Abstract
This meta-analysis examined whether effects of psychosocial interventions on psychological distress in cancer patients are conditional upon pre-intervention distress levels. Published articles and unpublished dissertations between 1980 and 2005 were searched for interventions reporting the Hospital Anxiety and Depression Scale (HADS) or the Spielberger State-Trait Anxiety Inventory (STAI). Multilevel mixed-effects modeling was used to meta-analyze effect-sizes separately for the HADS (27 trials, 2,424 patients) and STAI (34 trials, 2,029 patients). Pre-intervention distress significantly moderated intervention effects, explaining up to 50% of the between-study effect-size variance: effects on anxiety and depression were generally negligible when pre-intervention distress was low and pronounced when it was high. These results could not be explained by differences in intervention type, setting, dose, and whether intervention was targeted at distressed patients. Psychosocial interventions may be most beneficial for cancer patients with elevated distress. Future research should identify which treatment components are most effective for these patients to facilitate optimal treatment tailoring and cost-effective health care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A considerable number of trials have tested psychosocial interventions designed to reduce emotional distress and improve the quality of life of adult cancer patients. The overall efficacy of these interventions is vigorously debated (Stefanek et al. 2006). Studies have yielded mixed results, and previous systematic and meta-analytic reviews have drawn disparate conclusions about whether psychosocial treatment is generally beneficial (Meyer and Mark 1995; Rehse and Pukrop 2003; Tatrow and Montgomery 2006) or ineffective (Lepore and Coyne 2006; Newell et al. 2002) in reducing distress among cancer patients. Thus, it appears crucial to examine potential determinants of differential treatment efficacy, that is, to identify for whom and under what conditions interventions prove successful or not (King et al. 2008).
Intervention studies have commonly included cancer patients regardless of their current emotional well-being (Coyne et al. 2006; Sheard and Maguire 1999). However, there is substantial heterogeneity in the psychological sequelae of cancer diagnosis. While 20–40% of patients show clinically meaningful anxiety and depression, many report only transient emotional disruption and overall adjust quite well to the illness (van’t Spijker et al. 1997; Zabora et al. 2001). For that reason, it has been argued that the efficacy of intervention might well increase if it was selectively provided for those who are most in need because they experience significant psychological problems (Coyne et al. 2006; Sheard and Maguire 1999; Stanton 2005).
In recent years, evidence has emerged suggesting greater benefits of psychosocial interventions among patients who show elevated distress (Andersen et al. 2004; Boesen et al. 2005; Carmack Taylor et al. 2007; Given et al. 2004; Goodwin et al. 2001; Taylor et al. 2003) or lack psychosocial resources, such as self-esteem (Helgeson et al. 2006), optimism (Antoni et al. 2001), or social support (Scheier et al. 2007). However, it is unclear to what extent these encouraging results generalize across settings, interventions, and patient characteristics. Other studies have come to the opposite conclusion, suggesting stronger intervention effects for more positively adjusted patients compared to those with higher levels of depression (Doorenbos et al. 2006), anxiety (Carey and Burish 1985) or adjustment disorders (Hosaka et al. 2000). Systematic and integrative approaches to understand the need-benefit relationship in psychosocial interventions for cancer patients are warranted. In this report, we took a meta-analytic approach to evaluate the extent to which the efficacy of interventions in reducing distress is conditional upon patients’ pre-intervention anxiety and depression levels.
In a prior meta-analytic review, Sheard and Maguire (1999) found that interventions targeted at cancer patients who were either suffering from, or at high risk for, significant anxiety or depression showed clinically powerful effects (d = .85 for anxiety and d = .94 for depression) in contrast to those who were not (d = .33 for anxiety and d = .16 for depression). However, these differences were based upon a small number of studies and were not statistically significant. Similarly, Meyer and Mark (1995) did not find significantly greater effects in studies treating only patients with clear signs of emotional distress, chemotherapy side effects, or pain. Both of these reviews examined whether trials that involved screening for distress produced greater benefits. This analytic strategy is not optimal, however, because (1) few studies of this type have been conducted, and (2) if interventions specifically designed for distressed patients prove to be more effective, it remains unclear to what extent patient distress levels or the potentially unique aspects of this type of interventions account for a difference in effect sizes.
Here, rather than relying on study selection criteria, our goal was to investigate whether differences in pre-intervention distress levels that “naturally” occur across studies are systematically related to subsequent intervention effects. In order to make valid comparisons of pre-intervention distress between studies, all studies had to measure distress in the same way, or at least in sufficiently similar ways for the numerical values of distress to have comparable meaning across studies. Since a given score may indicate high or low distress on different measures, for the present project, only findings from studies that assessed distress with the same measure were aggregated. We focused on the Hospital Anxiety and Depression Scale (Zigmond and Snaith 1983) and the Spielberger State-Trait Anxiety Inventory (Spielberger 1983), because these well-validated measures are frequently employed in psychosocial oncology intervention research (Sheard and Maguire 1999; Tatrow and Montgomery 2006), commonly used as “benchmark” for validation of other measures, and recommended tools for distress screening in oncology practice (Carlson and Bultz 2003). Separate meta-analyses were conducted for the subscales of each of these instruments to examine the extent to which pre-intervention scores moderated intervention effects. We further examined if this moderating effect could be accounted for by intervention type, setting, or dose (factors previously found to moderate intervention effects in meta-analyses; Sheard and Maguire 1999; Tatrow and Montgomery 2006; Zimmermann et al. 2007), or by whether participants had been screened for distress (Lipsey 2003). Finally, we explored patient demographic and medical characteristics that might explain study-level differences in pre-intervention distress.
Methods
Study selection
The sample of studies was drawn from a larger systematic review of psychosocial interventions for cancer patients (Moyer et al. 2009). This larger review covers studies that (1) included 10 or more adults per group; (2) reported outcomes on psychological, emotional, behavioral, physiological, functional, or medical status; and (3) were first reported as a published article or an unpublished dissertation between January 1980 and December 2005. For the present analysis, studies were selected if they (4) used the Hospital Anxiety and Depression Scale or the Spielberger State-Trait Anxiety Inventory to evaluate outcomes, (5) presented the subscale scores for either measure at baseline, and (6) provided sufficient outcome data on the same measure to determine an unstandardized effect size. Reports were excluded if the original measure was modified.
Measures
Hospital anxiety and depression scale
The Hospital anxiety and depression scale (HADS) is a screening tool for emotional disorder in medical and surgical patients (Zigmond and Snaith 1983). Its two subscales measure symptoms of anxiety (HADS-A) and depression (HADS-D) during the past week. Total subscale scores range from 0 to 21. HADS-A scores of 9 or more, and HADS-D scores of 8 or more, are recommended as cutoffs for “caseness” of clinically meaningful anxiety and depression in cancer patients (Bjelland et al. 2002). The reliability and validity of the HADS subscales have been extensively established in a wide array of general medical and oncology patient samples (Bjelland et al. 2002).
