Abstract
Chronic inflammation can irreversibly damage components of the ossicular chain which may lead to sound conduction deafness. The replacement of impaired ossicles with prostheses does not reduce the risk of bacterial infections which may lead to loss of function of the implant and consequently to additional damage of the connected structures such as inner ear, meninges and brain. Therefore, implants that could do both, reconstruct the sound conduction and in addition provide antibacterial protection are of high interest for ear surgery. Layered double hydroxides (LDHs) are promising novel biomaterials that have previously been used as an antibiotic-releasing implant coating to curb bacterial infections in the middle ear. However, animal studies of LDHs are scarce and there exist only few additional data on the biocompatibility and hardly any on the biodegradation of these compounds. In this study, middle ear prostheses were coated with an LDH compound, using suspensions of nanoparticles of an LDH containing Mg and Al as well as carbonate ions. These coatings were characterized and implanted into the middle ear of healthy rabbits for 10 days. Analysis of the explanted prostheses showed only little signs of degradation. A stable health constitution was observed throughout the whole experiment in every animal. The results show that LDH-based implant coatings are biocompatible and dissolve only slowly in the middle ear. They, therefore, appear as promising materials for the construction of controlled drug delivery vehicles.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Chronic otitis media with or without formation of cholesteatoma is often associated with hearing loss due to destruction of the ossicular chain, that is the malleus, incus and stapes [1, 2]. To treat this conductive hearing loss it is usually necessary to insert ossicular replacement prostheses [3]. Despite aseptic conditions throughout implantation surgery there is a high risk of re-inflammation and -infection endangering the healing process and the function of the prosthesis [4]. For better control of inflammatory and infectious processes after implantation, a special pharmaceutically active coating of the prosthesis would be useful in order to complement or replace systemic drug applications. This has been shown for the local drug delivery of ciprofloxacin from a nanoporous silica coating on a standard total ossicular chain replacement prosthesis (TORP) [5]. As a material for those implants Bioverit® II has been proven biocompatible in several studies [6]. Bioverit® II is a bioglass-mica composite which is characterized by an easy manufacturing process and high resistance to biodegradation.
A promising class of material that has been employed recently in drug delivery studies are layered double hydroxides (LDHs). LDHs, also known as hydrotalcite-like compounds with the general formula [M II1−x M IIIx (OH) x+2 ][An−]x/n·yH2O, are composed of positively and negatively charged layers. MII represents bivalent (e.g. Mg2+, Ca2+, Mn2+, Zn2+) and MIII trivalent (e.g. Al3+, Co3+, Cr3+, Fe3+) cations of the main layer [7, 8]. The structure of magnesium-containing LDHs (Fig. 1) can be derived from the layered structure of brucite (Mg(OH)2), in which a certain amount of Mg2+ ions is replaced with trivalent cations; both types of metal ions are octahedrally coordinated by hydroxide ions (OH−) in the layers. Resulting surplus positive charges are balanced by anions An− placed in the interlayer spaces together with water molecules to fill the increased interlayer space [9]. The anions An− can be simple inorganic ones, as CO3 2− and SO4 2−, but also more complex anionic organic drugs [10–12]. These can then be released, when the LDH is used as a drug delivery system. The release of anions (e.g. drugs) from the LDH interlayer spaces can be achieved by anion exchange of the persisting LDH or by the dissolution of the LDH itself. Under acidic conditions, the dissolution of the LDH is triggered, but LDH will also dissolve slowly under neutral conditions [13].
Schematic structure of layered double hydroxides with positively charged layers and charge-balancing anions and additional water molecules located in the interlayer region (modified from [17])
In former studies several anti-inflammatory or antibacterial agents were applied in combination with LDHs as drug delivery systems. Mostly, only simple release experiments were performed and only few cell culture studies have been published. For example, a decrease in cell proliferation was reported by Dagnon et al. for implant surfaces covered with LDHs loaded with ibuprofen [14]. Strikingly, only very few in vivo studies have been reported so far. Silion et al. explored the in vivo behaviour of ketoprofen-loaded LDH in mice and found that intercalated ketoprofen has a better gastrointestinal compatibility and a stronger analgetic effect than the plain anti-inflammatory drug [15]. In another mouse study, Li et al. tested the protective potential as well as the therapeutic effects of LDHs as a DNA vaccine delivery vector. The LDH served as a suitable adjuvant to carry the vaccine and could thus inhibit tumour formation and suppress melanoma growth, respectively [16].
