Abstract
Severe congenital neutropenia (SCN) is a rareE primary immunodeficiency disorder characterized by early onset recurrent infections in association with persistent severe agranulocytosis. To identify the clinical, immunohematological, and molecular characteristics of patients with SCN, 18 Iranian patients with the mean age of 8.8 ± 5.8 years were investigated in this study. All of these patients experienced severe neutropenia; the mean of absolute neutrophil count was 281.4 ± 137.7 cells/mm3. Bone marrow findings were typified by a myeloid maturation arrest at the promyelocyte–myelocyte stage in these patients. Molecular analysis revealed different mutations in the ELA-2 gene of one patient and in the HAX-1 gene of another three patients. The most common presenting complaints in these patients were superficial abscesses, oral ulcers, cutaneous infections, omphalitis, and pneumonia. During the course of illness, all patients developed mucocutaneous manifestations, and 16 cases had respiratory infections. The most commonly manifestations were abscesses, oral ulcers, pneumonia, periodontitis, otitis media, cutaneous infections, mucocutaneous candidiasis, and acute diarrhea. Three patients died because of a severe infection. Although SCN is a rare disorder, early onset of severe and recurrent infections should always raise a suspicion, which deserves further evaluation for detecting such disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
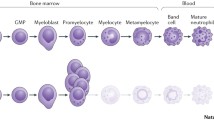
Severe congenital neutropenia [SCN; Online Mendelian Inheritance in Man (OMIM) #202700] is a rare inherited immunodeficiency disorder, characterized by persistent severe neutropenia and early onset severe systemic bacterial infections [1–4]. It was first described by Rolf Kostmann [5, 6] in 1956 in intermarried Swedish family with severe bacterial infections and severe neutropenia, which was characterized by a maturation block in the myelopoiesis at the promyelocytic/myelocytic stage. Although the first report indicated an autosomal recessive mode of inheritance in these patients, SCN is genetically heterogeneous, and autosomal dominant and sporadic forms of the disease were recognized later [1, 4, 7–9]. Several studies indicated mutations of the gene encoding neutrophil elastase (ELA2) as the underlying genetic defect in a number of cases with autosomal dominant and sporadic form of SCN [1, 10, 11]. Recent molecular studies to identify the genetic defects of autosomal recessive form of SCN revealed HAX1 mutations in these patients [12].
The SCN patients typically have persistent severe neutropenia of less than 0.5 × 109/l, increased susceptibility to recurrent severe bacterial infections from early infancy, and early-stage (promyelocyte-myelocyte) maturation arrest of myeloid differentiation in the bone marrow [1–4, 8].
In the absence of appropriate treatment, affected children suffer from early life threatening infections [2, 13, 14]. In addition, most patients die because of these infections despite antibiotic treatment [1]. Administration of recombinant human granulocyte colony-stimulating factor (G-CSF) could normalize neutrophil numbers in these patients to improve the prognosis and their quality of life [13–15].
The present study reports the clinical and laboratory findings of Iranian patients with SCN.
Materials and Methods
To determine the clinical and laboratory findings of Iranian patients with SCN, the records of 18 patients, who had been referred to the referral immunology and hematology departments in Iran, were reviewed (Table I). These data have already been gathered by interviewing the patients and reviewing their medical documents during a 20-year period (1986–2006).
Neutropenia is defined as a significant reduction in the absolute neutrophil count (ANC) of circulating neutrophils in the blood, which is calculated by multiplying the total of blood cell count by the percentage of neutrophils plus bands noted in the differential cell count. The definition of severe neutropenia was defined as less than 500/mm3. The diagnosis of SCN is made by severe chronic neutropenia with ANC continuously below 500/mm3 and maturation arrest of neutrophil precursors at the promyelocyte–myelocyte level. Although all of our patients fulfilled such criteria and had continuously ANC of less than 500/mm3, the patients’ ANC at the time of diagnosis is shown in Table II, when G-CSF therapy was not started for the patients and in a time they have not any active infection. The reference values of our hematological laboratory were used to put cut-off values for other hematological abnormalities (Table II). Serum immunoglobulin levels (IgG, IgM, and IgA) were measured by nephelometry, and the results were compared with reference values for age of our immunological laboratory (Table III).
