Likewise, a significantly higher CRP level was observed in patients with IL1β-511(C/T) genotype TT than in those with IL1β-511(C/T) genotype CT or TT (p = 0.0722 and p = 0.0012, respectively; Fig. 2c). Taken together, these results strongly suggest that IL1 gene cluster polymorphisms are involved in the modulation of CRP levels. Further, CRP levels were similar between IPA and non-IPA groups (9.73 versus 9.30 mg/dl, respectively).
a Distribution of CRP values by IL1Ra genotypes. ‡Comparison of CRP values in 1/1 genotype versus 1/2 genotype patients (p = 0.1477). *Comparison of CRP values in 1/1 genotype versus 2/2 genotype patients (p < 0.0001). +Comparison of CRP values in 1/2 genotype versus 2/2 genotype patients (p < 0.0001). b Distribution of CRP values by IL1α genotypes. ‡Comparison of CRP values in CC genotype versus CT genotype patients (p < 0.0001). *Comparison of CRP values in CC genotype versus TT genotype patients (p = 0.0210). +Comparison of CRP values in CT genotype versus TT genotype patients (p = 0.8743). c Distribution of CRP values by IL1β genotypes. ‡Comparison of CRP values in CC genotype versus CT genotype patients (p < 0.0001). *Comparison of CRP values in CC genotype versus TT genotype patients (p = 0.0012). +Comparison of CRP values in CT genotype versus TT genotype patients (p = 0.0722)
Discussion
Aspergillus, an ubiquitous fungus, poses a major health threat to an increasing number of cancer patients and transplant recipients, causing an IPA characterized by invasion and destruction of pulmonary tissue [5–11]. An intact host defense is important to prevent this infection, and individuals with impaired immunity are susceptible [65–68], showing a high incidence of IPA and an associated mortality of up to 90% [69]. Patients with identical malignant diseases, clinical conditions, and treatments are known to differ in their susceptibility to IPA and in the severity of the disease, and the contribution of the host’s genetic background to IPA risk is attracting research interest. However, a large proportion of the genetic background of IPA remains unidentified, and only a few cytokine gene polymorphisms (IL10, TNFα, TNFR2, and IL6) have been studied [32, 33, 70].
In the present study, genes located in the IL1 cluster were selected as candidates for screening. IL1α and IL1β are major inducers of proinflammatory immune responses, and there is substantial evidence that local production of these cytokines is very important in host resistance to IPA. The immune response against Aspergillus conidia is mainly produced via Th1 and is mediated by a range of cytokines, including IL1, IL6, IL12, TNFα, and IFNγ [71–74]. These cytokines regulate not only their own levels of expression by autocrine pathways but also downstream cytokine expression, thereby amplifying the proinflammatory response. IL1 and TNF mediate the Th1 immune response after IPA infection. In fact, bronchoalveolar macrophages stimulated by Aspergillus conidia produce both IL1α and IL1β cytokines, promoting recruitment of neutrophils and monocytes into acutely injured lungs by induction of E- and P-selectin receptors on venule endothelial cells [71–73]. Secretion of IL1 also induces production of acute phase proteins such as CRP [75] and regulates proliferation and activation of T lymphocytes, which have a relevant role in clearance of Aspergillus spp. from the lungs [74].
The IL1 cluster genes are polymorphic. A biallelic (C/T) SNP has been identified in the 5′ regulatory region of the promoter at position -889 [48]. Recent transfection studies demonstrated that the -889TT construct had significantly higher expression than the -889CC construct [76]. Moreover, peripheral blood mononuclear cells of TT genotype carriers produced higher IL1α mRNA and protein levels than did cells of CC genotype carriers [76]. Likewise, the capacity of the host to mount an IL1β driven response is influenced by sequence variants in the IL1 cluster [45, 46, 77] Polymorphism in the IL1β and IL1Ra gene was also found to influence the encoded cytokines. Rare alleles of these polymorphisms (IL1β-511T and IL1Ra allele 2) correlated with higher IL1β secretion in vitro [45] and in vivo [77]. Importantly, these polymorphic variants in the IL1 gene cluster may affect not only the primary inflammatory response but also the post-amplification response. This was demonstrated by the association between variants of these genes or the receptor antagonist molecule and infectious disease susceptibility or resistance, observed in septic shock [34, 35], tuberculosis and malaria [39–41], periodontitis [42], and viral infections caused by cytomegalovirus [78], Epstein–Barr [79], and HIV [80], among others. Hence, IPA pathogenesis may also be affected by variations in these genes.