In a former study, we have examined the antimicrobial effect of a Mg–Al−SO4-LDH mixed with ciprofloxacin as a coating on middle ear prostheses for rabbits. The coating used by Hesse et al. showed excellent activity against infection immediately after implantation and persisting attenuated activity when the re-infection was triggered 1 week after surgery [17]. The in vivo studies mentioned above concentrated on the effects of drug loaded LDH coatings on the animals [15–17].
To our knowledge, our present study is the first to examine the degradation behaviour of pure LDH as an implant coating in vivo. The aim of this study was to examine the degradation characteristics of LDH under the complex conditions in the middle ear, and by this complement our former investigations. Thorough knowledge on the degradation behaviour of LDH is crucial for further examinations and ultimately for the targeted application of LDHs as key components of controllable drug release systems, in particular for reconstructive middle ear surgery.
2 Materials and methods
2.1 Implants and coating material
Bioverit® II implants were purchased from 3di GmbH (Jena, Germany). The bioceramic implants with an average weight of 8 mg are composed of a 2.1 mm long shaft with a diameter of 0.9 mm attached to a base plate with a diameter of 2.5 mm and a height of 0.5 mm (Fig. 2a).
a SEM picture of an uncoated Bioverit® II middle ear implant as produced for the study (EDX sites are marked with white rectangles) b EDX spectrum of an uncoated and c LDH coated prostheses (before the insertion into the ear). The white arrows highlight the intensity sequences of the element peaks of Mg, Al and Si for uncoated and LDH coated prostheses
For our study we used a water-based suspension of nanocrystals of a Mg–Al–CO3-LDH with a Mg:Al ratio of 2:1 as the material to prepare the implant coating. In a typical synthesis the raw LDH was precipitated in water by adding a solution of MgCl2·6H2O (20 mmol, purum p.a. ≥98.0 %, Fluka, Buchs, Switzerland) and AlCl3·6H2O (10 mmol, purum p.a. ≥99.0 %, Fluka) to an intensely stirred solution of NaOH (60 mmol, reagent grade, anhydrous, ≥98 %, Fluka) and Na2CO3·H2O (12 mmol, ≥99.5 %, Fluka). After the raw product was aged for 15 min, the product was collected by centrifugation, and washed twice with deionized water. The remainder was redispersed in water and exposed to ultrasonication for one hour. The synthesis was performed at ambient conditions and all chemicals were used as purchased without further purification. Information about the crystalline structure of the LDH materials was collected by X-ray diffraction (XRD) with a Theta/Theta diffractometer from Stoe (Darmstadt, Germany).
The coating was performed via a spray-coating technique. For this purpose, the implants were heated to 150 °C and sprayed with the nebulized LDH nanosuspension using a commercially available air brush equipment (Conrad Electronic SE, Hirschau, Germany). Throughout the process the spraying geometry, characterized by an angle of 45° and a distance of 30 cm (nozzle to implant), was maintained.
The spraying process and coating thickness were indirectly controlled by energy dispersive X-ray spectroscopy (EDX) to map the initial situation for a comparison with the explanted prostheses. All coated prostheses were characterized individually. The coating process was judged as complete when the EDX spectrum corresponded to the expectation of a high-intensity magnesium peak, a medium-intensity aluminium peak and a low-intensity silicon peak (Fig. 2c). In all cases the silicon peak from the Bioverit® II could be detected, indicating that the EDX was able to detect signals from both the Bioverit® II substrate and the silicon-free LDH coating, hence, allowing to track even minor degradation.
For this purpose, the implants were rotated by an angle of 90° around their long axis after five sprays had been applied, totalling in 20 sprays for the initial coating. If the EDX spectrum was not satisfactory after 20 sprays, one spray on each side was performed in addition and the EDX measurement was repeated. An average LDH coating thickness on the middle ear implants of approximately 150 nm was estimated according to laser scanning microscopy measurements (VK-9710, Keyence, Neu-Isenburg, Germany) of similarly coated flat glass slides.
