Abstract
While many synthetic ceramic bone graft substitutes (BGSs) have osteoconductive properties (e.g. provide a physical scaffold for osteointegration of surrounding bone tissue), certain BGSs are osteostimulative in that they actively upregulate mesenchymal stem cell proliferation and stimulate differentiation into osteoblast-like cells. The osteostimulative properties of silicate-substituted calcium phosphate with enhanced porosity (SiCaP EP) were evaluated in vitro with STRO-1+ immunoselected human bone marrow derived mesenchymal stem cells (HBMSCs). Osteostimulative materials (SiCaP) and Bioglass 45S5 (Bioglass) were also assessed as positive controls along with non-silicate substituted hydroxyapatite as a negative control. HBMSCs were also assessed on Thermanox discs cultured in basal and osteogenic media to determine when osteogenic differentiation could be significantly detected with this in vitro cell system. HBMSC viability and necrosis, total DNA content, alkaline phosphatase (ALP) expression, and osteocalcin expression were evaluated after 7, 14, 21, and 28 days. It was demonstrated that SiCaP EP is osteostimulative based on its propensity to support STRO-1+ HBMSC proliferation and ability to promote the differentiation of HBMSCs down the osteoblastic lineage from ALP-expressing, matrix-producing osteoblasts to Osteocalcin-producing pre-osteocytes without the presence of external osteogenic factors. SiCaP EP permitted greater HBMSC attachment as well as ALP and Osteocalcin expression than Bioglass which may be attributed to its microstructure and chemistry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Efficacious synthetic bone graft substitutes (BGSs) are in demand due to the drawbacks of bone autograft (co-morbidities associated with second surgery [1]), allografts (risk of disease transmission and immunogenic response [1]), as well as potential complications associated with bone morphogenetic proteins (osteolysis, ectopic bone formation, retrograde ejaculation [2]). While many synthetic BGSs claim to be osteoconductive, in that they provide a physical scaffold for osteointegration of surrounding bone tissue, certain BGSs have the added advantage of being osteostimulative. Like osteoinductive materials, osteostimulative materials are able to actively upregulate mesenchymal stem cell proliferation and stimulate differentiation into osteoblast-like cells.
In-vivo, mesenchymal stem cells (MSCs) migrate to sites of damage and differentiate into the required cell type [3]; thus they play a vital role in tissue repair. In-vitro, MSCs can be directed along a restricted set of lineages in the presence of soluble factors; for example, the addition of β-glycerophosphate, ascorbic acid and dexamethasone results in commitment to the osteoblast lineage [4, 5]. This is a complex, highly regulated process involving the parallel and sequential expression of lineage specific genes. Alkaline phosphatase is produced early in the process, initially in parallel with osteoid production, then declining as matrix mineralization occurs [6]. Proteins such as Osteocalcin are secreted by osteoblasts later in the bone formation process and are incorporated into osteoid, the organic phase of bone [7]. The clinical efficacy of silicate-substituted calcium phosphate (SiCaP) has been demonstrated in spinal fusion [8] and foot and ankle procedures [9]. Several preclinical studies have been published verifying the osteoconductivity of SiCaP both as a bone void filler [10, 11] as well as for posterolateral spinal fusion [12]. SiCaP has a regulatory claim as being osteostimulative based on cell culture studies that showed that cellular responses, such as metabolic activity and proliferation, were accelerated when compared to an identical calcium phosphate material that did not contain silicate [13]. Other BGSs that contain Bioglass 45S5 (Bioglass) likewise have an osteostimulative claim defined as active stimulation of osteoblast proliferation and differentiation as evidenced by increased levels of DNA synthesis and of the osteoblast markers Osteocalcin and alkaline phosphatase [14–17].
The purpose of this study was to verify the osteostimulative potential of a new formulation of SiCaP with enhanced porosity (SiCaP EP). While SiCaP and SiCaP EP have the same chemical composition, SiCaP EP has increased strut porosity which mimics the microporous osteocyte lacunae network present in physiological bone. In common research terms, microporosity and strut porosity are used interchangeably. Strut pores are formed from the interconnected spaces existing between particles of calcium phosphate which have been sintered together to form the struts in the SiCaP EP scaffold. The term “strut-porosity” is used to describe the pore volume fraction of each strut.
The osteostimulative behavior of SiCaP EP was assessed by culturing STRO-1+ immunoselected human bone marrow derived mesenchymal stem cells (HBMSCs) in vitro. Since SiCaP and Bioglass are established osteostimulative BGSs, and non-silicate substituted hydroxyapatite (HA) is not considered osteostimulative; these materials were included as positive and negative controls, respectively. To verify whether osteogenic differentiation could be significantly detected with this in vitro cell system, HBMSCs were cultured on Thermanox (TMX) discs in osteogenic medium that contained ascorbic acid, β-glycerophosphate, and dexamethasone (factors that direct MSC differentiation to an osteoblastic cell line) and compared to HBMSCs cultured on TMX discs in basal medium that did not contain osteogenic factors. HBMSC viability and necrosis, proliferation as measured with DNA content, early osteogenic differentiation as assessed by alkaline phosphatase expression, and late osteogenic differentiation marker as measured by Osteocalcin expression was assessed after 7, 14, 21, and 28 days of culture.
