Abstract
Bacterial colonisation of exposed implant and abutment surfaces can lead to peri-implantitis, a common cause of oral implant failure. When an abutment becomes exposed in the oral environment the typical recommendation is to debride it, to obtain a smoother surface which might be expected to reduce bacterial colonisation. The aim of this study was to evaluate, in vitro, a conventional polishing protocol (PP1) and a simplified polishing protocol (PP2), suggested to have advantages over PP1. The surface morphology and roughness of titanium abutments were characterised at each stage of polishing, and adhesion of oral bacteria was evaluated, using atomic force microscopy, environmental scanning electron microscopy and optical profilometry. PP1 and PP2 methodologies resulted in indistinguishable surface finishes, with fewer scratches than the unmodified surface, and equal roughness values. PP2 resulted in less disruption and less removal of surface material. Early biofilm formation by Streptococcus mutans was reduced on surfaces polished using PP2, but not PP1. Biofilms of Actinomyces naeslundii were more extensive on polished abutment surfaces. Simplified protocol PP2 may be preferable to conventional protocol PP1, since less material is removed, and there is less chance of rough areas remaining. Polishing, however, does not necessarily reduce oral bacterial colonisation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over recent years there has been a marked increase in the use of dental implants [1, 2]. Although short- and long-term implant success rates are high, when failure does occur it is costly to rectify and often distressing for the patient. The most common cause of late implant failure is peri-implantitis, a major factor in which is the colonisation of an exposed implant or abutment surface by pathogenic oral bacteria in association with peri-implant bone loss and inflammation [3]. Although implant surfaces when exposed in the mouth always have the potential for microbial contamination, rough implant surfaces have been generally considered to enhance initial adhesion of oral bacteria and thus subsequent colonisation [4]. A reduction of titanium surface roughness has been positively correlated with a reduction in dental plaque formation [5, 6].
When an implant becomes exposed in the mouth, regular and effective debridement procedures are recommended. Methods of debridement include the use of hand instruments and abrasives either delivered by air polishing or rotary instrumentation [7–10]. Hand instruments with plastic or carbon-fibre tips are thought to be “implant-safe”, as their working surfaces are softer than the titanium surface, thereby minimising the risk of damaging the implant or abutment. The use of stainless steel curettes and metal tip ultrasonic scalers is not recommended as they can easily cause surface damage [8]. Should a rough titanium surface become exposed in the oral cavity, or a previously smooth titanium surface become damaged, then a surface polishing procedure (implantoplasty) may be recommended [11, 12]. Implantoplasty has been shown to positively influence implant survival rate and clinical success [13]. This is thought to be primarily because bacteria have been reported to colonise rough surfaces more readily than smooth surfaces [14, 15], and secondarily because smooth surfaces are more readily disinfected than rough surfaces [16]. Implantoplasty is often performed in conjunction with application of topical antimicrobials, or systemic antibiotics [3, 17, 18].
Although implantoplasty is widely recommended there is a lack of consensus with regard to the most effective polishing techniques [8, 13, 19, 20]. Fine grit diamond burs are recommended for the removal of titanium plasma-sprayed coatings and gross re-shaping of surface features [13, 19, 21]. The use of abrasive rubber points has also been shown to reduce the roughness of titanium surfaces [8, 13, 21]. In addition, the application of a sequence of abrasive cups or points followed by polishing agents has been proposed as a refinishing procedure for titanium abutments that have become scratched [20].
The aim of this study was to evaluate the effectiveness of a conventional protocol for polishing titanium abutments (polishing protocol 1, PP1), and to compare this to a simplified protocol that may have advantages over the more established method (polishing protocol 2, PP2). PP2 involves fewer steps and is therefore simpler and quicker to perform. More importantly, PP2 does not include the more aggressive debridement steps of diamond grit and carborundum, and hence might be expected to result in less disruption of the surface and less removal of surface features, which can compromise the fit of the prosthesis. The morphology and roughness of the abutment surface was examined at each stage of the process at a range of resolutions using atomic force microscopy (AFM), environmental scanning electron microscopy (ESEM) and optical profilometry (OP). Early biofilms formed by two oral bacteria, Streptococcus mutans and Actinomyces naeslundii, to abutment surfaces before and after polishing, in the presence of an in vitro-formed salivary pellicle, were compared.
