Abstract
The present study evaluates the influence of spirituality/religiosity (S/R) on the coping strategies used by people with cancer (breast and prostate) compared with those without cancer, in a sample of 445 Spanish participants (160 with cancer and 285 without). Significant interactions between the presence of cancer and S/R are observed in the use of coping strategies such as religion, humor and disconnection. Spirituality as a predictor variable through the use of religion as a strategy, increased the explanatory capacity of age by 58.9% (β = .794) while praying/talking to God predicts the use of this strategy with a β = .383. In people with cancer, active coping was predicted by spirituality (β = .327). However, spirituality was a negative predictor of maladaptive coping, with a beta coefficient equal to .383. The data suggest that patients’ beliefs need to be considered by health care professionals when designing interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Defining spirituality is a complex task due to the conceptual diversity that has existed when it comes to characterizing the construct (Kristeller et al., 2011; Paloutzian & Park, 2013). However, at present, there is consensus that “Spirituality is the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred.” (Puchalski et al., 2009, p.887). Spirituality relates to the way in which the moment is experienced, and the way in which people search for meaning and purpose or “transcendence” (Kristeller et al., 2011; Nolan et al., 2011). Spirituality can be understood as a way of perceiving, in an environment of a physical nature, the interaction with oneself and with “the other,” that is, a verbal regulation factor that could act as a belief. On the other hand, religiosity, or the way in which such a belief is disseminated, is of a normative, social or institutional nature (Testerman, 1997). Thus, religiosity can be understood to refer to the regulation of behavior on the basis of norms (religion) established by a social-religious organization. Religiosity, like religion, can be seen not only as an isolated behavior of an individual but also as a relationship with the whole community. The decision will depend, fundamentally, on personal spiritual needs, such as the need to feel part of a group, the need for a collective good, social support, and emotional support (Shatenstein & Ghadirian, 1998).
Spirituality/religiosity (S/R), as factors of verbal regulation (Carrasco, 2015), influence the way a person behaves (Pargament, 1999). The role of S/R in health care has been studied in professionals, patients and families (Gijsberts et al., 2019; Peteet & Balboni, 2013). Its influence is analyzed either as a mediating variable or considered in itself as a coping strategy for health (Burker et al., 2005; Darvishi et al., 2020), anxiety, depression and stress (Reutter & Bigatti, 2014), pain (Wiech et al., 2008) and cancer (Ahmadi et al., 2019; Kristeller et al., 2011; Peteet & Balboni, 2013; Trevino et al., 2016; Vespa et al., 2010).
S/R has been linked to secular coping strategies, understood as strategies that maintain a more naturalistic worldview and are therefore not based on religious practices, customs and/or rituals. (Krägeloh et al., 2012; Pasquale, 2007). Thus, these have been linked to active strategies such as positive reassessment, acceptance and humor (Farley et al., 2005), and with both active and emotional coping strategies (Bean et al., 2009; Ebert et al., 2002), with emotional strategies only (Schottenbauer et al., 2006) or with maladaptive strategies such as behavioral disconnection, denial and self-incrimination (Hastings et al. 2005; Liu & Iwamoto, 2007). Low factor loadings of religious coping (Kershaw et al., 2008; Lawrence & Fauerbach, 2003; Yang et al., 2008), or indications that this is an independent factor (Saroglou & Anciaux, 2004; Weininger et al., 2006; Wood & Rutterford, 2006), have also frequently been reported. In religious adaptation to secular methods of coping, it has been observed that in religious individuals, religious orientation affects the way religion is used as a resource for coping. An intrinsic religious orientation is more likely to be associated with problem-solving, while an extrinsic orientation is more likely to be related to the use of cognition in avoidance strategies (Aguilar-Vafaie & Abiari, 2007; Pargament et al., 1992).
There has been discussion of the extent to which religious coping can overlap with other strategies or whether it can provide a single coping strategy. Zwingmann et al. (2006) present data suggesting that the effects of religious coping on psychosocial adjustment in breast cancer patients were entirely mediated by non-religious coping strategies, and Perez et al. (2009) found that spiritual effort was mediated by acceptance. It has been observed that religious coping is just as often associated with problem-centered strategies, such as active coping, as it is with emotion-centered strategies, such as emotional support (Pargament et al., 2011). One suggested reason for these findings is that religious coping may be a unique strategy (Ai et al., 2009; Lewis et al., 2005), which is independent of other means of coping.
When faced with a cancer diagnosis, coping strategies are a determining factor in implementing adaptive processes (Hopman & Rijken, 2014). It is considered that strategies such as avoidance (Lan et al., 2019), repression (Cardona et al., 2013), passive coping (Vargas et al., 2011), self-blame (Teo et al., 2016), acceptance (Browall et al., 2016) and ruminant thinking (González et al., 2017) are generally less adaptive strategies. These strategies predict lower self-esteem and more depressive symptoms (Cieslak & Golusinski, 2018) and are often associated with low quality of life and negative emotional states (Brunault et al., 2016).
Those strategies that are considered to be more adaptive such as positive re-evaluation (Ortiz et al., 2014), problem-solving and religion-based coping (Park et al., 2018) are associated with a better quality of life (Finck et al., 2018), fewer mood swings (Ringwald et al., 2016), fewer depressive symptoms (Avis et al., 2013), a higher level of self-esteem (Ortiz et al., 2014) and increased psychological well-being (Danhauer et al., 2013).