2 Materials and methods
2.1 Cell isolation
Mesenchymal stem cells were obtained from bone marrow cell aspiration obtained from a haematologically normal male patient aged 27 years undergoing routine surgical intervention (bone marrow aspirate injection to non-unions in ulna and radius—Royal National Orthopaedic Hospital, Stanmore, UK). Consent was given by the patient to obtain bone marrow during their surgery, and the consent forms from the donor were signed and witnessed. Ethical approval was gained from the NHS Health Research Authority, National Research Ethical Committee London—Stanmore. Marrow cells were harvested using Minimal Essential Medium—alpha modification (αMEM: Gibco/Invitrogen/Life Technologies: Grand Island, NY, USA) alone from trabecular bone marrow samples and pelleted by centrifugation at 500 g for 5 min at 4 °C. The cell pellet was re-suspended in 10 ml αMEM and passaged through nylon mesh (70 μm pore size; Lockertex, Warrington, England). Samples of cell suspension were diluted with 0.4 % Trypan Blue solution (Sigma, UK) and the number and viability of nucleated cells determined. HBMSCs were maintained in α-MEM supplemented with 10 % FCS (Fetal Calf Serum: Gibco/Invitrogen/Life Technologies, Grand Island, NY, USA)/1 % Pen-strep (Gibco/Invitrogen/Life Technologies: Grand Island, NY, USA) at 37 °C in a 5 % humidified atmosphere.
After the first passage, when cells reached 80–85 % confluence, they were subjected to immunomagnetic cell sorting [18] using anti-STRO-1+, Alexa Fluor 647 and MACS anti-Alexa Fluor 647 MicroBeads® (Miltenyi Biotec, Bergisch Gladbach, Germany) antibodies. After trypsinization, cells were re-suspended in MACS Running Buffer (Miltenyi Biotec, Bergisch Gladbach, Germany). Cells were incubated on ice for 15 min with anti-STRO-1+ conjugated to Alexa Fluor 647 solution. Cells were then washed three times with the running buffer. Two hundred microliters of anti-Alexa Fluor 647 MicroBeads (Miltenyi Biotec, Surrey, UK) were added. Cells were incubated for 30 min on ice and then washed and re-suspended in 1 ml MACS running buffer.
Finally, cells were applied to magnetic sorting separation columns (Miltenyi Biotec) and separated into positively and negatively STRO-1+ labeled fractions by using a QuadroMACS separation unit and LS columns (Miltenyi Biotec). The STRO-1+ cell fraction was seeded in new separate 225 ml flasks in basic medium at a concentration of 30 cells/cm2. In order to obtain sufficient cell numbers for the required seeding densities, the cells underwent expansion to two passages.
2.2 Test materials
Five test articles were assessed in this study. Nunc Thermanox coverslips (Thermo Fisher Scientific: Waltham, MA, USA) with 13 mm diameter and 0.2 mm thickness were used as the control substrates to assess the basal versus osteogenic conditions. Bioglass 45S5 particles in a polyethylene glycol and glycerine carrier (Bioglass) were included as a positive control. SiCaP, SiCaP EP, and hydroxyapatite (HA) implants were manufactured as described previously [19–21]. Both SiCaP and SiCaP EP consisted of porous, irregularly shaped microgranules (1–2 mm) of phase pure silicate-substituted calcium phosphate (0.8 wt% Si) in an aqueous poloxamer carrier. The SiCaP and HA granules had a mean total porosity of 80 % and a mean strut porosity of 22.5 %, while the SiCaP EP granules had a mean total porosity of 82.5 % and a mean strut porosity of 39 %. Material characterization of chemical composition, density, total porosity, and strut porosity were measured as described previously [22]. SiCaP and SiCaP EP granules were imaged Scanning Electron Microscopy to assess the differences in strut porosity.
2.3 Experimental design
Ultra-low attachment 24 well plates (Corning Costar, Sigma Aldrich, UK) were used in all of the culture studies in order to isolate the effects of the test material on the cell population from the effects of the tissue culture plastic on the cell population. Seven cell culture systems were set up in all: empty wells with basal media, Thermanox disc in basal media (TMX basal control), Thermanox disc in osteogenic media (TMX osteogenic control), non silicate-substituted hydroxyapatite in basal media (HA), SiCaP in basal media (SiCaP), Bioglass in basal media (Bioglass), and SiCaP EP in basal media (SiCaP EP).
Test articles were weighed into each well and were normalized for the relative content of calcium salt of each device so that each well received 0.25 g calcium salt (Table 1). Prior to cell seeding, each substrate was incubated in 2 ml of media for 4 h. Basal media contained α-MEM supplemented with 10 % FCS/Pen-strep. Osteogenic media contained 90 % α-MEM, 10 % FCS, 50 ug/mL ascorbic acid (VWR BDH Prolabo: Leicestershire, England), 5 mM β-glycerophosphate (Calbiochem/Merck: Darmstadt, Germany), 100 nM dexamethasone (added fresh) (Alfa Aesar: Ward Hill, MA, USA), and 1 % Pen-Strep.
After the pre-incubation period, HBMSCs were seeded onto the substrates and the empty wells at a density of 2 × 104 cells/sample (or 2 × 104 cells/well). Substrates were not removed from the pre-incubation medium prior to cell seeding. HBMSCs were maintained at 37 °C in a 5 % humidified atmosphere. Well plates were cultured for 7, 14, 21 or 28 days and medium was changed every 3.5 days. During medium changes, 1 ml of the old media was aspirated from the top of the well and replaced with 1 ml of fresh media to avoid aspiration of the test article and/or HBMSCs. A 24 well plate for each test article/culture condition at each time point was set up: six wells were used for cell viability/necrosis analysis, six wells were used for DNA analysis, six wells were used for alkaline phosphatase (ALP) analysis, and six wells were used as spares so that N = 6 samples were assessed with each analytical method at each time point with an extra six wells available as spares. At each time point; the medium supernatant from the cultures dedicated for DNA and cell viability/necrosis assays were aspirated from each well plate and individually stored for the Osteocalcin assay (−80 °C) according to the assay manufacturer’s recommendations (N = 12 per time point). After removal of the supernatant from the wells at the respective 7, 14, 21, or 28 day time point; the Thermanox discs, HA, SiCaP, Bioglass, SiCaP EP and empty wells were assayed for viability/necrosis, total DNA and ALP.
