Abstract
This study examined whether spiritual beliefs are associated with greater decision-making satisfaction, lower decisional conflict and decision-making difficulty with the decision-making process in newly diagnosed men with prostate cancer. Participants were 1114 men diagnosed with localized prostate cancer who had recently made their treatment decision, but had not yet been treated. We used multivariable linear regression to analyze relationships between spirituality and decision-making satisfaction, decisional conflict, and decision-making difficulty, controlling for optimism and resilience, and clinical and sociodemographic factors. Results indicated that greater spirituality was associated with greater decision-making satisfaction (B = 0.02; p < 0.001), less decisional conflict (B = −0.42; p < 0.001), and less decision-making difficulty (B = −0.08; p < 0.001). These results confirm that spiritual beliefs may be a coping resource during the treatment decision-making process. Providing opportunities for patients to integrate their spiritual beliefs and their perceptions of their cancer diagnosis and trajectory could help reduce patient uncertainty and stress during this important phase of cancer care continuum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
Making an informed decision about how to treat one’s prostate cancer can be a time filled with anxiety, uncertainty, and stress (Dale et al., 2005; Kaplan et al., 2014; Zeliadt et al., 2006). Treatment options for clinically localized prostate cancer typically include definitive treatment with curative intent, including surgery or radiation therapy; or active surveillance, initial observation followed by definitive treatment if and when it is warranted by disease progression (American Urological Association Education and Research, 2007). Few randomized studies have been conducted to compare efficacy of these treatment modalities, and research outcomes do not provide clear evidence for superiority of one option (Bill-Axelson et al., 2011; Cooperberg et al., 2010; Wilt et al., 2009; Wilt et al., 2012). Consequentially, recommendations are that physicians and patients discuss benefits and risks of each intervention, and collaboratively weigh clinical indicators such as disease aggressiveness, patient’s life expectancy, and patient preferences and values with respect to potential side-effect and outcomes (American Urological Association Education and Research, 2007; Xu et al., 2011). Faith and spiritual beliefs may help prostate cancer patients cope with the fear and shock of a cancer diagnosis (Gall, 2004), however less is known about whether spirituality helps cancer patients cope with uncertainty and stress associated with treatment decision making or improves treatment decision-making experiences.
Spirituality has been conceptualized as a multidimensional set of beliefs and behaviors, including, but not limited to religious practices (Gall et al., 2005). It also includes secular beliefs, values, behavior, and personal experiences that bring peace and meaning into one’s life, as well as positive mental attributes such as purpose, connectedness, wellbeing, and hope (Gall et al., 2005; Hill & Pargament, 2003; Mattis, 2000). Stronger spiritual beliefs are associated with better physical and mental quality of life in survivorship (Krupski et al., 2006) and less treatment regret in prostate cancer patients (Hu et al., 2008). Patients also report that faith in God influences treatment choices (Silvestri et al., 2003), and more religious cancer patients have been found to choose more aggressive life-extending care (Balboni et al., 2007). However, theoretical perspectives and research on spirituality and cancer patients’ treatment decision making experiences are limited (Gall et al., 2005). Spirituality has been conceptualized as a source of support (Maton, 1989), a cognitive-affective frame for making meaning out of illness (Park, 2007), and as a source of coping resources (Gall, 2004); however these conceptual frameworks do not specifically address the role of spirituality and cancer treatment decision making. Furthermore, there is a dearth of empirical research exploring the role spiritual beliefs might have in improving cancer patients’ decision-making experiences (Zeliadt et al., 2006).