Spielberger state-trait anxiety inventory
The Spielberger state-trait anxiety inventory (STAI) differentiates between transient state anxiety (STAI-S) and more stable trait anxiety (STAI-T), with respondents reporting how they feel at the present moment and in general (Spielberger 1983). Each subscale comprises 20 items, with total scores ranging from 20 to 80. Reliability, construct validity, and utility for distress screening have been widely documented in general and oncology samples (Barnes et al. 2002; Spielberger 1983; Stark et al. 2002).
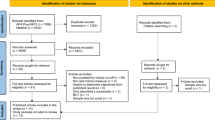
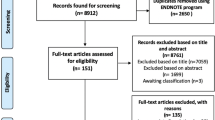
Study identification
Eligible projects for the larger systematic review were identified through several channels (see Moyer et al. 2009). Electronic databases (PsycINFO, PubMed, and Dissertation Abstracts International) were searched using applicable key terms for each database (the list of key terms is available from the authors upon request). The reference lists of included primary reports and of 94 prior reviews and meta-analyses were also examined. Descendancy searches were conducted on prior reviews (i.e., for subsequent articles that cited them), and journals (Psycho-Oncology, Journal of Clinical Oncology, Cancer, Journal of Psychosocial Oncology, European Journal of Cancer, and Cancer Nursing) were hand-searched. Approximately 12,200 reports were identified through electronic databases, and 327 through other channels. After initial inspection of all titles and abstracts, 1,002 potentially eligible reports were obtained and examined for inclusion, and 488 projects were included in the larger review.
The HADS was identified in 53 (11%) of those projects, out of which 27 (50.9%) provided usable data to be included in the analyses. Studies that were excluded administered a shortened HADS version (k = 1), reported no data on the measure (k = 9), reported no pre-intervention data (k = 3), reported insufficient data to compute intervention effect sizes (k = 6), did not report data separately for the subscales (k = 3), or reported data selectively only for one subscale despite administration of both subscales (k = 2). The STAI-S was identified in 77 (16%) projects, out of which 41 (53.2%) provided usable data. Twelve of these studies administered the STAI-T, as well. Excluded studies administered an abbreviated version (k = 2), used a modified timeframe in the instructions (k = 4), reported no data on the measure (k = 13), reported no pre-intervention data (k = 10), or provided insufficient data to compute effect sizes (k = 7).
Studies were both randomized controlled trials and single-group pre-post studies. One problem with the latter design is that, if pre-intervention distress moderates intervention effects, this can be an artifact of regression to the mean rather than the result of true moderation (Campbell and Kenny 1999; Finney 2008). Randomized control groups experimentally account for this. Because only 7 of the 41 STAI-S (and none for STAI-T) studies used a single-group pre-post design, we based the analyses on the 34 randomized controlled trials. Out of the 27 eligible HADS studies, 15 did not include a minimal or no-intervention control group, and 12 were randomized controlled trials. In light of this distribution, we retained all 27 trials to deliberately examine the influence of regression to the mean by comparing results across the design types.
Data abstraction
Coding of study characteristics
The mean baseline scores on the distress instruments were the primary moderator of interest. A weighted average was formed if pre-intervention scores were reported separately for experimental and control groups.
Intervention characteristics were also coded as alternative effect size moderators: whether or not interventions were specifically targeted at distressed patients was determined from the eligibility criteria. Type of intervention was coded as cognitive behavioral or non-cognitive behavioral (consisting of non-behavioral psychotherapy, educational, social support, complementary and alternative medicine techniques; coding each of these approaches separately would have rendered cell sizes too small for statistically meaningful comparison). Mode of intervention delivery was categorized into group-, individual-, or self-administered settings. Intervention dose was coded as brief (less than 4 sessions), intermediate (4–6 sessions), or long (more than 6 sessions); these categories were defined to achieve approximately equal numbers of studies in each category.
Patient characteristics were abstracted to determine potential correlates of pre-intervention distress. Demographic characteristics (mean age, percent female, percent married) and medical characteristics (percent with advanced/metastatic cancer, cancer type) were coded if available from the reports (see Table 1; descriptive information and results for individual studies are available from the authors). Additional patient characteristics (such as time since diagnosis and intervention site) were too infrequently reported to be included.
Coding of intervention effect sizes
Because the same measurement metric was used across studies (scale-point differences on the HADS and STAI subscales), intervention effect sizes were coded in an unstandardized format. To obtain the net intervention effect in randomized controlled trials, the mean change from baseline to follow-up in the control group was subtracted from the change in the intervention group. For six studies in which more than one intervention was compared with a no-treatment control, only the comparison of the most active treatment with the control group was included to avoid the possibility of misclassifying an active control groups as an intervention group. For one-group pre-post designs, effect sizes were calculated as the mean change from baseline to follow-up. For two studies in which different intervention groups were compared with each other, only the effect size for the most active group was included. When two or more treatment-groups were included but data was reported only for the combined groups, the data of the combined groups was used.
For studies assessing the HADS, effect sizes could be computed for both short-term (directly after the intervention) and for longer-term (Mdn = 3 months, range = 2–7 months post intervention) follow-up periods. For studies using the STAI, follow-up intervals were too heterogeneous to code separately; effect sizes were averaged in the case of multiple follow-ups to make use of all available outcome data.
Analytic strategy
We used multilevel modeling analysis (Bryk and Raudenbush 1992) to pool the results from individual study effect estimates. Meta-analysis can be readily conceptualized as a multi-level statistical problem, in that individual patients (level 1) are nested within studies (level 2). In a random effects meta-analysis, the unconditional (unmoderated) model can be expressed as
where y i represents the observed intervention effect of a study, μ is the average intervention effect, η i is the between study variance, and ε i is the within study sampling error.
This can be written more explicitly as a multilevel model in terms of
and
Study-level (level 2) predictors of effect sizes can be easily introduced as fixed effects to model conditional (moderated) intervention effects in mixed-effects “meta-regression” analyses.
Multilevel analyses were performed using the MIXED procedure in SAS (version 9.1 SAS Institute, Cary, NC, USA) and employing Full-Information Maximum Likelihood parameter estimation. Within-study variances were estimated assuming pre-post correlations of r = .70 (HADS), r = .50 (STAI-S), and r = .80 (STAI-T). Where standard deviations of outcome measures could not be discerned from reports, they were imputed using the pooled standard deviation from all other available studies in the same meta-analysis (Furukawa et al. 2006). The Q statistic (computed by summing the squared deviations of each study’s effect size from the average intervention effect) was used to test heterogeneity for statistical significance, and the I² statistic (which estimates what proportion of the between-study variance is due to actual differences rather than chance) was used to quantify the magnitude of heterogeneity, with values of 25, 50 and 75% representing low, medium, and high heterogeneity, respectively (Higgins et al. 2003). Effect size moderators were tested for statistical significance with Type III tests of fixed effects and based on standard normal distribution (van Houwelingen et al. 2002). The proportion of between-study variance that was explained by moderators was calculated as one minus the ratio of the residual variance in the conditional model to the variance in the unconditional model (Bryk and Raudenbush 1992).
