Abstract
In order to evaluate a structured support intervention programme, symptoms and quality of life (QOL) were studied in 61 consecutive cancer patients with different tumour diagnoses in relation to intervention and follow-up. The majority of the patients were female. The Edmonton symptom assessment scale (ESAS), the Norwegian fatigue questionnaire and the hospital anxiety and depression scale (HADS) were used. Data were analysed according to ANOVA and Tukey’s honest significant difference (HSD) test. ESAS sickness score (P=0.0001), depression (P=0.0001), anxiety (P=0.0001) and QOL (P=0.0009) improved and the improvements in depression and anxiety were still significant after 3 months (P=0.02 respectively). Aspects of fatigue also improved significantly in 7 of 11 questions after the intervention (P≤0.04) but these improvements were not observed after 3 months. Anxiety according to the HADS questionnaire improved significantly after the intervention (P=0.0006). The majority of the patients highly appreciated the possibility of sharing thoughts and troubles with others with similar experiences (59%). The programme was therefore found to improve QOL, and physical and psychological functions. Randomized studies in relation to immunological changes and follow-up are in progress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most people react to a diagnosis of cancer with psychological distress and exhibit both physical and psychological symptoms such as fatigue, anxiety and depression [31–33], and experience a reduced quality of life (QOL) [2, 9, 11, 37]. However, social support, educational programmes and exercise can modify psychosocial and physiological stress [5, 6, 10, 19, 20, 34, 36, 37], improve QOL [9, 18–20, 37] and perhaps even influence recurrence and survival [13].
Support groups also seem to offer cost-effective help to cancer patients [6] and even support to the partners of cancer patients has led to important effects on the patient [8]. Fatigue, defined as an unusual sense of tiredness affecting both physical and mental capacity which is unrelieved by rest, is a multidimensional symptom increasingly recognized in cancer patients [24, 43, 44]. Fatigue affects between 33% and 99% of cancer patients depending on study group, assessment instruments, treatment and time of testing [12, 41–44]. In addition fatigue has shown to be persistent long after the treatment is completed [12]. Cancer patients suffer from substantial fatigue as compared to healthy controls [3].
However, this symptom complex has been shown to improve after intervention [3, 12, 37, 39, 45]. An improved understanding of the cooperation between the brain, and the immune and neuroendocrine systems also further indicates the possible relevance of psychosocial wellbeing to objective health symptoms [1, 14, 26, 27, 38, 46]. Meta-analytic reviews suggest that different forms of stress are associated with negative immune responses [21, 22]. Thus, stress has been linked to changed immune functions and herpes virus latency [15] and depression has also been linked to immunity [22]. Such relationships have also been shown for healthy caregivers of spouses with Alzheimer disease [24], patients with AIDS [4] and cancer patients [30]. However, definite conclusions are hard to draw from interventions aimed at promoting the support and rehabilitation of cancer patients because of sometimes small study groups, differences in diagnosis, applied intervention schemes and type of therapy (individual versus group) [13, 14].
The aim of the present study was to evaluate a 7+4-day rehabilitation programme in terms of its effect on patient psychological and physiological functions, and the duration of any putative effect.
Material and methods
Support group programme
The rehabilitation intervention ran from Sunday to Saturday on a residential basis followed by a 4-day follow-up 2 months after the initial visit. The members of the team were oncologists (n=4), social workers (n=2), art therapists (n=2), masseuses (n=2), and a person trained in qi-gong and mental visualization (n=1). All personnel had several years of occupational experience and trained according to the method of Grahn [17]. During the intervention period the guests received information about cancer illnesses, aetiology, risk factors, treatments, psychological effects and coping mechanisms. Physical exercise, relaxation training, qi-gong and nonverbal communication (art therapy) were mixed with theoretical educational lectures. Social activities such as concerts, visits to museums and restaurants were provided as were opportunities for the guests to be together with individuals with similar experiences in beautiful and restful surroundings.