We assessed spirituality with the Functional Assessment of Chronic Illness Therapy-Spirituality (FACIT-Sp) (Peterman et al., 2002), which measures two kinds of generalized beliefs, beliefs about living a life with meaning and purpose, and feeling at peace (e.g., ‘I have a reason for living’) and beliefs about the role of faith in the context of one’s illness (e.g., ‘I find strength in my faith or spiritual beliefs’). A number of studies associate scores on the FACIT-Sp with QOL outcomes, including health-related QOL (Cotton et al., 1999; Krupski et al., 2006; Salsman et al., 2010; Tate & Forcheimer, 2002). The authors conceptualized the FACIT-Sp as dimensions of “spiritual well-being” (Peterman et al., 2002); however, they are neither coping appraisals nor coping behaviors. The FACIT-Sp assesses beliefs about the self and the self’s relationship with the world, and are thus, enduring mental representations. An important distinction can be made between mental representations which are structures, and dynamic appraisal processes or real-time relational evaluations of the significance of ongoing events for well-being (Cervone, 2004; Lazarus, 1991). Similarly, a distinction can be drawn between enduring mental representations and dynamic coping behaviors. Knowledge structures are distal determinants that may influence behavior through the way they inform appraisals (Cervone, 2004). We speculate that the spiritual beliefs assessed by the FACIT-Sp influence appraisals about the challenge of deciding how to treat one’s prostate cancer and are therefore likely determinants of coping in this situation. Enduring beliefs about spirituality may help men engage more actively in treatment decision-making, as part of facilitating active coping. Active coping, where individuals behaviorally or psychologically try to change the stressor itself, is considered a better method for adapting to illness compared to avoidance coping, which includes denial, or disengagement, behaviors that distract the person from the stressor, but do not change it (Roesch et al., 2005). After diagnosis, active coping may include engaging in treatment decision-making processes, including information seeking, deliberating over benefits and drawbacks of options, clarifying personal values, and ultimately enacting the decision. Some spiritual beliefs may facilitate active coping as patients with relatively stronger spiritual beliefs may feel supported or empowered by a higher power (Gall et al., 2005). Men with strong spiritual beliefs may also appraise the treatment decision as less threatening, which could increase their confidence in their coping abilities (Gall et al., 2005). Certain spiritual beliefs may also increase the likelihood of reappraising the treatment decision as an opportunity to gain insights about life (Pargament et al., 1998). These meaning-making functions of spiritual beliefs could facilitate engagement in decision-making behaviors. Finally, religions promote goals, values, priorities, and core schemas through which to interpret the world (Park, 2007); for those who are not religious, idiosyncratic spiritual belief systems may offer similar classes of beliefs. When made salient, values and priorities based in spirituality may be helpful for making a high-stakes decision such as deciding between cancer treatments (e.g. valuing sanctity of life could prioritize aggressive treatment).
Some spiritual beliefs, however, are not adaptive in the treatment decision-making context. These beliefs might be associated with avoidance coping, which is associated with worse adjustment among prostate cancer patients (Roesch et al., 2005). For example, putting all of one’s faith in God may limit active coping such as decision-making behavior (Gall et al., 2005). Given the adaptive nature of the beliefs (peace/meaning, faith during illness) assessed with the FACIT-Sp in the current study, we anticipate they are more likely to contribute to adaptive than maladaptive coping with treatment decision making.
The goal of our study was to explore whether spirituality is associated with patients’ experiences of the treatment decision-making process. We captured perceptions of this process with three outcomes measuring different aspects of the experience: decision-making satisfaction, which assesses satisfaction with components of the process (Holmes-Rovner et al., 1996), decisional conflict, which assesses uncertainty about treatment options (O’Connor, 1995), and decision-making difficulty, which assesses how difficult or stressful it is to make a treatment decision (Orom et al., 2009). These measures capture perceptions of a bounded event or series of events—making the treatment decision. The present study was premised on the idea that enduring spiritual beliefs are activated in the context of a prostate cancer diagnosis, and that these beliefs have positive effects on threat appraisals and coping behavior, including decision-making behaviors.
In previous studies, effects of spiritual beliefs on adjustment are shown to be mediated by optimism and resilience, perhaps because belief in a higher power and divine plan encourage a positive outlook and strength through stressful situations (Salsman et al., 2005; Scheier et al., 1994; Stewart & Yuen, 2011). As positive effects of spirituality on psychological adjustment in illness may be through optimism and resilience, we included these variables in our models of the treatment decision-making experience.
The research question guiding this study is, do men diagnosed with clinically localized PCa who have stronger spiritual beliefs including peace, meaning, and faith during illness, experience greater decision-making satisfaction, less decisional conflict, and less decision-making difficulty when deciding how to treat their prostate cancer? Results will help us better understand whether spirituality can function as coping resources during the treatment decision-making process in men newly diagnosed with clinically localized prostate cancer.