Materials and methods
The abutments used in this study were 5.5 mm Standard Titanium abutments (NobelBiocare AB, Gothenburg, Sweden). Each abutment was sectioned to provide specimens with approximately 3 mm × 4 mm surface area for polishing.
Two polishing protocols were employed:
Polishing protocol 1 (PP1): Fine diamond grit rotary bur (Drendel and Zweiling, Diamant GmbH, Berlin, Germany) for 15 s; green carborundum stone rotary point (Dedeco Dental Products, St. Paul, MN, USA) for 15 s; brown impregnated silicon rubber point (Shofu, Kyoto, Japan) for 15 s; green impregnated silicon rubber point (Shofu, Kyoto, Japan) for 15 s; cloth mop and polishing compound containing amorphous silica/silicon carbide (JF Jelenko, NY, USA) for 15 s. The fine grit diamond rotary bur was used in a high-speed dental handpiece at approximately 200,000 rpm under profuse water irrigation. All other points were used in a slow-speed dental handpiece at approximately 5,000 rpm with no water irrigation during polishing. After polishing, samples were cleaned by ultrasonicating in 95% ethanol for 60 s.
Polishing protocol 2 (PP2): Brown impregnated silicon rubber point (Shofu Inc., Kyoto, Japan) for 15 s; green impregnated silicon rubber point (Shofu Inc., Kyoto, Japan) for 15 s; cloth mop and polishing compound containing amorphous silica/silicon carbide (JF Jelenko & Co., NY, USA) for 15 s. Each polishing stage was performed using a slow-speed dental handpiece at approximately 5,000 rpm without irrigation. After polishing, samples were cleaned by ultrasonicating in 95% ethanol for 60 s.
Surface analysis
AFM was performed using a Nanoscope IIIa Multimode (Digital Instruments, Santa Barbara, CA, USA) equipped with a k-scanner, operating in tapping mode in air. AFM images of the abutment sections were obtained before polishing and after rubber cup and cloth mop polishing, since the surface was too rough to scan after diamond grit and carborundum polishing.
ESEM was performed using an ESEM 2020 (FEI UK, Cambridge, UK) in secondary electron mode with a tungsten filament and an acceleration voltage of 20 kV. Images of abutments were obtained after each polishing stage. Specimens for SEM were sputter-coated with a layer of gold approximately 30 nm thick. SEM was performed using an ISI 60 SEM (SEM Tech, Bonsall, UK) in secondary electron emission mode with an acceleration voltage of 20 kV.
OP was performed using a Proscan (Scantron, Taunton, UK) after each polishing stage. Roughness values for two different areas on each abutment section were calculated. The roughness values were found not be normally distributed, so non-parametric statistical analysis was performed on the median values using a Kruskal–Wallis test and box-whisker plots to identify statistically significant differences.
Bacteria
Streptococcus mutans NG8 and Actinomyces naeslundii NCTC 10301 were grown in screw cap bottles containing BHY medium (Brain Heart Infusion Broth (LabM) supplemented with 0.5% Yeast Extract (Difco)), or on BHY agar plates in candle jars at 37 °C. Glycerol stock cultures were used to inoculate fresh BHY broth and cultures were grown to OD600 = 0.9 (approximately 109 bacterial cells mL−1). Portions of these cultures (0.2 mL) were inoculated unto the wells of 12-well microtitre plates containing 2 mL filter-sterilised human saliva:BHY medium (1:1). Stimulated saliva was collected from 5 healthy adult volunteers, centrifuged at 15,000g for 30 min, and the supernatant was filter sterilized (0.45 μm filter) and frozen in portions at −70 °C.