After taking informed consent, 5 ml blood was taken from eight patients for extraction of DNA and molecular analysis. DNA was isolated from whole blood collected with ethylene diaminetetraacetic acid (EDTA) as anticoagulant, using a “Salting out” method. Subsequently, ELA2 (GeneID, 1991; protein accession, NP_001963.1; cDNA accession, NM_001972.2), HAX1 (GeneID, 10456; protein accession, NP_006109.2; cDNA accession, NM_006118.3) genes and the gene encoding the granulocyte colony-stimulating factor (G-CSF)-receptor (CSFR3) (GeneID: 1441; protein accession: NP_000751.1; cDNA accession: NM_000760.2) were sequenced in these patients.
To determine the frequency and duration of infections, review of the clinical history was performed. Data analysis was performed using SPSS statistical software package, version 11.0 (SPSS, Chicago, IL).
Results
Characteristics of Patients
Eighteen SCN patients (10 male and 8 female) with the mean age of 8.8 ± 5.8 years were reviewed in this study. The first manifestation had occurred at a median age of 4 (range, 1–20) months. Fifteen cases experienced symptoms by the age of 6 months, whereas only one patient did not experience any symptoms until the age of 1 year (Table I). The median age of patients at the time of diagnosis was 21 months (range, 5 months–10 years), with a median diagnosis delay of 15.5 months (range, 3 months–9.5 years). Although half of the patients were diagnosed until the age of 1.5 years, the diagnosis of two patients were made after the age of 5 years (Table I). Statistical analysis of these data was complicated by the fact that the diagnosis has increasingly been made at an earlier age in more recent years (r = −0.611, F = 9.554, P value = 0.007). A reverse association was observed between years of birth and delay of diagnosis (Fig. 1).
Consanguinity and Family History
Consanguineous marriage is defined as two partners have at least one ancestor in common, with the ancestor being no more distant than a great great grandparent. For descendants who are of the same generation, a consanguineous marriage would be between one person and a third cousin or a closer relative. In ten families, parents were consanguine (55.6%) (Table I; Fig. 2). A history of recurrent infections in siblings of the affected patients was found in four families.
The pedigrees of three patients with severe congenital neutropenia. Open shapes represent healthy individuals, filled shapes represent affected patients with syndrome, hatched shapes represent patients with recurrent infections without any specific diagnosis, and shapes with slashes represent deceased individuals. Boxes Males, circles females).
Presenting Features
The most common presenting feature of these SCN patients was skin abscesses, which was seen in five patients. The other presenting manifestations were oral ulcers (four patients), cutaneous infections (three patients), omphalitis (two patients), and pneumonia (two patients). Moreover, one patient presented with otitis media and another one with urinary tract infection.
Clinical Manifestations
During the course of disease, all patients developed mucocutaneous manifestations, and 16 cases had respiratory infections. The most commonly manifestations were abscesses (16 cases), oral ulcers (13 cases), pneumonia (11 cases), periodontitis (9 cases), otitis media (9 cases), cutaneous infections (7 cases), mucocutaneous candidiasis (5 cases), acute diarrhea (5 cases), urinary tract infection (3 cases), and acute sinusitis (2 cases). Moreover, five patients had also failure to thrive. In two patients, the course of the disease was complicated by bronchiectasis because of recurrent pneumonia. Abscesses have been detected as the most frequent manifestations of patients, affecting different organs, including cutaneous (ten cases), mastoidal (five cases), perianal (three cases), sacral (three cases), dental (two cases), submandibular (one case), and hepatic (one case). Nonspecific findings as hepatomegaly and splenomegaly were seen in four and six cases, respectively. In one third of the patients (six cases), lymphadenopathy has been recorded in the course of the disease.
Hematological Studies
All of these patients had severe chronic neutropenia during their disease. Laboratory analyses revealed low ANC, with the mean count of 281.4 ± 137.7 cells/mm3 (range, 72–490/mm3). Total white blood cell (WBC) counts ranged from normal to markedly elevated numbers in patients with acute infections. The median count of WBC at non-infections visits of the patients was 4,700/mm3 (range, 1,750–7,750/mm3). Six patients had thrombocytosis, five had anemia, and five had leukopenia; moreover, two patients had lymphocytosis, two had eosinophilia, and one had monocytosis (Table II).