Methods
Procedure
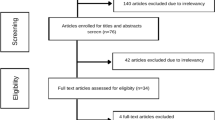
Data for the current study are from a larger multi-site longitudinal study of PCa treatment decision making. Participants in the parent study were newly diagnosed PCa patients, recruited from five clinical facilities, including two academic cancer centers and three community practices. Participants in the present analyses were among those recruited between 2010 and 2013 who completed questionnaires in the clinic or returned them by mail prior to treatment. Demographic, clinical data, optimism, and resilience were assessed with a questionnaire completed at, or near, time of consent, and treatment decision-making outcomes and spirituality were assessed in a second questionnaire completed after making the treatment decision, but prior to treatment. Study procedures were Institutional Review Board approved, and informed consent was obtained from all individual participants included in the study.
Participants
The subset of participants eligible to be included in the present study were 1135 participants who completed a baseline questionnaire as of October 2013 (n = 1599) and completed a questionnaire about treatment decision-making experiences by July 2014 (n = 1311). Cases (n = 145) with missing data on any variable included in the multivariable models were dropped (percentage missing per variable = 0.09–0.45 %). After excluding participants who reported “other” than the previously stated three categories for race/ethnicity (n = 19), the final sample contained 1114 individuals.
It is not possible to calculate response rates for the subset included in present analyses because at the time they were conducted, recruitment was ongoing. Recruiting, however, has since been completed. Among those patients eligible (n = 5203), 3338 were approached, 2477 were consented, and 2011 or 81.19 % of those consented completed the first questionnaire. Recruiters were unable to approach all patients because patients were seen at multiple facilities at the same time or at times during which the recruiters were not available.
Measures
Predictor variable
Spirituality was assessed with the FACIT-Sp (Peterman et al., 2002), a 12-item, 5-point Likert-type instrument made up of 2 subscales assessing strength and comfort from faith, and sense of meaning and purpose that spirituality provides (connection to a being larger than self) while coping with illness (α = 0.86). Response options range from not at all to very much. Scores are summative (range 0–48), with higher scores indicating higher levels of spiritual well-being.
Outcome variables
Patient satisfaction with the PCa decision-making process was assessed with a modified version of the Holmes-Rovner Satisfaction with Decision Scale (4 rather than 6 items; α = 0.87) (Holmes-Rovner et al., 1996). Items excluded from the scale assessed extent to which respondents expected to successfully carry out the decision made. Response options on the 5-point Likert-type items range from strongly disagree to strongly agree, and the 4 items were averaged (range 1–5), with higher levels indicating higher levels of decision-making satisfaction.
Decisional conflict was assessed using the 16-item Decisional Conflict Scale (O’Connor, 1995), assessing the degree to which participants are uncertain about their decision, believe that they are uninformed, unclear about personal values, unsupported in decision making, and feeling their choice was made appropriately (α = 0.89). Responses on the 5-point Likert items were yes, probably yes, unsure, probably no, and no. Scores were summed, divided by 16, and multiplied by 25 (range 0–100), with higher scores indicating increased decisional conflict.
Treatment decision-making difficulty was assessed using a 3-item instrument (α = 0.72) (Orom et al., 2009) that assesses the extent to which making the treatment decision was stressful and difficult, and whether knowing opinions of family members made the treatment decision more difficult. Response options on the 5-point Likert-type items range from strongly disagree to strongly agree. Scores are summative (range 3–15), with higher scores indicating greater decision-making difficulty.
Covariates
Optimism was assessed with the Life Orientation Test-Revised (Scheier et al., 1994). This 6-item scale assesses the extent to which respondents agree with statements including, ‘I’m always optimistic about my future’ (α = 0.82). Response options range from I agree a lot = 1, to I disagree a lot = 5, and scores are summative (range 6–30).
Resilience was assessed with the Brief Resilience Scale (Smith et al., 2008), a 6-item instrument assessing ability to recover from stressful situations. Items assess agreement with ideas such as, ‘I tend to bounce back quickly after hard times’(α = 0.86). Response options on the 5-point Likert-type items range from strongly disagree to strongly agree, and scores are averaged (range 1–5).
