Abstract
Nowadays, due to a growing number of tissue injuries, in particular, skin wounds, induction and promotion of tissue healing responses can be considered as a crucial step towards a complete regeneration. Recently, biomaterial design has been oriented towards promoting a powerful, effective, and successful healing. Biomaterials with wound management abilities have been developed for different applications such as providing a native microenvironment and supportive matrices that induce the growth of tissue, creating physical obstacles against microbial contamination, and to be used as delivery systems for therapeutic reagents. Until now, numerous strategies aiming to accelerate the wound healing process have been utilized and studied with their own pros and cons. In this review, tissue remodeling phenomena, wound healing mechanisms, and their related factors will be discussed. In addition, different methods for induction and acceleration of healing via cell therapy, bioactive therapeutic delivery, and/or biomaterial-based approaches will be reviewed.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
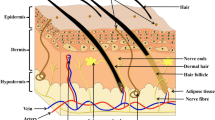
Undoubtedly, proper function of organs is highly dependent on their intrinsic ability of healing, remodeling, and regeneration. Several factors can interfere with this procedure and may lead to adverse conditions [1]. In particular, skin injuries, such as burn wounds, diabetic foot ulcers, surgical wounds, are currently considered as the most common complications [2]. According to the related reports, approximately 6% of the world population suffer from chronic wounds, which costs almost more than US$20 billion for medical care, annually [3]. In fact, maintenance of the integrity of the skin, the largest organ in the body, which acts as a physical, chemical, and biological barrier, is vital for a healthy life. Thus, in spite of vast markets in wound healing products, there is growing demand for professional wound treatment, especially in the case of chronic wounds, to reduce the economic burden of healthcare as well as raise the patient’s quality of life [2, 4]. Wound healing is a complicated process in the body, which depends on the presence of multiple types of cells, growth factors, cytokines, and extracellular matrix (ECM). In order to pave the way for ideal wound healing, comprehensive understanding about tissue remodeling and the healing process, along with cell-cell/biomaterial interactions, are considered important requirements that physicians must notice to benefit from biomaterial assisted wound healing [5]. One of the important aspects of successful regeneration is having a comprehensive understanding of the tissue remodeling process in order to emulate and induce it using suitable biomaterials. Our group have recently published a review discussing different types of bioactive materials and the inflammatory response following material implantation. Also, some approaches to modulate immune responses against implants have been reviewed [6]. Here, we aim to focus on tissue remodeling phenomena and wound healing mechanisms upon implantation as well as strategies to accelerate wound healing.
2 An overview of tissue remodeling
Tissue remodeling is a very complex phenomenon that consists of the reorganization or renovation of existing tissues. Actually, tissue remodeling can be referred to as tissue adaptation (in structure and function) to new conditions caused by various stimuli from inside or outside the tissue. Therefore, this process can change the characteristics of a tissue thereby altering in its dynamic equilibrium and causing changes in cellular composition and function. This process occurs physiologically or pathologically and is important in health and disease [7, 8].
2.1 Physiological tissue remodeling
Physiological tissue remodeling is an important mechanism in embryonic development, postnatal growth, healing, and improvement of health. The growth and remodeling of a tissue depends on its mechanical environment and genetic information. The mechanical environment can influence the development of tissue morphology and increase the size of existing structures, as well as the formation of proteins constructed by the tissue. Physiological tissue remodeling also occurs in some situations, such as ovulation and Pregnancy [9,10,11,12].
2.2 Pathological tissue remodeling
Tissue remodeling can occur in all pathological conditions. It is involved in hypertrophy, hypertension, ischemia, atherosclerosis, and asthma [13]. For example, asthma is characterized by a chronic inflammation of the airways. The healing process results in structural changes that enable the remodeling of the airways, which its mechanisms are unknown. It seems to be a heterogeneous and very dynamic process of cell dedifferentiation, migration, differentiation, and maturation, which leads to changes in connective tissue deposition and alters the restoration of the structure of airway. In the pathological remodeling of airways in asthma, mucus gland hyperplasia, neovascularization, fibrosis, and increase of smooth muscle mass occur [14].
2.3 Extracellular matrix remodeling
An ECM is a dynamic structure that is remodeled continuously to control tissue homeostasis. Mammalian ECM is composed of around 300 proteins, known as the core matrisome, which consist of 43 collagen subunits, 36 proteoglycans (PGs), and ~200 complex glycoproteins. Collagens are the main structural proteins of the ECM and exist in fibrillar (collagens I–III, V, and XI) and non-fibrillar forms. Collagen fibrils are responsible for the tensile strength of the ECM. Proteoglycans, such as aggrecan, versican, perlecan, and decorin, with attached glycosaminoglycan (GAG) side chains are scattered among collagen fibrils. They fill the extracellular interstitial space and are responsible for water maintenance in the tissue. GAGs, such as heparin sulfates, bind and sequester many growth factors in the ECM. Glycoproteins, such as laminins, elastin, fibronectins, thrombospondins, tenascins, and nidogen, have different functions. Not only they play an important role in ECM assembly, but are also involved in ECM–cell interactions acting as ligands for cell surface receptors such as integrins. Glycoproteins also store growth factors that bound to the ECM to be released after proteolysis. In addition to the mentioned proteins, there are many ECM-associated proteins that are not part of the matrisome. These proteins play an important role in ECM remodeling and include growth factors and cytokines, mucins, secreted C-type lectins, galectins, semaphorins, plexins, and ECM-modifying enzymes such as transglutaminase, lysyl oxidase, and hydroxylase, which are involved in crosslinking reactions.
The ECM can release growth factors, such as the epidermal growth factor (EGF), the fibroblast growth factor (FGF), and other signaling molecules including Wnts, transforming growth factor-β (TGFβ), amphiregulin, etc. After ECM cleavage, its components are released and they can influence ECM architecture and cell behavior. Meanwhile, ECM remodeling as a complex and highly regulated processes is started by cells through synthesis, degradation, reassembly, and chemical modification in order to maintain tissue homeostasis, particularly in response to injury. In pathological conditions, dysregulated ECM remodeling is observed, which can intensify the progression of the disease. For example, in fibrosis and cancer, abnormal deposition and stiffness of ECM are observed. Cleavage of ECM components, as the main process in ECM remodeling, can take place through different families of proteases, as presented below [15].
2.3.1 Matrix metalloproteinases
The main enzymes involved in ECM degradation are Matrix metalloproteinases (MMPs), whose activity is increased during repair or remodeling processes in diseased or inflamed tissue. They are produced as soluble or cell membrane-anchored proteinases, and can cleave specific ECM components. Matrix metalloproteinases can regulate the activity of several non-ECM bioactive substrates, and consequently affect different cellular functions. Matrix metalloproteinases are activated through proteolytic cleavage by Ser proteases or other MMPs, or via modification of their thiol group by oxidation, such as reactive oxygen species generated by leukocytes. Matrix metalloproteinases can degrade all ECM proteins, and their proteolytic actions on the ECM have crucial roles in organogenesis and branching morphogenesis. They may also be involved in vascular diseases such as hypertension, atherosclerosis, aortic aneurysm, and varicose veins. Matrix metalloproteinases play a role in the hemodynamic and vascular changes associated with pregnancy and preeclampsia, as well (Table 1) [16, 17].