2.4 Cell viability and necrosis
CellTracker Green (CTG) was used to label viable cells and Ethidium Homodimer-1 (EH-1: Molecular Probes: Paisley, United Kingdom) for necrotic cell nuclei (live/dead stain). The samples were washed in PBS and incubated for 45 min in 1 ml of standard CTG/EH-1 solution (10 µg/ml CTG, 5 µg/ml EH-1) [23]. After incubation, cells were observed by fluorescence microscopy (Diaphot, Nikkon, UK). Results were presented in a table of observations comparing the treatment groups and the controls. No statistical analysis was conducted for this test.
2.5 DNA content
Total DNA was determined using a standard DNA PicoGreen assay. In brief, cells were fixed in 70 % ethanol. The cells were then lysed in 0.5 mL of 0.05 % Triton X-100 (Sigma-Aldrich, Gillingham, United Kingdom) before undergoing three freeze–thaw cycles (15 min at −80 °C followed by 15 min at ambient temperature). Cell lysate was measured for DNA content using PicoGreen (Molecular Probes, Paisley, United Kingdom) according to the manufacturer’s protocol [24]. This assay is an ultra-sensitive fluorescent nucleic acid stain of double-stranded DNA. The PicoGreen dsDNA Quantitation Reagent is supplied as a concentrated dye solution in anhydrous dimethylsulfoxide (DMSO). Used in conjunction with the Fluorospectrometer, the PicoGreen assay provides a highly sensitive means of dsDNA quantitation with minimal consumption of sample and allows a quantification range of 50 pg to 2 µg.
The samples were analyzed using a Fluoroskan Ascent Microplate Fluorometer (Thermo Scientific: Waltham, MA, USA) and fluorescence observed using 510 nm excitation and 590 nm emission. Data were compared with a standard curve previously determined. At the end of the study a quantitative statistical comparison of the TMX basal control versus TMX osteogenic control was conducted to determine at which time points a significant difference could be observed. SiCaP EP was also quantitatively and statistically compared to HA, SiCaP, and Bioglass.
2.6 Alkaline phosphatase (ALP) expression
ALP in the cell lysate (as obtained for the DNA assay) was measured using p-nitrophenyl phosphate (pNPP) as the substrate in 2-amino-2-methyl-1-propanol alkaline buffer solution (Sigma, Poole, United Kingdom) according to the manufacturer’s protocol. Fifty microliters of the staining solution was added to 50 μL of the cell lysate sample, in a well of a 96-well plate. The plates were incubated at room temperature for 30 min [25]. Plates were read at 405 nm (Bio Rad Microplate Reader: Hercules, CA, USA). Data were compared with a standard curve previously determined and ALP specific activity expressed as nM pNPP/hour/ng DNA.
At the end of the study a quantitative comparison of the TMX basal control versus TMX osteogenic control was conducted to determine at which time points a significant difference could be observed. SiCaP EP was also quantitatively and statistically compared to HA, SiCaP, and Bioglass.
2.7 Osteocalcin expression
After the incubation period, cell culture supernatant was aspirated and stored at −80 °C. The Osteocalcin concentration was assayed using a Gla-Type Osteocalcin High Sensitive ELISA kit (Takara: Saint-Germain-en-Laye, France) [26]. Briefly, 100 μL of the supernatant was aspirated and added to a well in the antibody-coated 96-well plate. The plate was incubated at room temperature for 2 h. The sample was removed and the well washed three times with PBS. The antibody-POD conjugate solution (100 μL) was added to the well and the plate incubated for 1 h at room temperature. The solution was discarded and the well washed four times with PBS. The substrate solution (3,3′,5,5′-Tetramethylbenzidine solution) was then added and the plate incubated for 15 min. The stop solution (1 N sulphuric acid) was then added and the plate read immediately at 450 nm (Bio Rad Microplate Reader). At the end of the study a quantitative comparison of the TMX basal control versus TMX osteogenic control was conducted to determine at which time points a significant difference could be observed. SiCaP EP was also quantitatively and statistically compared to HA, SiCaP, and Bioglass.
2.8 Statistical analysis
Statistical analysis of the means for the parameters was performed with SPSS software (version 10.1; SPSS, Chicago, Illinois) using a Mann–Whitney U test at a risk α = 5 %. The Mann–Whitney U test (also called the Mann–Whitney–Wilcoxon (MWW) or Wilcoxon rank-sum test) is a non-parametric statistical hypothesis test for assessing whether two independent samples of observations have equally large values. Statistical differences between groups were identified.
3 Results
While both SiCaP and SiCaP EP consists of porous 1–2 mm granules containing silicate-substituted calcium phosphate suspended in an aqueous gel carrier, they differ in the amount of strut porosity which can only be observed on the microscopic level. Scanning Electron Microscopy images show that SiCaP EP has a greater amount of strut porosity in the 0.2–50 micron size range compared to SiCaP (Fig. 1).