To our knowledge, this is the first report of a candidate gene-association approach to address a role for IL1 cluster genes in the pathogenesis of IPA, evaluating the role of IL1α-889(C/T) and IL1β511(C/T) promoter polymorphisms in IPA susceptibility. The association of IPA susceptibility with a VNTR in the second intron of IL1Ra gene was also investigated.
No significant differences in IL1α, IL1β, or IL1Ra genotype distributions or in allele carriage rates were observed between the hematological patients and healthy controls. Moreover, the distribution of IL1α-889(C/T), IL1β-511(C/T), and IL1Ra VNTR genotypes and the corresponding allelic frequencies in these controls were similar to reports in other Caucasian populations [50, 61–64]. Interestingly, no differences were observed between IPA and non-IPA patients in the distribution of the underlying disease. Therefore, in this population of hematological patients, IL1 gene cluster polymorphisms were not associated with susceptibility to a specific hematological malignancy.
Analysis of individual loci failed to show any significant effect of IL1 gene polymorphisms on IPA susceptibility. No evidence was found of a single-marker association between IL1α, IL1β, or IL1Ra polymorphisms and risk of IPA. No significant differences in genotype or allele frequencies for IL1 cluster polymorphisms were found between the IPA and non-IPA cohorts. Nonetheless, using a recessive analysis model, a trend towards a higher presence of IL1β-511T allele in the IPA group than in the non-IPA patient group (p = 0.092) was found. Because individual IL1 cluster polymorphic loci seems not to be clearly associated with IPA, a haplotype analysis was performed with an EM algorithm to assess whether the combined effects of the IL1Ra, IL1α, and IL1β genotypes also influenced IPA susceptibility. The EM algorithm allows determination of haplotype frequencies and maximizes the probability of obtaining the observed genotypes. Haplotype analysis is considered useful to identify both rare and common disease genes and has frequently been proven more powerful than analysis of a single polymorphism [81, 82]. The present haplotype analysis revealed a significant association between VNTR2/-889C/-511T haplotype and IPA infection. Surprisingly, haplotype analysis also showed a significant association between VNTR2/-889C/-511C haplotype and resistance to IPA. The p value for the global haplotype association was 0.026, showing a significant global association of IL1 cluster genes with IPA susceptibility.
Taken together, these associations with IL1 gene cluster polymorphisms provide further evidence of a role for the IL1 gene cluster in IPA susceptibility, although the precise mechanisms by which these gene haplotypes influence disease susceptibility remain unclear. We cannot rule out the possibility that these haplotypes may be in linkage disequilibrium with unidentified susceptibility genes/polymorphisms that are responsible for the significant associations observed. These results confirm the importance of including a haplotype-based analysis, as others have recommended [83, 84], for adequate assessment of multilocus genetic association [84, 85] .
ELISA analysis of IL1α and IL1β showed that their levels were similar between IPA and non-IPA patients and did not significantly correlate with IL1α-889(C/T) or IL1β-511(C/T) genotypes or clinical symptoms. There may be several possible reasons for this absence of correlations. First, IL1α remains primarily cell-associated and is found mainly in cytosol and plasma membranes of cells; therefore, its plasma levels are not usually detectable. Second, dexamethasone, used in the general treatment of many of our hematological patients, is known to suppress IL1 production [86]. Third, a single point measurement is probably inadequate to assess changes that might be associated with underlying genetic variations. For these reasons, our study only analyzed polymorphisms that genetically determine both IL1α and IL1β expression [72].
There have been several reports on the relationships between IL1 gene cluster polymorphisms and CRP [87]. In this study, we observed statistical association between higher CRP levels and IL1α-889CC, IL1β-511TT, and IL1Ra2/2 genotypes, reflecting the importance of these IL1 gene cluster variants in CRP production. However, CRP values were similar between IPA and non-IPA patients. In agreement with others [88], our results suggest that measurement of CRP may not be considered to be useful to diagnosis and follow-up of fungal infection.
Another interesting finding of this study was the significantly greater positive GM percentage in patients with high-secretory phenotype (TT genotype) of IL1β-511 SNP than in those with low-secretory phenotype (CC genotype). Likewise, a significantly greater positive GM percentage was observed in patients with high-secretory phenotype (2/2 genotype) of IL1Ra SNP than in those with low-secretory phenotype (1/1 genotype). These data support the hypothesis that the IL1 gene cluster may determine susceptibility to IPA infection and suggest a protective effect of IL1β-511C/C and C/T genotypes and IL1Ra 1/1 and 1/2 genotypes against IPA (expression of positive GM).