Biofilm formation
Growth rates of S. mutans and A. naeslundii were measured by OD600. Abutment samples in microtitre plate wells were incubated in saliva medium with or without inoculation of bacterial culture. After incubation under 5% CO2 atmosphere at 37 °C for 16 h, the abutment sections were removed from the plate wells, rinsed gently in sterile distilled water and allowed to air dry. Experiments were performed at least twice. To estimate numbers of adherent bacteria, samples were rinsed gently in phosphate buffered saline (0.01 M phosphate buffer; 0.0027 M KCl, 0.137 M NaCl; pH 7.4) and transferred to microcentrifuge tubes (1.5 mL) containing 1 mL PBS and 0.05 g, 0.11 mm diameter sterile glass beads. The samples were vortex mixed for 1 min to disrupt bacterial biofilms and the suspension was serially diluted and plated onto BHY agar for determination of numbers of colony-forming units (CFU) per mL. This enabled approximate numbers of bacteria on the specimens to be determined.
AFM images of abutment surfaces coated with salivary proteins or with colonising bacteria were obtained as described above. To quantify bacterial coverage, five randomly selected areas (25 μm × 25 μm) were imaged from each of two abutment sections, and superimposed with a 10 × 10 grid. Each of the 100 squares was scored for >50% bacterial coverage, and thus calculation of percentage total coverage of the surface. The results were found not to be normally distributed and were therefore analysed using Kruskal–Wallis tests and box-whisker plots. SEM images of bacterial biofilms on abutment surfaces were also obtained as described above.
Results
The roughness of the abutment surfaces at each stage of the two polishing procedures is shown in Table 1. There was no statistically significant difference between the initial and final roughness values of the abutments. Although unpolished PP2 specimens had a numerically higher roughness than unpolished PP1 specimens, this was not significantly different owing to a large standard deviation for this group. In protocol PP1, debridement using diamond grit resulted in a large increase in roughness, which was decreased by subsequent polishing steps and reached the initial roughness after Shofu green polishing. In protocol PP2, there was a small increase in roughness after Shofu brown polishing, although this was not statistically significant. Roughness was reduced to the level of unpolished specimens by Shofu green polishing. Cloth mop polishing resulted in a numerical decrease in roughness, but this was not statistically significant.
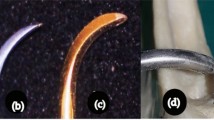
This pattern of roughness was confirmed by ESEM images. Scratches and pits were observed on the abutment surface immediately after removal from the manufacturer’s packaging (Figs. 1a and 2a). Diamond grit and carborundum polishing resulted in a large increase in surface roughness and removal of a significant amount of material from the abutment (Fig. 1b, c). When diamond grit and carborundum polishing were omitted (PP2), similar surface morphologies were obtained (Figs. 1c–f and 2b–d). Surface asperities and scratches were obliterated by these processes. Rubber cup polishing resulted in a progressively lower roughness, and also obliterated surface asperities and scratches (Figs. 1d, e and 2b, c).
ESEM images of abutment surfaces at various stages of polishing using protocol PP1. (a) Untreated, machined surface exhibiting pits and scratches; (b) polished using diamond grit; (c) polished using carborundum; (d) polished using rubber cup (Shofu green); (e) polished using rubber cup (Shofu brown); (f) polished using cloth mop. The scale bars represent 100 μm
AFM images of a PP2 abutment surface covered with salivary pellicle are shown in Fig. 3a, b. A typical pellicle appearance with a continuous layer containing globules of typical diameter 50–200 nm could be seen on the abutment surface; there was no visible difference between the pellicle formed on the differently polished abutments.
AFM images showing PP2 abutment surfaces coated with salivary pellicle. (a) Representative lower-resolution image. The axes measure 10 μm; (b) zoomed-in images of the same region, with axes measuring 2 μm. A darker shade represents a lower-lying region, and a lighter shade an elevated region. In both images a layer of pellicle composed of globular structures measuring approximately 10–100 nm can be observed
Abutments produced using protocols PP1 and PP2, and non-polished abutments, were then compared for their ability to support biofilm growth. There were statistically significant differences between the coverage of differently treated abutment surfaces with S. mutans (p = 0.006) or with A. naeslundii (p = 0.001). Representative AFM images of abutment surfaces following incubation with S. mutans or A. naeslundii are shown in Fig. 4. The AFM images were used to calculate the median bacterial coverage of the abutment surfaces (Table 2). Representative SEM images of abutment surfaces and bacteria showing similar behaviour are shown in Fig. 5a, b. It can be seen that the extent of colonisation of the surfaces varied according to surface. The unpolished abutments supported dense biofilm growth of S. mutans (Fig. 4a). This was reduced significantly by PP2 (Fig. 4c); there was a numerical reduction in coverage on PP1 samples (Fig. 4b), but the difference was not statistically significant. The unpolished abutments did not support a large extent of biofilm growth by A. naeslundii (Fig. 4d), but polishing using either PP1 or PP2 significantly increased A. naeslundii biofilm formation (Fig. 4e, f). Viable counts of bacteria adhered to the unpolished specimens after 16h were 5.3 × 106 CFU per specimen for S. mutans and 7.3 × 105 CFU per specimen for A. naeslundii, confirming differential adhesion levels of these species.