During the cell culture studies, all the test materials were easily handled. After 2 h of incubation, the test article carriers in SiCaP, SiCaP EP, and Bioglass were dissolved. From the first day of culture until the 28th day (the longest time-point) the media from the Bioglass test group presented a fuchsia color which indicated a basic media. At the 21st day, the pH of all media was measured (Table 2). All groups except Bioglass presented a pH that was close to neutral pH, while the Bioglass media had a pH of 8.7. The HA group also presented a fuchsia color indicating a basic media, but only in the day zero samples. After the first media change, the color was characteristic of a pH between 6.8 and 8.2. Inversely, the media of SiCaP and SiCaP EP had a tendency to a yellow color on day 0, indicating a light acidity of the media. After the first media change, the color became normal.
Light microscopy analysis of the empty well group (negative control in which cells were seeded directly into the wells of non-adherent tissue culture plastic without the addition of a test article) demonstrated that cells did not adhere to the well plate itself. This therefore validates the use of these non-adherent well plates to minimize the confounding effect of cells proliferating and differentiating after attachment to the tissue culture plastic instead of (or in addition to) the test article in the other treatment groups.
Fungal contamination occurred in various plates, predominantly in the longer experiments. However, contamination did not occur in more than six wells in any plate. Therefore, the contamination did not compromise the experiment since the spare wells were available as replacements.
Light microscopy images taken of the cultured plates after 14 days indicated that cells attached and spread over the TMX substrates. Conversely the cells did not attach to the non-adherent tissue culture plastic in empty wells, rather the cells formed clumps which were suspended in the media.
3.1 Cell viability and necrosis
The cells were assessed with a live/dead cell assay. Because of the opacity of the materials, it was very difficult to properly visualize the cells, as the substrates prevented light transmission. However, it was possible to visualize a certain amount of cells in all the treatments. As this was a qualitative analysis, the percentage of living cells, compared with dead cells, was classified from (−) to (+++) (Table 3).
The results of cell viability and necrosis assay indicate that all test groups were able to sustain live human bone marrow derived mesenchymal stem cells out to 28 days. Over 90 % of cells in wells containing the TMX basal control, TMX osteogenic media, HA, SiCaP, and SiCaP EP were live cells according to this assay. The proportion of live cells in the Bioglass treatment group was lower than for the other treatment groups. The estimated range was between 40 and 90 % based on this assay.
3.2 Total DNA
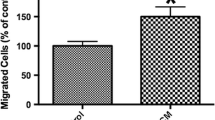
The DNA assay demonstrated a trend for increasing cell proliferation in the TMX basal and osteogenic controls over the 28 day period (Fig. 2a). There were more cells proliferating on TMX in the osteogenic medium than basal medium at 21 and 28 days, although this did not reach statistical significance using a non-parametric Mann–Whitney–Wilcoxon test (p = 0.065) but did with a student t test after confirming both populations were normal in distribution (p < 0.05). There was a significantly greater amount of HBSMCs proliferating on SiCaP EP (p < 0.05) than HA at 7, 14, and 21 days and was equivalent at 28 days (Fig. 2b). The amount of HBMSCs proliferating on SiCaP EP was significantly greater (p < 0.05) than SiCaP at 7 and 14 days and was equivalent at 21 and 28 days (Fig. 2c). There was significantly greater HBMSC proliferation on SiCaP EP (p < 0.05) than Bioglass at all time-points (Fig. 2d).
3.3 Alkaline phosphatase (ALP)
The amount of ALP detected in the well plates corresponded with the increase in cell number for the basal and osteogenic controls (Fig. 3a). There was a greater amount of ALP detected in well plates containing TMX discs and osteogenic medium than those containing TMX discs and basal medium at 28 days, although this did not reach statistical significance using a non-parametric Mann–Whitney–Wilcoxon test (p = 0.065) but did with a student t test after confirming both populations were normal in distribution (p < 0.05). There was a peak in ALP expression at day 14 and day 28 for both Thermanox controls (Fig. 3a).
ALP expression per unit cell DNA on SiCaP EP was generally flat across the time course (Figs. 3b–d). There was significantly more (p < 0.05) ALP expression normalized to cell DNA for HA than SiCaP EP at 7, 14, and 21 days but not at 28 days (Fig. 3b). ALP expression peaked at around day 21 for the HA group. Peak ALP expression per unit cell DNA was observed for SiCaP over the period 0–14 days (Fig. 3c). The amount of ALP expressed per unit DNA was statistically higher (p < 0.05) in the SiCaP EP test group compared to the SiCaP test group at 21 and 28 days (Fig. 3c). There was significantly more (p < 0.05) ALP expression in the SiCaP EP group compared to the Bioglass group at all time-points (Fig. 3d). Peak ALP expression was observed at day 28 for the Bioglass group.
3.4 Osteocalcin
There was a general trend for an increase in Osteocalcin production over the 28 day period for cells cultured in osteogenic media whereas for cells cultured in basal media there was a general trend for a decrease in Osteocalcin over the same period (Fig. 4a). There was significantly more Osteocalcin detected for cells cultured in basal media at 7 and 14 days when compared to cells cultured in osteogenic media (Fig. 4a). There was significantly more Osteocalcin detected for cells cultured in osteogenic media at 28 days when compared to cells cultured in basal media (Fig. 4a).