Conclusions
This is the first study to describe an association between IL1 cluster polymorphisms and haplotypes and IPA infection. The most important finding was that the risk of developing IPA is influenced by inter-individual variation in inflammatory response, through a combination of the effects of IL1Ra, IL1α, and IL1β genotypes. Confirmation of these results in a multicenter study would rule out the possibility of any center effect on our findings. Likewise, studies of larger numbers of patients from different populations are warranted to assess whether IL1 cluster gene polymorphisms and related haplotypes could serve as susceptibility or resistance markers for IPA infection. IL1 cluster gene polymorphisms analysis may become a useful tool to identify high-risk hematological patients.
References
Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest 2002;121:1988–199.
Denning DW. Invasive aspergillosis. Clin Infect Dis. 1998;26:781–803.
Denning DW, Anderson MJ, Turner G, Latge JP, Bennett JW. Sequencing the Aspergillus fumigatus genome. Lancet Infect Dis. 2002;2:251–3.
Gerson SL, Talbot GH, Hurwitz S, Strom BL, Lusk EJ, Cassileth PA. Prolonged granulocytopenia: the major risk factor for invasive pulmonary aspergillosis in patients with acute leukemia. Ann Intern Med. 1984;100:345–51.
Jantunen E, Anttila VJ, Ruutu T. Aspergillus infections in allogeneic stem cell transplant recipients: have we made any progress? Bone Marrow Transplant. 2002;30:925–9.
Baddley JW, Stroud TP, Salzman D, Pappas PG. Invasive mold infections in allogeneic bone marrow transplant recipients. Clin Infect Dis. 2001;32:1319–24.
Latge JP. Aspergillus fumigatus and aspergillosis. Clin Microbiol Rev. 1999;12:310–50.
Wingard JR. Fungal infections after bone marrow transplant. Biol Blood Marrow Transplant. 1999;5:55.
Saugier-Veber P, Devergie A, Sulahian A, Ribaud P, Traore F, Bourdeau-Esperou H, et al. Epidemiology and diagnosis of invasive pulmonary aspergillosis in bone marrow transplant patients: results of a 5 year retrospective study. Bone Marrow Transplant. 1993;12:121.
Clark TA, Hajjeh RA. Recent trends in the epidemiology of invasive mycoses. Curr Opin Infect Dis. 2002;15:569.
Weinberger M, Elattar I, Marshall D, Steinberg SM, Redner RL, Young NS, et al. Patterns of infection in patients with aplastic anemia and the emergence of Aspergillus as a major cause of death. Medicine 1992;71:24–43.
Marr KA, Carter RA, Boeckh M, Martin P, Corey L. Invasive aspergillosis in allogeneic stem cell transplant recipients: changes in epidemiology and risk factors. Blood 2002;100:4358–66.
Grow WB, Moreb JS, Roque D, Manion K, Leather H, Reddy V, et al. Late onset of invasive Aspergillus infection in bone marrow transplant patients at a university hospital. Bone Marrow Transplant. 2002;29:15–9.
Herbrecht R, Denning DW, Patterson TF, Patterson TF, Bennett JE, Greene RE, et al. Invasive fungal infections group of the European organisation for research and treatment of cancer and the global Aspergillus study group: voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–15.
Schaffner A, Douglas H, Braude A. Selective protection against conidia by mononuclear and against mycelia by polymorphonuclear phagocytes in resistance to Aspergillus. J Clin Invest. 1982;69:617–31.
Wang JE, Warris A, Ellingsen EA, Jorgensen PF, Flo TH, Espevik T, et al. Involvement of CD14 and toll-like receptors in activation of human monocytes by Aspergillus fumigatus hyphae. Infect Immun. 2001;69:2402–6.
Mambula SS, Sau K, Henneke P, Golenbock DT, Levitz SM. Toll-like receptor (TLR) signaling in response to Aspergillus fumigatus. J Biol Chem. 2002;277:39320–6.
Huffnagle GB, Deepe GS. Innate and adaptive determinants of host susceptibility to medically important fungi. Curr Opin Microbiol 2003;6:344–50.