The most frequently observed coping strategies in cancer patients are active (Joaquín-Mingorance et al., 2019) and problem-focused (Cao et al., 2018). These include positive re-evaluation and personal growth, active self-improvement and planning, followed by the use of religious beliefs (Granero-Molina et al., 2014), acceptance and social support (Cardenal & Cruzado, 2014). Age is a relevant aspect when analyzing the implications of a cancer diagnosis; since at early ages, it is usually consistently associated with a greater negative impact; while at an older age, it is usually associated with a more adaptive and positive coping style (Boyle et al., 2017).
Based on the results of previous research, this study aims to improve our understanding of the role of spirituality/religiosity in secular coping strategies used by people with a cancer diagnosis, in comparison with those who do not have cancer. It is expected that those who have received a cancer diagnosis will score higher on spirituality than people who have not been diagnosed with cancer. Further, people who recognize themselves as believers will show more active coping strategies than those who define themselves as non-believers. Finally, it is expected that scores on spirituality could predict active coping strategies and the use of religion as a coping strategy in people with cancer.
Method
Participants
The sample was composed of 445 participants (Mage = 46.87, SD = 10.68; Min = 31, Max = 79). Of the study participants, 36% (N = 160) had been diagnosed with cancer (34.4% men with prostate cancer and 65.6% women with breast cancer) and 64% (N = 285) had no diagnosis of cancer (31.58% men and 68.42% women).
Instruments
In order to collect the information, an ad hoc interview was designed, requesting socio-demographic information (year of birth and gender) and information on issues related to the disease (which were not addressed in participants without cancer). The following information was requested in relation to the disease: “Type of cancer” (breast or prostate), “Approximately how long (months) since the diagnosis of the disease,” “Have you had surgery?” (Yes/No), “What treatments have you had (radiation, chemotherapy, hormone therapy, no treatment, or other)?” People who had not been diagnosed with cancer were asked if they are suffering from any other disease (e.g., cardiovascular, bone, immunological, neurological or infectious disease).
The participants classified themselves according to the extent or type of religious belief as: (1) Non-believer (NB).–I have no doubt, I do not believe in the existence of divine, superior or beyond beings, outside the realm of nature, (2) Non-practicing believer (NPB).–I believe in the existence of one or more divine beings, superior or from the beyond, but months can pass without attending mass-cult and/or religious events and (3) Practicing believer (PB).–I believe in the existence of one or more divine beings, superior or from the beyond and I usually attend mass-cult and/or religious events, attempting to fulfill the precepts of my religion. Finally, they were asked “Estimate the number of times you usually attend religious or spiritual events in a month” (attend religious events) and “how many days a week you talk/pray/converse with your God” (Praying/Talking with God).
Spirituality was evaluated by means of the Beliefs and Values Scale (BVS) (King et al., 2006) in its Spanish translation (Carrasco, 2015) which consists of 20 items (e.g., “I believe that I possess a soul or spirit and that it can survive my death”) with a 5-point Likert type scale consisting of -strongly agree (4); agree (3); neither agree nor disagree (2); disagree (1); strongly disagree (0). In this study, the scale had shown very acceptable reliability, with a Cronbach’s Alpha value of α = 0.965.
To evaluate the coping strategies, The Brief COPE Scale (Carver, 1997) was used in its Spanish adaptation COPE-28 (Moran et al., 2010). This scale presents a total of 28 items, which are answered on a Likert-type scale with four response alternatives (Nothing, A little, Quite and A lot). The instrument assesses 14 main response strategies: active coping (taking direct action to eliminate or reduce the stressor), planning (thinking about how to cope with the stressor and planning strategies), use of emotional support (getting emotional support, understanding), use of social support (getting help and advice from others), religion (tendency to turn to religion in times of stress), positive reassessment (looking for positive aspects of the problem and trying to improve or grow from the situation), acceptance (accepting the facts of what is happening, and that they are real), denial (denying the reality of the stressful event), humor (laughing at the situation), self-distraction (trying to distract oneself with other activities to avoid focusing on the stressor), self-blame (blaming oneself for the situation), behavioral disconnection (reducing efforts to deal with the stressor), venting (tendency to express feelings of emotional distress) and substance use (using alcohol or other substances to feel good or help deal with the stressor). In this study, the reliability coefficient of the scale, evaluated using Cronbach’s Alpha, was acceptable (α = 0.730).
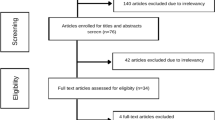
Procedure
We decided to only consider people with prostate and breast cancer since these are two of the most common types of cancer; thus, other types of cancer or other chronic diseases were considered as exclusion criteria. A mixed procedure was employed to recruit the sample. Both prostate and breast cancer associations were contacted, and data were collected in person, while an online questionnaire was designed and distributed via e-mail to various cancer associations in the country (Spain). For people without cancer, we approached various associations and asked for volunteers within the same age range, with the only requirement being to not have an illness. Approval for this study was obtained from the Andalusian Ethics Committee of Biomedical Research (Evaluation Committee of Huelva; Internal Code: 1113 N-16. The procedures used in this work adhere to the tenets of the Declaration of Helsinki of 1975, revised in 2013. Written informed consent was obtained from all the participants.