Results
Hospital anxiety and depression scale (HADS)
Table 2 provides a summary of effects in the studies using the HADS-A and HADS-D.
Unconditional mean intervention effects
We first examined the unconditional mean intervention effects on HADS anxiety and depression. For HADS-A, the random-effects model showed a change of anxiety by −1.96 points (SE = 0.33, p < .0001) on the 22-point scale, indicating a medium effect size (Cohen’s d = .50). For HADS-D, the change was −1.32 points (SE = 0.25, p < .0001), representing a small to medium effect (d = .37). However, the studies varied substantially in their effects on HADS-A (Q = 239.65, df = 26, p < .0001, I 2 = 89.2) and HADS-D (Q = 206.55, df = 26, p < .0001, I 2 = 87.4). Thus, the examination of effect size moderators was warranted.
Pre-intervention distress as a moderator of intervention effects
When HADS-A pre-intervention scores were examined as a predictor of differential treatment effects, the regression slope was significant at −.53 (SE = .11, p < .0001); studies including patients with higher anxiety levels showed greater intervention effects. Pre-intervention scores explained 54.3% of the effect size variance. As shown in Fig. 1a, the efficacy of an intervention was estimated to be zero for a baseline anxiety score of 4.20. Significantly positive outcomes at p < .01 were predicted for baseline scores exceeding 5.85. At a baseline anxiety “caseness” cutoff score of 9, the intervention effect was −2.56 points, shifting patients approximately from the 75th to the 55th percentile on general population norms (Crawford et al. 2001).
Bubble plots of the relationships between pre-intervention scale scores and intervention effects. The size of the circle corresponds to the inverse variance of the effect size in that trial. Solid lines represent regression slopes, and dashed lines represent weighted grand mean pre-intervention scores and intervention effects. STAI spielberger state-trait anxiety inventory (possible range of scores = 20–80); HADS hospital anxiety and depression scale (possible range of scores = 0–21)
Similar results emerged for HADS-D pre-intervention scores as moderator of corresponding intervention effects. Studies including patients with higher depression levels yielded significantly greater effects (p < .0001), with a regression slope of −.48 (SE = .10). Pre-intervention scores explained 51.5% of the variance in treatment efficacy. As illustrated in Fig. 1b, zero intervention effect was estimated for a baseline depression score of 2.27. Significantly positive effects at p < .01 were predicted for scores exceeding 3.61. For a depression “caseness” score of 8, the intervention effect was −2.73 points, shifting patients approximately from the 90th to the 70th percentile on general population norms (Crawford et al. 2001).
Study characteristics as moderators of intervention effects
As shown in Table 2, effect sizes did not differ by type of intervention or the number of intervention sessions (dose). However, interventions specifically targeted at patients with elevated distress yielded greater effects than unselective interventions on both HADS-A scores (z = −2.39, p < .05) and HADS-D scores (z = −2.99, p < .01). Moreover, interventions provided in an individual setting showed greater effects than those in a group setting (z = −3.53, p < .001 for HADS-A; z = −2.80, p < .01 for HADS-D) and those in a self-administered setting (z = −2.43, p < .05 for HADS-A; z = −2.43, p < .05 for HADS-D). To determine whether these intervention characteristics would explain the moderating effect of pre-intervention distress levels, we tested multiple regression mixed-effects models in which intervention effects on either HADS subscale were predicted from all five moderator variables (i.e., pre-intervention distress, intervention targeted or not, intervention type, setting, and dose) simultaneously. In these models, pre-intervention distress remained the only significant moderator of intervention effects on both HADS-A (z = −2.82, p < .01) and HADS-D (z = −3.05, p < .01) scores, uniquely explaining 14.5% of the anxiety effects variance and 18.9% of the depression effects variance, respectively.
Influence of design type
Given that regression to the mean may favorably bias the estimated relationship between baseline scores and treatment effects in studies that lack a control group (Campbell and Kenny 1999), we compared the moderating effects of pre-intervention HADS scores on intervention outcomes by design type. The separate regression slopes remained significant for both randomized controlled trials (for HADS-A: slope = −.67, SE = .21, p < .01; for HADS-D: slope = −.40, SE = .15, p < .01) and single-group studies (for HADS-A: slope = −.47, SE = .13, p < .001; for HADS-D: slope = −.57, SE = .15, p < .0001), and did not significantly differ from one another (for HADS-A: z = −.81, p = .42; for HADS-D: z = .83, p = .41).
The multilevel modeling approach using the maximum likelihood function also allowed examination of meta-analytic models that adjusted for the missing control groups of single-group studies. To do this, we computed pre-post change scores separately for all intervention groups and all available control groups. We then fitted multivariate mixed-effects models in which these change scores were simultaneously predicted from pre-intervention HADS scores, such that the difference in regression slopes indicated the moderating effect of pre-intervention distress, with missing control groups estimated from the available data (Kalaian and Raudenbush 1996). Pre-post change in the control groups was negatively associated with baseline scores indicating regression to the mean (for HADS-A: slope = −.11, SE = .15, p = .49; for HADS-D: slope = −.29, SE = .14, p = .03). However, the differences in slopes showed adjusted moderating effects of pre-intervention scores that remained significant for HADS-A (slopes difference = −.45, SE = .18, p = .01) and HADS-D (slopes difference = −.34, SE = .14, p = .02).
Longer-term follow-up intervention effects
Longer-term follow-up results (2–7 months after the interventions) were available for 12 of the 27 studies. Multivariate mixed-effects models were examined to compare these longer-term effects with the immediate intervention effects presented above (with missing follow-up effects estimated from the available data). Pre-intervention distress scores significantly moderated longer-term intervention effects on HADS-A (slope = −.48, SE = .12, p < .0001) and HADS-D (slope = −.25, SE = .11, p = .03). The meta-regression slopes on immediate versus longer-term effects did not differ from one another for HADS-A (z = 0.55, p = .58). For HADS-D, however, the slope was significantly flattened at longer-term (z = 2.18, p = .03) relative to immediate effects: For a depression “caseness” score of 8, the intervention effect was still significant (raw effect = −1.79, SE = .38, p < .0001), but significantly weaker than those obtained immediately post intervention (z = 2.73, p < .01). There was no concomitant increase in intervention effect for lower levels of baseline depression (i.e., intervention effects remained non-significant at p > .01 for baseline HADS-D scores <3.42).
Correlates of pre-intervention distress
The final step in the HADS analyses was to examine potential correlates of pre-intervention distress levels. Across all studies, the inverse variance-weighted grand mean HADS-A score at study entry was 7.84 (SE = .42), and the mean HADS-D score was 5.08 (SE = .37), which places the patients approximately at the 70th percentile of general population norms for both scales (Crawford et al. 2001). However, as illustrated in Fig. 1, the variability between studies was substantial for HADS-A (Q = 488.29, df = 26, p < .0001, I 2 = 94.7) and HADS-D (Q = 551.54, df = 26, p < .0001, I 2 = 95.3).