AFM images showing biofilm formation on abutment surfaces. (a) S. mutans on an unpolished sample, showing extensive bacterial coverage with some areas of titanium visible; (b) S. mutans on a PP1 sample showing extensive bacterial coverage; (c) S. mutans on a PP2 sample showing extensive bacterial coverage; (d) A. naeslundii on an unpolished sample showing sparse bacterial coverage with many areas of titanium visible; (e) A. naeslundii on a PP1 sample showing greater bacterial coverage; (f) A. naeslundii on a PP2 sample showing intermediate bacterial coverage. The axes measure 25 μm in all images
To rule out the possibility that differences in biofilm coverage between S. mutans and A. naeslundii were due simply to bacterial growth rates, doubling times of the organisms in saliva medium were measured. Although the doubling time of S. mutans (t d = 1.4 h) was less than that of A. naeslundii (t d = 2.3 h) the final growth yield for A. naeslundii after 8 h was similar to that of S. mutans.
Discussion
The studies presented in this article were undertaken to determine the effects of polishing of titanium abutments on surface morphology, roughness, and propensity to be colonised by oral bacteria.
The machined titanium surface of abutments exhibited some pits and scratches. Since great care was taken not to damage the abutments between removing them from the packaging and placing analysis, these imperfections were clearly generated during the manufacturing process. Rubber cup polishing was sufficient to obliterate scratches and other imperfections in the abutment surfaces.
The final appearance of the abutment surfaces, and the roughness after Shofu green and cloth mop polishing, was indistinguishable between PP1 and PP2 (Figs. 1 and 2; Table 1), and there was no statistically significant difference between adhesion of two oral bacterial species to surfaces prepared using PP1 or PP2 (Table 2). Both protocols obliterated scratches and pits on the abutment surfaces. Thus it can be concluded that the resulting surfaces from the two protocols are equivalent. Diamond grit and carborundum polishing, however, removed considerable material from the abutment surface. These stages could be considered unnecessarily destructive as their inclusion in protocol PP1 did not significantly affect the final surface finish compared to that generated by protocol PP2. Removal of surface material is likely to detrimentally affect the fit of the prosthesis that rests on the abutment. Additionally, by using PP1, some areas might be roughened with diamond grit or carborundum and be missed by subsequent finer polishing steps, thereby creating areas with much rougher surfaces than initially present. Therefore it may be preferable to polish the abutment surface using only rubber cups, and to neglect the more aggressive polishing steps, as these apparently do not offer any advantage.
The additional step of polishing using a cloth mop is not usually used in the clinic. Using currently available technology it would be necessary to remove the abutment from the patient’s mouth before carrying out this step, creating an additional workload for the clinician and dental team, and requiring consideration of cross-infection hazards. Additionally, although roughness is numerically reduced by cloth mop polishing, this difference was not statistically significant. Whether this significantly influences clinical success, and is to be recommended, requires further investigation.
The roughness values of the unpolished and polished abutment surfaces were all in the region of 0.2 μm, found previously to be a “threshold R a”, below which a change in roughness does not significantly effect plaque accumulation [5]. Our results demonstrate that polishing abutments significantly influences subsequent oral bacterial biofilm formation. However, highly polished surfaces coated with salivary pellicle do not necessarily result in reduced levels of bacterial colonisation. We have observed differential bacterial coverage with surfaces with the same roughness but different detailed surface morphology. However, we are investigating initial bacterial adhesion as compared to plaque accumulation over long periods in vivo, and as such our work differs significantly from previous studies. Nevertheless, our results suggest a different performance of surfaces with the same roughness but different morphology in the mouth.