Immunological Studies
Laboratory analysis revealed an increased IgG serum level, with median of 1,534.5 (range, 920–3,800) mg/dl. The median serum levels for IgM and IgA was 126 (68–491) mg/dl and 85 mg/dl (30–730 mg/dl), respectively. In comparison of immunoglobulin levels of these patients with normal age-matched population, 11 patients had higher serum level of IgG (61.1%), whereas 6 patients had higher serum level of IgM and 5 had higher serum level of IgA as well (Table III).
Bone Marrow Studies
Bone marrow studies indicated a maturation arrest of neutrophil precursors at an early stage; these findings were typified by a myeloid maturation arrest at the promyelocyte–myelocyte stage in all of these patients. There was slightly increased number of promyelocytes, with atypical nuclei and vacuolization of the cytoplasm, and a marked absence of mature granulocyte forms in these patients (Fig. 3). Cellularity was normal, except in P6 and P16, in which it slightly decreased. Megakaryocytes were normal in number and morphology.
Molecular Studies
Molecular analysis was conducted in eight patients (Table III). ELA2 was sequenced in all these patients. Only one patient had mutations in this gene (P8). He had two heterozygous single base changes in exon 3, leading to amino acid substitutions (V69L and V72L). HAX-1 was also sequenced in these patients; two unrelated patients had homozygous single nucleotide insertion, leading to a premature stop codon (W44X; P11 and P12), and one patient had a homozygous single base pair substitution, leading to a nonsense mutation R86X (P9). CSF3R is also sequenced in these patients; no somatic mutations in CSF3R were identified in these patients.
Mortality
The patients were followed through a period of 5.5 ± 3.9 years (a total of 99 patient years). Twelve out of these patients are alive, three patients could not be localized, and the remaining three patients have already died, all because of septicemia (P6 in 2000 and P13 in 2002 and P17 in 1999). All patients are prescribed to G-CSF therapy after diagnosis; however, none of the patients received regular G-CSF therapy, and all received this treatment irregularly. We started G-CSF therapy with an initial dose of 6 μg/kg bid, but this dose adjusts individually on the basis of clinical manifestations and ANC, and it was increased even more than 100 μg kg−1 daily−1 in acute infections setting. The survival curve is shown in Fig. 4. Postdiagnosis survival was estimated as 90% for the first 2 years, which remains the same until 11 years after diagnosis when a drop of nearly 30% in survival is seen. None of our patients developed myelodysplastic syndromes or acute leukemia.
Discussion
SCN is a rare disorder with an estimated frequency of 1–2 cases per 106 population in general [1] and cumulative incidence of 0.27 per 106 population in Iran during the last 10 years [16]. We reported in this paper the clinical, immuno-hematological, and molecular investigations in all diagnosed SCN patients in Iran.
The distribution of gender was approximately equal, as expected according to the patterns of inheritance [1, 4, 7–9]. Almost all patients experienced the first manifestation of disease during the first 6 months of their life and also experienced recurrent severe bacterial infections during the infancy, which is a hallmark of SCN [1–4]. Early onset recurrent infections are one of the characteristics of SCN patients (median of 4 months in our SCN patients), whereas it is similar to other primary immunodeficiency diseases (median of 7 months in Iranian patients) as well [16]. Superficial abscesses, omphalitis, pneumonia, and otitis media are the most common manifestations leading to the diagnosis of SCN [1]. Although the diagnosis was made approximately 1 year after the first symptom, this diagnosis lag was much lower than the delay in other primary immunodeficiency disorders [16], as SCN can easily be diagnosed by chronic severe neutropenia in repeated complete blood cell count; it should be noted that in all cases, neutropenia had been detected much earlier, but this finding did not lead to SCN diagnosis at that time. The diagnosis delay has been significantly decreased in the recent years. It is caused by increasing the awareness of medical staff by educational programs in the country [16, 17]. However, it should be emphasized that only the patients who survived long enough to be diagnosed and referred to the referral centers in Iran were investigated in this study. In fact, this number of patients does not necessarily reflect the actual prevalence of SCN in the country in this period, as there are a number of undiagnosed patients who will die before the diagnosis was made.