As might be expected, higher pre-intervention scores were found in studies targeted at clinically distressed patients relative to other studies on HADS-A (z = 2.95, p < .01) and HADS-D (z = 3.03, p < .01); further analyses were controlled for this study inclusion criterion. No significant associations were found between pre-intervention scores and participant age, gender, marital status, or cancer type. However, distress systematically varied by cancer stage: HADS-D scores were significantly higher in studies with more patients in advanced/metastatic stages (z = 2.37, p < .05); the comparable trend was found for HADS-A scores (z = 1.65, p = .10).
Spielberger state-trait anxiety inventory (STAI)
Table 3 provides a summary of effects in studies using the STAI-T and STAI-S.
Unconditional mean intervention effects
Overall, the net intervention effect was small to medium on STAI-T scores (d = .36, raw effect = −3.75, SE = 1.11, p < .0001) and medium on STAI-S scores (d = .62, raw effect = −5.72, SE = 1.21, p < .0001). Heterogeneity was large and significant in the effects on STAI-T scores (Q = 45.67, df = 11, p < .0001, I 2 = 75.9) and on STAI-S scores (Q = 240.06, df = 33, p < .0001, I 2 = 86.3).
Pre-intervention distress as a moderator of intervention effects
Effects on trait anxiety were significantly moderated by pre-intervention STAI-T scores (slope = −.33, SE = .09, p < .001). However, Fig. 1c indicates two potential outliers with high STAI-T scores; when these were removed, the moderator effect was no longer significant (slope = −.10, SE = .17, p = .54).
Pre-intervention STAI-S scores significantly moderated corresponding intervention effects (slope = −.58, SE = .13, p < .0001); studies were more effective for patients with higher initial state anxiety. Baseline scores explained 43.1% of the variation in effect sizes. Zero intervention effect was predicted for a baseline score of 33.88 (Fig. 1d). Significantly positive outcomes at p < .01 were predicted for baseline scores exceeding 39.29. At a norm score of 49 for patients with anxiety reaction the net intervention effect was −8.76 scale-points, shifting patients approximately from the 85th to the 70th percentile on norms for healthy adults (Spielberger 1983).
Study characteristics as moderators of intervention effects
For STAI-T outcomes, group interventions were significantly more effective than individual (z = −4.42, p < .0001) and self-administered (z = −5.52, p < .0001) interventions. Virtually all of the true effect-size variance was explained by this factor, such that the moderating effect of pre-intervention distress was no longer significant when controlling for mode of delivery (z = 1.26, p > .20).
For STAI-S outcomes, interventions targeted at distressed patients showed greater effects than those that were not (z = −2.35, p < .05), and interventions involving more than 6 sessions were more effective than those with 4–6 sessions (z = −2.15, p < .05). However, when STAI-S intervention effects were predicted from pre-intervention scores and all alternative moderators (i.e., pre-intervention distress, intervention targeted or not, intervention type, setting, and dose) simultaneously, pre-intervention STAI-S scores showed the only significant moderating effect (z = −3.35, p < .001), uniquely explaining 21.4% of the anxiety effects variance.
Correlates of pre-intervention distress
Across all studies, the weighted mean STAI-T score at study entry was 40.95 (SE = 2.15), and the mean STAI-S score was 43.58 (SE = 1.23), which places the patients approximately at the 50th percentile on norms for general medical and surgical patients and at the 75th percentile for normal adults for both scales (Spielberger 1983). As shown in Fig. 1, the variability in baseline scores was substantial for STAI-T (Q = 455.02, df = 11, p < .0001, I 2 = 97.6) and STAI-S (Q = 1625.67, df = 33, p < .0001, I 2 = 98.0). Studies targeted at distressed patients showed higher pre-intervention STAI-S scores (z = 2.13, p < .05). Other patient characteristics were not significantly associated with baseline STAI scores.
Discussion
The results of this meta-analysis are largely consistent with the notion that effects of psychosocial interventions on anxiety and depression in cancer patients are conditional upon the patients’ initial distress levels. On average, intervention benefits were in the small to medium range, which coincides with previous meta-analytic findings in the field (Rehse and Pukrop 2003; Sheard and Maguire 1999; Tatrow and Montgomery 2006). However, the studies varied markedly in the magnitude of effect sizes, and distress levels at study entry explained sizeable proportions of this variability. In a linear fashion, the difference in therapeutic effects was up to 0.5 points for each point difference in initial anxiety and depression levels, such that the efficacy of interventions in reducing distress was negligible where initial distress was low and pronounced where initial distress was high.
This effect was quite robust across different measures of psychological distress: it was evident for both anxiety and depression outcomes in studies that administered the Hospital Anxiety and Depression Scale (HADS), and it replicated in a non-overlapping sample of studies assessing state-anxiety with the Spielberger State-Trait Anxiety Inventory (STAI). The results remained equivocal for changes in STAI trait-anxiety, suggesting the possibility that the moderating effect of pre-intervention distress is more pronounced for situational and possibly more cancer-specific aspects of distress than for characterological forms of distress. Study characteristics pertaining to intervention design and delivery that have been found to influence therapeutic benefits in previous meta-analyses (Sheard and Maguire 1999; Tatrow and Montgomery 2006; Zimmermann et al. 2007) also moderated effect size outcomes in the present analysis. However, patient distress levels at study entry uniquely explained differences in intervention efficacy when these features were held constant, and irrespective of whether or not interventions were purposely designed to address patients with elevated distress. This further raises confidence in the findings being meaningful and not the result of spurious relationships (Lipsey 2003). In addition, study selection criteria and empirical analyses suggested that the results were not an artifact of regression to the mean.
This meta-analysis differs from previous ones in that it was designed to investigate the specific hypothesis that pre-intervention distress moderates intervention efficacy in studies using the HADS or the STAI. Several limitations associated with this approach must be noted. The HADS and STAI were reported only in a subset of all studies in the field, and we did not contact study authors to obtain missing information, which may limit the conclusiveness of our findings. Although addressing both anxiety and depression, anxiety measures predominated in the analyses. The results may or may not generalize to other measures or to different aspects of well-being in cancer patients, such as quality of life or physical symptoms including pain and fatigue. Furthermore, in order to retain a sufficient body of research required for meta-regression analyses, we could not restrict the investigation exclusively to large-scale randomized controlled trials, and other high quality trials that did not administer the HADS or STAI could not be included.
Despite these limitations, the findings bear potentially important implications for understanding the differential utility of psychosocial interventions for reducing acute forms of distress, for preventing the initial onset of distress, and for preventing the recurrence of distress in individuals with cancer. Each of these aspects is discussed in turn.