Data Analyses
The statistical analyses were conducted using IBM SPSS Statistics 20 software (SPSS Inc., Chicago, IL, 2017). First, the reliability of the scales was analyzed from the internal consistency analysis, using Cronbach’s Alpha statistic. The basic descriptive statistics were considered to characterize the sample (means, standard deviation, percentages, etc.). The Student t test was used to compare two independent samples; Cohen’s d was used to calculate the effect size (“small” effect: between 0.2 and 0.3, “medium” effect: around 0.5 and “large” effect: > 0.8). The Chi2 test (χ2) was used to compare categorical variables. ANOVA was used to compare mean scores in the categorical variables; the effect size (η2) is considered to be large if η2 > 0.14. A univariate ANOVA test was conducted to analyze the interactions between the type of belief and the presence or absence of disease.
Finally, according to the conclusions of the factor analysis conducted by Krägeloh et al. (2012) on the relationships between S/R and coping strategies in health care settings, composite modes of coping were created from the 14 subscales of the COPE Brief. Three general subscales were formed for use in part of the statistical analyses: active coping (acceptance, active coping, humor, planning, positive re-evaluation, religion), emotional coping (use of emotional support, use of social support) and maladaptive coping (denial, disconnection from behavior, self-blame, self-distraction, substance use, venting). The ANOVA test and corresponding effect sizes were used (η2) to compare the mean scores for the three factors among the belief groups. Finally, a linear regression analysis was conducted to individually predict the various coping strategies and the three factors.
Results
The sample was composed of 445 participants, of which 32.6% were men and 67.4% were women. The basic characteristics of the sample according to gender and the categorization of participants based on religious beliefs can be seen in Table 1.
Participants with cancer indicated a time from diagnosis of M = 48.43 months (SD = 41.59) (Mmale = 54.96, SD = 33.775 y Mfemale = 45.01, SD = 44.921); with no significant differences between men and women (t = 1.443, p = 0.151, d = 0.24). Of the 160 participants who reported having cancer, 78.8% have undergone surgery for the disease, 67.5% have received radiotherapy treatment, 70.6% have undergone chemotherapy and 53.1% have been treated with hormone therapy.
Participants were defined as NB 33.93% (N = 151), NPB 36.85% (N = 164) and PB 29.21% (N = 130). It was observed that in the spirituality test (BVS), the three groups of beliefs are statistically different (F(2,444) = 585.704, p < 0.001) where the PBs obtain (M = 84.02, SD = 8.70) values higher than the NPBs (M = 69.82, SD = 11.61) and the NBs (M = 39.17, SD = 12.95). With respect to the variable attendance at religious events, the PB (M = 6.34, SD = 13.81) differs significantly from the NPBs (M = 0.47, SD = 0.83) and the NBs (M = 0.17, SD = 0.96), but the latter two groups do not differ (F(2,444) = 30.453, p < 0.001). Finally, there were differences between the three groups with regard to the number of times they report praying or talking to God, with the PBs doing this with the highest frequency (M = 6.08, SD = 1.74), followed by the NPBs (M = 3.34, SD = 2.68) and the NBs (M = 0.17, SD = 0.96), a difference that reached statistical significance (F(2,444) = 320.536, p < 0.001).
The mean score on the Beliefs and Values Scale (BVS-Spirituality) for the whole sample was 63.57 points (SD = 21.62), with M = 60.97 (SD = 22.66) for males and 64.82 (SD = 21.03) for females. Table 2 shows how the participants with a cancer diagnosis—in comparison with those who have not—are significantly more likely to identify themselves as believers, either PB or NPB, (p < 0.001, Cramer’s V = 0.271). Likewise, the participants diagnosed with cancer, as opposed to those without cancer, obtained higher scores on spirituality; but they do not differ in terms of the number of times they attend religious events or in the number of days they report praying/talking to God.
Further, an ANOVA conducted on the scores obtained on the different coping strategies of people with a cancer diagnosis according to the religious group with which they identify revealed differences in active coping and religion. For those without a cancer diagnosis, there are differences in all the strategies except for those of positive reevaluation, denial, self-distraction, disconnection and substance use (Table 3).
After conducting Bonferroni’s post hoc test on the group with a cancer diagnosis, it was observed that for the active coping strategy, there were differences between the NB > PB, with a small effect size and between the three religious belief groups (PB > NPB > NB), presenting a large effect size. In addition, in disconnection, there is a residual difference between NB > PB. Further, in the group without a cancer diagnosis, the variables of planning and mood differed significantly between the groups NB > NPB and NB > PB with a medium effect size, while for the emotional support strategy (NB > NPB, NB > PB), these differences had a small effect size. The social support and active coping strategies both present a small effect size, and only between NB > PB. In acceptance as a strategy the differences, with a small effect size, are between NB > NPB; while for venting and self-incrimination, also with a small effect size, differences were observed between the groups NB > PB and NPB > PB. Finally, for religion as a coping strategy, there were differences between the three groups, with a large effect size (PB > NPB > NPB).
Table 4 displays the results of the univariate ANOVA conducted on the coping strategies, controlling for the presence of cancer and the belief group with which the participants identify.
A significant interaction was found between the presence of cancer and the belief group, with religion, humor and disconnection as coping strategies. The belief group scored significantly higher on active coping, planning, social support and self-blame.
Linear regression analysis was conducted with the aim of predicting the use of the different coping strategies, considering age, spirituality, praying/talking to God and attending religious events as predictive variables (Table 5). It can be observed that in the use of religion as a coping strategy, spirituality increases the explanatory capacity of the model by 58.9% with respect to the age variable (β = 0.794, p < 00.001).