2.2 In vivo setup
The in vivo study (permitted by the Lower Saxony State Office for Consumer Protection and Food Safety, Dept. of Animal Welfare, No. 33.9-42502-04-11/0610, considering the German Animal Welfare legislation) included 30 approximately six-month-old male New Zealand White rabbits (Charles River Laboratories, Sulzfeld, Germany). The animals had an average weight of 3.3 kg and were housed in single cages with an artificial day-night rhythm of 12 h in the Institute of Laboratory Animal Science and Central Animal Facility of the Hannover Medical School. The rabbits were accordingly divided into three groups (n = 10), each with an observation period after surgery of four, 7 and 10 days.
The anaesthetic management and implantation procedure was performed following the same protocol described in the studies by Hesse et al. and Stieve et al. [17, 18]. Accordingly, the prostheses were implanted into the right middle ear via a retroauricular access, while the left ear was used as control. The implantation procedure is documented in Fig. 3. After implantation the animals were supplied with an oral dose of 0.15 mg kg−1 meloxicam (Metacam®, Boehringer Ingelheim, Ingelheim am Rhein, Germany) 1 day pre-surgery and 3 days post surgery for analgesia. Oral antibiotic prophylaxis of 10 mg kg−1 enrofloxacin (Baytril®, Bayer, Leverkusen, Germany) also began 24 h before implantation, and was continued for 4 days post implantation.
Sequence of endoscopic images of the implantation procedure with a Retroauricular acess, b Incision of ear canal (meatus acusticus externus), c Ear canal with tympanic membrane, d Tympanotomy for accessing the middle ear, e View on middle ear with filled diamond, malleus filled triangle, incus filled circle stapes and filled star chorda tympani, f Extraction of incus, g Luxation of malleus, h Extraction of crura stapes, i Insertion of middle ear prosthesis between tympanic membrane and remaining base of stapes, j Closure of middle ear
After four, 7 and 10 days, respectively, subjects were sedated and euthanized with regard to animal welfare. Both middle ears were irrigated with 1.5 mL distilled water with a syringe by piercing the tympanic membrane, avoiding damage of the bulla. The rinsing solution was collected immediately and stored in sterile reaction tubes. Afterwards, pH values of the samples were estimated with a calibrated PB–20 Basic pH-Meter (Sartorius, Göttingen, Germany) by directly immersing the electrode into the respective solutions. The bulla tympanica was opened to estimate the middle ear microscopically. Finally the prosthesis was explanted and chemically analyzed.
2.3 Clinical evaluation
To examine the health status of the animals, we observed the behaviour, appetite, defecation and urination, body weight and rectal temperature up to 4 days post implantation. Afterwards, the animals were weighed weekly.
To detect possible systemic inflammation, blood samples were taken before implantation and at the end of the examination periods (per animal 0.5 mL blood in an EDTA micro tube, Sarstedt, Nümbrecht, Germany) and analysed with an animal blood counter (scil Vet ABC™ hematology analyzer, scil animal care company, CSF, Viernheim, Germany).
2.4 Microscopic examination of the middle ear
After ventral opening of the bulla tympanica the implant situation in the middle ear was microscopically evaluated using light microscopy (Microscope Zeiss®, Jena, Germany/Camera Lumenera®, Ottawa, Canada), whereas, the left middle ear served as control. The main focus was on the position and appearance of the prosthesis, the local mucosal reaction, possible inflammation signs e.g. hyper-vascularised mucosa, swelling, aggregation of watery, serous, mucous or bloody fluids.
A JEOL JSM-6700F field-emission scanning electron microscope (Jeol, Eching, Germany) was used for the collection of SEM images of the prostheses. The device was operated with an accelerating voltage of 2.0 kV at a working distance of 8 mm using the LEI-detector. The SEM was equipped with an INCA 300 energy dispersive X-ray (EDX) detector (Oxford Instruments PLC, Abingdon, UK).
2.5 Chemical analyses of the coatings
The main focus was on the tracking of the element ratios, in particular the Mg:Al ratio, at the implant surfaces and the intensities (Ielement) in the respective EDX spectra. To illustrate the course of changes of the coatings, each implant was measured before implantation and subsequently in the post-explanted state. The EDX spectrum of uncoated Bioverit® II is characterized by a low-intensity magnesium peak, a medium-intensity aluminium peak and a high-intensity silicon peak: IMg < IAl < ISi with a Mg:Al ratio of approximately 0.6. When coated with Mg4Al2-LDH, the intensities shifted to the expected, vice versa sequence: IMg < IAl < ISi → IMg > IAl > ISi (Fig. 2b, c) with an average Mg:Al ratio of approximately 1.5, close to the ratio of 1.8 of the Mg4Al2-LDH in the suspension.