The consanguinity rate in our SCN patients was 55%, which was much higher than the rate in general population and much lower than the overall rate in all Iranian primary immunodeficient patients [18]. Although an autosomal recessive mode of inheritance is expected in the patients from consanguineous families, it is not true for all patients because consanguineous marriages in the patients with X-linked inheritance are as high as in normal population [18], and there is also a SCN patient from non-consanguineous family (P11) with homozygous single nucleotide insertion (autosomal recessive form).
An increased susceptibility to infections was detected in our SCN patients. Mucocutaneous manifestations and respiratory infections were the most common feature of these patients during the course of disease. The predominant manifestation of our patients was recurrent bacterial infections. Common initial bacterial infections include skin abscesses, pneumonia, periodontitis, and otitis media [1]. Although recurrent infections are the most important characteristics of other primary immunodeficiency diseases as well, respiratory and gastrointestinal manifestations were the most common problems in these patients [16]. Pneumonia, diarrhea, otitis media, and sinusitis are the frequent manifestations in primary immunodeficiency diseases, whereas abscesses and oral ulcers were more common in our SCN patients. The presence of abscesses, ulcers, and gingivitis implies clinically significant neutropenia. Gingival hyperplasia and aphthous stomatitis in these patients lead to loss of permanent teeth in childhood [1]. In one third of our SCN patients, splenomegaly was recorded in the course of the disease, which is in agreement with other studies; the overall incidence of splenomegaly is estimated 21% before treatment with G-CSF and 34–48% through 10 years of treatment [1].
All of our SCN patients had severe neutropenia of less than 500 cells/mm3 during their disease. As it was seen in our study, other hematological abnormalities usually occur in association with neutropenia [1, 2]. Although mild anemia and thrombocytosis were seen in one third of our patients, increase in the blood monocytes and eosinophils was rare. Bone marrow studies indicated an early-stage maturation arrest of myeloid differentiation. Although bone marrow pictures could confirm the diagnosis of SCN, clinical features of disease and peripheral blood smear are still the most important parts of the diagnostic evaluation [2].
Increased immunoglobulin serum levels, especially IgG, were seen in our SCN patients. Elevated serum level of immunoglobulin is a common finding in SCN patients and maybe caused by a possible gene defect in both, myelopoiesis and lymphopoiesis or secondary to recurrent infections. However, it is proposed that increased IgG level in SCN patients is not related to their infectious status [1]. All of our HAX1 patients had elevated IgG level; two had elevated IgM and IgA levels as well. Igs serum levels were much higher than other patients without HAX1 mutations. Although B-cell abnormalities have not previously been reported in SCN patients, HAX1 participates in B-cell receptor-mediated signal transduction [19]. Further studies on higher number of SCN patients should be performed to compare clinical and laboratory data between groups. As increased immunoglobulin serum levels are not expected in other primary immunodeficiency diseases, high immunoglobulin serum levels should rise suspicious to SCN in neutropenic patients with recurrent infections.
Although the underlying genetic defect of SCN is not completely understood [1], molecular analysis of our SCN patients indicated different mutations in the ELA2 gene of one patient and in the HAX1 gene of another three patients. Mutations of ELA2 are the underlying genetic defect in 60–80% of autosomal dominant and sporadic cases of SCN [1, 10]. Mutations of HAX1 have recently been introduced as the underlying genetic defect of an autosomal recessive form of SCN [12]. Neutrophil elastase protein has a role in synthesizing the promyelocytes [20] and HAX1 is proposed to have a role in controlling the apoptosis [21]; therefore, increased apoptosis in myeloid progenitor cells could be a mechanism of neutropenia in SCN patients [20, 22]. As there are also some patients without any mutations in above-mentioned genes, it seems that there are still some additional genes in controlling the survival of neutrophils, which should be further investigated by future genetic studies in these patients. Although approximately one fifth of SCN patients are complicated with leukemia during their disease [23], none of our patients have developed myelodysplastic syndromes or acute leukemia until now. This condition has a high correlation with occurrence of CSF3R mutations [24], which were not found in our patients. However, it has not been checked in all patients. Further follow-up studies for CSF3R mutations are also required to estimate the risk of myelodysplasia and leukemia in these patients. Although molecular analysis of SCN patients is useful as a predictor for response to treatment and outcome in SCN patients, the diagnosis rests primarily on the clinical picture of the disorders and cell blood count with manual WBC differentiation [2].