It should be noted that the explanatory contribution of spirituality is positive in the use of strategies such as religion, positive re-evaluation and acceptance; while in the other strategies, its contribution has negative values. In this sense, planning (β = −0.190, p ˂ 0.001), self-incrimination (β = −0.156, p = 0.001) and humor (β = −0.107, p < 00.001) can be highlighted. Further, the variable praying/talking with God made a marked and positive contribution to the explanatory value of the models in religious strategies (β = 0.383, p ˂ 0.001) and negative in the strategies of self-incrimination (β = −0.196, p = 0.008) and venting (β = −0.245, p = 0.001).
If we consider the results of the factor analysis carried out by Krägeloh et al. (2012) and the coping strategies are grouped into three factors (active coping mode, emotional coping mode and maladaptive coping mode) the ANOVA revealed that Group PB differs from the other two groups in two of the three factors (Table 6).
Thus, PBs obtained higher scores, when compared with NPBs and NBs, in the active coping mode (Factor 1) and lower scores in the maladaptive coping mode (Factor 3).
Finally, a linear regression analysis was carried out with the aim of predicting the three factors in the participants that present a cancer diagnosis, with the predictive variables of both age and spirituality. This analysis revealed that spirituality increases the explanatory value of the model for Factor 1 by 10.5% (β = 0.327, p < 0.001) and by 3.8%, but with a negative explanatory value, for Factor 3 (β = −0.196, p = 0.013). Moreover, in participants without the disease, spirituality explains Factor 1 with a β = 0.153, p = 0.011 and negatively explains Factor 2, with a β = −0.149, p = 0.012) (see Table 7).
Discussion
The main objective of this study was to improve our understanding of the role of spirituality/religiosity in the secular coping strategies used by people diagnosed with cancer, compared with those who have not been diagnosed with cancer.
The data appear to support the first of our hypotheses, since participants with a cancer diagnosis show higher scores on spirituality than those without such a diagnosis. In addition, participants with a cancer diagnosis are more likely to consider themselves as believers—either practicing or non-practicing—than participants who do not have the disease, who mostly acknowledge being non-believers. These findings are consistent with the evidence reported in previous research where the use of religion or religious beliefs has repeatedly been shown to be a coping strategy used by people with cancer (Elumelu et al., 2015; Granero-Molina et al., 2014; Krägeloh et al., 2012; Rutskij et al., 2010), with spirituality being very common among cancer patients in southern Europe (Travado et al., 2010). Practicing believers—through regular participation in religious rituals in the community—are likely to encounter groups that act as support groups, where religious coping strategies and consistent social support are strengthened in comparison with non-practicing believers and non-believers (Ahmadi, et al., 2019; Ju et al., 2016; Peres et al., 2017; Shatenstein & Ghadirian, 1998).
With regard to the second of our hypotheses, where it was expected that people who acknowledge being believers will show more active coping strategies than those who identify themselves as non-believers, the results have shown that this is not fully confirmed in all the active strategies that have individually been considered in the COPE scale. People who identify themselves as believers only show higher scores than non-believers in using religion as an active coping strategy; and these differences emerged for both practicing and non-practicing believers. These data support the findings of other studies where spirituality/religiosity has been linked to the use of religion as an active coping strategy with adaptive outcomes (Elumelu et al., 2015; Granero-Molina et al., 2014; Park et al., 2018; Rutskij et al., 2010). However, our findings can be contrasted with the results of research studies suggesting that S/R is linked to active strategies such as positive re-evaluation, acceptance and humor (Farley et al., 2005), active emotional coping strategies (Bean et al., 2009; Ebert et al., 2002), emotional strategies only (Schottenbauer et al., 2006) and even with maladaptive strategies such as behavioral disconnection, denial and self-incrimination (Hastings et al., 2005; Liu & Iwamoto, 2007).
Further, when considering the trifactorial model proposed by Krägeloh et al. (2012), these data support the notion that practicing believers obtain higher scores on active strategies. It is possible to observe how practicing believers—as opposed to non-practicing believers and non-believers—score higher on Factor 1 or the active coping mode (acceptance, active coping, humor, planning, positive re-evaluation, religion); while non-believers and non-practicing believers do not differ with regard to this factor. However, practicing believers score lower than non-believers and non-practicing believers in the maladaptive (or Factor 3) coping mode (denial, disconnection from behavior, self-blame, self-distraction, substance use, venting). The latter result runs counter to the findings reported by Hastings et al. (2005) and Liu and Iwamoto (2007) who observed that S/R is associated with maladaptive strategies such as behavioral disconnection, denial and self-incrimination. This could be explained if we consider the fact that in religious people, S/R affects the way religion is used to cope with stressful situations (Aguilar-Vafaie & Abiari, 2007; Pargament et al., 1992).