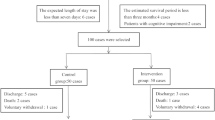
Participants
The protocols were completed by 59 consecutive patients (57 women and 2 men) with a median age of 53 years (range 29–81 years). The patients were suffering from mammary cancer (61%), gynaecological cancer (20%) and gastrointestinal cancer (9%), and the remaining 10% were suffering from CNS tumours, lymphoma or pulmonary cancer. The median time from end of treatment to intervention was 1.2 years (range 6 months to 3 years). Assessments were first made before the start of the support programme. They were then repeated at the end of the residential week and 3, 6 and 12 months after the intervention.
Controls
Nine healthy individuals (eight women and one man) with a median age of 59 years completed the same questions once in parallel with the first group of patients.
Questionnaires
Physical and psychological symptoms and QOL were measured using the Edmonton symptom assessment scale (ESAS) [7]. The questionnaire consists of nine visual analogue scales (VAS) for nine different symptoms where 0 is absence of symptom and 10 the worst imaginable symptom. The symptoms are pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, dyspnoea and wellbeing. The sum of all symptoms, measured in centimetres, gives a total sickness score. In addition, QOL was measured by on a VAS where the worst possible QOL was 10 and the optimal QOL was 0.
Anxiety and depression were measured using the hospital anxiety and depression scale (HADS) [47] which was designed to screen for anxiety and depression in a hospital setting. Seven items add up to an anxiety subscale, and seven items to a depression subscale. Each item is rated on a four-point scale (0, less than before; 1, not so much; 2, quite a lot; 3, very much), giving a maximum subscale scores of 21 each for depression and anxiety. Scores of more than 10 on either subscale are supposed to indicate clinical depression or anxiety, whilst subscale scores in the range of 8–10 represent borderline depression or anxiety.
Fatigue was assessed using the Norwegian fatigue questionnaire, a self-reporting instrument that consists of four response alternatives to 11 symptoms experienced during the most recent period of time as compared to how the patient felt when last feeling well. The issues were feeling tired, the need for more rest, feeling drowsy, problems with starting things, lack of energy, reduced muscle strength, feeling frail, problems concentrating, losing the thread when speaking to people, difficulty finding the right word, and subjective memory problems. The fatigue questionnaire measures physical fatigue (PF, four items) and mental fatigue (MF, seven items), and all 11 items together represent total fatigue (TF).
Statistics
Data were analysed by repeated measurements, using analysis of variance (ANOVA). Significant main effects were followed by Tukey’s honest significant difference (HSD) test.
Results
ESAS
The scores for all symptoms in the ESAS questionnaire had decreased on day 7 as compared to day 0, and were higher for the patients on day 0 than for the ten healthy controls (data not shown). The overall mean values and SD and the results of the ANOVA are shown in Table 1.
QOL, and depression, anxiety and sickness scores were significantly improved on day 7 compared to day 0, but at 3 months only depression and anxiety just reached statistical significance. No effect could be seen at 6 and 12 months.
HADS
The mean values for anxiety and depression improved after the support intervention but only the HADS anxiety score reached statistical significance according to the ANOVA and Turkey HSD (Table 2). The effects were not statistically significant at 6 and 12 months. However, 61% of the patients had an anxiety score of more than 8 on day 1, but had an anxiety score of more than 8 at 12 months. For the depression scores the corresponding percentages were 30% on day 1 and 21% at 12 months (data not shown). Thus, there were numerical but not statistically significant changes.
Fatigue
Significant changes were shown in the different items of the fatigue questionnaire. Less fatigue was observed in 7 of 11 questions and a borderline trend was noted in one additional item after the intervention as compared to day 0, but not after 3, 6 or 12 months. The items with significant changes were question 1—feeling tired (P=0.00001), question 2—need for rest (P=0.00001), question 3—feeling drowsy (P=0.03), question 5—lack of energy (P=0.0009), question 6—lack of muscular strength (P=0.005), question 7—feeling frail (P=0.002), question 8—problems with concentration (P=0.07), and question 11—subjective memory problems (P=0.002) (Table 3). Physical and mental fatigue reached statistically significant improvement after the intervention but remained significant at 3 months for physical fatigue only (Table 4).