2.3.2 Adamalysins (ADAMs)
Adamalysins (ADAMs) are membrane-bound enzymes, capable of detaching a multitude of proteins from the surface of the cells. They are, therefore, considered as crucial modulators of physiological and pathophysiological processes, such as cell-cell fusion, adhesion, and intracellular signaling. Their functional involvement has been documented in sperm-egg binding and fusion, trophoblast invasion, and matrix degradation during pregnancy, angiogenesis, and neovascularization. Clinically, ADAMs are used in pathological processes, including cancer, inflammation, neurodegeneration, and fibrosis, through shedding of the apoptosis-inducing FAS ligand, cytokines, and growth factors. This protein family includes ADAMs (a disintegrin and metalloproteinase) and ADAMTS (ADAMs with a thrombospondin motif). Among the identified genes for these enzymes, only a few are translated into active proteinases. They can cleave transmembrane protein ectodomains that are adjacent to the cell membrane and result in releasing the complete ectodomain of cytokines, growth factors, receptors, and adhesion molecules. The disintegrin domains mediate cell–ECM interactions by binding integrins, and the Cys-rich domains interact with heparan sulfate proteoglycans (HSPGs). ADAM10, ADAM12, and ADAM15 can also cleave collagens and other ECM proteins. In contrast to ADAMs, ADAMTS are metaloproteinases with thrombospondin type I-like repeats in their carboxy-terminal sequences. Acting in processing procollagen and aggrecan, ADAMTS play an important role in inflammatory diseases, especially in cartilage degeneration. ADAMTS2, ADAMTS3, and ADAMTS14 are pro-collagen N-propeptidases that process pro-collagens I, II, and III and are important for the deposition of normal collagen fibrils onto the ECM in a tissue-specific manner. The functions of some ADAMTS are still unclear [18].
2.3.3 Meprins
Meprins belong to the astacin family and are composed of two subunits (α and β) that are encoded by two different genes. The astacins are a subfamily of the metzincin superfamily of metalloproteinases. To date, more than 200 members of this family have been identified in species ranging from bacteria to humans. Astacins are involved in developmental morphogenesis, matrix assembly, tissue differentiation, and digestion. Meprins are the only astacin proteinase that functions on the membrane and on the ECM. They are unique in their domain structure and covalent subunit dimerization, oligomerization propensities, and expression patterns. Meprins can cleave ECM proteins such as collagen IV, nidogen, and fibronectin. Meprins can also indirectly regulate ECM remodeling by activating the other metalloproteinases. For example, ADAM10 is cleaved by meprin-β20, and both meprin-α and meprin-β promote the cleavage of pro-MMP9 by MMP3, ultimately accelerating the activation of MMP9. Compared with the other metalloproteinases, the roles of meprins in ECM remodeling are poorly understood [19].
2.3.4 Metalloproteinase inhibitors
ECM proteolysis requires tight regulation to avoid excessive and deleterious tissue degradation. Although there are no specific activators of MMPs, some MMP inhibitors have been identified. Therefore, the activity of endogenous inhibitors that inactivate ECM proteinases is important for tissue integrity. Matrix metalloproteinases inhibitors are often used to investigate the role of MMPs in different physiological processes and in the pathogenesis of specific diseases. They have been evaluated as diagnostic and therapeutic tools in cancer, autoimmune, and cardiovascular diseases [20]. Matrix metalloproteinases inhibitors include endogenous tissue inhibitors (TIMPs) and pharmacological inhibitors such as zinc chelators, doxycycline, and marimastat. The major cellular inhibitors of the MMPs sub-family are tissue inhibitors of metalloproteinases (TIMPs), exhibiting varying efficacy against different members, as well as different tissue expression patterns and modes of regulation. The TIMP family consists of four members (TIMP1–TIMP4) that reversibly inhibit the activity of MMPs, ADAMs, and ADAMTS, but not meprins. Matrix metalloproteinases-to-TIMP ratios determine the overall proteolytic activity, and each TIMP displays preferential MMP-binding specificity. TIMP3 is sequestered in the ECM, whereas the other TIMPs are present in soluble form in vivo. TIMP3 is the main inhibitor of ADAMs and ADAMTS. The membrane-associated reversion-inducing Cys-rich protein with Kazal motifs (RECK) also regulates the activity of MMPs and ADAMs. Cystatin C, elafin, and fetuin A have been identified as natural inhibitors of meprins [21].
Other proteins that have modest inhibitory activity against some of the MMPs include domains of netrins, the procollagen C-terminal proteinase enhancer, the RECK, and the tissue factor pathway inhibitor (TFPI-2). Reversion-inducing Cys-rich protein with Kazal motifs also regulates the activity of MMPs and ADAMs. Cystatin C, elafin, and fetuin A have been identified as natural inhibitors of meprins. Although several MMP inhibitors have been synthesized and tested both experimentally and clinically, only one MMP inhibitor, i.e. doxycycline, has been currently approved by the Food and Drug Administration (FDA). This is mainly due to the undesirable side effects of MMP inhibitors especially on the musculoskeletal system. While most experimental and clinical trials of MMP inhibitors have not demonstrated significant benefits, some trials still have showed promising results. With the advent of new genetic and pharmacological tools, disease-specific MMP inhibitors with fewer undesirable effects are being developed and could be useful in the management of vascular disease [16].
2.3.5 Other enzymes important in ECM remodeling
In addition to the mentioned enzymes, there are some other important enzymes in ECM remodeling, including Ser proteases, which target many ECM proteins. Two plasminogen activators: urokinase and tissue plasminogen activators target plasminogen to generate plasmin (a protein that degrades fibrin, fibronectin, and laminin). The Ser protease elastase that is released by neutrophils and promotes the breakdown of fibronectin and elastin, and the membrane-anchored Ser protease matriptase being expressed by epithelial cells, are important in order to maintaining the intestinal barrier.
Moreover, cathepsins are found both in extracellular and intracellular lysosomes. Secreted cathepsins degrade ECM proteins, but many cells can also internalize ECM components such as collagen through endocytosis and degrade them in the lysosomes. Cathepsins Families include the Ser cathepsins (cathepsins A and G), Asp cathepsins (cathepsins D and E) and Cys cathepsins.
Finally, heparanases and sulfatases can alter the properties of ECM PGs. Heparanase, an endoglucuronidase, is responsible for heparan sulfate (HS) cleavage and regulates the structure and function of HSPGs. This results in structural alterations of the ECM, as well as the release of bioactive saccharide fragments and HS-bound growth factors and cytokines. Suphatase 1 and sulfatase 2 are secreted endosulfatases that remove 6-O-sulfate residues from HS and modulate HS binding of many cytokines and growth factors, including FGF1 and vascular endothelial growth factor [22, 23].
2.3.6 ECM maturation
Activated fibroblasts, in particular “myofibroblasts,” participate in the tissue repair by secretion of significant amounts of ECM proteins, which are responsible for contraction of wounds (Fig. 1) [24]. Therefore, repair and remodeling of injured tissues depend on the timely activation and deactivation of myofibroblasts. For instance, prolonged or excessive myofibroblast’s activity may result in fibrosis and organ dysfunction [25,26,27]. In addition to fibroblasts, mesenchymal stem cells (MSCs) and macrophages are both involved in tissue remodeling and ECM synthesis. Due to the high plasticity of MSCs, they are involved in physiological and regenerative tissue remodeling. Moreover, macrophages are critical cells in tissue remodeling after injury, which can change their phenotypes, as well as their metabolic, and functional activities; this is known as divergent polarization in response to microenvironment [28].