Streptococcus mutans and Actinomyces naeslundii are not usually associated with active peri-implantitis [22]. However, these are amongst the main colonisers of oral surfaces and they readily form biofilms, paving the way for colonisation of more pathogenic species. Adhesion of S. mutans was reduced by using PP1, while adhesion of A. naeslundii was increased by polishing using either technique. Dependence of adhesion on surface characteristics is not straightforward. It is known that different species bacteria vary in the degree to which they adhere to titanium [23]. However, the differential coverage of the bacterial species on the polished versus unpolished surfaces (Figs. 4 and 5) is likely to be related to the different surface morphologies and properties of the bacteria, as well as to the nature of the salivary pellicle formed. The rod-shaped bacterium A. naeslundii may be better able to make multiple adhesive contacts with a smooth surface. Conversely, the cocci chains of S. mutans might be better retained on a surface within pits and crevices. Although the measured roughness was similar for the polished and unpolished surfaces, this is only one representation of surface morphology, and it can be seen (Figs. 1 and 2) that the detailed morphologies of the surfaces were quite different.
The differential coverage by the two bacterial species could also be related to chemical effects of material deposited in or on the surface during the polishing process that is not removed by ultrasonication. Since oral bacteria recognize multiple salivary components, the nature of components of saliva that adsorb to the titanium surface may in turn affect the propensity for the different bacteria to adhere [24]. There was no visible difference between the pellicles formed on the abutment surfaces, which resembled salivary pellicles observed by other authors [25, 26]. A biochemical analysis of the pellicle components present on the various surfaces may reveal if different salivary components adsorb to the unpolished and polished surfaces.
Adhesion of bacteria may be affected by the hydrophobicity of the bacterial cell surface [27, 28] and the surface energy of the titanium abutment. Different surface treatments may change the surface energy of the titanium. However, it should be noted that we have incorporated a salivary pellicle in our studies since exposed surfaces in the mouth are rapidly coated with saliva. Thus we have not measured direct adhesion of bacteria to the titanium surface. Most studies investigating the adhesion of oral bacteria to biomaterials have not incorporated saliva, and have compared strains of a single species rather than comparing different species [29–32]. Our results indicate that this is likely to give only a limited view of the potential for bacterial colonisation.
References
M. A. S. GARCES and C. G. ESCODA, Med. Oral Patol. Oral Cir. Bucal 9 (2004) 63
M. DEL FABBRO, T. TESTORI, L. FRANCETTI and R. WEINSTEIN, Int. J. Periodontics Restorative Dent. 24 (2004) 565
L. J. A. HEITZ-MAYFIELD and N. P. LANG, Int. J. Oral Maxillofac. Implants 19 (2004) 128
M. QUIRYNEN, M. De SOETE and D. VAN STEENBERGHE, in Proceedings of the 3rd European Workshop on Periodontology, edited by N. P. Lang, T. Karring and J. Lindhe (Quintessence Books, Berlin, 1999) p. 102