Accordingly, the progress of in vivo LDH degradation for each group (4, 7 and 10 days) was evaluated at the cation ratio and the intensities of the element peaks in the EDX spectra. Hence, an advanced degradation of the LDH coating is expected to be characterized by an obvious decrease of the Mg:Al ratio and a re-reversion of the peak intensity sequence: IMg > IAl > ISi → IMg < IAl < ISi.
Due to the unique geometry of the implants, customized sample holders were fabricated by drilling the shape of the implants into standard graphite blocks suitable for scanning electron microscopy (SEM). EDX measurements were performed on each of the prostheses, near to and far away from the base plate. As shown in Fig. 2a, the EDX measurements were performed with a 200-fold magnification, totalling in 20 EDX spectra for each group (n = 10, 4, 7 and 10 days). The JSM-6700F was operated in EDX mode with 10 kV (accelerating voltage) and 10 µA at a range of 0–10 kV with regard to the prostheses elemental composition at the surface, i.e. Mg, Al, Si, O, C, K, F and Na.
3 Results
3.1 Clinical evaluation
All 30 rabbits showed a good general health status throughout the experiment without any inflammation signs of the wound or fever. Food and water intake as well as urination and defecation behaviour were normal. Two animals showed a slight head tilt for not more than 3 days after implantation, a rare but typical side effect of the implantation as described in earlier studies [17].
All rabbits showed an inconspicuous haematologic status prior to implantation and at the end of the study in agreement with the clinical appearance of the animals.
3.2 pH measurements
After the removal of the implants the pH values were measured in the rinsing solutions taken from the implanted right ears as well as from the left ears (control side). A slightly higher pH could be observed in the implanted ears (7.3 ± 0.3) than in the control side ears (6.7 ± 0.4). No correlation between the pH and the period of application was observed.
3.3 Microscopic examination
The appearance of the examined ears was in agreement with the expectations of an implanted middle ear after respective timepoints. After 4 days the microscopic view showed a minimal watery-bloody milieu with occasional appearance of a mucotympanum. After longer implantation periods, blood clots and mucus were resorbed and smooth mucosa became visible (Fig. 4). No signs of inflammation could be observed by microscopic means.
3.4 Chemical analysis of the coatings
The successful synthesis of pure Mg–Al–CO3-LDH was confirmed by XRD measurements of dried material from the nanosuspension. Unfortunately, a direct detection of LDH on the implant by XRD was not possible due to the geometry and small size of the middle ear implants. Weighing the samples was also not suitable for tracking the coating and was considered to be ineffective once the implants were contaminated with organic material after explantation. In order to prove the general applicability of the LDH nanosuspension for the spray coating process, and to optimize the substrate temperature used in this process (150 °C), flat glass slides were used as test substrates and spray-coated using a process similar to the one applied to the middle ear implants. These samples could be investigated by XRD. Crystalline LDH coatings were observed in all cases.
For each group (4, 7 and 10 days) 20 EDX spectra were collected and considered for the evaluation of the LDH degradation. Over the period of 10 days, no remarkable decrease of the magnesium to aluminium ratio determined at the surfaces (Fig. 5) and furthermore no change of the relative intensities of the element peaks in the EDX spectra could be observed. This is a sign that the Mg–Al–CO3-LDH coatings are practically biostable. As Mg is present with a higher contribution in the LDH coating but occurs with a minor contribution in the Bioverit® II substrate, a degradation of the LDH coating would result in a decrease of the Mg:Al ratio. Also the SEM images did not show any signs for alterations of the surface structure.