Schematic of myofibroblast that secrets elastins, fibrillins and LTBPs, proteoglycans, tenascins, matricellular proteins, collagens, and fibronectins [24]. Reprinted with permission
In the remodeling stage, the tissue achieves the maximum tensile strength through reorganization, degradation, and resynthesis of the ECM. In fact, remodeling is marked by changing and maturing of ECM components, as well as the resolution of the initial inflammation (Fig. 2) [29].
Sequential illustration of the stages involved in tissue repair [29]
2.4 Mechanical remodeling
Studies have documented that many tissues such as cartilage, bone, ligament, cardiac muscle, and blood vessels require a mechanically dynamic environment for their normal function. In fact, continuous exposure to the mechanical forces can lead to tissue remodeling [30]. On the basis of scaffold’s properties, cellular functions such as attachment, migration, differentiation, proliferation, and apoptosis can be affected by external signals, whose cells sense via receptor–ligand interactions from outside of the cytoskeletal domain. Considering the mechanical stimulus during tissue development, researchers have employed tissue engineering approaches to mimic physical stimuli to encourage tissue growth and repair; especially for load-bearing applications. For example, it has been shown that application of mechanical forces including hydrostatic pressure or direct compression in bioreactors during the culture of chondrocytes result in more ECM secretion compared to that in a static culture [31].
Thus, mechanical signals and internal cell-generated forces are mainly responsible for altering the tissue pattern and play an important role in embryogenesis and morphogenesis, along with chemical regulators. Studies have demonstrated that fluid shear forces are crucial in arterio-venous cell fate determination and also promote kidney development by orchestrating the movement of the epithelium, which results in functional nephrons. Moreover, application of mechanical tensions on the substrate of neural cells can cause better cell adhesion, nerve guidance, as well as formation of mature neuronal networks [32].
3 Wound healing process
As mentioned before, only by understanding the normal process of tissue repair, the development of therapeutic approaches is possible. In this sight, it should be noted that wound healing is a complicated dynamic mechanism attributed to tissue growth and remodeling in orchestrated intercellular and extracellular pathways. Wound healing can be categorized into 4 steps: hemostasis and inflammation, migration, proliferation, and maturation (known as the scar formation phase) (Fig. 3) [3, 5, 33, 34].
Schematic of wound healing phases. After formation of fibrin clot in hemostasis, in the presence of secretion of growth factors and cytokines, phagocytic cells migrate to the site of injury in order to run inflammatory pathway. By proliferation of skin cells and angiogenesis, granulation tissue is formed. Finally, remodeled collagenous matrix fills the wounded site and epithelialisation is ceased [34]. Reprinted with permission
3.1 Hemostasis and inflammation
When an injury occurs, keratinocytes presented in the damaged epidermal layer, along with the platelets, secrete IL-1 and hemostatic factors, respectively, while the bleeding helps remove antigens and pathogens from the wound site. After the formation of the fibrin network by enzymatic activity of thrombin on fibrinogen released in the exudates, the blood clot containing platelet plaque is created, which serves as a preliminary matrix for inflammatory cells settlement [35].
The inflammatory phase starts shortly after hemostasis, because the degranulated platelets also release the α-granules, resulting in the secretion of several growth factors, including the EGF, the platelet-derived growth factor (PDGF), and TGF-β, as well as inflammatory interleukins and cytokines, which pave the way for recalling neutrophils and other cells to the wound bed. It should be noted that, in the presence of the protein enriched exudates, histamine and serotonin can run the vasodilatation of peripheral vessels with the benefit of the increased vascular permeability, then the monocytes can easily penetrate and start phagocytosis. TGF-β plays an important role in the transition of monocytes into macrophages and by changing their phenotypes from pro-inflammatory (M1 macrophage) to pro-healing (M2 macrophage). Secretion of more cytokines and growth factors can bring about angiogenesis, creation of granulated tissue, and healing. When the transition of M1 to M2 is ceased, chronic and non-healing wounds (e.g. diabetic wounds) are formed [5, 36,37,38]. Interestingly, one of the main strategies for improvement of wound healing could be using biomaterials to induce M1-M2 transition. For example, in one study, Zhang and Sefton have injected methacrylic acid (MAA) beads subcutaneously in CD1 mice and investigated the vascular formation during a period of 7 days. They found out that in addition to the absorption of factors and proteins to the surface of the beads, MAA beads induced a polarization bias towards M2 macrophages, which is a key element in the process of vessel formation, as well as healing [34, 39].
3.2 Migration
This phase involves movement of the epithelial cells and fibroblasts to the damaged area. In addition, due to the release of VEGF and FGF, angiogenesis proceeds through the migration and proliferation of vascular cells such as endothelial cells. TGF-β, FGF, and PDGF factors affect the penetration of fibroblasts and the change in their phenotype to myoblasts, which help in wound closure. During the epithelialization, secretion of EGF, FGF, and TGF-α leads to the migration, polarization, and proliferation of epithelial cells and keratinocytes. Moreover, keratinocytes undergo differentiation forming multilayers to restore epidermis [40, 41].
3.3 Proliferation
The proliferative phase occurs almost simultaneously or immediately after the migratory phase. In this phase, the wound bed is filled with growing skin cells and more secreted growth factors and cytokines such as TNF-α and IL-6. At this stage, the hair follicle stem cells and bone marrow derived stem cells (such as MSCs) differentiate into epidermal and dermal cells and proliferate in order to regenerate the tissue and replace the missing cells. However, in chronic and non-healing wounds, this ability is deregulated due to continuous inflammation, infection, prolonged hypoxia, or other pathological issues. Granulated tissue formation is started with the growth of the capillaries and lymph vessels into the wound. Moreover, collagen synthesized by fibroblasts plays an important role in increasing the strength of the new formed tissue and its shaping. Therefore, macrophages, fibroblasts, and blood vessels, along with a loose matrix made of collagen, glycoprotein, fibronectin, and hyaluronic acid (HA), comprise the granulated tissue [5, 37, 42].
3.4 Maturation and remodeling
In the maturation or remodeling phase, the cellular connective tissue is constructed, and the new epithelial layer becomes stable, which results in the formation of the final scar. The granulated tissue transforms into a cell-free mass. For this purpose, a matrix made of densely packed collagen fibers being supplemented by proteoglycans and glycoproteins is created. Finally, after synthesis of new collagen in the presence of TGF-β, the scar tissue formation is completed [5, 43].