In view of the threatening and chronically stressful experience of the cancer diagnosis and treatment, the conventional research strategy has been to provide psychosocial intervention unselectively to all patients in the hope that this may both alleviate acute distress and prevent emerging distress (Coyne et al. 2006; Sheard and Maguire 1999). Mirroring this notion, the studies included in the present analyses showed extensive variability in anxiety and depression levels at the outset of trials; differences across studies spanned 50% of the possible range on each scale. Those trials conducted with patients reporting significant depression and state-anxiety demonstrated strong and clinically meaningful effects. This is encouraging evidence for the efficacy of psychosocial interventions with respect to alleviating acute forms of distress in patients with cancer. On the other hand, a considerable number of studies were conducted with remarkably well-adjusted patients scoring even below healthy population norms. In such trials, a reduction of acute distress is clearly not indicated and nearly impossible statistically due to floor effects. These interventions may still prove beneficial for anxiety and depression if they serve a preventative function, such that distress levels increase in the control group and remain low in the experimental group. Our results indicated that initially well-adjusted control groups tended to regress toward the population mean. Other than this, however, the minuscule intervention effects found in these trials do not speak for their utility in preventing anxiety and depression.
In light of this evidence, should psychosocial intervention be limited to patients with acute distress and should efforts to prevent distress be dismissed? Well-adjusted patients may possibly benefit from treatment in ways not addressed in this review (e.g., by improving other aspects of quality of life). Moreover, a recent randomized controlled trial (Kissane et al. 2007) has demonstrated the potential prophylactic benefits of psychological intervention in preventing depressive disorders in cancer patients. The efficacy of distress prevention may be facilitated if programs are strategically tailored toward substantial risk-factors for distress rather than assuming that all patients are equally at risk. Our results showed more pronounced depression levels in studies with higher rates of patients with advanced cancer, replicating previous reports of heightened distress in patients with poorer prognosis (Brandberg et al. 1992; Harrison and Maguire 1994). However, information on stage of cancer was available only in a subset (55%) of the studies, which limits the conclusiveness of this finding, and no other demographic (age, gender, marital status) or medical (cancer type) variables were associated with pre-intervention distress. Other research has yielded mixed evidence for the role of demographic and medical characteristics in predicting distress among cancer patients (Osborne et al. 2003; van’t Spijker et al. 1997; Zabora et al. 2001). It is possible that these characteristics are too crude to identify patients at risk for elevated distress. Prospective research designs capable of following the dynamic interplay of personal and situational factors over time will be necessary to understand who is likely to develop significant distress at what point of the cancer treatment trajectory and who is not.
The prevention of recurrent emotional pathology and maintenance of positive intervention effects is as vital as primary distress prevention for optimal cancer care. Our analysis of longer-term follow-up effects on HADS outcomes showed no lagged preventive effects in studies involving initially well-adjusted patients, whereas interventions conducted with initially distressed patients evidenced sustained benefits for anxiety and depression. However, the longer-term benefits for samples with initially high depression were significantly less pronounced than immediate post-intervention effects, suggesting that these patients were likely to return to their problematic emotional condition in the long-run. Thus, what appears to be true for successful intervention in general may similarly hold for attempts to increase the durability of intervention effects such as booster or maintenance sessions: patients with high distress at study entry may benefit the most. As intuitively appealing as this notion is, the differential efficacy of strategies to prevent the recurrence of distress in cancer patients remains to be tested empirically.
Conclusions
Successful implementation of psychosocial care as an integral part of medical oncology requires that intervention strategies be maximally effective while minimizing costs and reducing the burden to cancer patients. Short instruments such as the HADS and STAI are cost-effective screening tools (Carlson and Bultz 2003), and even ultra-short measures like a single-item Distress Thermometer have been found useful for distress screening in cancer (Mitchell 2007). Consensus-based guidelines as those by the Distress Management Panel of the National Comprehensive Cancer Network (2008) recommend routine screening and selective referral based on patients’ distress levels. However, it has been noted that such practice is not widely adopted, and there is a need for strong empirical evidence that this would likely result in meaningfully improved cancer care (Jacobsen 2007; Keller et al. 2004). Our results are encouraging in this respect. In future research, it will be important to dismantle the specific treatment ingredients that render psychosocial intervention for patients with elevated distress levels most beneficial. In addition, effectiveness trials will be necessary to establish whether screening and selective intervention are feasible, accepted by patients, and can be successfully adapted in routine clinic settings. Such evidence may be critical to ensure optimal provision of psychosocial care for cancer patients and their individual needs.
References
Note: * References in HADS meta-analysis; ** references in STAI meta-analysis
*Adamsen, L., Midtgaard, J., Rorth, M., Borregaard, N., Andersen, C., Quist, M., et al. (2003). Feasibility, physical capacity, and health benefits of a multidimensional exercise program for cancer patients undergoing chemotherapy. Supportive Care in Cancer, 11, 707–716.
**Ahles, T. A., Tope, D. M., Pinkson, B., Walch, S., Hann, D., Whedon, M., et al. (1999). Massage therapy for patients undergoing autologous bone marrow transplantation. Journal of Pain and Symptom Management, 18, 157–163.
**Ali, N. S., & Khalil, H. Z. (1989). Effect of psychoeducational intervention on anxiety among Egyptian bladder cancer patients. Cancer Nursing, 12, 236–242.
*Allison, P. J., Nicolau, B., Edgar, L., Archer, J., Black, M., & Hier, M. (2004). Teaching head and neck cancer patients coping strategies: Results of a feasibility study. Oral Oncology, 40, 538–544.
*Ambler, N., Rumsey, N., Harcourt, D., Khan, F., Cawthorn, S., & Barker, J. (1999). Specialist nurse counsellor interventions at the time of diagnosis of breast cancer: Comparing ‘advocacy’ with a conventional approach. Journal of Advanced Nursing, 29, 445–453.
Andersen, B. L., Farrar, W. B., Golden-Kreutz, D. M., Glaser, R., Emery, C. F., Crespin, T. R., et al. (2004). Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. Journal of Clinical Oncology, 22, 3570–3580.
Antoni, M. H., Lehman, J. M., Kilbourn, K. M., Boyers, A. E., Culver, J. L., Alferi, S. M., et al. (2001). Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology, 20, 20–32.
**Arakawa, S. (1997). Relaxation to reduce nausea, vomiting, and anxiety induced by chemotherapy in Japanese patients. Cancer Nursing, 20, 342–349.
Barnes, L. L. B., Harp, D., & Jung, W. S. (2002). Reliability generalization of scores on the Spielberger State-Trait Anxiety Inventory. Educational and Psychological Measurement, 62, 603–618.
Bjelland, I., Dahl, A. A., Haug, T. T., & Neckelmann, D. (2002). The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research, 52, 69–77.
Boesen, E. H., Ross, L., Frederiksen, K., Thomsen, B. L., Dahlstrom, K., Schmidt, G., et al. (2005). Psychoeducational intervention for patients with cutaneous malignant melanoma: A replication study. Journal of Clinical Oncology, 23, 1270–1277.
Brandberg, Y., Bolund, C., Sigurdardottir, V., Sjoden, P.-O., & Sullivan, M. (1992). Anxiety and depressive symptoms at different stages of malignant melanoma. Psycho-Oncology, 1, 71–78.