Finally, the third of the hypotheses, where it was anticipated that spirituality scores would predict active coping strategies and the use of religion as a coping strategy in people with cancer, was only partially confirmed since spirituality has only been shown to improve the predictive model of the use of religion as an active coping strategy. However, the contribution of this factor to the model was found to be negative with respect to the rest of the individual active strategies. As observed in the trifactorial model developed by Krägeloh et al. (2012), spirituality presents, alongside age, an explanatory capacity of 32.7% in for Factor 1 or active coping mode in individuals with cancer and 15.3% in the population without a cancer diagnosis. With respect to maladaptive coping strategies or Factor 3, spirituality makes a negative contribution to age (β = −0.196). As explained in relation to the second hypothesis, these results can be understood if we consider the fact that religious coping overlaps with other strategies, or results in a single strategy (Ai et al., 2009; Lewis et al., 2005; Zwingmann et al., 2006), since R/S would act differently in believers and non-believers (Aguilar-Vafaie & Abiari, 2007). This debate still requires the support of further research to elucidate the relationships between S/R and secular coping strategies. Secular methods of coping and the lack of clarity with regard to whether religious coping can be assigned a higher-order factor structure could certainly reflect differences in the role that S/R plays in different groups of people (Aguilar-Vafaie & Abiari, 2007; Pargament et al., 1992). Coping strategies result from the way in which we construct the sense or meaning that is attributed to life events, both positive and negative. Further, it is important to identify how the individual resolves the discrepancy or differentiation between the global and situational meaning of events (Park, 2010). Thus, significant differences and similarities in existential, spiritual and religious coping have been observed across different countries and cultures. For example, Swedish people mainly use meaningful coping strategies based on meditation or relaxation, whereas Korean people resort to prayer and the use of a healthy diet as a means of survival (Ahmadi et al., 2017). This highlights the importance of considering the cultural context when we explore the use of meaningful coping strategies among people who have experienced cancer.
As limitations of the study, it is important to highlight the cross-sectional nature of the research design, since this does not allow for establishing how the use of coping strategies evolves and its relationships with the two variables considered (S/R) in these patients throughout the development of the disease or with advancing age. The selection of the participants makes it difficult to generalize the findings, and in this sense, it would be of interest to control and consider the different degrees or stages of the disease as well as the diversity of treatments that the patients have received, analyzing if specific changes occur in the strategies used and the characteristics of their relationships with S/R in the patients. In future studies, it will be important to consider religiosity, and religious diversity, from the perspective of intrinsic/extrinsic orientation, which has been shown to produce different results in the way people with diseases approach difficult or stressful situations.
In conclusion, the data supports the need to consider the S/R variable in both the social and health interventions implemented with people diagnosed with cancer, since, as regulatory factors, these are of relevance in the behavior shown when facing the disease.
References
Aguilar-Vafaie, M. E., & Abiari, M. (2007). Coping response inventory: Assessing coping among Iranian college students and introductory development of an adapted Iranian coping response inventory (CRI). Mental Health, Religion & Culture, 10(5), 489–513. https://doi.org/10.1080/13674670600996639.
Ahmadi, F., Park, J., Kim, K. M., & Ahmadi, N. (2017). Meaning-making coping among cancer patients in Sweden and South Korea: A comparative perspective. Journal of Religion and Health, 56(5), 1794–1811. https://doi.org/10.1007/s10943-017-0383-3.
Ahmadi, F., Erbil, P., Ahmadi, N., & Cetrez, O. A. (2019). Religion, culture and meaning-making coping: A study among cancer patients in Turkey. Journal of Religion and Health, 58(4), 1115–1124. https://doi.org/10.1007/s10943-018-0646-7.
Ai, A. L., Seymour, E. M., Tice, T. N., Kronfol, Z., & Bolling, S. F. (2009). Spiritual struggle related to plasma interleukin-6 prior to cardiac surgery. Psychology of Religion and Spirituality, 1(2), 112–128. https://doi.org/10.1037/a0015775.
Avis, N. E., Levine, B., Naughton, M. J., Case, L. D., & Naftalis, E. (2013). Age-related longitudinal changes in depressive symptoms following breast cancer diagnosis and treatment. Breast Cancer Research Treatment, 139(1), 199–206. https://doi.org/10.1007/s10549-013-2513-2.
Bean, M. K., Gibson, D., Flattery, M., Duncan, A., & Hess, M. (2009). Psychosocial factors, quality of life, and psychological distress: Ethnic differences in patients with heart failure. Progress in Cardiovascular Nursing, 24(4), 131–140. https://doi.org/10.1111/j.1751-7117.2009.00051.x.
Boyle, C. C., Stanton, A. N., Ganz, P. A., & Bower, J. E. (2017). Posttraumatic growth in breast cancer survivors: Does age matter? Psycho-Oncology, 26(6), 800–807. https://doi.org/10.1002/pon.4091.
Browall, M., Kenne, S. E., Persson, L. O., Wengström, Y., & Gaston-Johansson, F. (2016). Patient-reported stressful events and coping strategies in post-menopausal women with breast cancer. European Journal of Cancer Care, 25(2), 324–333. https://doi.org/10.1111/ecc.12294.
Brunault, P., Champagne, A. L., Huguet, G., Suzanne, I., Senon, J. L., Body, G., Rusch, E., Magnin, G., Voyer, M., Réveillère, C., & Camus, V. (2016). Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non-metastatic breast cancer patients. Psycho-Oncology, 25(5), 513–520. https://doi.org/10.1002/pon.3947.
Burker, E. J., Evon, D. M., Sedway, J. A., & Egan, T. (2005). Religious and non-religious coping in lung transplant candidates: Does adding God to the picture tell us more? Journal of Behavioral Medicine, 28(6), 513–526. https://doi.org/10.1007/s10865-005-9025-4.
Cao, W., Qi, X., Cai, D. A., & Han, X. (2018). Modeling posttraumatic growth among cancer patients: The roles of social support, appraisals, and adaptive coping. Psycho-Oncology, 27(1), 208–215. https://doi.org/10.1002/pon.4395.