3.5 Angiogenesis in wound healing process
Angiogenesis, which is the process of vessel formation from existing ones, has a fundamental impact on wound healing. During the healing phase, a number of functional and dysfunctional capillaries in the form of organized radial shaped vessels are formed at the wound border, which are then eliminated in maturation or apoptotic processes [44]. One of the major signaling pathways for angiogenesis is through the activation of the heterodimeric protein complex of hypoxia-induced factor (HIF) due to the existing hypoxia in the wound bed [45]. However, other signaling pathways, such as inflammatory pathways (which are mostly mediated by interferon-γ (IFN-γ), TNF-α, IL-4, etc.) and sonic hedgehog pathways also play important roles in the modulating and maturating the neovascularization process [46, 47]. Pathological issues such as diabetes and vascular diseases can lead to impairment of normal angiogenesis, causing wound healing disturbance. Thus, induction of angiogenesis can be considered as a pivotal step to improve the microenvironment that impedes skin repair caused by chronic wounds. For this purpose, application of stem cells, co-culture with vascular cells, and controlled delivery of angiogenic growth factors such as VEGF, FGF, PDGF have been utilized in different researches. For example, Lai et al. used a collagen-HA fibrous scaffold containing growth factor loaded particles to cure diabetic wounds by induction of angiogenesis. Results have represented fast re-epithelialization, growth of endothelial cells, and formation of a thread-like tubular system [48]. Moreover, Wu et al. have documented that by using a cell therapy approach and, in particular, injection of MSCs into the site of injury, improvement of non-healing wounds can occur through wound closure and angiogenesis [49].
4 Wound healing acceleration strategies
As mentioned before, wound healing is a complicated multiphase process, which requires comprehensive understanding of molecular pathways. Over the years, studies have investigated the healing process from a variety of points of view. Different strategies conducted to accelerate wound healing rely on 3 dominant methods (Fig. 4):
-
(1)
Cell therapy based on using multi potent stem cells and co-culture techniques to create new skin.
-
(2)
Bioactive therapeutic delivery, which consists of engineering the release of healing components to enhance the rate of wound repair.
-
(3)
Application of biomaterial/scaffold for skin tissue engineering and inducing regeneration.
In this section, each method will be briefly discussed, and the related case studies will be referred. Considering the 3 aspects of tissue engineering, an ideal approach would be the combination of all the above strategies whereby a 3D functional structure containing healthy cells is formed and their behavior is regulated by signaling molecules.
4.1 Cell therapy
Cell delivery, which in this regard is described as transporting either skin or vascular cells to the site of injury, has attracted much attention in the acceleration of regenerative wound healing. Among the different cells, stem cells, due to their potential to differentiate into several cell types and self-renewal properties, have been suggested specially for the treatment of chronic and non-healing wounds [50, 51]. The majority of the cells are used for skin regeneration, including adipose derived stem cells (ADSCs), MSCs, endothelial progenitor cells (EPCs), induced pluripotent stem cells (iPSCs), etc (Fig. 5) [52, 53]. Studies have shown that not only do EPCs help improving angiogenesis and epithelialization, but also their co-culture with fibroblasts can lead to scarless wound healing. On the other hand, MSCs can play a pivotal role in wound healing and induction of angiogenesis. These cells are obtained from different tissues such as adipose, bone marrow, sweat glands, pancreas, etc. However, isolation of adipose tissue harvested from patients is the best and less immunogenic way for supplying cells in skin tissue engineering [54, 55].
A schematic of different sources of stem cells for wound healing applications [55]. Reprinted with permission
Countless advantages of ADSCs, including easy culturing, accessibility, high proliferation, and differentiation, make them promising for wound healing applications. For example, in a study performed by Ozpur et al., in order to create artificial skin tissue, fibrin gels containing keratinocytes and ADSCs, were used. Results showed that the substitute provided re-epithelialization of the wound as well as increased collagen deposition and vessel formation [56]. In another study, Cerqueira et al. seeded ADSCs and endothelial cells (both were extracted from human adipose tissue) in gellan gum–HA (GG–HA) hydrogels. It was demonstrated that cells incorporated in the GG-HA hydrogel can promote neovascularization and granulation tissue formation with greater wound closure, re-epithelialization, and resemblance of normal skin tissue [57].
It should be noted that low cell viability is one of the main problems in conventional cell therapy [58]. In order to address this problem, cell delivery within hydrogels and cell imprinting are suggested as an alternative cellular approach to achieve better healing. Using bioprinting and modified laser induced forward transfer technologies; it is possible to make a 3D skin graft [59, 60]. Koch et al. used a laser-assisted method to print fibroblasts and keratinocytes embedded in collagen gel, layer by layer. After 10 days of culturing, cells proliferated and showed high viability, making an integrated graft with tight cellular junction [61].
4.2 Bioactive therapeutic delivery
Because of the fact that systemic use of effective biomolecules has some disadvantages such as low bioavailability, toxicity, and significant side effects caused by non-target delivery, localized and targeted delivery of therapeutics can increase the number of predictable release patterns in the therapeutic window. With the benefit of biomaterials and encapsulation of therapeutics into nano/micro carriers or engineered scaffolds, sustained and localized delivery of therapeutics can be developed [62]. An ideal carrier for bioactive therapeutic delivery should be biocompatible, biodegradable, non-cytotoxic, and easy to fabricate by tailoring the physical/chemical properties. Till now, therapeutics have been loaded into different nano/micro carriers such as fibers, spheres, capsules, sheets, rods, and dot arrays (Fig. 6). These carriers can be produced in form of core-shell structures with the benefit of storing the drug in the core cavity, while modifying shell composition (polymers or lipids) to adjust the release pattern [63].
Illustration of different design of nano/microparticles. The efficiency of particles can be adjusted from different aspects which mainly includes modification of composition, physical properties, surface chemistry and targeting ligands [63]. Reprinted with permission
The vast lists of drugs known to have antibacterial, regenerative, and angiogenic effects from natural bioactive and biochemical therapeutics have been used in wound healing treatments. For example curcumin [64], berberine [65], rosemary oil [66], thyme extract [67], Aloe vera [68, 69], and honey [70], as natural agents, and gentamicin [71], tetracycline hydrochloride [72], vancomycine [73, 74], melatonin [75], simvastatin [76], and erythropoietin [77] as chemical agents, can be suggested. In a study by Ghayempour et al., microemulsions made of Aloe vera extract encapsulated into Tragacanth gum were prepared as a wound healing product. High antimicrobial activities (80–90%) against different bacterial species, high cell viability, and the ability to induce migration of fibroblasts were some of the promising obtained results mentioned by these authors [78]. In addition to the aforementioned particles, metallic and semi conductive nanoparticles; namely copper, silver, iron oxide, zinc oxide, and titanium dioxide, along with graphene oxide, have been frequently used in the field of wound healing due to their antimicrobial activities and high penetration ability through the cell membrane [63, 79]. However, because of the undefined fate in the body and possible cytotoxicity, their uses are restricted.