Syme RM, Spurrell JC, Amankwah EK, Green FH, Mody CH. Primary dendritic cells phagocytose Cryptococcus neoformans via mannose receptors and Fcgamma receptor II for presentation to T lymphocytes. Infect Immun. 2002;70:5972–81.
Bozza S, Gaziano R, Spreca A, Bacci A, Montagnoli C, di Francesco P, et al. Dendritic cells transport conidia and hyphae of Aspergillus fumigatus from the airways to the draining lymph nodes and initiate disparate Th responses to the fungus. J Immunol. 2002;168:1362–71.
Steinkasserer A, Spurr NK, Cox S, Jeggo P, Sim RB. The human IL-1 receptor antagonist gene (IL1RN) maps to chromosome 2q14-q21, in the region of the IL-1a and IL-1b loci. Genomics 1992;13:654–7.
Dinarello CA. The interleukin-1 family: 10 years of discovery. FASEB J. 1994;8:1314–25.
Dinarello CA. Biologic basis for interleukin-1 in disease. Blood 1996;87:2095–147.
Sims JE, March CJ, Cosman D, Widmer MB, MacDonald HR, McMahan CJ, et al. cDNA expression cloning of the IL-1 receptor, a member of the immunoglobulin superfamily. Science 1988;241:585–9.
Gauldie J, Sauder DN, Adam MC, Dinarello CA. Purified interleukin-1 (IL-1) from human monocytes stimulates acute-phase protein synthesis by rodent hepatocytes in vitro. Immunology 1987;60:203–7.
Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34:909–17.
Cox A, Camp NJ, Cannings C, di Giovine FS, Dale M, Worthington J, et al. Combined sib-TDT and TDT provide evidence for linkage of the interleukin-1 gene cluster to erosive rheumatoid arthritis. Hum Mol Genet. 1999;8:1707–13.
Jouvenne P, Chaudhary A, Buchs N, Giovine FS, Duff GW, Miossec P. Possible genetic association between interleukin-1 alpha gene polymorphism and the severity of chronic polyarthritis. Eur Cytokine Netw. 1999;10:33–6.
Francis SE, Camp NJ, Dewberry RM, Gunn J, Syrris P, Carter ND, et al. Interleukin-1 receptor antagonist gene polymorphism and coronary artery disease. Circulation 1999;99:861–6.
Nemetz A, Nosti-Escanilla MP, Molnár T, Köpe A, Kovács A, Fehér J, et al. IL1B gene polymorphisms influence the course and severity of inflammatory bowel disease. Immunogenetics 1999;49:527–31.
Brouard J, Knauer N, Boelle PY, Corvol H, Henrion-Caude A, Flamant C, et al. Influence of interleukin-10 on Aspergillus fumigatus infection in patients with cystic fibrosis. J Infect Dis. 2005;191:1988–91.
Sainz J, Hassan L, Perez E, Romero A, Moratalla A, Lopez-Fernandez E, et al. Interleukin-10 promoter polymorphism as risk factor to develop invasive pulmonary aspergillosis. Immunol Lett. 2007;109:76–82.
Sainz J, Perez E, Hassan L, Moratalla A, Romero A, Collado MD, et al. Variable number of tandem repeats of TNF receptor type 2 promoter as genetic biomarker of susceptibility to develop invasive pulmonary aspergillosis. Hum Immunol. 2007;68:41–50.
Fang XM, Schroder S, Hoeft A, Stuber F. Comparison of two polymorphisms of the interleukin-1 gene family: interleukin-1 receptor antagonist polymorphism contributes to susceptibility to severe sepsis. Crit Care Med. 1999;27:1330–4.
Ma P, Chen D, Pan J, Du B. Genomic polymorphism within interleukin-1 family cytokines influences the outcome of septic patients. Crit Care Med. 2002;30:1046–50.
Arnalich F, Lopez-Maderuelo D, Codoceo R, Lopez J, Solis-Garrido LM, Capiscol C, et al. Interleukin-1 receptor antagonist gene polymorphism and mortality in patients with severe sepsis. Clin Exp Immunol. 2002;127:331–6.
Tsai FJ, Hsieh YY, Chang CC, Lin CC, Tsai CH. Polymorphisms for interleukin 1 beta exon 5 and interleukin 1 receptor antagonist in Taiwanese children with febrile convulsions. Arch Pediatr Adolesc Med. 2002;156:545–8.