Discussion
As compared to healthy controls the patients had high sickness scores, poorer QOL and more pronounced symptoms of anxiety and depression as measured by the ESAS questionnaire, and also higher anxiety and depression score according to the HADS questionnaire and more symptoms of fatigue. A general improvement was observed in subjective symptoms, with significantly lower levels of sickness, anxiety and fatigue. The support group intervention was highly appreciated by the patients (59%) giving them the opportunity to share thoughts and troubles with individuals with the same experience. The results indicate that the present intervention had beneficial effects on various psychosocial variables in cancer patients. However, most parameters in the present study showed short-term changes, with a decline in the effects after 3 months. Several studies on support groups in the Stanford Cancer Supportive Care Program [37] have suggested that a multimodal programme could contribute to improved wellbeing, reduced stress, increased Karnofsky score, more restful sleep, and increased energy. Reduction of anxiety and depression after participation in a support programme has also been reported by Montazeri et al. [36]. There could be several reasons why our study had a less long-lasting effect. The standard deviations were sometimes wide which may be explained by the fact that the participants had different tumours with very different treatments and prognoses. A considerable number of the patients were in advanced stages and had progressive disease as evident from the number of patients (n=9) who died during the observation period. Moreover, the number of participating subjects was also rather limited.
Different questionnaires can give different indications, as shown in the present study in which anxiety and depression as measured by the ESAS, but not by the HADS, showed significant improvement which remained after 3 months. The HADS questionnaire might have greater power in patients with stable disease as shown in the study by Ibbotson et al. [23], which is a drawback in studies such as ours in which nine patients died as a result of progression of their disease during the observation period. Still it was evident that the number of patients having high depression and anxiety scores was larger before than after the intervention. However, the limited number of patients makes interpretation difficult. In a study by Heim et al. [18] similar results to ours concerning the duration of the improvement were found, and these authors discuss the need for longer and/or repeated rehabilitation periods to consolidate a long-lasting effect of the intervention.
The cancer-related symptom of fatigue proved to be prominent also in our study and the patients experienced far more fatigue of all kinds in comparison to healthy controls, which is in accordance with other reports [16, 25, 35]. In the present programme, physical training (walking, swimming and relaxation) is included and could have been a factor in the positive effect on both fatigue and QOL in accordance with reports of others [5, 34, 35, 37, 39, 40, 44, 45]. Unfortunately, we were not able to identify major improvements after 3 months, a phenomenon also recognized by others [18, 19]. More women than men took part in the support group, which reduces the generalizability of our findings. However, this is a well-known phenomenon found by others [28, 29, 37]. Even online cancer support groups meet with this problem [28].
This pilot study demonstrated effects of our support programme at least up to 3 months after the intervention. The lack of a more prolonged effect could partly be due to the negative influence of clinical progression and restart of therapy in some of the patients. This may imply that the effect of the present intervention is underestimated, but the lack of a proper control group makes this notion speculative. To further study the impact of the same intervention programme on immune competence, QOL and clinical symptoms a randomized study is in progress in a more homogeneous group of breast cancer patients. Identification of a positive effect of the support group programme in this homogeneous, controlled randomized group of patients may be of great importance for the treatment policy for cancer patients in the future.