4.3 Gene therapy
Skin is considered as a suitable target for delivery of genetic-based therapeutics, due to the readily attainable anatomical position for gene transfer and visually observable therapeutic effects. Among several studies performed for skin gene therapy, those encapsulated into the nano/micro carriers, tissue scaffolds, or even using genetic manipulated cells are more prosperous regarding their potential to both protect genetic based therapeutics from enzymatic degradation and improve their healing effects [80, 81]. Application of siRNAs and miRNAs, as RNA-based structures, which either interfere or inhibit translation of mRNAs to protein, is extremely influential and prevalent in the scope of wound healing treatment [82]. Based on the researches, miR-210, -205, -203, -198, -184, -155, -132, -126, -99 and -21 are able to regulate proliferation, differentiation, and migration of keratinocytes and endothelial cells [40]. In addition, several studies are aimed to use siRNAs as therapeutics for selective inhibition of MMP, fibrotic tissue growth factors, inflammatory cytokines, p53, and also prolyl hydroxylase domain (PHD) proteins to induce fast healing and angiogenesis in specially chronic and non-healing wounds. As an example, Martin et al. applied PHD2 siRNAs loaded in modified polyurethane scaffolds in order to heal a diabetic wound. Results showed that %65 of total prolyl hydroxylases were inhibited, which can cause increase in production of VEGF, improvement of angiogenesis, and skin regeneration [83]. In another study, Yang et al. used loaded electrospun fibers for sequential delivery of basic-FGF (bFGF) plasmids, which promoted neovascularization and enhanced collagen synthesis, as well as formation of skin appendages [40].
4.4 Growth factor delivery
Growth factors are polypeptides released by numerous cells in a given time to stimulate cellular proliferation, differentiation, and migration. Regarding the key role of growth factors in the regulation of the wound healing process, controlled and sequential delivery to the wound sites is the topic of many current researches. Numerous growth factors such as EGF, VEGF, FGF, TGF, and PDGF have been studied in order to induce wound healing through angiogenesis, matrix deposition and re-epithelialization [81, 84]. One of the main concerns in the delivery of growth factors is their short half-life, which instantly produces enzymatic degradation, thereby making their sustained release crucial in tissue engineering [85]. Research findings have confirmed increased epithelialization, neovascularization, migration of keratinocytes, and fast healing of venous and diabetic foot ulcers after applying EGF on the wound site [86]. On the other hand, clinical trials conducted on second-degree burn patients suggested that instant application of FGF on the wound surface can accelerate wound healing rates and formation of protective and strong granulated tissue [87]. Interestingly, utilization of growth factors in combination with cells or natural materials for chronic and non-healing wound treatment has attracted extensive attention. For example, neovascularization, re-epithelialization, and wound closure have been documented in the results of studies using MSCs that secrete VEGF and platelet-rich plasma as potent sources of growth factors in full-thickness wounds [40].
4.5 Scaffolds/biomaterial assisted wound healing
Due to the fact that ECM plays a crucial role in wound healing and tissue homeostasis, creation of a supportive scaffold for the cells similar to their native niche is essential for optimizing cell behaviors. Scaffolds can be made of either natural or synthetic biomaterials, as well as a combination of them in the form of hydrogels, electrospun fibers, films, etc. Biocompatibility, biodegradation, bioactivity, and cellular adhesion, are some of the properties of natural biomaterials. Collagen, gelatin, HA, chitosan, alginate, elastin, and silk fibroin are some of the natural polymers providing bioactive scaffolds that can create complex cellular interactions during healing [59, 88]. Among these natural materials, several studies have emphasized the significant effect of GAGs, and in particular HA, in wound healing. Presence of high water content in their molecular chain, along with the ability to act as a reservoir of growth factors, makes them ideal for the scope of tissue regeneration [40, 89]. However, low stability in harsh wound areas and poor mechanical strength of natural polymers require their modification. In this regard, synthetic biomaterials such as polyvinyl alcohol, polyethylene glycol (PEG), polyurethane (PU), PCL, poly(l-lactic acid), polyglycolic acid (PGA), and poly lactic-co-glycolic acid, whose tailored-made properties and easy fabrication can be used in combination with natural materials to create an ideal substitute [90].
It is worth mentioning that human body byproducts including amniotic membrane (AM), Wharton’s jelly, hair derived keratin, platelet-rich plasma, etc. can also be used for improvement of skin wound healing. The innate healing ability of these structures mostly comes from their active protein domains and growth factors presented inside them. AMs, which can be used whether directly or decellularized, have shown advantages such as cost effectiveness, low foreign body reaction, and high potential for re-epithelialization. This membrane is suitable for covering both full and partial thickness wounds instead of skin grafts [40, 91, 92].
From various forms of scaffolds, nanofibers and hydrogels are frequently utilized as a skin substitute with or without cells or bioactive therapeutics. Nanofibers can assist increasing cellular interactions by simulating a native ECM microenvironment, thereby improving adhesion and forming a porous structure [93]. Nanofibrous wound dressings readily absorb exudates from the wound site while keeping them moistened as well as promoting oxygen diffusion through the injury [94]. Moreover, owing to the high surface to volume ratio, nanofibers can be easily modified for delivery of bioactive therapeutics. There are numerous methods for nanofiber synthesis such as phase separation, template synthesis, self-assembly, and electrospinning. Because of the low cost, higher control over fiber diameter, and the ability to produce fibers from different kinds of polymers, electrospun fibers are quite versatile [95, 96].
Since too slow or too quick degradation can promote fibrosis and/or insufficient support for tissue ingrowth, the degradation rate of a tissue regenerative material should be matched with the rate of tissue development [42]. In this regard, hydrogels and specially injectable hydrogels have attracted scientific researches to restore functional tissue with minimal invasion [97]. High hydrophilicity, tissue-like elasticity, and facile transport of nutrients and waste make hydrogels promising candidates for expanded usage in vitro and in vivo. Temperature sensitive gel formation using poly(N-isopropylacrylamide (PNIPAM)) [98], photo-crosslinkable gels using UV radiation to acrylated natural or synthetic polymers (e.g. polyethylene glycol diacrylate (PEG-DA) and gelatin methacrylate (GelMa)) [97], and microporous annealed particle (MAP) gels are hot topics and frequent structures used in tissue engineering and drug delivery application with noticeable results. In a study done by Lisovsky et al. the ability of methacrylate moieties for induction of angiogenesis was investigated [34]. Further, in a Chen et al. work, the angiogenic ability of injectable scaffold made of Deferoxamine loaded GelMa was evaluated. Results confirmed the up-regulated expression of HIF-α and fast wound healing in diabetic rats after 14 days [99]. Recently, Huang et al. proposed new hybrid scaffolds based on GelMa which incorporated tofu and red jujube as bioactive components in order to increase the antioxidant activity as well as the wound healing rate. In vivo results performed on skin wound model represented minor immunological stimulation (due to the induced M2 differentiation of macrophages) as well as enhanced antioxidant activities of the hydrogels. Prepared hydrogels, also, accelerated the rate of wound healing and skin tissue regeneration [100, 101].
In 2015, Griffin et al. created an injectable biomaterial from MAP gels with tailored degradation to a desired rate. This novel gel structure provided a linked interconnected network suitable for cell migration and high tissue integration. In fact, these groups used self-assembly of hydrogel microparticles formed by microfluidic water-in-oil droplet segmentation, whose cluster of microgels were annealed to each other via surface functionalities. Moreover, the design could be accompanied with encapsulation of cells. The aforementioned MAP structure was then injected and molded into any shape to create a 3D stable scaffold (Fig. 7) [102].