C. M. L. BOLLEN, W. PAPAIOANNOU, J. VAN ELDERE, E. SHEPERS, M. QUIRYNEN and D. VAN STEENBERGHE, Clin. Oral Implant Res. 7 (1996) 201
M. QUIRYNEN, C. M. L. BOLLEN, W. PAPAIOANNOU, J. VAN ELDERE and D. VAN STEENBERGHE, Int. J. Oral Maxillofac. Implants 11 (1996) 169
J. A. SPEELMAN, B. COLLAERT and B. KLINGE, Clin. Oral Implant Res. 3 (1992) 120
S. MATARASSO, G. QUAREMBA, F. CORAGGIO, E. VAIA, C. CAFIERO and N. P. LANG, Clin. Oral Implant Res. 7 (1996) 64
H. STROOKER, S. ROHN and A. J. VAN WINKERHOFF, Int. J. Oral Maxillofac. Implants 13 (1998) 845
A. BAGNO and C. DI BELLO, J. Mater. Sci. Mater. Med. 15 (2004) 935
S. A. JOVANOVIC, E. B. KENNEDY, F. A. CARRANZA and K. DONATH, Int. J. Oral Maxillofac. Implants 8 (1993) 13
J. L. LOZADA, R. A. JAMES, M. BOSKOVIC, C. CORDOVA and S. EMANUELLI, J. Oral Implantol. 16 (1990) 42
E. ROMEO, M. GHISOLFI, N. MURGOLO, M. CHIAPASCO, D. LOPS and G. VOGEL, Clin. Oral Implant Res. 16 (2005) 9
R. L. TAYLOR, J. VERRAN, G. C. LEES and A. J. P. WARD, J. Mater. Sci. Mater. Med. 9 (1998) 17
D. R. DRAKE, J. PAUL and J. C. KELLER, Int. J. Oral Maxillofac. Implants 14 (1999) 226
R. PALMER, P. PALMER and L. HOWE, Br. Dent. J. 187 (1999) 653
A. MOMBELLI, Periodontology 2000 28 (2002) 177
N. P. LANG, T. BERGLUNDH, L. J. A. HEITZ-MAYFIELD, B. E. PJETURSSON, G. E. SALVI and M. SANZ, Int. J. Oral Maxillofac. Implants 19 (2004) 150
L. RIMONDINI, F. C. SIMONCINI and A. CARRASSI, Clin. Oral Implant Res. 11 (2000) 129
W. W. HALLMON, T. C. WALDROP, R. M. MEFFERT and B. W. WADE, Int. J. Oral Maxillofac. Implants 11 (1996) 96
A. RUHLING, A. HELLWEG, T. KOCHLER and H. C. PLAGMANN, Clin. Oral Implant Res. 12 (2001) 301
K. HEYDENRIJK, H. J. A. MEIJER, W. A. VAN DER REIJDEN, G. M. RAGHOEBAR, A. VISSINK and B. STEGENGA, Int. J. Oral Maxillofac. Implants 17 (2002) 829
H. KUULA, E. KONONEN, K. LOUNATMAA, Y. T. KONTTINEN and M. KONONEN, Int. J. Oral Maxillofac. Implants 19 (2004) 803
M. EDGERTON, S. E. LO and F. A. SCANNAPIECO, Int. J. Oral Maxillofac. Implants 11 (1996) 443
U. LENDENMANN, J. GROGAN and F. G. OPPENHEIM, Adv. Dent. Res. 14 (2000) 22
D. DEIMLING, L. BRESCHI, W. HOTH-HANNIG, A. RUGGERI, C. HANNIG, Y. NEKRASHEVYCH, C. PRATI and M. HANNIG, Eur. J. Oral Sci. 112 (2004) 503
K.A. STREVETT and G. CHEN, Res. Microbiol. 154 (2003) 329
M. GRIVET, J. J. MORRIER, G. BENAY and O. BARSOTTI, J. Mater. Sci. Mater. Med. 11 (2000) 637
S. SARDIN, J. J. MORRIER, G. BENAY and O. BARSOTTI, J. Oral Rehabil. 31 (2004) 140
F. MABBOUX, L. PONSONNET, J. J. MORRIER, N. JAFFREZIC and O. BARSOTTI, Colloids Surf. B: Biointerfaces 39 (2004) 199
L. MONTANARO, D. CAMPOCCIA, S. RIZZI, M. E. DONATI, L. BRESCHI, C. PRATI and C. R. ARCIOLA, Biomaterials 25 (2004) 4457
L. G. HARRIS and R. G. RICHARDS, J. Mater. Sci. Mater. Med. 15 (2004) 311
Acknowledgements
We are grateful to Jonathan Hawkins of the Interface Analysis Centre and Jane Brittan of the Oral Microbiology group.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barbour, M.E., O’Sullivan, D.J., Jenkinson, H.F. et al. The effects of polishing methods on surface morphology, roughness and bacterial colonisation of titanium abutments. J Mater Sci: Mater Med 18, 1439–1447 (2007). https://doi.org/10.1007/s10856-007-0141-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-007-0141-2