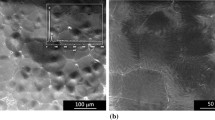
Whereas the carbon content was low before the implantations, as expected, it was considerably increased after the in vivo exposition. Organic debris (blood stains, mucus, and cell detritus) with high carbon content was found adhering to the implants’ surfaces in varying amounts and could also be seen by eye. Figure 6 exemplarily shows photographical and SEM images of two prostheses explanted 4 days after implantation. An increasing carbon content proportionally decreased the relative contributions of the other elements such as magnesium and aluminium, but did not influence their ratio.
a and c Pictures of explanted prostheses, shown here by way of example for prostheses which had remained in the middle ear for 4 days. b and d SEM images of the samples shown in a and c, respectively. EDX data were taken at the sites indicated by the white rectangles b1, b2, d1 and d2 images with higher magnification of the respective sites
4 Discussion
4.1 Animal health screening and microscopic examination
No harmful effect of the LDH coatings could be observed for any of the animals studied. All groups presented normal behaviour and clinical health status. In addition, the microscopic examination of the middle ear showed no pathological findings and no adverse effects of the LDH coating could be detected. This confirms a very good biocompatibility of LDHs as an implant coating material in the middle ear.
4.2 pH measurements
The slight increase of the pH in the operated ears can be assigned to the presence of the layered double hydroxide. Mildly alkaline effects are a consequence of a decomposition of the LDH:
This reaction probably occurs only to a very small extent which is not detectable in the EDX spectra. Since inflammatory reactions commonly acidify the surrounding tissue, the data shown and the post mortem microscopic examinations allow the conclusion that no severe inflammatory reaction was present [19, 20].
4.3 In vivo stability of LDH coatings
The main result from this study, apart from the conclusion that the LDH has a very good biocompatibility, is the unexpected stability of the LDH coatings. Except for the mildly alkaline effect, no changes could be observed even after 10 days of implantation.
With regard to the estimated coating thickness of 150 nm, suitable implantation periods had to be chosen. Janning et al. examined the dissolution character of magnesium hydroxide (Mg(OH)2), a substance similar to magnesium-containing LDHs, in a peri-implant bone environment and found that the volume of implanted Mg(OH)2 cylinders was reduced by 7 % after 2 weeks and by 19 % of its initial volume after 6 weeks of implantation [21]. Considering these results, with degradation occurring at the µm scale in the course of several weeks, examination periods of 4, 7 and 10 days were chosen with regard to the much thinner coating. Additionally, many release systems show burst release behaviour [22], making the early stages of possible degradation processes more interesting for this empiric study.
It has to be emphasized that the middle ear illustrates a special environment for implants. For the first days after surgical procedure, the tympanic cavity is liquid-filled, blood and mucus surrounding the implantation site. Throughout the healing, liquids are resorbed, ventilation and pressure equalization of the middle ear are restored and the fluid is replaced by an air-filled environment. Based on our knowledge gained from earlier studies and from human middle ear surgery, our different examination periods seem suitable to include and track the extensive reorganization processes.
It also has to be pointed out that the coated prostheses were implanted under physiological conditions in a healthy middle ear. Commonly, prostheses as therapeutic tools will be implanted into inflamed and infected surroundings, which might influence the degradation process and by this the drug release behavior. Accordingly, examination times have to be adjusted to the indications caused by a corresponding infection model.
4.4 Consequences for LDH-based drug delivery systems
In our former in vivo drug delivery study, the delivery system consisted mainly of a physical mixture of ciprofloxacin with a Mg–Al–SO4-LDH [17]. Considering the results obtained on Mg–Al–CO3-LDH coatings, we suppose that the LDH component of the ciprofloxacin/Mg–Al–SO4-LDH mixture used in our earlier investigations did not dissolve entirely. Nonetheless, sufficient amounts of drug could be released to suppress infection. With the findings presented here we expect that the drug had been released independently from the dissolution of the Mg–Al–SO4-LDH. It is likely that the Mg–Al–SO4-LDH matrix served mainly as a physico-chemical barrier and as a mild pH-balancing agent. Concerning this matter, the biostability of the Mg–Al–CO3-LDH shown in this study indicates biodegradation characteristics comparable to an analogous Mg–Al–CO3-LDH based drug release system. Hence, both LDHs appear promising as key components of drug release systems, in particular in the middle ear. However, drug and indication specific demands, exemplarily desired release rates, have to be considered.