Bryk, A. S., & Raudenbush, S. W. (1992). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications.
*Burton, M. V., & Parker, R. W. (1995). A randomized control trial of preoperative psychology preparation for mastectomy. Psycho-Oncology, 4, 1–19.
Campbell, D. T., & Kenny, D. A. (1999). A primer on regression artifacts. New York, NY: Guilford Press.
Carey, M. P., & Burish, T. G. (1985). Anxiety as a predictor of behavioral therapy outcome for cancer chemotherapy patients. Journal of Consulting and Clinical Psychology, 53, 860–865.
Carlson, L. E., & Bultz, B. D. (2003). Cancer distress screening. Needs, models, and methods. Journal of Psychosomatic Research, 55, 403–409.
Carmack Taylor, C. L., de Moor, C., Basen-Engquist, K., Smith, M. A., Dunn, A. L., Badr, H., et al. (2007). Moderator analyses of participants in the active for life after cancer trial: Implications for physical activity group intervention studies. Annals of Behavioral Medicine, 33, 99–104.
**Cartledge Hoff, A., & Haaga, D. A. F. (2005). Effects of an education program on radiation oncology patients and families. Journal of Psychosocial Oncology, 23, 61–79.
**Carty, J. L. (1990). Relaxation with imagery: An adjunctive treatment for anticipatory nausea and/or vomiting (Doctoral dissertation, The Catholic University of America, 1990). Dissertation Abstracts International, 51, 131.
**Cheung, Y. L., Molassiotis, A., & Chang, A. M. (2003). The effect of progressive muscle relaxation training on anxiety and quality of life after stoma surgery in colorectal cancer patients. Psycho-Oncology, 12, 254–266.
**Cohen, L., Warneke, C., Fouladi, R. T., Rodriguez, M. A., & Chaoul-Reich, A. (2004). Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer, 100, 2253–2260.
Coyne, J. C., Lepore, S. J., & Palmer, S. C. (2006). Efficacy of psychosocial interventions in cancer care: Evidence is weaker than it first looks. Annals of Behavioral Medicine, 32, 104–110.
Crawford, J. R., Henry, J. D., Crombie, C., & Taylor, E. P. (2001). Normative data for the HADS from a large non-clinical sample. British Journal of Clinical Psychology, 40, 429–434.
*Cull, A., Stewart, M., & Altman, D. G. (1995). Assessment of and intervention for psychosocial problems in routine oncology practice. British Journal of Cancer, 72, 229–235.
*Davidson, J. R., Waisberg, J. L., Brundage, M. D., & MacLean, A. W. (2001). Nonpharmacologic group treatment of insomnia: A preliminary study with cancer survivors. Psycho-Oncology, 10, 389–397.
**Davison, B. J., & Degner, L. F. (1997). Empowerment of men newly diagnosed with prostate cancer. Cancer Nursing, 20, 187–196.
**Dobkin, P. L. (1987). The use of systematic desensitization, a biobehavioral intervention, in the reduction of aversive chemotherapy side effects in cancer patients (Doctoral dissertation, University of Georgia, 1987). Dissertation Abstracts International, 48, 163.
**Dodd, M. J. (1987). Efficacy of proactive information on self-care in radiation therapy patients. Heart and Lung, 16, 538–544.
**Dodd, M. J. (1988). Efficacy of proactive information on self-care in chemotherapy patients. Patient Education and Counseling, 11, 215–225.
Doorenbos, A., Given, B., Given, C., & Verbitsky, N. (2006). Physical functioning: Effect of behavioral intervention for symptoms among individuals with cancer. Nursing Research, 55, 161–171.
**Elsesser, K., Van Berkel, M., Sartory, G., Biermann-Göcke, W., et al. (1994). The effects of anxiety management training on psychological variables and immune parameters in cancer patients: A pilot study. Behavioural & Cognitive Psychotherapy, 22, 13–23.
**Feldman, C. S. (1989). The role of imagery in the hypnotic treatment of adverse reactions to cancer chemotherapy (Doctoral dissertation, University of South Carolina, 1989). Dissertation Abstracts International, 50, 4216–4217.
Finney, J. W. (2008). Regression to the mean in substance use disorder treatment research. Addiction, 103, 42–52.
*Fukui, S., Kugaya, A., Okamura, H., Kamiya, M., Koike, M., Nakanishi, T., et al. (2000). A psychosocial group intervention for Japanese women with primary breast carcinoma. Cancer, 89, 1026–1036.
Furukawa, T. A., Barbui, C., Cipriani, A., Brambilla, P., & Watanabe, N. (2006). Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology, 59, 7–10.
**Gaston-Johansson, F., Fall-Dickson, J. M., Nanda, J., Ohly, K. V., Stillman, S., Krumm, S., et al. (2000). The effectiveness of the comprehensive coping strategy program on clinical outcomes in breast cancer autologous bone marrow transplantation. Cancer Nursing, 23, 277–285.
Given, C., Given, B., Rahbar, M., Jeon, S., McCorkle, R., Cimprich, B., et al. (2004). Effect of a cognitive behavioral intervention on reducing symptom severity during chemotherapy. Journal of Clinical Oncology, 22, 507–516.
Goodwin, P. J., Leszcz, M., Ennis, M., Koopmans, J., Vincent, L., Guther, H., et al. (2001). The effect of group psychosocial support on survival in metastatic breast cancer. New England Journal of Medicine, 345, 1719–1726.
*Greer, S., Moorey, S., & Baruch, J. (1991). Evaluation of adjuvant psychological therapy for clinically referred cancer patients. British Journal of Cancer, 63, 257–260.
*Greer, S., Moorey, S., Baruch, J. D., Watson, M., Robertson, B. M., Mason, A., et al. (1992). Adjuvant psychological therapy for patients with cancer: A prospective randomised trial. BMJ, 304, 675–680.
**Hagopian, G. A., & Rubenstein, J. H. (1990). Effects of telephone call interventions on patients’ well-being in a radiation therapy department. Cancer Nursing, 13, 339–344.
Harrison, J., & Maguire, P. (1994). Predictors of psychiatric morbidity in cancer patients. British Journal of Psychiatry, 165, 593–598.
Helgeson, V. S., Lepore, S. J., & Eton, D. T. (2006). Moderators of the benefits of psychoeducational interventions for men with prostate cancer. Health Psychology, 25, 348–354.
*Hidderley, M., & Holt, M. (2004). A pilot randomized trial assessing the effects of autogenic training in early stage cancer patients in relation to psychological status and immune system responses. European Journal of Oncology Nursing, 8, 61–65.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327, 557–560.
Hosaka, T., Sugiyama, Y., Tokuda, Y., & Okuyama, T. (2000). Persistent effects of a structured psychiatric intervention on breast cancer patients’ emotions. Psychiatry and Clinical Neurosciences, 54, 559–563.
Jacobsen, P. B. (2007). Screening for psychological distress in cancer patients: Challenges and opportunities. Journal of Clinical Oncology, 25, 4526–4527.