Demographic data and clinical variables
Participants self-reported level of education completed (high school, some college, college graduate or greater), race/ethnicity (non-Hispanic Black, Hispanic, non-Hispanic White; hereafter referred to as Black, Hispanic, and White), date of birth from which investigators calculated age at diagnosis, employment status (employed/not employed), and perceived social status (MacArthur scale of subjective social status) (Adler et al., 2000), and marital status (single/never married/divorced/widowed versus married/cohabitating). Participants also self-reported Gleason score from the biopsy that led to their diagnosis (≤5, 6, 7, 8–10, “don’t know”), and PSA level (≤4, 5–9, 10–14, 15–20, >20, “don’t know”) at time of diagnosis.
Statistical analyses
We conducted unadjusted linear regressions to examine bivariate relationships between spirituality and each decision-making outcome variable. Next, we conducted multivariable linear regressions with robust standard errors to examine associations of spirituality with each of the outcome variables as well as the two spirituality subscales, while controlling for optimism, resilience, Gleason score, PSA, education, perceived social status, employment status, marital status, site, and age at diagnosis. Optimism and resilience were included in the multivariable model to control for the potential association between spirituality and these variables. Income was not included in models due to the large number of missing values on the variable (13.90 %) and significant associations between income and education (r = 0.42, p < 0.001), and income and social status (r = 0.36, p < 0.001).
Results
Descriptive statistics
Participants were 84 % White, 9 % Black, and 7 % Hispanic, and 59 % had a college education or greater. Mean age at diagnosis was 63, 77 % reported having a biopsy Gleason score of 6 or 7; and 87 % reported that their PSA at diagnosis was 9 or lower (see Table 1 for participant characteristics). Table 1 also contains mean scores on decision-making outcomes, which were associated but not redundant. The correlation between decision-making satisfaction and decisional conflict was r = −0.56, p < .001; between decision-making satisfaction and decision-making difficulty was r = −0.26, p < .001; and between decisional conflict and decision-making difficulty was r = 0.30, p < .001.
Unadjusted linear regressions
In unadjusted analysis, greater spirituality was associated with greater decision-making satisfaction [B = 0.02; 95 % Confidence Interval (CI) 0.01, 0.02; p < .001], less decisional conflict (B = −0.42; 95 % CI −0.50, −0.35; p < .001), and less decision-making difficulty (B = −0.10; 95 % CI −0.12, −0.08; p < .001).
Multivariable regression analyses
In multivariable models (Table 2), greater spirituality was associated with greater decision-making satisfaction (B = 0.02; 95 % CI 0.01, 0.02; p < .001; partial η2 = 0.05). Greater spirituality was also associated with less decisional conflict (B = −0.42; 95 % CI −0.51, −0.33; p < .001; partial η2 = 0.07) and less decision-making difficulty (B = −0.08; 95 % CI −0.10, −0.05; p < .001; partial η2 = 0.04).Footnote 1 Among covariates (see Table 2), greater resilience was associated with less decisional conflict and decision-making difficulty. Being Black compared to White was associated with lower decision-making satisfaction and greater decisional conflict. Being Hispanic compared to White was also associated with lower decision-making satisfaction. Older age at diagnosis was associated with less decision-making satisfaction, greater decisional conflict, and less decision-making difficulty. Finally, being married or cohabitating was associated with less decisional conflict and less decision-making difficulty.
Discussion
Results contribute to a growing body of literature that addresses the potential role of spirituality and coping post cancer diagnosis (Gall et al., 2005). We found associations between the extent to which men reported spiritual well-being and a better decision-making process, including greater decision-making satisfaction and less decisional conflict and decision-making difficulty. Results are consistent with existing frameworks that conceptualize spirituality as a resource in adjustment to illness (Gall et al., 2005; Jenkins & Pargament, 1995; Maton, 1989; Park, 2007). Our findings indicate that application of spiritual coping frameworks might be relevant to the cancer treatment decision-making phase.