Virta M, Hurme M, Helminen M. Increased frequency of interleukin-1beta (-511) allele 2 in febrile seizures. Pediatr Neurol. 2002;26:192–5.
Bellamy R, Ruwende C, Corrah T, McAdam KP, Whittle HC, Hill AV. Assessment of the interleukin 1 gene cluster and other candidate gene polymorphisms in host susceptibility to tuberculosis. Tuberc Lung Dis. 1998;79:83–9.
Wilkinson RJ, Patel P, Llewelyn M, Hirsch CS, Pasvol G, Snounou G, et al. Influence of polymorphism in the genes for the interleukin-1 receptor antagonist and IL-1b on tuberculosis. J Exp Med. 1999;189:1863–73.
Walley AJ, Aucan C, Kwiatkowski D, Hill AV. Interleukin-1 gene cluster polymorphisms and susceptibility to clinical malaria in a Gambian case-control study. Eur J Hum Genet. 2004;12:132–8.
McDevitt MJ, Wang HY, Knobelman C, Newman MG, di Giovine FS, Timms J, et al. Interleukin-1 genetic association with periodontitis in clinical practice. J Periodontol. 2000;71:156–63.
Endres S, Cannon JG, Ghorbani R, Dempsey RA, Sisson SD, Lonnemann G, et al. In vitro production of IL-1 beta, IL-1 alpha, TNF and IL-2 in healthy subjects: distribution, effect of cyclooxygenase inhibition and evidence of independent gene regulation. Eur J Immunol. 1989;19:2327–33.
Hall SK, Perregaux DG, Gabel CA. Correlation of polymorphic variation in the promoter region of the interleukin-1β gene with secretion of interleukin-1b protein. Arthritis Rheum. 2004;50:1976–83.
Pociot F, Molvig J, Wogensen L, Worsaae H, Nerup J. A TaqI polymorphism in the human interleukin-1 beta (IL-1 beta) gene correlates with IL-1 beta secretion in vitro. Eur J Clin Invest. 1992;22:396–402.
Hwang IR, Kodama T, Kikuchi S, Sakai K, Peterson LE, Gram DY, et al. Effect of interleukin 1 polymorphisms on gastric mucosal interleukin 1beta production in Helicobacter pylori infection. Gastroenterology 2002;123:1793–803.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, et al. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and haematopoietic stem cell transplants: an international consensus. Clin Infect Dis. 2002;34:7–14.
McDowell TL, Symons JA, Ploski R, Forre O, Duff GW. A genetic association between juvenile rheumatoid arthritis and a novel interleukin-1 alpha polymorphism. Arthritis Rheum. 1995;38:221–8.
Di Giovine FS, Takhsh E, Blakemore AI, Duff GW. Single base polymorphism at -511 in the human interleukin-1 beta gene (IL1 beta). Hum Mol Genet. 1992;1:450.
Craggs A, West S, Curtis A, Welfare M, Hudson M, Donaldson P, et al. Absence of a genetic association between IL-1RN and IL-1B gene polymorphisms in ulcerative colitis and Crohn disease in multiple populations from northeast England. Scand J Gastroenterol. 2001;36:1173–8.
Latge JP, Kobayashi H, Debeaupuis JP, Diaquin M, Sarfati J, Wieruszeski JM, et al. Chemical and immunological characterization of the extracellular galactomannan of Aspergillus fumigatus. Infect Immun. 1994;62:5424–33.
Marr KA, Balajee SA, McLaughlin L, Tabouret M, Bentsen C, Walsh TJ. Detection of galactomannan antigenemia by enzyme immunoassay for the diagnosis of invasive aspergillosis: variables that affect performance. J Infect Dis. 2004;190:641–9.
Becker MJ, Lugtenburg EJ, Cornelissen JJ, Van Der Schee C, Hoogsteden HC, De Marie S. Galactomannan detection in computerized tomography-based broncho-alveolar lavage fluid and serum in hematological patients at risk for invasive pulmonary aspergillosis. Br J Haematol. 2003;121:448–57.
Herbrecht R, Letscher-Bru V, Oprea C, Lioure B, Waller J, Campos F, et al. Aspergillus galactomannan detection in the diagnosis of invasive aspergillosis in cancer patients. J Clin Oncol. 2002;20:1898–906.