Kalaian, H. A., & Raudenbush, S. W. (1996). A multivariate mixed linear model for meta-analysis. Psychological Methods, 1, 227–235.
Keller, M., Sommerfeldt, S., Fischer, C., Knight, L., Riesbeck, M., Lowe, B., et al. (2004). Recognition of distress and psychiatric morbidity in cancer patients: A multi-method approach. Annals of Oncology, 15, 1243–1249.
**Kim, S. D., & Kim, H. S. (2005). Effects of a relaxation breathing exercise on anxiety, depression, and leukocyte in hemopoietic stem cell transplantation patients. Cancer Nursing, 28, 79–83.
King, A. C., Ahn, D. F., Atienza, A. A., & Kraemer, H. C. (2008). Exploring refinements in targeted behavioral medicine intervention to advance public health. Annals of Behavioral Medicine, 35, 251–260.
*Kissane, D. W., Bloch, S., Smith, G. C., Miach, P., Clarke, D. M., Ikin, J., et al. (2003). Cognitive-existential group psychotherapy for women with primary breast cancer: A randomised controlled trial. Psycho-Oncology, 12, 532–546.
Kissane, D. W., Grabsch, B., Clarke, D. M., Smith, G. C., Love, A. W., Bloch, S., et al. (2007). Supportive-expressive group therapy for women with metastatic breast cancer: Survival and psychosocial outcome from a randomized controlled trial. Psycho-Oncology, 16, 277–286.
*Kite, S. M., Maher, E. J., Anderson, K., Young, T., Young, J., Wood, J., et al. (1998). Development of an aromatherapy service at a cancer centre. Palliative Medicine, 12, 171–180.
**Kwekkeboom, K. L. (2003). Music versus distraction for procedural pain and anxiety in patients with cancer. Oncology Nursing Forum, 30, 433–440.
Lepore, S. J., & Coyne, J. C. (2006). Psychological interventions for distress in cancer patients: A review of reviews. Annals of Behavioral Medicine, 32, 85–92.
**Lin, M. L., Tsang, Y. M., & Hwang, S. L. (1998). Efficacy of a stress management program for patients with hepatocellular carcinoma receiving transcatheter arterial embolization. Journal of the Formosan Medical Association, 97, 113–117.
*Lindemalm, C., Strang, P., & Lekander, M. (2005). Support group for cancer patients. Does it improve their physical and psychological wellbeing? A pilot study. Supportive Care in Cancer, 13, 652–657.
*Liossi, C., & White, P. (2001). Efficacy of clinical hypnosis in the enhancement of quality of life of terminally ill cancer patients. Contemporary Hypnosis, 18, 145–160.
Lipsey, M. W. (2003). Those confounded moderators in meta-analysis: Good, bad, and ugly. Annals of the American Academy of Political and Social Science, 587, 69–81.
**Mantovani, G., Astara, G., Lampis, B., Bianchi, A., Curreli, L., Orru, W., et al. (1996). Evaluation by multidimensional instruments of health-related quality of life of elderly cancer patients undergoing three different “psychosocial” treatment approaches. A randomized clinical trial. Supportive Care in Cancer, 4, 129–140.
**McQuellon, R. P., Wells, M., Hoffman, S., Craven, B., Russell, G., Cruz, J., et al. (1998). Reducing distress in cancer patients with an orientation program. Psycho-Oncology, 7, 207–217.
Meyer, T. J., & Mark, M. M. (1995). Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychology, 14, 101–108.
*Midtgaard, J., Rorth, M., Stelter, R., Tveteras, A., Andersen, C., Quist, M., et al. (2005). The impact of a multidimensional exercise program on self-reported anxiety and depression in cancer patients undergoing chemotherapy: A phase II study. Palliative and Supportive Care, 3, 197–208.
Mitchell, A. J. (2007). Pooled results from 38 analyses of the accuracy of distress thermometer and other ultra-short methods of detecting cancer-related mood disorders. Journal of Clinical Oncology, 25, 4670–4681.
**Miyashita, M. (2005). A randomized intervention study for breast cancer survivors in Japan: Effects of short-term support group focused on possible breast cancer recurrence. Cancer Nursing, 28, 70–78.
*Montazeri, A., Jarvandi, S., Haghighat, S., Vahdani, M., Sajadian, A., Ebrahimi, M., et al. (2001). Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Education and Counseling, 45, 195–198.
*Moorey, S., Greer, S., Bliss, J., & Law, M. (1998). A comparison of adjuvant psychological therapy and supportive counselling in patients with cancer. Psycho-Oncology, 7, 218–228.
**Morrow, G. R. (1986). Effect of the cognitive hierarchy in the systematic desensitization treatment of anticipatory nausea in cancer patients: A component comparison with relaxation only, counseling, and no treatment. Cognitive Therapy and Research, 10, 421–446.
Moyer, A., Sohl, S. J., Knapp-Oliver, S. K., & Schneider, S. (2009). Characteristics and methodological quality of 25 years of research investigating psychosocial interventions for cancer patients. Cancer Treatment Reviews, 35, 475–484.
*Moynihan, C., Bliss, J. M., Davidson, J., Burchell, L., & Horwich, A. (1998). Evaluation of adjuvant psychological therapy in patients with testicular cancer: Randomised controlled trial. BMJ, 316, 429–435.
National Comprehensive Cancer Network (2008). NCCN clinical practice guidelines in oncology: Distress management—v.1.2008. National Comprehensive Cancer Network. Available from http://www.nccn.org.
Newell, S. A., Sanson-Fisher, R. W., & Savolainen, N. J. (2002). Systematic review of psychological therapies for cancer patients: Overview and recommendations for future research. Journal of the National Cancer Institute, 94, 558–584.
Osborne, R. H., Elsworth, G. R., & Hopper, J. L. (2003). Age-specific norms and determinants of anxiety and depression in 731 women with breast cancer recruited through a population-based cancer registry. European Journal of Cancer, 39, 755–762.
**Palekar, I. S. (1994). Effect of autogenic relaxation with imagery on chemotherapy side effects, as predicted by personality characteristics (Doctoral dissertation, The University of Akron, 1994). Dissertation Abstracts International, 56, 311.
**Poroch, D. (1995). The effect of preparatory patient education on the anxiety and satisfaction of cancer patients receiving radiation therapy. Cancer Nursing, 18, 206–214.
**Prince, B. J. (1995). Hospitalized, post-mastectomy coping modification and anxiety reduction (Doctoral dissertation, Yeshiva University, 1995). Dissertation Abstracts International, 56, 117.
**Rash, J. L. (1991). The use of guided mental imagery in its effect on anxiety and depression in the cancer patient (Doctoral dissertation, United States International University, 1991). Dissertation Abstracts International, 52, 154.
**Rawl, S. M., Given, B. A., Given, C. W., Champion, V. L., Kozachik, S. L., Barton, D., et al. (2002). Intervention to improve psychological functioning for newly diagnosed patients with cancer. Oncology Nursing Forum, 29, 967–975.