Although it seems that postdiagnosis survival was 90% for the first 2 years in our study, it should be emphasized that the postdiagnosis survival should be much lower that this, as we just select the cases who survived long enough to refer to a medical center; therefore, there would be several undiagnosed patients who died in the first 2 years of life and before the diagnosis was made. It should also be considered that the remaining 90% survival until 11 years after diagnosis is because of receiving G-CSF therapy in the period after diagnosis, which is effective for reducing the risk of sepsis. Recombinant human G-CSF is the first choice of treatment for SCN patients that could increase the number of neutrophils, reduce the number of infections and hospitalization, and improve the prognosis and their quality of life [1, 3, 13–15]. Three of our patients who did not receive regular use of G-CSF died because of sepsis. Unfortunately, other patients do not receive regular use of G-CSF as well because of imbalance between the cost of drug and their socioeconomic conditions; they are at the risk of life-threatening infections now [2, 13, 14].
Conclusion
Severe and recurrent infections must always initiate the search for an immunodeficiency syndrome because a delay in diagnosis may result in chronic infection, irretrievable end-organ damage, or even death of the patient. Presence of neutropenia in association with increased immunoglobulin serum levels should rise suspicious to SCN in patients with recurrent infections, especially in those with superficial abscesses and oral ulcers. Timely referral to a hematologist and/or clinical immunologist remains the key to the successful diagnosis and management of patients with SCN.
References
Welte K, Zeidler C, Dale DC. Severe congenital neutropenia. Semin Hematol 2006;43:189–95.
Rezaei N, Farhoudi A, Ramyar A, Pourpak Z, Aghamohammadi A, Mohammadpour B, et al. Congenital neutropenia and primary immunodeficiency disorders: a survey of 26 Iranian patients. J Pediatr Hematol Oncol 2005;27:351–6.
Zeidler C, Welte K. Kostmann syndrome and severe congenital neutropenia. Semin Hematol 2002;39:82–8.
Zeidler C, Schwinzer B, Welte K. Congenital neutropenias. Rev Clin Exp Hematol 2003;7:72–83.
Kostmann R. Infantile genetic agranulocytosis: a new recessive lethal disease in man. Acta Paediatr Scand 1956;45:1–78.
Kostmann R. Infantile genetic agranulocytosis: a review with presentation of ten new cases. Acta Paediatr Scand 1975;64:362–8.
Berliner N, Horwitz M, Loughran TP Jr. Congenital and acquired neutropenia. Hematology 2004;63–79.
Ancliff PJ, Gale RE, Liesner R, Hann IM, Linch DC. Mutations in the ELA2 gene encoding neutrophil elastase are present in most patients with sporadic severe congenital neutropenia but only in some patients with the familial form of the disease. Blood 2001;98:2645–50.
Notarangelo L, Casanova JL, Conley ME, Chapel H, Fischer A, Puck J, et al. International Union of Immunological Societies Primary Immunodeficiency Diseases Classification Committee: Primary immunodeficiency diseases: an update from the International Union of Immunological Societies Primary Immunodeficiency Diseases Classification Committee Meeting in Budapest, 2005. J Allergy Clin Immunol 2006;117:883–96.
Dale DC, Person RE, Bolyard AA, Aprikyan AG, Bos C, Bonilla MA, et al. Mutations in the gene encoding neutrophil elastase in congenital and cyclic neutropenia. Blood 2000;96:2317–22.
Salipante S, Benson KF, Luty J, Hadavi V, Kariminejad R, Kariminejad MH, et al. Double de novo mutations of ELA2 in cyclic and severe congenital neutropenia. Hum Mutat 2007; DOI 10.1002/humu.20520.
Klein C, Grudzien M, Appaswamy G, Germeshausen M, Sandrock I, Schäffer AA, et al. HAX1 deficiency causes autosomal recessive severe congenital neutropenia (Kostmann disease). Nat Genet 2007;39:86–92.
Zeidler C, Boxer L, Dale DC, Freedman MH, Kinsey S, Welte K. Management of Kostmann syndrome in the G-CSF era. Br J Haematol 2000;109:490–5.