Cardenal, M. C., & Cruzado, J. A. (2014). Coping strategies and emotional distress in women with inconclusive results in screening mammography [Spanish]. Psicooncología, 11(2), 285–299. https://doi.org/10.5209/rev_PSIC.2014.v11.n2-3.47389.
Cardona, E. J., Jaramillo, A. C., & Díaz, V. E. (2013). Relationship between type C personality and cancer: State of the art [Spanish]. Psicoespacios: Revista Virtual de la Institución Universitaria de Envigado, 7(10), 66–92. https://doi.org/10.25057/21452776.140.
Carrasco, Y. (2015). Religion and its influence on health behaviors [Spanish]. (Doctoral thesis not published). University of Huelva. Spain.
Carver, C. S. (1997). You want to measure coping but your protocol´s too long: Consider the Brief COPE. International Journal of Behavioral Medicine, 4(1), 92–100. https://doi.org/10.1207/s15327558ijbm0401_6.
Cieslak, K., & Golusinski, W. (2018). Coping with loss of ability vs. emotional control and self-esteem in women after mastectomy. Reports of Practical Oncology and Radiotherapy, 23(3), 168–174. https://doi.org/10.1016/j.rpor.2018.02.002.
Danhauer, S. C., Douglas-Case, L., Tedeschi, R., Russell, G., Vishnevsky, T., Triplett, K., & Avis, N. E. (2013). Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology, 22(12), 2676–2683. https://doi.org/10.1002/pon.3298.
Darvishi, A., Otaghi, M., & Mami, S. (2020). The effectiveness of spiritual therapy on spiritual well-being, self-esteem and self-efficacy in patients on hemodialysis. Journal of Religion and Health, 59(1), 277–288. https://doi.org/10.1007/s10943-018-00750-1.
Ebert, S. A., Tucker, D. C., & Roth, D. L. (2002). Psychological resistance factors as predictors of general health status and physical symptom reporting. Psychology, Health & Medicine, 7(3), 363–375. https://doi.org/10.1080/13548500220139449.
Elumelu, T. N., Asuzu, C. C., & Akin-Odanye, E. O. (2015). Impact of active coping, religion and acceptance on quality of life of patients with breast cancer in the department of radiotherapy. UCH. BMJ Support Palliat Care, 5(2), 175–180. https://doi.org/10.1136/bmjspcare-2012-000409.
Farley, T., Galves, A., Dickinson, L. M., & Diaz-Perez, M. J. (2005). Stress, coping, and health: A comparison of Mexican immigrants, Mexican-Americans, and Non-hispanic whites. Journal of Immigrant Health, 7(3), 213–220. https://doi.org/10.1007/s10903-005-3678-5.
Finck, C., Barradas, S., Zenger, M., & Hinz, A. (2018). Quality of life in breast cancer patients: Associations with optimism and social support. International Journal of Clinical and Health Psychology, 18(1), 27–34. https://doi.org/10.1016/j.ijchp.2017.11.002.
Gijsberts, M. J., Liefbroer, A. I., Otten, R., & Olsman, E. (2019). Spiritual care in palliative care: A systematic review of the recent European literature. Medical Science, 7(2), E-25. https://doi.org/10.3390/medsci7020025.
González, M., Ibáñez, I., & Barrera, A. (2017). Rumination, worry and negative problem orientation: Transdiagnostic processes of anxiety, eating behavior and mood disorders [Spanish]. Acta Colombiana de Psicología, 20(2), 42–52. https://doi.org/10.14718/ACP.2017.20.2.3.
Granero-Molina, J., Diaz, M. M., Márquez, J., Castro-Sánchez, A. M., López, O. M., & Fernández-Sola, C. (2014). Religious faith in coping with terminal cancer: What is the nursing experience? European Journal of Cancer Care, 23(3), 300–309. https://doi.org/10.1111/ecc.12150.
Hastings, R. P., Kovshoff, H., Brown, T., Ward, N. J., Espinosa, F. D., & Remington, B. (2005). Coping strategies in mothers and fathers of preschool and school-age children with autism. Autism, 9(4), 377–391. https://doi.org/10.1177/1362361305056078.
Hopman, P., & Rijken, M. (2014). Illness perceptions of cancer patients: Relationships with illness characteristics and coping. Psycho-Oncology, 24(1), 11–18. https://doi.org/10.1002/pon.3591.
Joaquín-Mingorance, M., Arbinaga, F., Carmona-Márquez, J., & Bayo-Calero, J. (2019). Coping strategies and self-esteem in women with breast cancer. Annals of Psychology, 35(2), 188–194. https://doi.org/10.6018/analesps.35.2.336941.
Ju, C., Zhang, B., You, X., Alterman, V., & Li, Y. (2016). Religiousness, social support and subjective well-being: An exploratory study among adolescents in an Asian atheist country. International Journal of Psychology, 53(2), 97–106. https://doi.org/10.1002/ijop.12270.
Kershaw, T. S., Mood, D. W., Newth, G., Ronis, D. L., Sanda, M. G., Vaishampayan, U., & Northouse, L. L. (2008). Longitudinal analysis of a model to predict quality of life in prostate cancer patients and their spouses. Annals of Behavioral Medicine, 36(2), 117–128. https://doi.org/10.1007/s12160-008-9058-3.
King, M., Jones, L., Barnes, K., Low, J., Walker, C., Wilkinson, S., & Tookman, A. (2006). Measuring spiritual belief: Development and standardization of a beliefs and values scale. Psychological Medicine, 36(3), 417–425. https://doi.org/10.1017/S003329170500629X.