MAP scaffolds injected and molded to form star shape that is maintained after annealing. After formation of microgels through in-droplet mixing of pre-gels and crosslinker solutions, annealing occurs to form a microporous scaffold either with or without presence of the cells [102]. Reprinted with permission
5 Conclusion
Addressing the complications during impaired wound healing is still a challenge in medicine due to the sophisticated healing process with multiple effective cellular signaling pathways. Despite striking progress in this field, chronic and non-healing wounds are still of major concerns. There are numerous strategies for the treatment of ulcers from auto/allografts to wound dressings and skin substitutes, which have limitations in scarless regeneration, normal healing, and sufficient angiogenesis. In order to raise the efficiency of these products, complimentary approaches should be applied to accelerate wound healing. The engineering of scaffold structures, integration of bioactive therapeutics, as well as stem cells into such environment can enhance the capability of active guidance in skin regeneration. Understanding the dynamics of cell-cell and cell-ECM interactions in healthy and impaired wound healing also could help identify the most appropriate strategies to overcome disadvantages of currently applied wound dressings.
References
Valero C, Javierre E, García-Aznar JM, Menzel A, Gómez-Benito MJ. Challenges in the modeling of wound healing mechanisms in soft biological tissues. Ann Biomed Eng. 2015;43:1654–65.
Darwin E, Tomic-Canic M. Healing chronic wounds: current challenges and potential solutions. Curr Dermatol Rep. 2018;7:296–302.
Whittam AJ, Maan ZN, Duscher D, Wong VW, Barrera JA, Januszyk M, et al. Challenges and opportunities in drug delivery for wound healing. Adv Wound Care. 2016;5:79–88.
Frykberg RG, Banks J. Challenges in the treatment of chronic wounds. Adv Wound Care. 2015;4:560–82.
Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol. 2015;173:370–8.
Nour S, Baheiraei N, Imani R, Rabiee N, Khodaei M, Alizadeh A, et al. Bioactive materials: a comprehensive review on interactions with biological microenvironment based on the immune response. J Bionic Eng. 2019;16:563–81.
Kassab GS. A systems approach to tissue remodeling. J Biomech Eng. 2009;131:101008.
Desmoulière A, Darby IA, Gabbiani G. Normal and pathologic soft tissue remodeling: role of the myofibroblast, with special emphasis on liver and kidney fibrosis. Lab Investig. 2003;83:1689.
Khalil RA. Matrix metalloproteinases and tissue remodeling in health and disease: target tissues and therapy. Vol. 148. Academic Press; 2017.
Tsafriri A. Ovulation as a tissue remodelling process. In: Tissue renin-angiotensin systems. Springer, Basel, 1995. p. 121–40.
Cowin SC. Tissue growth and remodeling. Annu Rev Biomed Eng 2004;6:77–107.
Fernandes T, Baraúna VG, Negrão CE, Phillips MI, Oliveira EM. Aerobic exercise training promotes physiological cardiac remodeling involving a set of microRNAs. Am J Physiol-Heart Circulatory Physiol. 2015;309:H543–52.
Vignola AM, Kips J, Bousquet J. Tissue remodeling as a feature of persistent asthma. J Allergy Clin Immunol. 2000;105:1041–53.
Athari SS, Pourpak Z, Folkerts G, Garssen J, Moin M, Adcock IM, et al. Conjugated alpha-alumina nanoparticle with vasoactive intestinal peptide as a nano-drug in treatment of allergic asthma in mice. Eur J Pharmacol. 2016;791:811–20.
Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat Rev Mol Cell Biol. 2014;15:786.
Baker AH, Edwards DR, Murphy G. Metalloproteinase inhibitors: biological actions and therapeutic opportunities. J Cell Sci. 2002;115:3719–27.
Caley MP, Martins VLC, O’Toole EA. Metalloproteinases and Wound Healing. Adv Wound Care. 2015;4:225–34.
Van Goor H, Melenhorst WB, Turner AJ, Holgate ST. Adamalysins in biology and disease. J Pathol. 2009;219:277–86.
Sterchi EE, Stöcker W, Bond JS. Meprins, membrane-bound and secreted astacin metalloproteinases. Mol Asp Med. 2008;29:309–28.
Benjamin MM, Khalil RA. Matrix metalloproteinase inhibitors as investigative tools in the pathogenesis and management of vascular disease. In: Matrix metalloproteinase inhibitors. Springer, Basel, 2012. p. 209–79.
Levin M, Udi Y, Solomonov I, Sagi I. Next generation matrix metalloproteinase inhibitors — novel strategies bring new prospects. Biochimica et Biophysica Acta. 2017;1864:1927–39.
Cox TR, Erler JT. Remodeling and homeostasis of the extracellular matrix: implications for fibrotic diseases and cancer. Dis Models Mechanisms. 2011;4:165–78.
Karsdal MA, Nielsen MJ, Sand JM, Henriksen K, Genovese F, Bay-Jensen A-C, et al. Extracellular matrix remodeling: the common denominator in connective tissue diseases possibilities for evaluation and current understanding of the matrix as more than a passive architecture, but a key player in tissue failure. Assay Drug Dev Technol. 2013;11:70–92.
Klingberg F, Hinz B, White ES. The myofibroblast matrix: implications for tissue repair and fibrosis. J Pathol. 2013;229:298–309.
Shinde AV, Humeres C, Frangogiannis NG. The role of α-smooth muscle actin in fibroblast-mediated matrix contraction and remodeling. Biochimica et Biophysica Acta. 2017;1863:298–309.
Viennet C, Muret P. Fibroblast evaluation: extracellular matrix synthesis. In: Measuring the Skin. Springer, Cham, 2016. p. 1–5.
Kasetti RB, Maddineni P, Millar JC, Clark AF, Zode GS. Increased synthesis and deposition of extracellular matrix proteins leads to endoplasmic reticulum stress in the trabecular meshwork. Sci Rep. 2017;7:14951.
Andreeva ER, Buravkova LB. The role of interplay of mesenchymal stromal cells and macrophages in physiological and reparative tissue remodeling. Hum Physiol. 2018;44:102–14.
Gonzalez ACdO, Costa TF, Andrade ZdA, Medrado ARAP. Wound healing - a literature review. An Brasileiros de Dermatologia. 2016;91:614–20.
Reddi AH. Chapter 11 - Morphogenesis and tissue engineering. In: Lanza R, Langer R, Vacanti J, editors. Principles of tissue engineering (fourth edition). Boston: Academic Press; 2014. p. 209–23.
Ikada Y (editor). Chapter 4 - Challenges in tissue engineering. Interface science and technology. Vol. 8. Elsevier, 2006; p. 423–62.
Mammoto T, Ingber DE. Mechanical control of tissue and organ development. Development. 2010;137:1407–20.
Sorg H, Tilkorn DJ, Hager S, Hauser J, Mirastschijski U. Skin wound healing: an update on the current knowledge and concepts. Eur Surg Res 2017;58:81–94.
Lisovsky A, Chamberlain MD, Wells LA, Sefton MV. Cell interactions with vascular regenerative MAA-based materials in the context of wound healing. Adv Healthc Mater. 2015;4:2375–87.
Han G, Ceilley R. Chronic wound healing: a review of current management and treatments. Adv Therapeutics. 2017;34:599–610.
Alvarez MM, Liu JC, Santiago GT-d, Cha B-H, Vishwakarma A, Ghaemmaghami AM, et al. Delivery strategies to control inflammatory response: modulating M1-M2 polarization in tissue engineering applications. J Controlled Release. 2016;240:349–63.