Certainly the preparation of simple physical mixtures is an undemanding process, allowing for the facile and fast preparation of drug delivery systems including easily producible carbonate-LDHs and many other water-stable pharmaceuticals [23]. The LDHs offer a versatile material with regard to their composition and corresponding chemical properties. As mentioned above, the choice of the anion can be altered, as well the cations and their ratio [24, 25], while maintaining the general LDH formula [M II1−x M IIIx (OH) x+2 ][An−]x/n·yH2O.
On the contrary, the preparation of LDH intercalation compounds, where an anionic drug has to be intercalated into the LDH structure in order to form to a true common chemical compound, involves a much larger amount of work effort [26, 27]. Synthesis routes with satisfying yields and purities have to be elaborated and adjusted for every individual drug. The release of a drug from a drug-LDH intercalation compound is either accompanied by the decomposition of the LDH coating or occurs via anion exchange. These complex processes can be very different depending on the type of the drug used. When drug/LDH mixtures (in contrast to intercalation compounds) are used, drug release rates can be adjusted by altering the ratio of components and the composition of the LDH. Preferably, the adjustments could be included in the respective coating process. In order to promote the homogeneity of the coatings and to establish a reproducible process eligible for market authorization, automation of the coating techniques, exemplary for our study i.e. controlled spray duration per cycle, humidity and substrate temperature, would be of interest.
5 Conclusion
In the middle ear, Mg–Al–CO3-LDH can serve as a highly biocompatible and practically biostable (at least for the timeframe of the current investigation of 10 days) coating material which can provide mild pH balance and is suitable for the construction of drug release systems, as shown before for Mg–Al–SO4-LDH [17]. Throughout the examination, the pure LDH coatings on middle ear implants had no harmful effects on the animals’ health.
For further drug release applications for which the utilization of sophisticated, pure drug-LDH intercalation compounds has been considered to be necessary, simple mixtures of agents with LDH could prove to be sufficient. This might reduce the effort associated with synthesis and processing of pure intercalation compounds.
References
Madana J, Yolmo D, Kalaiarasi R, Gopalakrishnan S, Sujatha S. Microbiological profile with antibiotic sensitivity pattern of cholesteatomatous chronic suppurative otitis media among children. Int J Pediatr Otorhinolaryngol. 2011;75:1104–8.
Osma U, Cureoglu S, Hosoglu S. The complications of chronic otitis media: report of 93 cases. J Laryngol Otol. 2000;114:97–100.
Battaglia A, McGrew BM, Jackson CG. Reconstruction of the entire ossicular conduction mechanism. Laryngoscope. 2003;113:654–8.
Hwang J, Chu C, Liu T. Changes in bacteriology of discharging ears. J Laryngol Otol. 2002;116:686–9.
Lensing R, Bleich A, Smoczek A, Glage S, Ehlert N, Luessenhop T, et al. Efficacy of nanoporous silica coatings on middle ear prostheses as a delivery system for antibiotics: an animal study in rabbits. Acta Biomater Acta Materialia Inc. 2013;9:4815–25.
Vogt JC, Brandes G, Krüger I, Behrens P, Nolte I, Lenarz T, et al. A comparison of different nanostructured biomaterials in subcutaneous tissue. J Mater Sci Mater Med. 2008;19:2629–36.
Khan AI, O’Hare D. Intercalation chemistry of layered double hydroxides: recent developments and applications. J Mater Chem. 2002;12:3191–8.
Zhang LH, Li F, Evans DG, Duan X. Cu–Zn–(Mn)–(Fe)–Al Layered double hydroxides and their mixed metal oxides: physicochemical and catalytic properties in wet hydrogen peroxide oxidation of phenol. Ind Eng Chem Res. 2010;49:5959–68.
Evans D, Duan X. Preparation of layered double hydroxides and their applications as additives in polymers, as precursors to magnetic materials and in biology and medicine. Chem Commun. 2006;485–96. doi:10.1039/B510313B.
Khan A, Lei L, Norquist A, O’Hare D. Intercalation and controlled release of pharmaceutically active compounds from a layered double hydroxide. Chem Commun. 2001;2342–3. doi:10.1039/B106465G.
Ambrogi V, Fardella G, Grandolini G, Perioli L. Intercalation compounds of hydrotalcite-like anionic clays with antiinflammatory agents–I. Intercalation and in vitro release of ibuprofen. Int J Pharm. 2001;220:23–32.