Rehse, B., & Pukrop, R. (2003). Effects of psychosocial interventions on quality of life in adult cancer patients: Meta analysis of 37 published controlled outcome studies. Patient Education and Counseling, 50, 179–186.
**Sabo, C. E., & Michael, S. R. (1996). The influence of personal message with music on anxiety and side effects associated with chemotherapy. Cancer Nursing, 19, 283–289.
*Savard, J., Simard, S., Ivers, H., & Morin, C. M. (2005). Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. Journal of Clinical Oncology, 23, 6083–6096.
Scheier, M. F., Helgeson, V. S., Schulz, R., Colvin, S., Berga, S. L., Knapp, J., et al. (2007). Moderators of interventions designed to enhance physical and psychological functioning among younger women with early-stage breast cancer. Journal of Clinical Oncology, 25, 5710–5714.
Sheard, T., & Maguire, P. (1999). The effect of psychological interventions on anxiety and depression in cancer patients: Results of two meta-analyses. British Journal of Cancer, 80, 1770–1780.
**Smith, M., Casey, L., Johnson, D., Gwede, C., & Riggin, O. Z. (2001). Music as a therapeutic intervention for anxiety in patients receiving radiation therapy. Oncology Nursing Forum, 28, 855–862.
*Spiegel, D., Morrow, G. R., Classen, C., Raubertas, R., Stott, P. B., Mudaliar, N., et al. (1999). Group psychotherapy for recently diagnosed breast cancer patients: A multicenter feasibility study. Psycho-Oncology, 8, 482–493.
Spielberger, C. D. (1983). Manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press.
**Stalpers, L. J., da Costa, H. C., Merbis, M. A., Fortuin, A. A., Muller, M. J., & van Dam, F. S. (2005). Hypnotherapy in radiotherapy patients: A randomized trial. International Journal of Radiation Oncology, Biology, Physics, 61, 499–506.
Stanton, A. L. (2005). How and for whom? Asking questions about the utility of psychosocial interventions for individuals diagnosed with cancer. Journal of Clinical Oncology, 23, 4818–4820.
Stark, D., Kiley, M., Smith, A., Velikova, G., House, A., & Selby, P. (2002). Anxiety disorders in cancer patients: Their nature, associations, and relation to quality of life. Journal of Clinical Oncology, 20, 3137–3148.
Stefanek, M. E., Jacobsen, P. B., & Christensen, A. J. (2006). The society of behavioral medicine’s “great debate”: An introduction. Annals of Behavioral Medicine, 32, 83–84.
*Strauss-Blasche, G., Gnad, E., Ekmekcioglu, C., Hladschik, B., & Marktl, W. (2005). Combined inpatient rehabilitation and spa therapy for breast cancer patients: Effects on quality of life and CA 15-3. Cancer Nursing, 28, 390–398.
Tatrow, K., & Montgomery, G. H. (2006). Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: A meta-analysis. Journal of Behavioral Medicine, 29, 17–27.
*Tattersall, M. H., Butow, P. N., Griffin, A. M., & Dunn, S. M. (1994). The take-home message: Patients prefer consultation audiotapes to summary letters. Journal of Clinical Oncology, 12, 1305–1311.
Taylor, K. L., Lamdan, R. M., Siegel, J. E., Shelby, R., Moran-Klimi, K., & Hrywna, M. (2003). Psychological adjustment among African American breast cancer patients: One-year follow-up results of a randomized psychoeducational group intervention. Health Psychology, 22, 316–323.
*Thomas, R., Daly, M., Perryman, B., & Stockton, D. (2000). Forewarned is forearmed—Benefits of preparatory information on video cassette for patients receiving chemotherapy or radiotherapy—A randomised controlled trial. European Journal of Cancer, 36, 1536–1543.
*Thorsen, L., Skovlund, E., Stromme, S. B., Hornslien, K., Dahl, A. A., & Fossa, S. D. (2005). Effectiveness of physical activity on cardiorespiratory fitness and health-related quality of life in young and middle-aged cancer patients shortly after chemotherapy. Journal of Clinical Oncology, 23, 2378–2388.
**Trask, P. C., Paterson, A. G., Griffith, K. A., Riba, M. B., & Schwartz, J. L. (2003). Cognitive-behavioral intervention for distress in patients with melanoma: Comparison with standard medical care and impact on quality of life. Cancer, 98, 854–864.
van Houwelingen, H. C., Arends, L. R., & Stijnen, T. (2002). Advanced methods in meta-analysis: Multivariate approach and meta-regression. Statistics in Medicine, 21, 589–624.
van’t Spijker, A., Trijsburg, R. W., & Duivenvoorden, H. J. (1997). Psychological sequelae of cancer diagnosis: A meta-analytical review of 58 studies after 1980. Psychosomatic Medicine, 59, 280–293.
*Walker, L. G., Walker, M. B., Ogston, K., Heys, S. D., Ah-See, A. K., Miller, I. D., et al. (1999). Psychological, clinical and pathological effects of relaxation training and guided imagery during primary chemotherapy. British Journal of Cancer, 80, 262–268.
*Watson, M., Fenlon, D., McVey, G., & Fernandez-Marcos, M. (1996). A support group for breast cancer patients: Development of a cognitive-behavioural approach. Behavioural and Cognitive Psychotherapy, 24, 73–81.
**Williams, S. A., & Schreier, A. M. (2004). The effect of education in managing side effects in women receiving chemotherapy for treatment of breast cancer. Oncology Nursing Forum, 31, E16–E23.
**Winzelberg, A. J., Classen, C., Alpers, G. W., Roberts, H., Koopman, C., Adams, R. E., et al. (2003). Evaluation of an internet support group for women with primary breast cancer. Cancer, 97, 1164–1173.
**Wyatt, G. K., Donze, L. F., & Beckrow, K. C. (2004). Efficacy of an in-home nursing intervention following short-stay breast cancer surgery. Research in Nursing and Health, 27, 322–331.
*Yates, P., Edwards, H., Nash, R., Aranda, S., Purdie, D., Najman, J., et al. (2004). A randomized controlled trial of a nurse-administered educational intervention for improving cancer pain management in ambulatory settings. Patient Education and Counseling, 53, 227–237.
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C., & Piantadosi, S. (2001). The prevalence of psychological distress by cancer site. Psycho-Oncology, 10, 19–28.
Zigmond, A. S., & Snaith, R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67, 361–370.
Zimmermann, T., Heinrichs, N., & Baucom, D. H. (2007). “Does one size fit all?” moderators in psychosocial interventions for breast cancer patients: A meta-analysis. Annals of Behavioral Medicine, 34, 225–239.
Acknowledgments
Preparation of this manuscript was supported by a grant from the National Cancer Institute (R01 CA100810) to Anne Moyer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schneider, S., Moyer, A., Knapp-Oliver, S. et al. Pre-intervention distress moderates the efficacy of psychosocial treatment for cancer patients: a meta-analysis. J Behav Med 33, 1–14 (2010). https://doi.org/10.1007/s10865-009-9227-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-009-9227-2