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73:3861–85.
Minutti CM, Knipper JA, Allen JE, Zaiss DMW. Tissue-specific contribution of macrophages to wound healing. Semin Cell Dev Biol. 2017;61:3–11.
Hu S, De Vos P. Polymeric approaches to reduce tissue responses against devices applied for islet-cell encapsulation. Front Bioeng Biotechnol. 2019;7:134.
Rousselle P, Braye F, Dayan G. Re-epithelialization of adult skin wounds: cellular mechanisms and therapeutic strategies. Adv Drug Deliv Rev. 2018;5:pii: S0169-409X(18)30158-3.
Shaw TJ, Martin P. Wound repair: a showcase for cell plasticity and migration. Curr Opin Cell Biol. 2016;42:29–37.
Keane TJ, Horejs CM, Stevens MM. Scarring vs. functional healing: matrix-based strategies to regulate tissue repair. Adv Drug Deliv Rev. 2018;129:407–19.
Boateng JS, Matthews KH, Stevens HNE, Eccleston GM. Wound healing dressings and drug delivery systems: a review. J Pharmacuetical Sci. 2008;97:2892–923.
Novosel EC, Kleinhans C, Kluger PJ. Vascularization is the key challenge in tissue engineering. Adv Drug Deliv Rev. 2011;63:300–11.
Pugh CW, Ratcliffe PJ. Regulation of angiogenesis by hypoxia: role of the HIF system. Nat Med. 2003;9:677–84.
Renault M, Roncalli J, Tongers J, Klyachko E, Misener S, Volpert OV, et al. Sonic hedgehog induces angiogenesis via Rho kinase-dependent signaling in endothelial cells. J Mol Cell Cardiol. 2011;49:490–8.
Kreuger J, Phillipson M. Targeting vascular and leukocyte communication in angiogenesis, inflammation and fibrosis. Nat Rev Drug Discov. 2016;15:125–42.
Lai HJ, Kuan CH, Wu HC, Tsai JC, Chen TM, Hsieh DJ, et al. Tailored design of electrospun composite nanofibers with staged release of multiple angiogenic growth factors for chronic wound healing. Acta Biomater. 2014;10:4156–66.
Leonida MD, Kumar I. Bionanomaterials for Skin Regeneration. Cham: Springer International Publishing; 2016.
Dreifke MB, Jayasuriya AA, Jayasuriya AC. Current wound healing procedures and potential care. Mater Sci Eng C Mater Biol Appl. 2015;48:651–62.
Nourian Dehkordi A, Mirahmadi Babaheydari F, Chehelgerdi M, Raeisi Dehkordi S. Skin tissue engineering: wound healing based on stem-cell-based therapeutic strategies. Stem Cell Res Ther. 2019;10:111.
Dash BC, Xu Z, Lin L, Koo A, Ndon S, Berthiaume F, et al. Stem cells and engineered scaffolds for regenerative wound healing. Bioengineering. 2018;5:pii: E23.
Lee DE, Ayoub N, Agrawal DK. Mesenchymal stem cells and cutaneous wound healing: novel methods to increase cell delivery and therapeutic efficacy. Stem Cell Res Ther. 2016;7:37.
Frueh FS, Menger MD, Lindenblatt N, Giovanoli P, Laschke MW. Current and emerging vascularization strategies in skin tissue engineering. Crit Rev Biotechnol. 2017;37:613–25.
Duscher D, Barrera J, Wong VW, Maan ZN, Whittam AJ, Januszyk M, et al. stem cells in wound healing: the future of regenerative medicine? A mini-review. Gerontology. 2016;62:216–25.
Ozpur MA, Guneren E, Canter HI, Karaaltin MV, Ovali E, Yogun FN, et al. Generation of Skin tissue using adipose tissue-derived stem cells. Plast Reconstr Surg. 2016;137:134–43.
Cerqueira MT, da Silva LP, Santos TC, Pirraco RP, Correlo VM, Reis RL, et al. Gellan gum-hyaluronic acid spongy-like hydrogels and cells from adipose tissue synergize promoting neoskin vascularization. ACS Appl Mater Interfaces. 2014;6:19668–79.
Battiston KG, Cheung JW, Jain D, Santerre JP. Biomaterials in co-culture systems: towards optimizing tissue integration and cell signaling within scaffolds. Biomaterials. 2014;35:4465–76.
Stratton S, Shelke NB, Hoshino K, Rudraiah S, Kumbar SG. Bioactive polymeric scaffolds for tissue engineering. Bioact Mater. 2016;1:93–108.
Arslan-Yildiz A, Assal RE, Chen P, Guven S, Inci F, Demirci U. Towards artificial tissue models: past, present, and future of 3D bioprinting. Biofabrication. 2016;8:014103.
Koch L, Deiwick A, Schlie S, Michael S, Gruene M, Coger V, et al. Skin tissue generation by laser cell printing. Biotechnol Bioeng. 2012;109:1855–63.
Ho J, Walsh C, Yue D, Dardik A, Cheema U. Current advancements and strategies in tissue engineering for wound healing: a comprehensive review. Adv Wound Care. 2017;6:191–209.
Korrapati PS, Karthikeyan K, Satish A, Krishnaswamy VR, Venugopal JR, Ramakrishna S. Recent advancements in nanotechnological strategies in selection, design and delivery of biomolecules for skin regeneration. Mater Sci Eng C Mater Biol Appl. 2016;67:747–65.
Hormozi M, Assaei R, Boroujeni MB. The effect of aloe vera on the expression of wound healing factors (TGFbeta1 and bFGF) in mouse embryonic fibroblast cell: In vitro study. Biomed Pharmacother. 2017;88:610–6.
Klempaiová M, Dragúňová J, Kabát P, Hnátová M, Koller J, Bakoš D. Cytotoxicity testing of a polyurethane nanofiber membrane modified with chitosan/β-cyclodextrin/berberine suitable for wound dressing application: evaluation of biocompatibility. Cell Tissue Bank. 2016;17:665–75.
Khezri K, Farahpour MR, Mounesi Rad S. Accelerated infected wound healing by topical application of encapsulated Rosemary essential oil into nanostructured lipid carriers. Artif Cells, Nanomed, Biotechnol. 2019;47:980–8.
Dadras Chomachayi M, Solouk A, Akbari S, Sadeghi D, Mirahmadi F, Mirzadeh H. Electrospun nanofibers comprising of silk fibroin/gelatin for drug delivery applications: thyme essential oil and doxycycline monohydrate release study. J Biomed Mater Res Part A. 2018;106:1092–103.
Garcia-Orue I, Gainza G, Gutierrez FB, Aguirre JJ, Evora C, Pedraz JL, et al. Novel nanofibrous dressings containing rhEGF and Aloe vera for wound healing applications. Int J Pharmaceutics. 2017;523:556–66.
Oryan A, Mohammadalipour A, Moshiri A, Tabandeh MR. Topical application of aloe vera accelerated wound healing, modeling, and remodeling. Ann Plast Surg. 2016;77:37–46.