Prostate cancer treatment decision making can be a significant stressor (Gwede et al., 2005; Orom et al., 2009). Key pathways described within theoretical frameworks that delineate relationships between spirituality and coping with illness may provide insight into how spirituality influences coping with prostate cancer treatment decision-making. Maton’s work on spiritual support (Maton, 1989), Park’s conceptualization of spirituality as meaning making (Maton, 1989; Park, 2007), and Gall et al. (2005) integration of spirituality into transactional coping theory incorporate the notion that spirituality contributes to positive appraisals of illness stressors. Spiritual beliefs and supportive components of an individual’s relationship with a higher power, including perceptions of God’s love, presence, guidance, and constancy, are hypothesized to increase adoption of positive reappraisal of illness threats (Gall et al., 2005). In the context of treatment decision making, these positive appraisals may increase perceived control over, and self-efficacy for, or confidence in decision-making behaviors. Both should increase the likelihood of engaging in decision-making behaviors such as information-seeking, deliberating over benefits and drawbacks of options, clarifying personal values, and ultimately enacting the decision (Gall, 2004; Jenkins & Pargament, 1995). Positive appraisals may also reduce anxiety, an additional barrier to engaging in decision-making behaviors (Swainston et al., 2011; Sweeny et al., 2010).
Spirituality as a meaning-making resource has been described as a system of motivational, affective, and cognitive components for making meaning in life (Park, 2007) and may be the ultimate outcome of spiritual coping (Gall et al., 2005). Many positive appraisals may contribute to making meaning in the face of cancer stressors that can otherwise lead to considerable sense of loss of sense of coherence and uncertainty. To the extent that this reduces psychological distress, patients may be more able to engage in decision-making behaviors.
In sum, although untested, existing theoretical frameworks contain psychological processes through which spiritual beliefs and schemas plausibly influence adaptive coping with decision-making stressors. Mediating pathways may include positive appraisals, increased decision-making self-efficacy, perceived control, reduced anxiety, and meaning making. Additional research should test whether relationships between spirituality and treatment decision-making experiences reflect one or more of these particular processes.
The study findings have important implications for supportive care in cancer. Given the possibility that spiritual beliefs influence coping with treatment decision making, supportive care might include discussion of spiritual beliefs early in diagnosis, while patients are making their treatment decisions. While such discussions may be routine with patients, with terminal disease (Richardson, 2012), having them with patients with better prognosis who are early in their cancer trajectory, including clinically localized prostate cancer patients deciding how to treat their cancer, may be innovative. Nurses, psychologists, and social workers have a unique opportunity to speak with patients about their spiritual beliefs and their potential role in the decision-making process (Richardson, 2012). Because the meaning of spirituality and religiosity differs among individuals, such interventions may include a comprehensive assessment of spiritual and existential beliefs, and follow-up discussion could help newly diagnosed patients make salient and clarify their spiritual beliefs, enabling them to interpret illness experiences in the context of these beliefs (Pearce et al., 2012). Most spiritual interventions have been focused on improving psychological well-being post-treatment and results show a moderate-sized ameliorative effect on outcomes such as depression and anxiety (Oh & Kim, 2012). Addressing spiritual beliefs early in the cancer trajectory, as a way of helping patients clarify their priorities and values and reappraising the illness threat during decision-making, would be a novel application in the domain of spirituality and cancer care.
Limitations and strengths
There are several important limitations in the current study. Firstly, the cross-sectional nature of the present study limits conclusions regarding causation or changes in spiritual well-being over time. Nevertheless, further research in this area with a measure of spirituality rather than spiritual well-being would help clarify these important issues. An additional limitation of the instrument is that it excludes the measurement of other constructs and beliefs, including feelings of abandonment by God, expressions of dissatisfaction with clergy or religious community members, reinterpretations of illness as acts of the devil, and a sense of anger or confusion over one’s relationship with God, may be maladaptive (Gall et al., 2005; Pargament et al., 1998). These beliefs may be one reason that reviews of spiritual coping strategies note mixed to little evidence for the beneficial effect of religious and spiritual coping in illness (Park, 2007; Thune-Boyle et al., 2006). In contrast, our findings suggest a more adaptive role for spiritual beliefs, perhaps in part due to the nature of the beliefs we assessed, but also perhaps because of the outcomes measured. None of the previous studies explored associations between spirituality and treatment decision-making experiences. In addition, Gleason score was self-reported, and some men cannot accurately report their Gleason score; however, using a self-reported score can be advantageous because it captures an element of men’s perceived cancer aggressiveness, which may influence the treatment decision-making experience, the focus of the present study. That said, in a subset of participants in the parent study who had valid responses for both self-reported and medical record-abstracted Gleason scores (n = 1550), percent agreement between the two was 79 %. Finally, associations between spirituality and decision-making outcomes were modest, although reliable. Future studies might examine whether relationship between spirituality and decision-making experiences are stronger for some individuals than others and identify moderating factors of this relationship.