Carlsson G, Fasth A. Infantile genetic agranulocytosis, morbus Kostmann: presentation of six cases from the original “Kostmann family” and a review. Acta Paediatr 2001;90:757–64.
Bonilla MA, Gillio AP, Ruggeiro M, Kernan NA, Brochstein JA, Abboud M, et al. Effects of recombinant human granulocyte colony-stimulating factor on neutropenia in patients with congenital agranulocytosis. N Engl J Med 1989;320:1574–80.
Rezaei N, Aghamohammadi A, Moin M, Pourpak Z, Movahedi M, Gharagozlou M, et al. Frequency and clinical manifestations of patients with primary immunodeficiency disorders in Iran: update from the Iranian primary immunodeficiency registry. J Clin Immunol 2006;26:519–32.
Rezaei N, Farhoudi A, Pourpak Z, Aghamohammadi A, Moin M, Movahedi M, et al. Neutropenia in Iranian patients with primary immunodeficiency disorders. Haematologica 2005;90:554–6.
Rezaei N, Pourpak Z, Aghamohammadi A, Farhoudi A, Movahedi M, Gharagozlou M, et al. Consanguinity in primary immunodeficiency disorders; the report from Iranian primary immunodeficiency registry. Am J Reprod Immunol 2006;56:145–51.
Suzuki Y, Demoliere C, Kitamura D, Takeshita H, Deuschle U, Watanabe T. HAX-1, a novel intracellular protein, localized on mitochondria, directly associates with HS1, a substrate of Src family tyrosine kinases. J Immunol 1997;158:2736–44.
Aprikyan AA, Liles WC, Boxer LA, Dale DC. Mutant elastase in pathogenesis of cyclic and severe congenital neutropenia. J Pediatr Hematol Oncol 2002;24:784–6.
Cilenti L, Soundarapandian MM, Kyriazis GA, Stratico V, Singh S, Gupta S, et al. Regulation of HAX-1 anti-apoptotic protein by Omi/HtrA2 protease during cell death. J Biol Chem 2004;279:50295–301.
Carlsson G, Aprikyan AA, Tehranchi R, Dale DC, Porwit A, Hellstrom-Lindberg E, et al. Kostmann syndrome: severe congenital neutropenia associated with defective expression of Bcl-2, constitutive mitochondrial release of cytochrome c, and excessive apoptosis of myeloid progenitor cells. Blood 2004;103:3355–61.
Rosenberg PS, Alter BP, Bolyard AA, Bonilla MA, Boxer LA, Cham B, et al. Severe Chronic Neutropenia International Registry: the incidence of leukemia and mortality from sepsis in patients with severe congenital neutropenia receiving long-term G-CSF therapy. Blood 2006;107:4628–35.
Dong F, Brynes RK, Tidow N, Welte K, Lowenberg B, Touw IP. Mutations in the gene for the granulocyte colony-stimulating-factor receptor in patients with acute myeloid leukemia preceded by severe congenital neutropenia. N Engl J Med 1995;333:487–93.
Acknowledgments
This research has been supported by Immunology, Asthma and Allergy Research Institute, Tehran University of Medical Sciences and Health Services grant. The authors would like to thank all the patients and their families for their kind collaboration in this study. We would like to thank Dr. Bodo Grimbacher for his great collaboration in arrangement of molecular studies of the patients and critical comments on this manuscript. We are very grateful for all laboratory personnel of Department of Allergy and Clinical Immunology of Children Medical Center. We are also thanking the colleagues in Department of Pediatric Hematology/Oncology of Hannover Medical School and the Division of Rheumatology and Clinical Immunology of Freiburg University Hospital for their collaboration in molecular analysis of the samples. We gratefully acknowledge the efforts of Miss Tahereh AghaBagheri Kashi, Miss. Zahra Shobayri and Mrs. Saeideh Zoroofchi for arrangement and administrative efforts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rezaei, N., Moin, M., Pourpak, Z. et al. The Clinical, Immunohematological, and Molecular Study of Iranian Patients with Severe Congenital Neutropenia. J Clin Immunol 27, 525–533 (2007). https://doi.org/10.1007/s10875-007-9106-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-007-9106-y