Maertens J, Verhaegen J, Demuynck H, Brock P, Verhoef G, Vanderberghe P, et al. Autopsy-controlled prospective evaluation of serial screening for circulating galactomannan by a sandwich enzyme-linked immunosorbent assay for hematological patients at risk for invasive aspergillosis. J Clin Microbiol. 1999;37:3223–8.
Maertens J, Van Eldere J, Verhaegen J, Verbeken J, Verschakelen J, Boogaerts M. Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis. 2002;186:1297–306.
Maertens J, Theunissen K, Verbeken E, Lagrou K, Verhaegen J, Boogaerts M, et al. Prospective clinical evaluation of lower cut-offs for galactomannan detection in adult neutropenic cancer patients and hematological stem cell transplant recipients. Br J Haematol. 2004;126:852–60.
Sole X, Guino E, Valls J, Iniesta R, Moreno V. SNPStats: a web tool for the analysis of association studies. Bioinformatics 2006;22:1928–9.
Tishkoff SA, Pakstis AJ, Ruano G, Kidd KK. The accuracy of statistical methods for estimation of haplotype frequencies: an example from the CD4 locus. Am J Hum Genet. 2000;67:518–22.
Fallin D, Cohen A, Essioux L, Chumakov I, Blumenfeld M, Cohen D, et al. Genetic analysis of case/control data using estimated haplotype frequencies: application to APOE locus variation and Alzheimer’s disease. Genome Res. 2001;11:143–51.
Mansfield JC, Holden H, Tarlow JK, Di Giovine FS, McDowell TL, Wilson AG, et al. Novel genetic association between ulcerative colitis and the anti-inflammatory cytokine interlukin-1 receptor antagonist. Gastroenterology 1994;106:637–42.
Hefler LA, Grimm C, Lantzsch T, Lampe D, Leodolter S, Koelbl S, et al. Interleukin-1 and interleukin-6 gene polymorphisms and the risk of breast cancer in Caucasian women. Clin Cancer Res. 2005;11:5718–21.
Parks CG, Cooper GS, Dooley MA, Treadwell EL, St Clair EW, Gilkeson GS, et al. Systemic lupus erythematosus and genetic variation in the interleukin 1gene cluster: a population based study in the southeastern United States. Ann Rheum Dis. 2004;63:91–4.
Lin RC, Morris BJ. Association analysis of polymorphisms at the interleukin-1locus in essential hypertension. Am J Med Genet. 2002;107:311–16.
Schaffner A, Douglas H, Braude A. Selective protection against conidia by mononuclear and against mycelia by polymorphonuclear phagocytes in resistance to Aspergillus: observations on these two lines of defense in vivo and in vitro with human and mouse phagocytes. J Clin Invest. 1982;69:617–31.
Waldorf AR, Levitz S, Diamond RD. In vivo bronchoalveolar macrophage defense against Rhizopus oryzae and Aspergillus fumigatus. J Infect Dis. 1984;150:752–60.
Cenci E, Mencacci A, Fe d, ’ C, Del Sero G, Mosci P, Montagnoli C, et al. Cytokine- and T helper-dependent lung mucosal immunity in mice with invasive pulmonary aspergillosis. J Infect Dis. 1998;178:1750–60.
Romani L. The T cell response against fungal infections. Curr Opin Immunol. 1997;9:484–90.
Paterson DL, Singh N. Invasive aspergillosis in transplant recipients. Medicine 1999;78:123.
Sainz J, Pérez E, Gómez-Lopera S, López-Fernández E, Moratalla L, Oyonarte S, et al. Genetic variants of IL6 gene promoter influence on C-reactive protein levels but are not associated with susceptibility to Invasive pulmonary aspergillosis in hematological patients. Cytokine. 2008;41:268–278.
Gotsch U, Jager U, Dominis M, Vestweber D. Expression of P-selectin on endothelial cells is upregulated by LPS and TNF-alpha in vivo. Cell Adhesion Commun. 1994;2:7–14.
Haraldsen G, Kuale D, Lieu B, Farstad IN, Brandzaly P. Cytokine-regulated expression of E-selectin, intracellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1) in human intestinal microvascular endothelial cells. J Immunol. 1996;156:2558–65.
Kansas GS. Selectins and their ligands: current concepts and controversies. Blood 1996;88:3259–87.
Vecchiarelli A, Dottorini M, Pietrella D, Monari C, Retini C, Todisco T, et al. Role of human alveolar macrophages as antigen-presenting cells in Cryptococcus neoformans infection. Am J Resp Cell Mol Biol. 1994;11:130–7.