Strengths of our study include large sample size and inclusion of optimism and resilience within the models, accounting for potential confounding of spiritual beliefs and these enduring belief tendencies. In addition, analysis of three decision-making outcome variables allows for evaluation of the association of spirituality with multiple components of the decision-making experience. Research on the association between spirituality and well-being has been critiqued for using scales, including the FACIT-Sp, that include items that capture constructs related to well-being (Visser et al., 2010). The present work demonstrates that the FACIT-Sp is meaningfully related to treatment decision-making experiences that are conceptually very distinct from well-being. The present findings help build confidence that spiritual beliefs play a causal role in coping with a cancer diagnosis, and are not simply a facet of psychological adjustment to the disease.
To our knowledge, this is the first study to report an association between spirituality and decision making for men with clinically localized prostate cancer who are post-diagnosis, but pre-treatment. Spiritual beliefs may be a coping resource that has yet to be systematically incorporated into processes and structures sometimes used to help men with prostate cancer make treatment decisions, including interactions with health care and psychosocial support providers, as well as decision-aids. Providing opportunities for patients to discuss their spiritual beliefs in context of their diagnosis and treatment decision making could make salient beliefs that help reduce patient uncertainty and anxiety during this stressful phase of the cancer care continuum.
Notes
As the FACIT-Sp subscales assess quite distinct constructs, it is possible that one or the other was largely responsible for the reported associations with the decision-making outcomes. We wanted to verify that both subscales were associated with the decision-making scales. They were; scores on the meaning/peace subscale were significantly associated with greater decision-making satisfaction (B = 0.03; 95 % CI 0.03, 0.04; p < .001), lower decisional conflict (B = −0.77; 95 % CI −0.92, −0.62; p < .001), and lower decision-making difficulty (B = −0.15; 95 % CI −0.19, −0.11; p < .001). Scores on the faith in illness subscale were also associated with greater decision-making satisfaction (B = 0.02; 95 % CI 0.01, 0.02; p < .001), less decisional conflict (B = −0.39; 95 % CI −0.53, −0.24; p < .001), and less decision-making difficulty (B = −0.06; 95 % CI −0.10, −0.02; p = 0.003).
References
Adler, N. E., Epel, E. S., Castellazzo, G., & Ickovics, J. R. (2000). Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy, White women. Health Psychology, 19, 586–592. doi:10.1037/0278-6133.19.6.586
American Urological Association Education and Research. (2007). Prostate cancer: Guideline for the management of clinical localized prostate cancer: 2007 update. Rockville: National Guideline Clearinghouse.
Balboni, T., Vanderweker, L., Block, S. D., Paulk, M., Lathan, C., Peteet, J., & Prigerson, H. G. (2007). Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Journal of Clinical Oncology, 25(5), 555–560.
Bill-Axelson, A., Holmberg, L., & Ruutu, M. (2011). Radical prostatectomy versus watchful waiting in early prostate cancer. New England Journal of Medicine, 364(18), 1708–1717.
Cervone, D. (2004). The architecture of personality. Psychological Review, 111, 183–204.
Cooperberg, M., Broering, J., & Carroll, P. (2010). Time trends and local variation in primary treatment of localized prostate cancer. Journal of Clinical Oncology, 28(7), 1117–1123.
Cotton, S., Levine, E., Fitzpatrick, C., Dold, K., & Targ, E. (1999). Exploring the relationships among spiritual well-being, quality of life, and psychological adjustment in women with breast cancer. Psycho-Oncology, 8, 429–438.