Osteocalcin production was significantly higher (p < 0.05) in the SiCaP EP group than the HA group at all time-points (Fig. 4b). There was no evidence of any increase in Osteocalcin production across the study for the HA control. There was significantly more (p < 0.05) Osteocalcin production in cells cultured at 7 days on SiCaP compared to SiCaP EP, but at all other time-points overall Osteocalcin production was equivalent (Fig. 4c). Peak production of Osteocalcin was between 3 and 7 days for SiCaP and between 7 and 11 days for SiCaP EP. Overall Osteocalcin production was significantly higher (p < 0.05) in the SiCaP EP group than the Bioglass group at 14, 21, 28 days, but Osteocalcin production was significantly higher (p < 0.05) for Bioglass than SiCaP EP at 7 days (Fig. 4d). Peak Osteocalcin production occurred during the 3–7 day period for the Bioglass group.
4 Discussion
Osteostimulative materials provide an efficacious option amongst synthetic bone graft materials due to their ability to upregulate mesenchymal stem cell attachment, proliferation, and direct their differentiation into osteoblast-like cells. This is similar to the behavior of osteoinductive growth factors, but avoids the detrimental side effects associated with supraphysiological doses of bone morphogenetic proteins [27]. Previous studies have pursued various approaches to modify synthetic calcium phosphate materials to direct osteogenic differentiation of stem cells, including altering the chemical composition and modifying the physical structure.
Coating calcium phosphates with polymeric materials (including silk [28, 29] and electrospun poly(d,l-lactide-co-glycolide) fibers [30] ) were observed to increase osteogenic differentiation of stem cells. Enhanced osteogenic differentiation was also demonstrated by doping calcium phosphates with metals including zinc [31], magnesium [32], and strontium [33]. Previous investigations have shown that increasing the silicon content of hydroxyapatite [34] and adding mesoporous silicon particles to electrospun poly (ε-caprolactone) [35] stimulated stem cell attachment and differentiation. Additionally, Cameron et al. previously compared human mesenchymal stem cell (hMSC) response to silicate substituted calcium phosphate (Si-CaP) and non-silicated HA [36]. Compared to non-silicated HA, it was found that Si-CaP supported greater attachment and proliferation of hMSCs and also induced osteogenesis to a greater extent than HA as evidenced through up-regulation of osteoblast-related genes, presence of osteogenic-associated proteins, and production of mineralized matrix. These results corroborate the observation in this current study that the presence of silicon increases bone producing potential.
It has been hypothesized that substrate structure affects mesenchymal cell growth and differentiation processes via topography sensing and mechanotransduction [37]. Potential topography sensing mechanisms include formation of focal adhesion complexes which can modulate intracelluar signaling cascades, the deformation of the cytoskeleton and nuclear membranes which can open nucleopores and increase transport of mRNA molecules and subsequent protein translation, and curvature sensing mechanisms which can generate vesicle trafficking of proteins and thus serve as geometry sensors. Mechanotransduction refers to the translation of physical processes driven by surface geometry (e.g. hydrodynamic and elastic forces caused by cytoskeletal reorganization) into biomolecular interactions. Hypothesized mechanisms of mechanotransduction include transcription activation of specific genes in response to changes in nuclear morphology and chromosomal locations, tension-induced integration of actin and tubulin filaments activating local focal adhesion kinase phosphorylation and signal transduction towards the nucleus via microtubules, or stretching of actin stress fibers with focal adhesion complexes which change the position and proximity of signaling proteins thereby initiating an altered signaling cascade [37].
Several studies have investigated the effect of calcium phosphate microstructure and nanostructure on stem cell differentiation. For example, nano-sized hydroxyapatite has been used as a composite with poly(d,l-lactic acid) (PLA) [38] and also as a coating for porous biphasic calcium phosphate ceramics [39] producing materials capable of supporting mesenchymal stem cell proliferation and osteogenic differentiation. Lee et al. developed porous scaffolds of calcium phosphate cement combined with alginate, and determined that scaffolds with the highest porosity investigated showed favorable mesenchymal stem cell proliferation and osteogenic differentiation [40].
The main strategy employed in this study was to maintain the demonstrated efficacy of the silicate-substituted calcium phosphate chemistry, but to enhance its osteostimulative attribute by increasing the microporosity of the scaffold. By mimicking the porous strut network of trabecular bone, it was hypothesized that SiCaP EP would provide an ideal microenvironment to direct mesenchymal stem cell attachment, proliferation, and osteogenic differentiation.
A DNA assay was included in this study to determine whether human bone marrow derived mesenchymal stem cells were able to survive, attach, and proliferate on each of the test materials and control articles. Cells were able to attach to the Thermanox discs in both basal and osteogenic media (Fig. 2a). In these conditions cells proliferated increasingly over the 28 day experimental period as indicated by an increase in the amount of cell DNA detected.
The SiCaP EP group sustained the largest population of cells compared to all other controls and treatment groups at the earlier time-points, and there was no decline in cell number over the latter time-points as the number of cells found on most other treatment groups increased to an equivalent level. This observation could either be attributed to a greater propensity of the SiCaP EP scaffold to sustain larger amounts of cell attachment and proliferation in the period 0–14 days; or a greater propensity of the scaffolds in the positive control test groups to contribute to cell death and/or inhibition of initial cell attachment and proliferation at earlier time-points; or a combination of all of these factors.
Alkaline phosphatase (ALP) is produced early in the osteoblastic lineage, initially in parallel with osteoid production, then declining as matrix mineralization occurs and so was used in this study as a marker for early stage differentiation [6]. Proteins such as Osteocalcin are secreted by osteoblasts and are incorporated into osteoid, the organic phase of bone [7]. Osteocalcin is a late stage marker for osteoblastic lineage. Osteocalcin is secreted by osteoblasts as the matrix is mineralizing around them, and thus was used in this study as a measure for later stage osteoblastic differentiation.