Krägeloh, C., Chai, U., Shepherd, P., & Billington, P. (2012). How religious coping is used relative to other coping strategies depends on the individual’s level of religiosity and spirituality. Journal of Religion and Health, 51(3), 1137–1151. https://doi.org/10.1007/s10943-010-9416-x.
Kristeller, J. L., Sheets, V., Johnson, T., & Frank, B. (2011). Understanding religious and spiritual influences on adjustment to cancer: Individual patterns and differences. Journal of Behavioral Medicine, 34(6), 550–561. https://doi.org/10.1007/s10865-011-9335-7.
Lan, M., Zhang, L., Zhang, Y., & Yan, J. (2019). The relationship among illness perception, coping and functional exercise adherence in Chinese breast cancer survivors. Journal of Advanced Nursing, 75(1), 75–84. https://doi.org/10.1111/jan.13832.
Lawrence, J. W., & Fauerbach, J. A. (2003). Personality, coping, chronic stress, social support and PTSD symptoms among adult burn survivors: A path analysis. Journal of Burn Care and Rehabilitation, 24(1), 63–72. https://doi.org/10.1097/00004630-200301000-00016.
Lewis, C. A., Maltby, J., & Day, L. (2005). Religious orientation, religious coping and happiness among UK adults. Personality and Individual Differences, 38(5), 1193–1202. https://doi.org/10.1016/j.paid.2004.08.002.
Liu, W. M., & Iwamoto, D. K. (2007). Conformity to masculine norms, Asian values, coping strategies, peer group influences and substance use among Asian American men. Psychology of Men & Masculinity, 8(1), 25–39. https://doi.org/10.1037/1524-9220.8.1.25.
Moran, C., Landero, R., & González, M. T. (2010). COPE-28: A psychometric analysis of the Spanish version of the Brief COPE [Spanish]. Universitas Psychologica, 9(2), 543–552.
Nolan, S., Saltmarsh, P., & Leget, C. (2011). Spiritual care in palliative care: Working towards an EAPC task force. European Journal of Palliative Care, 18(2), 86–89.
Ortiz, E., Méndez, L., Camargo, J., Chavarro, S., Toro, G., & Vernaza, M. (2014). Relationship between coping strategies, anxiety, depression and self-esteem in a group of adult patients diagnosed with cancer [Spanish]. Psychologia: Avances de la Disciplina, 8(1), 77–83. https://doi.org/10.21500/19002386.1216.
Paloutzian, R. F., & Park, C. L. (2013). Handbook of the Psychology of Religion and Spirituality. Guilford Press.
Pargament, K. (1999). The Psychology of Religion and Coping: Theory, Research and Practice. The Guilford Press.
Pargament, K., Olsen, H., Reilly, B., Falgout, K., Ensing, D. S., & van Haitsma, K. (1992). God help me (II): The relationship of religious orientations to religious coping with negative life events. Journal for the Scientific Study of Religion, 31(4), 504–513. https://doi.org/10.2307/1386859.
Pargament, K., Feuille, M., & Burdzy, D. (2011). A systematic review of studies using the Brief COPE: Religious coping in factor analyses. Religions, 2(1), 51–76. https://doi.org/10.3390/rel2010051.
Park, C. L. (2010). Making sense of the meaning literature: An integrative review of meaning making and its effects on adjustment to stressful life events. Psychological Bulletin, 136(2), 257–301. https://doi.org/10.1037/a0018301.
Park, C. L., Waddington, E., & Abraham, R. (2018). Different dimensions of religiousness/spirituality are associated with health behaviors in breast cancer survivors. Psycho-Oncology, 27(10), 2466–2472. https://doi.org/10.1002/pon.4852.
Pasquale, F. (2007). Unbelief and irreligion, empirical study and neglect of. In T. Flynn (Ed.), The New Encyclopedia of Unbelief. (pp. 760–766). Prometheus Books.
Peteet, J. R., & Balboni, M. J. (2013). Spirituality and religion in oncology. CA: A Cancer Journal for Clinicians, 6(4), 280–289. https://doi.org/10.1002/caac.21187.
Peres, M. F. P., Kamei, H. H., Tobo, P. R., & Lucchetti, G. (2017). Mechanisms behind religiosity and spirituality’s effect on mental health, quality of life and well-being. Journal of Religion and Health, 57(5), 1842–1855. https://doi.org/10.1007/s10943-017-0400-6.
Pérez, J. E., Chartier, M., Koopman, C., Vosvick, M., Gore-Felton, C., & Spiegel, D. (2009). Spiritual striving, acceptance coping, and depressive symptoms among adults living with HIV/AIDS. Journal of Health Psychology, 14(1), 88–97. https://doi.org/10.1177/1359105308097949.
Puchalski, C., Ferrell, B., Virani, R., Otis-Green, S., Baird, P., Bull, J., Chochinov, H., Handzo, G., Nelson-Becker, H., Prince-Paul, M., Pugliese, K., & Sulmasy, D. (2009). Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. Journal of Palliative Medicine, 12(10), 885–904. https://doi.org/10.1089/jpm.2009.0142.
Reutter, K. K., & Bigatti, S. M. (2014). Religiosity and spirituality as resiliency resources: Moderation, mediation, or moderated mediation? Journal for the Scientific Study of Religion, 53(1), 56–72. https://doi.org/10.1111/jssr.12081.