Dale, W., Bilir, P., Han, M., & Meltzer, D. (2005). The role of anxiety in prostate carcinoma: A structured review of the literature. Cancer, 104, 467–468. doi:10.1002/cncr.21198
Gall, T. (2004). The role of religious coping in adjustment to prostate cancer. Cancer Nursing, 27(6), 454–461.
Gall, T., Charbonneau, C., Clarke, N., & Grant, K. (2005). Understanding the nature and role of spirituality in relation to coping and health: A conceptual framework. Canadian Psychology, 46(2), 88–104.
Gwede, C. K., Pow-Sang, J., Seigne, J., Heysek, R., Helal, M., Shade, K., & Jacobsen, P. (2005). Treatment decision-making strategies and influences in patients with localized prostate carcinoma. Cancer, 104(7), 1381–1390.
Hill, P. C., & Pargament, K. I. (2003). Advances in the conceptualization and measurement of religion and spirituality. American Psychologist, 58(1), 64–74.
Holmes-Rovner, M., Kroll, J., Schmitt, N., Rovner, D., Breer, M., Rothert, M., & Talarczyk, G. (1996). Patient satisfaction with health care decisions: The satisfaction with decision scale. Medical Decision Making, 16(1), 56–64.
Hu, J., Kwan, L., Krupski, T., Anger, J., Maliski, S., Connor, S., & Litwin, M. (2008). Determinants of treatment regret in low-income, uninsured men with prostate cancer. Oncology Nursing Forum, 72(6), 1274–1279. doi:10.1016/j.urology.2007.11.066
Jenkins, R., & Pargament, K. I. (1995). Religion and spirituality as resources for coping with cancer. Journal of Psychosocial Oncology, 13, 51–74.
Kaplan, A., Crespi, C., Saucedo, J., Connor, S., Litwin, M., & Saigal, C. (2014). Decisional conflict in economically disadvantaged men with newly diagnosed prostate cancer. Cancer, 120, 2721–2727. doi:10.1002/cncr.28755
Krupski, T., Kwan, L., Fink, A., Sonn, G., Maliski, S., & Litwin, M. (2006). Spirituality influences health related quality of life in men with prostate cancer. Psycho-Oncology, 15, 121–131.
Lazarus, R. S. (1991). Emotion and adaptation. New York: Oxford University Press.
Maton, K. (1989). The stress-buffering role of spiritual support: Cross-sectional and prospective investigations. Journal for the Scientific Study of Religion, 28(3), 310–323.
Mattis, J. S. (2000). African American women’s definitions of spirituality and religiosity. Journal of Black Psychology, 26(1), 101–122.
O’Connor, A. (1995). Validation of a decisional conflict scale. Medical Decision Making, 15, 25–30.
Oh, P., & Kim, Y. (2012). Meta-analysis of spiritual intervention studies on biological, psychological, and spiritual outcomes. Journal of the Korean Academy of Nursing, 42(6), 833–842.
Orom, H., Penner, L., West, B., Downs, T., Rayford, W., & Underwood, W. I. (2009). Personality predicts prostate cancer treatment decision-making difficulty and satisfaction. Psycho-Oncology, 18, 290–299. doi:10.1002/pon.1385
Pargament, K., Smith, B., Koenig, H., & Perez, L. (1998). Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion, 27(4), 710–724.
Park, C. (2007). Religiousness/spirituality and health: A meaning systems perspective. Journal of Behavioral Medicine, 30, 319–328. doi:10.1007/s10865-007-9111-x
Pearce, M., Coan, A., Herndon, J., Koenig, H., & Abernethy, A. P. (2012). Unmet spiritual care needs impact emotional and spiritual well-being in advanced cancer patients. Supportive Care in Cancer, 20, 2269–2276.
Peterman, A. H., Fitchett, G., Brady, M. J., Hernandez, L., & Cella, D. (2002). Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy-spiritual well-being scale (FACIT-Sp). Annals of Behavioral Medicine, 24(1), 49–58.