References
Ader R (2000) On the development of psychoneuroimmunology. Eur J Pharmacol 405:167–176
Andersen BL (1994) Surviving cancer. Cancer 74:1484–1495
Andrykowski MA, Curran SL, Lightner R (1998) Off-treatment fatigue in breast cancer survivors: a controlled comparison. J Behav Med 21:1–18
Appay V, Rowland-Jones SL (2002) Premature ageing of the immune system: the cause of AIDS? Trends Immunol 23:580–585
Blanchard CM, Courneya KS, Laing D (2001) Effects of acute exercise on state anxiety in breast cancer survivors. Oncol Nurs Forum 28:1617–1621
Bottomley A (1997) Cancer support groups—are they effective? Eur J Cancer Care (Engl) 6:11–17
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7:6–9
Bultz BD, Speca M, Brasher PM, Geggie PH, Page SA (2000) A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psychooncology 9:303–313
Carlson LE, Speca M, Patel KD, Goodey E (2003) Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med 65:571–581
Cella DF, Yellen SB (1993) Cancer support groups: the state of the art. Cancer Pract 1:56–61
Cunningham AJ, Edmonds CV, Jenkins G, Lockwood GA (1995) A randomised comparison of two forms of a brief, group, psychoeducational program for cancer patients: weekly sessions versus a “weekend intensive”. Int J Psychiatry Med 25:173–189
Escalante CP (2003) Treatment of cancer-related fatigue: an update. Support Care Cancer 11:79–83
Fawzy FI, Fawzy NW, Hyun CS, Elashoff R, Guthrie D, Fahey JL, Morton DL (1993) Malignant melanoma. Effects of an early structured psychiatric intervention, coping, and affective state on recurrence and survival 6 years later. Arch Gen Psychiatry 50:681–689
Garssen B, Goodkin K (1999) On the role of immunological factors as mediators between psychosocial factors and cancer progression. Psychiatry Res 85:51–61
Glaser R, Kiecolt-Glaser JK, Speicher CE, Holliday JE (1985) Stress, loneliness, and changes in herpesvirus latency. J Behav Med 8:249–260
Glaus A (1998) Fatigue in patients with cancer. Analysis and assessment. Recent Results Cancer Res 145:I–XI, 1–172
Grahn G (1993) “Learning to cope”—an intervention in cancer care. Support Care Cancer 1:266–271
Heim ME, Kunert S, Ozkan I (2001) Effects of inpatient rehabilitation on health-related quality of life in breast cancer patients. Onkologie 24:268–272
Helgeson VS, Cohen S, Schulz R, Yasko J (2000) Group support interventions for women with breast cancer: who benefits from what? Health Psychol 19:107–114
Helgeson VS, Cohen S, Schulz R, Yasko J (2001) Long-term effects of educational and peer discussion group interventions on adjustment to breast cancer. Health Psychol 20:387–392
Herbert TB, Cohen S (1993) Depression and immunity: a meta-analytic review. Psychol Bull 113:472–486
Herbert TB, Cohen S (1993) Stress and immunity in humans: a meta-analytic review. Psychosom Med 55:364–379
Ibbotsson T, Maguire P, Selby P, Priestman T, Walace L (1994) Screening for anxiety and depression in cancer patients: the effects of disease and treatment. Eur J Cancer 30A:37–40
Irwin M, Hauger R, Patterson TL, Semple S, Ziegler M, Grant I (1997) Alzheimer caregiver stress: basal natural killer cell activity, pituitary-adrenal cortical function, and sympathetic tone. Ann Behav Med 19:83–90
Irvine D, Vincent L, Graydon JE, Bubela N, Thompson L (1994) The prevalence and correlates of fatigue in patients receiving treatment with chemotherapy and radiotherapy. A comparison with the fatigue experienced by healthy individuals. Cancer Nurs 17:367–378
Kiecolt-Glaser JK, Glaser R, Strain EC, Stout JC, Tarr KL, Holliday JE, Speicher CE (1986) Modulation of cellular immunity in medical students. J Behav Med 9:5–21