Ringwald, J., Wochnowski, C., Bosse, K., Giel, E., Schäffeler, N., Zipfel, S., & Teufel, M. (2016). Psychological distress, anxiety, and depression of cancer-affected BRCA1/2 mutation carriers: a systematic review. Journal of Genetic Counseling, 25(5), 880–891. https://doi.org/10.1007/s10897-016-9949-6.
Rutskij, R., Gaarden, T., Bremnes, R., Dahl, O., Finset, A., Fossa, S. D., et al. (2010). A study of coping in long-term testicular cancer survivors. Psychology, Health & Medicine, 15(2), 146–158. https://doi.org/10.1080/13548501003623955.
Saroglou, V., & Anciaux, L. (2004). Liking sick humor: Coping styles and religion as predictors. Humor: International Journal of Humor Research, 17(3), 257–277. https://doi.org/10.1515/humr.2004.012.
Schottenbauer, M. A., Klimes-Dougan, B., Rodriguez, B. F., Arnkoff, D. B., Glass, C. R., & LaSalle, V. H. (2006). Attachment and affective resolution following a stressful event: General and religious coping as possible mediators. Mental Health, Religion and Culture, 9(5), 448–471. https://doi.org/10.1080/13694670500440684.
Shatenstein, B., & Ghadirian, P. (1998). Influences on diet, health behaviours and their outcome in select ethno cultural and religious groups. Nutrition, 14(2), 223–230. https://doi.org/10.1016/s0899-9007(97)00425-5.
Teo, I., Fingeret, M. C., Liu, J., & Chang, D. W. (2016). Coping and quality of life of patients following microsurgical treatment for breast cancer-related lymphedema. Journal of Health Psychology, 21(12), 2983–2993. https://doi.org/10.1177/1359105315589801.
Testerman, J.K. (1997). Spirituality vs. religion: Implications for healthcare. Presentation in 20th Annual Faith and Learning Seminar. California, EE.UU.
Travado, L., Grassi, L., Gil, F., Martins, C., Liaventura, C., Bairradas, J., & The Southern European Psycho-Oncology Study Group (2010). Do spirituality and faith make a difference? Report from the Southern European Psycho-Oncology Study Group. Palliative and Supportive Care, 8(4), 405–413. Doi: https://doi.org/10.1017/S147895151000026X.
Trevino, K. M., Naik, A. D., & Moye, J. (2016). Perceived and actual change in religion/spirituality in cancer survivors: Longitudinal relationships with distress and perceived growth. Psychology of Religion and Spirituality, 8(3), 195–205. https://doi.org/10.1037/rel0000030.
Vargas, S., Herrera, G. P., Rodríguez, L., & Sepúlveda, G. J. (2011). Reliability of the questionnaire Brief COPE inventory in Spanish version for assessing coping strategies in patients with breast cancer [Spanish]. Investigación en Enfermería: Imagen y Desarrollo, 12(1), 7–24.
Vespa, A., Jacobsen, P. B., Spazzafumo, L., & Balducci, L. (2010). Evaluation of intrapsychic factors, coping styles, and spirituality of patients affected by tumors. Psycho-Oncology, 20(1), 5–11. https://doi.org/10.1002/pon.1719.
Weininger, C. F., Shalev, A. Y., Ofek, H., Freedman, S., Weissman, C., & Einav, S. (2006). Posttraumatic stress disorder among hospital surgical physicians exposed to victims of terror: A prospective, controlled questionnaire survey. Journal of Clinical Psychiatry, 67(6), 890–896. https://doi.org/10.4088/JCP.v67n0605.
Wiech, K., Farias, M., Kahane, G., Shackel, N., Tiede, W., & Tracey, I. (2008). An fMRI study measuring analgesia enhanced by religion as a belief system. Pain, 139(2), 467–476 https://doi.org/10.1016/j.pain.2008.07.030.
Wood, R. L. L., & Rutterford, N. A. (2006). Demographic and cognitive predictors of long-term psychosocial outcome following traumatic brain injury. Journal of the International Neuropsychological Society, 12(3), 350–358. https://doi.org/10.1017/S1355617706060498.
Yang, H. C., Brothers, B. M., & Andersen, B. L. (2008). Stress and quality of life in breast cancer recurrence: Moderation or mediation of coping? Annals of Behavioral Medicine, 35(2), 188–197. https://doi.org/10.1007/s12160-008-9016-0.
Zwingmann, C., Wirtz, M., Müller, C., Körber, J., & Murken, S. (2006). Positive and negative religious coping in German breast cancer patients. Journal of Behavioral Medicine, 29(6), 533–547. https://doi.org/10.1007/s10865-006-9074-3.
Funding
This work has not received funding.
Author information
Authors and Affiliations
Contributions
All authors made significant contributions to the study design, acquisition of data, drafting of the article and final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Ethical approval
Approved by the Andalusian Ethics Committee of Biomedical Research (Evaluation Committee of Huelva. Internal Code: 1113 N-16).
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Declaration of Helsinki of 1975, revised in 2013.
Informed consent
The participants filled Informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arbinaga, F., Mendoza-Sierra, M.I., Bohórquez, M.R. et al. Spirituality, Religiosity and Coping Strategies Among Spanish People Diagnosed with Cancer. J Relig Health 60, 2830–2848 (2021). https://doi.org/10.1007/s10943-021-01247-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10943-021-01247-0