Richardson, P. (2012). Assessment and implementation of spirituality and religiosity in cancer care: Effects on patient outcomes. Clinical Journal of Oncology Nursing, 16(4), E150–E155. doi:10.1188/12.CJON.E150-E155
Roesch, S., Adams, L., Hines, A., Palmores, A., Vyas, P., Tran, C., & Vaughn, A. (2005). Coping with prostate cancer: A meta-analytic review. Journal of Behavioral Medicine, 28(3), 281–293. doi:10.1007/s10865-005-4664-z
Salsman, J., Brown, T., Brechting, E., & Carlson, C. (2005). The link between religion and spirituality and psychological adjustment: The mediating role of optimism and social support. Personality and Social Psychology Bulletin, 31, 522–535. doi:10.1177/0146167204271563
Salsman, J., Yost, K., West, D., & Cella, D. (2010). Spiritual well-being and health related quality of life in colorectal cancer: A multi-site examination of the role of personal meaning. Supportive Care in Cancer,. doi:10.1007/s00520-010-0871-4
Scheier, M., Carver, C., & Bridges, M. (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A re-evaluation of the life orientation test. Journal of Personal Social Psychology, 67, 1063–1078.
Silvestri, G., Knittig, S., Zoller, J., & Nietert, P. (2003). Importance of faith on medical decisions regarding cancer care. Journal of Clinical Oncology, 21(7), 1379–1382.
Smith, B., Dalen, J., Wiggins, K., Tooley, E., Christopher, P., & Bernard, J. (2008). The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine, 15, 194–200.
Stewart, D., & Yuen, T. (2011). A systematic review of resilience in the physically ill. Psychosomatics, 52(3), 199–208.
Swainston, K., Campbell, C., van Wersch, A., & Durning, P. (2011). Treatment decison making in breast cancer: A longitudinal exploration of women’s experiences. British Journal of Health Psychology, 17(1), 155–170. doi:10.1111/j.2044-8287.2011.02028.x
Sweeny, K., Melnyk, D., Miller, W., & Shepperd, J. (2010). Information avoidance: Who, what, when, and why. Review of General Psychology, 14(4), 340–353. doi:10.1037/a0021288
Tate, D., & Forcheimer, M. (2002). Quality of life, life satisfaction, and spirituality: Comparing outcomes between rehabilitation and cancer patients. American Journal of Physical Medicine and Rehabilitation, 81, 400–410.
Thune-Boyle, I., Stygall, J., Keshtgar, M., & Newman, S. (2006). Do religious/spiritual coping strategies affect illness adjustment in patients with cancer? A systematic review of the literature. Social Science and Medicine, 63, 151–164.
Visser, A., Garssen, B., & Vingerhoets, A. (2010). Spirituality and well-being in cancer patient: A review. Psycho-Oncology, 19, 565–572.
Wilt, T., Brawer, M., Barry, M., et al. (2009). The prostate cancer intervention versus observation trial: VA/NCI/AHRQ cooperative studies program #407 (PIVOT): Design and baseline results of a randomized controlled trial comparing radical prostatectomy to watchful waiting for men with clinically localized prostate cancer. Contemporary Clinical Trials, 30(1), 81–87.
Wilt, T., Brawer, M., & Jones, K. (2012). Radical prostatectomy versus observation for localized prostate cancer. New England Journal of Medicine, 367(3), 203–213.
Xu, J., Dailey, R., Eggly, S., Neale, A., & Schwartz, K. (2011). Men’s perspectives on selecting their prostate cancer treatment. Journal of the National Medical Association, 103, 468–478.
Zeliadt, S., Ramsey, S., Penson, D., Hall, I., Ekqueme, D., Stroud, L., & Lee, J. (2006). Why do men choose one treatment over another? A review of patient decision making for localized prostate cancer. Cancer, 106(9), 1865–1974. doi:10.1002/cncr.21822
Funding
NCI R01 CA152425.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michelle A. Mollica, Willie Underwood III, Gregory G. Homish, D. Lynn Homish, Heather Orom declare that they have no conflict of interest.
Human and animal rights and Informed consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Mollica, M.A., Underwood, W., Homish, G.G. et al. Spirituality is associated with better prostate cancer treatment decision making experiences. J Behav Med 39, 161–169 (2016). https://doi.org/10.1007/s10865-015-9662-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-015-9662-1