Gauldie J, Sauder DN, Adam MC, Dinarello CA. Purified interleukin-1 (IL-1) from human monocytes stimulates acute-phase protein synthesis by rodent hepatocytes in vitro. Immunology 1987;60:203–7.
Dominici R, Cattaneo M, Malferrari G, Archi D, Mariani C, Grimaldi LME, et al. Cloning and functional analysis of the allelic polymorphism in the transcription regulatory region on interleukin-1a. Immunogenetics 2002;54:82–6.
Hulkkonen J, Vilpo J, Vilpo L, Koski T, Hurme M. Interleukin-1 beta, interleukin 1 receptor antagonist and interleukin-6 plasma levels and cytokine gene polymorphisms in chronic lymphocytic leukaemia: correlation with prognostic parameters. Haematologica 2000;85:600–6.
Hurme M, Helminen M. Resistance to human cytomegalovirus infection may be influenced by genetic polymorphisms of the tumor necrosis factor-alpha and interleukin-1 receptor antagonist genes. Scand J Infect Dis. 1998;30:447–9.
Hurme M, Helminen M. Polymorphism of the IL-1 gene complex and Epstein-Barr virus seronegative and seropositive adult blood donors. Scand J Immunol. 1998;48:219–22.
Witkin SS, Linhares IM, Gerber S, Caetano ME, Segurado AC. Interleukin-1 receptor antagonist gene polymorphism and circulating levels of HIV-1 RNA in Brazilian women. J Virol. 2001;75:6242–4.
Rioux JD, Daly MJ, Silverberg MS, Lindblad K, Steinhart H, Cohen Z, et al. Genetic variation in the 5q31 cytokine gene cluster confers susceptibility to Crohn disease. Nat Genet. 2001;29:223–8.
Johnson GC, Esposito L, Barratt BJ, Smith AN, Heward J, Di Genova G, et al. Haplotype tagging for the identification of common disease genes. Nat Genet. 2001;29:233–7.
Schaid DJ, Rowland CM, Tines DE, Jacobson RM, Poland GA. Score tests for association between traits and haplotypes when linkage phase is ambiguous. Am J Hum Genet. 2002;70:425–44.
Schaid DJ. Relative efficiency of ambiguous vs. directly measured haplotype frequencies. Genet Epidemiol. 2002;23:426–43.
Johnson JA, Terra SG. Beta-adrenergic receptor polymorphisms: cardiovascular disease associations and pharmacogenetics. Pharm Res. 2002;19:1779–87.
Kamberi M, Brummer E, Stevens DA. Regulation of bronchoalveolar macrophage proinflammatory cytokine production by dexamethasone and granulocyte-macrophage colony-stimulating factor after stimulation by Aspergillus conidia and lipopolysaccharide. Cytokine 2002;19:14–20.
Berger P, McConnell JP, Nunn M, Kornman KS, Sorrell J, Stephenson K, et al. C-reactive protein levels are influenced by common IL-1 gene variations. Cytokine 2002;17:171–4.
Yonemori K, Kanda Y, Yamamoto R, Hamaki T, Suguro M, Chizuka A, et al. Clinical value of serial measurement of serum C-reactive protein level in neutropenic patients. Leuk Lymphoma. 2001;41:607–14.
Acknowledgments
We are indebted to the patients and healthy controls who participated in this study. The advice of Dr. Victor Moreno (Catalan Institute of Oncology) on the development of the genetic tests is acknowledged. The authors thank C. González Moreno (leukemia survivor) for her generous donation, Elena Lamas (laboratory technician) for sample collection and technical support, and staff of the Research Unit of Virgen de las Nieves University Hospital for providing the necessary facilities. This study was supported by a grant (259/04) from the Servicio Andaluz de Salud (SAS), a grant from Fundación anti-cancer San Francisco Javier y Santa Cándida, and a postdoctoral training grant from the Fundación para la Investigación Biosanitaria de Andalucía Oriental-Alejandro Otero (FIBAO).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sainz, J., Pérez, E., Gómez-Lopera, S. et al. IL1 Gene Cluster Polymorphisms and Its Haplotypes may Predict the Risk to Develop Invasive Pulmonary Aspergillosis and Modulate C-reactive Protein Level. J Clin Immunol 28, 473–485 (2008). https://doi.org/10.1007/s10875-008-9197-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-008-9197-0