El-Kased RF, Amer RI, Attia D, Elmazar MM. Honey-based hydrogel: in vitro and comparative in vivo evaluation for burn wound healing. Sci Rep. 2017;7:9692.
Dwivedi C, Pandey I, Pandey H, Patil S, Mishra SB, Pandey AC, et al. In vivo diabetic wound healing with nanofibrous scaffolds modified with gentamicin and recombinant human epidermal growth factor. J Biomed Mater Res Part A. 2018;106:641–51.
Zahedi P, Fallah-Darrehchi MJF. Electrospun egg albumin-PVA nanofibers containing tetracycline hydrochloride: morphological, drug release, antibacterial, thermal and mechanical properties. Fibers and Polymers. 2015; 16, 2184–92.
López-Iglesias C, Barros J, Ardao I, Monteiro FJ, Alvarez-Lorenzo C, Gómez-Amoza JL, et al. Vancomycin-loaded chitosan aerogel particles for chronic wound applications. Carbohydr Polym. 2019;204:223–31.
Monteiro N, Martins M, Martins A, Fonseca NA, Moreira JN, Reis RL, et al. Antibacterial activity of chitosan nanofiber meshes with liposomes immobilized releasing gentamicin. Acta Biomaterialia. 2015;18:196–205.
Jin H, Zhang Z, Wang C, Tang Q, Wang J, Bai X, et al. Melatonin protects endothelial progenitor cells against AGE-induced apoptosis via autophagy flux stimulation and promotes wound healing in diabetic mice. Exp Mol Med. 2018;50:154.
Asai J, Takenaka H, Hirakawa S, Sakabe J, Hagura A, Kishimoto S, et al. Topical simvastatin accelerates wound healing in diabetes by enhancing angiogenesis and lymphangiogenesis. Am J Pathol. 2012;181:2217–24.
Elsherbiny A, Hogger DC, Borozadi MK, Schmidt CA, Plock J, Largo RD, et al. EPO reverses defective wound repair in hypercholesterolaemic mice by increasing functional angiogenesis. J Plast Reconstr Aesthet Surg. 2012;65:1559–68.
Ghayempour S, Montazer M, Mahmoudi Rad M. Encapsulation of aloe vera extract into natural tragacanth gum as a novel green wound healing product. Int J Biol Macromol. 2016;93:344–9.
Bui VKH, Park D, Lee YC. Chitosan combined with ZnO, TiO2 and Ag nanoparticles for antimicrobial wound healing applications: a mini review of the research trends. Polymers. 2017;9:21.
Miller KJ, Brown DA, Ibrahim MM, Ramchal TD, Levinson H. MicroRNAs in skin tissue engineering. Adv Drug Deliv Rev. 2015;88:16–36.
Laiva AL, O’Brien FJ, Keogh MB. Innovations in gene and growth factor delivery systems for diabetic wound healing. J Tissue Eng Regen Med. 2018;12:e296–312.
Chouhan D, Dey N, Bhardwaj N, Mandal BB. Emerging and innovative approaches for wound healing and skin regeneration: current status and advances. Biomaterials. 2019;216:119267.
Martin JR, Nelson CE, Gupta MK, Yu F, Sarett SM, Hocking KM, et al. Local delivery of PHD2 siRNA from ROS-degradable scaffolds to promote diabetic wound healing. Adv Health Mater. 2016;5:2751–7.
Yildirimer L, Thanh NT, Seifalian AM. Skin regeneration scaffolds: a multimodal bottom-up approach. Trends Biotechnol. 2012;30:638–48.
Peplow PV, Baxter GD. Gene expression and release of growth factors during delayed wound healing: a review of studies in diabetic animals and possible combined laser phototherapy and growth factor treatment to enhance healing. Photomed Laser Surg. 2012;30:617–36.
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 2008;16:585–601.
Borena BM, Martens A, Broeckx SY, Meyer E, Chiers K, Duchateau L, et al. Regenerative skin wound healing in mammals: state-of-the-art on growth factor and stem cell based treatments. Cell Physiol Biochem. 2015;36:1–23.
Ali Khan Z, Jamil S, Akhtar A, Mustehsan Bashir M, Yar M. Chitosan based hybrid materials used for wound healing applications- a short review. Int J Polym Mater Polym Biomater. 2019;68:1–18.
Mogosanu GD, Grumezescu AM. Natural and synthetic polymers for wounds and burns dressing. Int J Pharm. 2014;463:127–36.
Norouzi M, Boroujeni SM, Omidvarkordshouli N, Soleimani M. Advances in skin regeneration: application of electrospun scaffolds. Adv Health Mater. 2015;4:1114–33.
Skardal A, Mack D, Kapetanovic E, Atala A, Jackson JD, Yoo J, et al. Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl Med. 2012;1:792–802.
Chen F-M, Liu X. Advancing biomaterials of human origin for tissue engineering. Prog Polym Sci. 2016;53:86–68.
Imani R, Yousefzadeh M, Nour S. Functional nanofiber for drug delivery applications. In: Barhoum A, Bechelany M, Makhlouf A, editors. Handbook of nanofibers. Cham: Springer International Publishing; 2018. p. 1–55.
Liu M, Duan XP, Li YM, Yang DP, Long YZ. Electrospun nanofibers for wound healing. Mater Sci Eng C Mater Biol Appl. 2017;76:1413–23.
Chou S-F, Gunaseelan S, Kiellani MHH, Thottempudi VVK, Neuenschwander P, Nie H. A review of injectable and implantable biomaterials for treatment and repair of soft tissues in wound healing. J Nanotechnol. 2017;2017:1–15.
Pereira RF, Barrias CC, Granja PL, Bartolo PJ. Advanced biofabrication strategies for skin regeneration and repair. Nanomed. 2013;8:603–21.
Dimatteo R, Darling NJ, Segura T. In situ forming injectable hydrogels for drug delivery and wound repair. Adv Drug Deliv Rev. 2018;127:167–84.
Tang Z, Okano T. Recent development of temperature-responsive surfaces and their application for cell sheet engineering. Regenerative Biomater. 2014;1:91–102.
Chen H, Guo L, Wicks J, Ling C, Zhao X, Yan Y, et al. Quickly promoting angiogenesis by using a DFO-loaded photo-crosslinked gelatin hydrogel for diabetic skin regeneration. J Mater Chem B. 2016;4:3770–81.
Huang J, Chen L, Gu Z, Wu J. Red jujube-incorporated gelatin methacryloyl (GelMA) hydrogels with anti-oxidation and immunoregulation activity for wound healing. J Biomed Nanotechnol. 2019;15:1357–70.
Huang J, Chen L, Yuan Q, Gu Z, Wu J. Tofu-based hybrid hydrogels with antioxidant and low immunogenicity activity for enhanced wound healing. J Biomed Nanotechnol. 2019;15:1371–83.
Griffin DR, Weaver WM, Scumpia PO, Di Carlo D, Segura T. Accelerated wound healing by injectable microporous gel scaffolds assembled from annealed building blocks. Nat Mater. 2015;14:737–44.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nour, S., Baheiraei, N., Imani, R. et al. A review of accelerated wound healing approaches: biomaterial- assisted tissue remodeling. J Mater Sci: Mater Med 30, 120 (2019). https://doi.org/10.1007/s10856-019-6319-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6319-6