When analyzing ALP normalized for DNA content, cells cultured on Thermanox appeared to have peak ALP expression at 14 and 28 days when cells were cultured in either basal or osteogenic medium. This sequential pattern of differentiation into mature osteoblasts was similar to the temporal pattern observed in HBMSCs in a previous study assessing silicate substituted calcium phosphate [36].
ALP production normalized to DNA remained greater for SiCaP EP treatments compared to SiCaP at 21 and 28 days and Bioglass at all time-points. However, the amount of ALP detected per unit of DNA was significantly lower for the SiCaP EP treatment group than that for the HA treatment group at 7, 14, and 21 days and equivalent at 28 days. This suggests that ALP up-regulation for SiCaP EP likely peaked before the 7 day time-point, but later for the HA control group. ALP expression per unit cell DNA was not up-regulated until day 28 in the Bioglass group.
Osteocalcin (or bone gamma-carboxyglutamic acid-containing protein (BGLAP)) is a late stage osteoblast specific protein, produced and exogenously expressed only by mature osteoblasts prior to the onset of mineralization [41]. While more Osteocalcin was detected from cells cultured on TMX discs in basal media compared to osteogenic media at early time points (7 and 14 days), the basal media Osteocalcin levels decreased over time while the osteogenic media Osteocalcin levels increased over time. At 28 days, more Osteocalcin was detected from cells cultured on TMX in osteogenic media compared to those in basal media.
The SiCaP EP group exhibited greater Osteocalcin expression compared to the HA group at all time points. The HA test article did not trigger Osteocalcin secretion in osteoblasts attached to the material substrate and this did not change over the entire duration of the study.
Osteocalcin production was equivalent between the SiCaP EP and SiCaP groups except at 7 days. Peak Osteocalcin production was observed at 7 days for the SiCaP group and between 7 and 11 days for the SiCaP EP group. Cameron et al. likewise reported a substantial increase in Osteocalcin gene up-regulation between days 7 and 14 after culturing human bone marrow derived mesenchymal stem cells on Si-CaP [36].
Osteocalcin production was greater for the SiCaP EP treatment group compared to Bioglass group at all time points except at 7 days. Peak Osteocalcin production was observed at 7 days for Bioglass and decreased from that time-point onwards.
Osteocalcin secretion by differentiated osteoblasts was substantially higher for the SiCaP EP treatment group compared to the HA negative control group indicating that despite the differentiation of stem cells (as confirmed by ALP up-regulation), the HA osteoblasts were less functional and typical of an earlier osteoblastic phenotype relative to differentiating osteoblasts attached to SiCaP EP. Peak Osteocalcin production occurred over an equivalent timeframe (7–14 days) for SiCaP EP and the positive controls Bioglass and SiCaP.
HBMSCs cultured on SiCaP EP had greater attachment, ALP expression, and Osteocalcin production at all time points (except at 7 days for Osteocalcin) compared to Bioglass. The color of the media indicated that the pH of the wells containing Bioglass was alkaline throughout the entire study, while hat the wells containing SiCaP and SiCaP EP were slightly acidic up to the first media change but were neutral from that point on. The media color observations were further substantiated with pH testing at 21 days (Table 2). These observations appear to correspond to observations for the lower amount of cell DNA detected in the Bioglass wells at the corresponding time-points as well as studies reported in the literature which demonstrated that Bioglass 45S5 was observed to cause a pH increase up to 12 which was attributed to the rapid release of protons/cations [42].
It seems plausible that the greater the alkalinity of the media (most probably due to device dissolution and/or buffering), the greater the probability for cell death or inhibitory effect on cell attachment and proliferation. For the Bioglass group, the effect of the device on pH was sustained over the 28 day period which prevented cell attachment and proliferation from reaching the same level as the other groups in the study. In vitro studies have demonstrated that human osteoblast cells cultured on bioactive glass underwent apoptosis and necrosis which was attributed to rapid release of sodium and silicon ions at high concentrations [43]. Conversely, SiCaP and SiCaP EP have a silicon content (0.8 wt%) that more closely resembles the physiological concentration of silicon found in active sites of bone calcification [44] and did not produce the highly alkaline environment observed in the Bioglass group.
A major differentiating factor of this study is that the mesenchymal stem cells cultured on the synthetic substrates were only exposed to basal medium without osteogenic factors. Previous studies assessed MSC behavior on synthetic scaffolds in the presence of osteogenic medium (containing factors like dexamethasone, ascorbic acid, and β–glycerophosphate), thus the cells had a stimulating medium which could direct osteogenic differentiation [28–35, 38–40]. In the current study, it was demonstrated that the synthetic scaffold itself was able to direct stem cell differentiation in the absence of external chemical factors.
Another distinguishing aspect of this study is the use of the STRO-1+ fraction of human mesenchymal stem cells directly isolated from a human donor. Previous studies have used animal stem cells without specifically sorting the MSCs [32–34, 39, 40]. Other studies have used human mesenchymal stem cells either from a commercial source [31, 35] or with no information provided about their origin [29–31, 35]. A variety of cells are found in bone marrow besides mesenchymal stem cells including hematopoietic cells, red blood cells, platelets, white blood cells, fibroblasts, adipocytes, osteoblasts, osteoclasts, and endothelial cells. To ensure that the osteogenic response detected was derived from undifferentiated stem cells, mesenchymal stem cells were immunoselected using the STRO-1+ marker of primitive bone marrow stromal cells [45].
