Abstract
Initial bacterial adhesion on dental implant abutment is related to its surface chemical composition and physical characteristics. Selection of appropriate abutment materials resistant to bacterial adhesion is important for dental implant maintenance. The aim of present study was to evaluate the effect of different properties of abutment materials on initial bacterial adhesion in vitro. Polished zirconia (PZ group), polished titanium (PT group) and ground titanium (GT group) samples were prepared to simulate clinical dental implant abutments. Chemical compositions, morphology, roughness, hydrophilicity and surface free energy of materials were analyzed. Oral commensal bacterium Streptococcus mitis was used to evaluate initial bacterial adhesion via turbidity test and colony-forming unit counting. The results showed that GT group presented the highest roughness, hydrophilicity and surface free energy. After 6-h incubation, GT group showed the significantly highest adhered bacteria counts; while non-significant difference existed between PT and PZ groups. Within the clinically applicable range used in present study, the surface physical characteristics, instead of surface chemical composition, of dental abutment material have the pronounced influence on initial 6-h bacterial adhesion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In order to restore the function and esthetic appearance of lost teeth, dental implant therapy is a common clinical modality nowadays. Currently, the 5-year survival rate of implant-supported fixed prosthesis has been shown to exceed 90% [1, 2]. Nonetheless, many researchers have pointed out mechanical and biological complications that can occur following implant insertion [3, 4]. Infection around implants is perhaps the most common complication reported. According to meta-analysis by Derks’ group, the prevalence of peri-implant mucositis is 43%, whereas peri-implantitis reaches 22% [5]. The massive bone loss following peri-implantitis greatly increases the cost and difficulty of restoring failed implants. Thus, the prevention of peri-implantitis has moved to the forefront of contemporary dental practice.
The development of peri-implantitis is influenced by multiple factors, while bacteria play a key role in disease progression. Researchers have yet conclusively identified the exact species that cause peri-implantitis; however, gram-negative anaerobic periodontal pathogens have been implicated [6, 7]. In oral cavity, these pathogens do not exist solitarily but locate in a complex system known as biofilm. The biofilm formation begins with acquired pellicle deposition, followed by the adhesion of primary colonizers, such as Streptococcus mitis. These primary colonizers metabolize and modify the micro-environment, thereby facilitating the cohesion of anaerobic periodontal pathogens that lead to following inflammation and bone resorption [8,9,10]. Once the biofilm system matured, the inner microorganism can be protected from the outer chemical and mechanical forces. So, it is important to control the biofilm formation at the beginning.
Factors associated with initial bacterial adhesion can be grossly classified as host-related, bacteria-related and substrate-related [1, 11,12,13]. Among these factors, the substrate-related factors might be the most manipulable one for clinician. In implant-restoration system, the transmucosal part, generally referred as the implant abutment, is very important because of its position as the forefront facing both supra-gingival and sub-gingival microbial challenges. The abutment should be selected carefully to provide mechanical, biological and esthetic advantages. Traditionally, titanium (Ti) is used as abutment material and proved with long term data support. Recently, zirconia (ZrO2) abutments are widely used because of its superiority in esthetics. Nonetheless, studies concerning the bacterial adhesion to zirconia and titanium have produced conflicting results [14,15,16,17,18]. Besides the surface chemical composition of implant abutment, the influences of physical surface characteristics, e.g., roughness, hydrophilicity, and surface free energy, should be taken into considerations as well.
Since there are so many different abutments that can be chosen nowadays, further clarification about the impacts of the abovementioned properties on bacterial adhesion are beneficial for clinicians in abutment selection, especially for those patients with high risks for peri-implant infections. However, studies discussing these surface characteristics mainly focus on implant fixture instead of abutments. Comprehensive studies which analyze all these characteristics of abutments were very limited. The aim of present study was to evaluate the impacts of surface chemical composition and physical characteristics on initial bacterial adhesion on implant abutments. Our null hypothesis is that the initial bacterial adhesion is influenced by the surface chemical composition of abutment as much as its physical characteristics.
2 Experimental
2.1 Sample preparation
Two kinds of clinical implant abutment materials were used in this study: commercially pure titanium (grade IV titanium, Ultimate Materials Technology, Hsinchu, Taiwan) and zirconia (yttria-stabilized tetragonal zirconia polycrystalline (Y-TZP), Coalition Technology, Tainan, Taiwan). Both materials were fabricated in the shape of round disks, with a diameter of 15 mm and a thickness of 1 mm.