Kiecolt-Glaser JK, Robles TF, Heffner KL, Loving TJ, Glaser R (2002) Psycho-oncology and cancer: psychoneuroimmunology and cancer. Ann Oncol 13 [Suppl 4]:165–169
Klemm P, Bunell D, Cullen M, Soneji R, Gibbons P, Holecek A (2003) Online cancer support groups: review of the research literature. Comput Inform Nurs 21(3):136–142
Krizek C, Roberts C, Ragan R, Ferrara JJ, Lord B (1999) Gender and cancer support group participation. Cancer Pract 7(2):86–92
Levy SM, Herberman RB, Maluish AM, Schlien B, Lippman M (1985) Prognostic risk assessment in primary breast cancer by behavioral and immunological parameters. Health Psychol 4:99–113
Maguire GP, Lee EG, Bevington DJ, Kuchemann CS, Crabtree RJ, Cornell CE (1978) Psychiatric problems in the first year after mastectomy. BMJ 1:963–965
Maguire P, Tait A, Brooke M, Thomas C, Sellwood R (1980) Effect of counselling on the psychiatric morbidity associated with mastectomy. BMJ 281:1454–1456
Maguire P (2002) Improving the recognition of concerns and affective disorders in cancer patients. Ann Oncol 13 [Suppl 4]:177–181
Meyer TJ, Mark MM (1995) Effects of psychosocial interventions with adult cancer patients: a meta-analysis of randomized experiments. Health Psychol 14:101–108
Mock V, Pickett M, Ropka ME, Muscari Lin E, Stewart KJ, Rhodes VA, McDaniel R, Grimm PM, Krumm S, McCorkle R (2001) Fatigue and quality of life outcomes of exercise during cancer treatment. Cancer Pract 9:119–127
Montazeri A, Jarvandi S, Haghighat S, Vahdani M, Sajadian A, Ebrahimi M, Haji-Mahmoodi M (2001) Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Educ Couns 45:195–198
Rosenbaum E, Gautier H, Fobair P, Neri E, Festa B, Hawn M, Andrews A, Hirshberger N, Selim S, Spiegel D (2004) Cancer supportive care, improving the quality of life for cancer patients. A program evaluation report. Support Care Cancer 12:293–301
Schedlowski M, Benschop RJ, Schmidt RE (1995) Psychological aspects of stress immunology. Immunol Today 16:165
Schwartz AL (2000) Daily fatigue patterns and effect of exercise in women with breast cancer. Cancer Pract 8:16–24
Schwartz AL, Mori M, Gao R, Nail LM, King ME (2001) Exercise reduces daily fatigue in women with breast cancer receiving chemotherapy. Med Sci Sports Exerc 33:718–723
Servaes P, Verhagen C, Bleijenberg G (2002) Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer 38:27–43
Smets EM, Garssen B, Schuster-Uitterhoeve AL, de Haes JC (1993) Fatigue in cancer patients. Br J Cancer 68:220–224
Stone P, Richards M, Hardy J (1998) Fatigue in patients with cancer. Eur J Cancer 34:1670–1676
Stone P, Richards M, A’Hern R, Hardy J (2000) A study to investigate the prevalence, severity and correlates of fatigue among patients with cancer in comparison with a control group of volunteers without cancer. Ann Oncol 11:561–567
Thune I, Smeland S (2000) Is physical activity important in treatment and rehabilitation of cancer patients? Tidsskr Nor Laegeforen 120:3302–3304
Vedhara K, Fox JD, Wang EC (1999) The measurement of stress-related immune dysfunction in psychoneuroimmunology. Neurosci Biobehav Rev 23:699–715
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361
Acknowledgements
We thank the patient guests and staff at the Foundation of Lustgården Mälardalen for making this study possible, and the Swedish Cancer Society for support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lindemalm, C., Strang, P. & Lekander, M. Support group for cancer patients. Does it improve their physical and psychological wellbeing? A pilot study. Support Care Cancer 13, 652–657 (2005). https://doi.org/10.1007/s00520-005-0785-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0785-8