5 Conclusion
SiCaP EP was able to promote the proliferation of an equivalent number of human bone marrow derived mesenchymal stem cells (HBMSCs) compared to the positive controls (Bioglass and SiCaP) as demonstrated through cell DNA analysis. SiCaP EP promoted early-stage differentiation of HBMSCs as demonstrated through equivalent or better up-regulation of ALP expression compared to negative and positive controls. SiCaP EP promoted late-stage differentiation of HBMSCs as demonstrated through up-regulated production of Osteocalcin compared to the negative control and equivalent temporal up-regulation compared to the positive controls. SiCaP EP is osteostimulative based on its propensity to support HBMSC proliferation and promote the differentiation of HBMSCs down the osteoblastic lineage without the presence of external osteogenic factors from ALP-expressing, matrix-producing osteoblasts to Osteocalcin-producing pre-osteocytes. The greater HBMSC attachment, ALP expression, and Osteocalcin production in the SiCaP EP group compared to Bioglass could be attributed to its enhanced microstructure and chemistry.
References
Giannoudis PV, Dinopoulos H, Tsiridis E. Bone substitutes: an update. Injury. 2005;36:S20–7.
Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J. 2011;11:471–91.
Chamberlain G, Fox J, Ashton B, Middleton J. Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells. 2007;25:2739–49.
Beresford JN, Joyner CJ, Devlin C, Triffitt JT. The effects of dexamethasone and 1,25-dihydroxyvitamin D3 on osteogenic differentiation of human marrow stromal cells in vitro. Arch Oral Biol. 1994;39:941–7.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–7.
Stein GS, Lian JB, Owen TA. Relationship of cell growth to the regulation of tissue-specific gene expression during osteoblast differentiation. FASEB J. 1990;4:3111–23.
Glimcher MJ. Recent studies of the mineral phase in bone and its possible linkage to the organic matrix by protein-bound phosphate bonds. Philos Trans R Soc Lond B Biol Sci. 1984;304:479–508.
Jenis LG, Banco RJ. Efficacy of silicate-substituted calcium phosphate ceramic in posterolateral instrumented lumbar fusion. Spine. 2010;35(20):E1058–63.
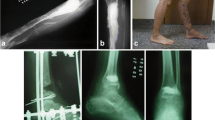
Pomeroy GC, DeBen S. Ankle arthrodesis with silicate-substituted calcium phosphate bone graft. Foot Ankle Online J. 2013;6(1):2.
Hing KA, Revell PA, Smith N, Buckland T. Effect of silicon level on rate, quality and progression of bone healing within silicate-substituted porous hydroxyapatite scaffolds. Biomaterials. 2006;27:5014–26.
Hing KA, Wilson LF, Buckland T. Comparative performance of three ceramic bone graft substitutes. Spine J. 2007;7:475–90.
Wheeler DL, Jenis LG, Kovach ME, Marini J, Turner AS. Efficacy of silicated calcium phosphate graft in posterolateral lumbar fusion in sheep. Spine J. 2007;7:308–17.
ACTIFUSE Indications for Use. Apatech, 25003; October 2009.
Vrouwenvelder WC, Groot CG, de Groot K. Histological and biochemical evaluation of osteoblasts cultured on bioactive glass, hydroxylapatite, titanium alloy, and stainless steel. J Biomed Mater Res. 1993;27:465–75.
Xynos ID, Hukkanen MV, Batten JJ, Buttery LD, Hench LL, Polak JM. Bioglass 45S5 stimulates osteoblast turnover and enhances bone formation In vitro: implications and applications for bone tissue engineering. Calcif Tissue Int. 2000;67:321–9.
Xynos ID, Edgar AJ, Buttery LD, Hench LL, Polak JM. Ionic products of bioactive glass dissolution increase proliferation of human osteoblasts and induce insulin-like growth factor II mRNA expression and protein synthesis. Biochem Biophys Res Commun. 2000;276:461–5.
Bosetti M, Cannas M. The effect of bioactive glasses on bone marrow stromal cells differentiation. Biomaterials. 2005;26:3873–9.
Bensidhoum M, Chapel A, Francois S, Demarquay C, Mazurier C, Fouillard L, Bouchet S, Bertho JM, Gourmelon P, Aigueperse J, Charbord P, Gorin NC, Thierry D, Lopez M. Homing of in vitro expanded Stro-1- or Stro-1+ human mesenchymal stem cells into the NOD/SCID mouse and their role in supporting human CD34 cell engraftment. Blood. 2004;103:3313–9.
Hing KA, Annaz B, Saeed S, Revell PA, Buckland T. Microporosity enhances bioactivity of synthetic bone graft substitutes. J Mat Sci. 2005;16:467–75.
Chiang YM, Birnie DP, Kingery WD. Physical ceramics: principles for ceramic science and engineering. New York: Wiley; 1997.
Hing KA. Bioceramic bone graft substitutes: influence of porosity and chemistry. Int J Appl Ceram Technol. 2005;2:184–99.
Campion C, Chander C, Buckland T, Hing K. Increasing strut porosity in silicate-substituted calcium-phosphate bone graft substitutes enhances osteogenesis. J Biomed Mater Res B. 2011;97(2):245–54.
Yang XB, Webb D, Blaker J, Boccaccini AR, Maquet V, Cooper C, Oreffo RO. Evaluation of human bone marrow stromal cell growth on biodegradable polymer/bioglass composites. Biochem Biophys Res Commun. 2006;342:1098–107.