Zirconia samples were mechanically polished to simulate clinical polished zirconia abutment. As for the titanium group, according to the data provided by manufacturers and previous study [19], the arithmetical mean roughness (Ra) of commercial standardized abutments varied according to brands and designs. Besides polished surfaces, another group of titanium samples underwent grinding using #240-grit SiC sandpaper to simulate the surface of those commercial titanium abutments with higher Ra. Three different sample groups were collected: polished zirconia group (PZ group), polished titanium group (PT group) and ground titanium group (GT group). All samples were cleaned using 75% ethanol, followed by distilled water with a sonicator and then air-dried and stored in a desiccator cabinet.
2.2 Chemical composition analysis
The surface chemical composition of the test samples was analyzed by X-ray photoelectron spectroscopy (XPS, Sigma Probe, Thermo-VG Scientific, Waltham, MA, USA). The X-ray source was monochromatic Al K-alpha (1486.6 eV), and the beam size was 400 µm. The wide energy range survey was performed for all group. Further Zr 3d and Ti 2p scans were performed in PZ and PT/GT groups for further clarification.
2.3 Physical characteristics analysis
The surface morphology of the samples was evaluated by optical microscope (OM, Olympus BX51 M, Olympus corporation, Tokyo, Japan) and atomic force microscope (AFM, Dimension Edge, Bruker corporation, Santa Barbara, CA, USA). Field emission scanning electronic microscope (FESEM, JSM-7600F, JEOL Ltd., Akishima, Tokyo, Japan) were also used to observe sample surface and adhered bacteria before and after bacterial culture.
A profilometer (Surtronic 3+, Taylor Hobson, Leicester, UK) was used to measure the surface roughness (Ra) of the tested samples at three randomly selected sites on each sample with cut-off length of 0.8 mm.
The sessile drop method was used to evaluate the surface hydrophilicity and surface free energy. Deionized water and diiodomethane were used as representative polar and non-polar liquids. The side view of droplets on the sample surface was recorded using a contact angle goniometer (Model 100SB, Sindatek, New Taipei City, Taiwan), and its corresponding software (MagicDroplet) was employed to calculate the surface free energy using Owens–Wendt method [20] and the Equation-of-state [21].
2.4 Bacterial adhesion analysis
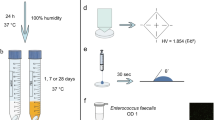
A pure strain of oral commensal frozen bacterium Streptococcus mitis (ATCC 49456) was revived with brain heart infusion (BHI) medium in an anaerobic environment at 37 °C. The bacteria were cultured to its logarithmic phase just before use. The optical density (OD, wavelength: 600 nm) of the bacteria suspension was measured by a spectrophotometer (U-1900, Hitachi High Technologies America, Waltham, MA, USA) and controlled around 0.9.
Following disinfection using ultraviolet irradiation, samples were placed into individual well of polystyrene culture test plates. 200 μl bacteria suspension was loaded onto each sample. After initial bacterial adhesion for 1 h, half of the samples were sent for bacteria counts. As for the remaining samples, 1 ml BHI medium was added to each well to provide nutrition for further bacterial dividing and growing. Following incubation for another 5 h, these samples were also sent for bacteria counting.
During the bacteria counting procedure, the culture medium was removed. The samples were gently washed with phosphate buffered saline (PBS) solution to remove the un-adhered bacteria. The samples with adhered bacteria were placed into new wells with PBS. The adhered bacteria were then transferred to PBS solution via sonication. The quantity of adhered bacteria was measured using two methods: turbidity measurement according to OD measurements by spectrophotometer, and conventional plate counting of colony-forming unit (CFU) following serial dilution.
2.5 Statistical analysis
Data of turbidity measurement and CFU counting were analyzed using two-way ANOVA with factors of study groups and incubation time. As for surface roughness, hydrophilicity and surface free energy, data were analyzed using one-way ANOVA. The post hoc Tukey HSD test was adopted for inter-group comparison. The probability value (P) was used for statistical evaluation. The significant level (α) was set at 0.05. Statistical significance existed if P < 0.05. All of the calculations were done by SPSS Statistics (IBM, Armonk, NY, USA).