Frunza MS, Popa MI, Lisa G, Hritcu D, Lion MSI, Marcel Lone Pop A. New hybrid compounds containing intercalated ciprofloxacin into layered double hydroxides: synthesis and characterization. Rev Roum Chim. 2008;53:827–31.
Boclair J, Braterman P. Layered double hydroxide stability. 1. Relative stabilities of layered double hydroxides and their simple counterparts. Chem Mater. 1999;11:298–302.
Dagnon KL, Ambadapadi S, Shaito A, Ogbomo SM, DeLeon V, Golden TD, et al. Poly(L-lactic acid) nanocomposites with layered double hydroxides functionalized with ibuprofen. J Appl Polym Sci. 2009;113:1905–15.
Silion M, Hritcu D, Jaba IM, Tamba B, Ionescu D, Mungiu OC, et al. In vitro and in vivo behavior of ketoprofen intercalated into layered double hydroxides. J Mater Sci Mater Med. 2010;21:3009–18.
Li A, Qin L, Wang W, Zhu R, Yu Y, Liu H, et al. The use of layered double hydroxides as DNA vaccine delivery vector for enhancement of anti-melanoma immune response. Biomaterials. 2011;32:469–77.
Hesse D, Badar M, Bleich A, Smoczek A, Glage S, Kieke M, et al. Layered double hydroxides as efficient drug delivery system of ciprofloxacin in the middle ear: an animal study in rabbits. J Mater Sci Mater Med. 2013;24:129–36.
Stieve M, Hedrich HJ, Battmer RD, Behrens P, Müller P, Lenarz T. Experimental middle ear surgery in rabbits: a new approach for reconstructing the ossicular chain. Lab Anim. 2009;43:198–204.
Dissemond J, Witthoff M, Brauns TC, Haberer D, Goos M. pH values in chronic wounds. Evaluation during modern wound therapy. Der Hautarzt. 2003;54:959–65.
Bartsch I, Willbold E, Rosenhahn B, Witte F. Non-invasive pH-determination adjacent to degradable biomaterials in vivo. Acta Biomater. 2014;10:34–9.
Janning C, Willbold E, Vogt C, Nellesen J, Meyer-Lindenberg A, Windhagen H, et al. Magnesium hydroxide temporarily enhancing osteoblast activity and decreasing the osteoclast number in peri-implant bone remodelling. Acta Biomater. 2010;6:1861–8.
Huang X, Brazel CS. On the importance and mechanisms of burst release in matrix-controlled drug delivery systems. J Control Release. 2001;73:121–36.
Chakraborti M, Jackson J, Plackett D, Gilchrist S, Burt H. The application of layered double hydroxide clay (LDH)-poly (lactide-co-glycolic acid)(PLGA) film composites for the controlled release of antibiotics. J Mater Sci Mater Med. 2012;23:1705–13.
Panda HS, Srivastava R, Bahadur D. Stacking of lamellae in Mg/Al hydrotalcites: effect of metal ion concentrations on morphology. Mater Res Bull. 2008;43:1448–55.
Vucelic M, Jones W, Moggridge G. Cation ordering in synthetic layered double hydroxides. Clays Clay Miner. 1997;45:803–13.
Carlino S, Hudson M. Reaction of molten sebacic acid with a layered (Mg/Al) double hydroxide. J Mater Chem. 1994;4:99–104.
Del Arco M, Cebadera E, Gutiérrez S, Martín C, Montero MJ, Rives V, et al. Mg, Al layered double hydroxides with intercalated indomethacin: synthesis, characterization, and pharmacological study. J Pharm Sci. 2004;93:1649–58.
Acknowledgments
We acknowledge the financial support of the project by the German Research Foundation (DFG) within the Collaborative Research Centre SFB 599 (subprojects D1 and DR1). This work also profited from collaboration in the Cluster of Excellence “Hearing4all”.
Author information
Authors and Affiliations
Corresponding authors
Additional information
F. Duda and M. Kieke have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Duda, F., Kieke, M., Waltz, F. et al. Highly biocompatible behaviour and slow degradation of a LDH (layered double hydroxide)-coating on implants in the middle ear of rabbits. J Mater Sci: Mater Med 26, 9 (2015). https://doi.org/10.1007/s10856-014-5334-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-014-5334-x