Wang Y, Volloch V, Pindrus MA, Blasioli DJ, Chen J, Kaplan DL. Murine osteoblasts regulate mesenchymal stem cells via WNT and cadherin pathways: mechanism depends on cell–cell contact mode. J Tissue Eng Regen Med. 2007;1:39–50.
Arpornmaeklong P, Brown SE, Wang Z, Krebsbach PH. Phenotypic characterization, osteoblastic differentiation, and bone regeneration capacity of human embryonic stem cell-derived mesenchymal stem cells. Stem Cells Dev. 2009;18:955–68.
Ye CP, Heng BC, Liu H, Toh WS, Cao T. Culture media conditioned by heat-shocked osteoblasts enhances the osteogenesis of bone marrow-derived mesenchymal stromal cells. Cell Biochem Funct. 2007;25:267–76.
Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J. 2011;11(6):471–91.
Li JJ, Gil ES, Hayden RS, Li C, Roohani-Esfahani SI, Kaplan DL, Zreiqat H. Multiple silk coatings on biphasic calcium phosphate scaffolds: effect on physical and mechanical properties and in vitro osteogenic response of human mesenchymal stem cells. Biomacromolecules. 2013;14(7):2179–88.
Zhang Y, Wu C, Friis T, Xiao Y. The osteogenic properties of CaP/silk composite scaffolds. Biomaterials. 2010;31(10):2848–56.
Bao C, Chen W, Weir MD, Thein-Han W, Xu HH. Effects of electrospun submicron fibers in calcium phosphate cement scaffold on mechanical properties and osteogenic differentiation of umbilical cord stem cells. Acta Biomater. 2011;7(11):4037–44.
Luo X, Barbieri D, Davison N, Yan Y, de Bruijn JD, Yuan H. Zinc in calcium phosphate mediates bone induction: in vitro and in vivo model. Acta Biomater. 2014;10(1):477–85.
Hussain A, Bessho K, Takahashi K, Tabata Y. Magnesium calcium phosphate as a novel component enhances mechanical/physical properties of gelatin scaffold and osteogenic differentiation of bone marrow mesenchymal stem cells. Tissue Eng Part A. 2012;18(7–8):768–74.
Mohan BG, Suresh Babu S, Varma HK, John A. In vitro evaluation of bioactive strontium-based ceramic with rabbit adipose-derived stem cells for bone tissue regeneration. J Mater Sci. 2013;24(12):2831–44.
Nair MB, Varma HK, John A. Triphasic ceramic coated hydroxyapatite as a niche for goat stem cell-derived osteoblasts for bone regeneration and repair. J Mater Sci. 2009;20(Suppl 1):S251–8.
Fan D, Akkaraju GR, Couch EF, Canham LT, Coffer JL. The role of nanostructured mesoporous silicon in discriminating in vitro calcification for electrospun composite tissue engineering scaffolds. Nanoscale. 2011;3(2):354–61.
Cameron K, Travers P, Chander C, Buckland T, Campion C, Noble B. Directed osteogenic differentiation of human mesenchymal stem/precursor cells on silicate substituted calcium phosphate. J Biomed Mater Res A. 2013;101(1):13–22.
Ozdemir T, Higgins AM, Brown JL. Osteoinductive biomaterial geometries for bone regenerative engineering. Curr Pharm Des. 2013;19(19):3446–55.
Danoux CB, Barbieri D, Yuan H, de Bruijn JD, van Blitterswijk CA, Habibovic P. In vitro and in vivo bioactivity assessment of a polylactic acid/hydroxyapatite composite for bone regeneration. Biomatter. 2014;4:e27664.
Hu J, Zhou Y, Huang L, Liu J, Lu H. Effect of nano-hydroxyapatite coating on the osteoinductivity of porous biphasic calcium phosphate ceramics. BMC Musculoskelet Disord. 2014;15:114.
Lee GS, Park JH, Shin US, Kim HW. Direct deposited porous scaffolds of calcium phosphate cement with alginate for drug delivery and bone tissue engineering. Acta Biomater. 2011;7(8):3178–86.
Marinucci L, Balloni S, Becchetti E, Bistoni G, Calvi EM, Lumare E, Ederli F, Locci P. Effects of hydroxyapatite and Biostite on osteogenic induction of hMSC. Ann Biomed Eng. 2010;38(3):640–8.
Gubler M, Brunner TJ, Zehnder M, Waltimo T, Sener B, Stark WJ. Do bioactive glasses convey a disinfecting mechanism beyond a mere increase in pH? Int Endod J. 2008;41:670–8.
Gough JE, Clupper DC, Hench LL. Osteoblast responses to tape-cast and sintered bioactive glass ceramics. J Biomed Mater Res A. 2004;69(4):621–8.
Carlisle EM. Silicon: a possible factor in bone calcification. Science. 1970;167(916):279–80.
Stewart K, Monk P, Walsh S, Jefferiss CM, Letchford J, Beresford JN. STRO-1, HOP-26 (CD63), CD49a and SB-10 (CD166) as markers of primitive human marrow stromal cells and their more differentiated progeny: a comparative investigation in vitro. Cell Tissue Res. 2003;313(3):281–90.
Acknowledgments
This research study was funded by Baxter Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Godoy, R.F., Hutchens, S., Campion, C. et al. Silicate-substituted calcium phosphate with enhanced strut porosity stimulates osteogenic differentiation of human mesenchymal stem cells. J Mater Sci: Mater Med 26, 54 (2015). https://doi.org/10.1007/s10856-015-5387-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-015-5387-5