3 Results
3.1 Chemical composition
The results of XPS analysis results are shown in Fig. 1. According to Fig. 1a, the major peaks in PT and GT groups were very similar, including Ti 2p and O 1s. The presence of C 1s peak noted in PT group might be related to the residual polishing grit used during manufacturing process. Figure 1c shows the Ti 2p scan of PT and GT groups. The binding energy of the peak located about 459 eV, which indicated the existence of TiO2. As for PZ group, according to Fig. 1b, the major peaks location indicated the presence of Zr 3d3, Zr 3p3, and O 1s. In Fig. 1d, the Zr 3d scan showed the peak located around 182 eV, which indicated the existence of ZrO2. To sum up, the main surface chemical composition of the PT and GT groups was TiO2, while the PZ group was composed of ZrO2.
3.2 Physical characteristics
Figure 2 shows the surface morphology of the test samples observed by OM, FESEM and AFM. The GT group presented even striations in a single direction, while the PT and PZ groups presented shallow, random carving marks. FESEM observation also presented similar results. The 3D reconstruction images from AFM showed uniform waves with greater amplitude in GT group, while small and even irregularity presented in PT and PZ groups.
The roughness of the three study groups is listed in Table 1. The GT group presented a significantly rougher surface than the other two groups (P < 0.05); however, no significant difference was observed between PT and PZ groups. Contact angle data pertaining to hydrophilicity are listed in Table 2. The contact angles (θ) of polar deionized water in PZ, PT and GT groups significantly differed from each other (P < 0.05). As for the contact angles of non-polar diiodomethane, significant greater value existed only in PT group (P < 0.05). The surface free energies of the test samples are listed in Table 3. Significant inter-group differences were observed among the three test groups (P < 0.05), regardless of the equation used.
3.3 Bacterial adhesion
The results of turbidity test are listed in Table 4. The OD of adhered bacteria varied according to the incubation time and study groups. Significant increase in OD were observed from 1 to 6 h of incubation in all groups (P < 0.05). After 1-h incubation, significant difference was observed only between PZ and GT groups. After 6 h, the GT group presented an OD higher than those of PT and PZ groups (P < 0.05); however, no significant difference was observed between PT and PZ groups.
Table 5 shows the results of CFU counting of adhered bacteria. All three study groups presented significant increases in the adhered bacteria between 1 and 6 h (P < 0.05). No significant inter-group differences in the amount of adhered bacteria were observed at 1 h. After 6 h, the GT group presented significantly more bacteria adhesion than the other two groups (P < 0.05); however, no significant difference was observed between PT and PZ groups.
Figure 3 shows the distribution and morphology of bacterial adhesion observed by FESEM. After 1-h incubation, bacteria adhered on all three study groups in a sparse manner without significant difference in density. After 6 h, the amount and density of adhered bacteria increased in all groups. Unlike the solitary presence observed in 1 h, most of bacteria presented in chains or clusters. Among the three study groups, the GT group showed the densest bacterial distribution.
4 Discussion
Surface roughness, chemical composition and many surface characteristics are shown to affect bacterial adhesion [22]. The importance of surface roughness in bacterial adhesion has been reported and rough surfaces are proved to facilitate bacterial adhesion [23,24,25]. This is commonly considered as a result of geometrical protection from shear forces and an increase in total surface area available. In present study, the GT group, which exhibited higher Ra (Table 1, Fig. 2), showed significantly more bacterial adhesion. The difference in bacterial adhesion between PT and PZ groups, which showed similar surface roughness (Table 1, Fig. 2), was non-significant (Fig. 3, Tables 4, 5). The results of present study supported the impact of surface roughness in bacterial adhesion. Clinically, the surface roughness should be carefully evaluated before abutment selection. Nonetheless, the importance of surface roughness should not be exaggerated. Seeking for abutments with extremely low Ra is neither practical nor reasonable because its influence gets limitations. Previous studies reported that when Ra is less than 0.2 µm, any reduction in surface roughness has no major effect on both bacteria species in biofilm and the amount of biofilm detected [19, 26]. Namely, this 0.2 µm “threshold of roughness” has been verified. In present study, the Ra values of PZ and PT groups were both under 0.2 µm. As for GT group, the one with Ra more than 0.2 µm showed the greatest amounts of adhered bacteria. Our results lent credence to the assumption of previous articles mentioned above.
Surface chemical composition of implant abutment is one of the most discussed issues in abutment selection. Titanium and zirconia are both common choices. In the present experiment, although PT and PZ groups were different in surface chemical composition (Fig. 1), they exhibited similar surface roughness (Table 1, Fig. 2) and we failed to observe significant differences in bacterial adhesion between these two groups (Fig. 3, Tables 4, 5). As for PT and GT groups, although their surface chemical compositions were similar, significant difference in bacterial adhesion existed. These findings indicated that, according to the condition setting in present study, surface chemical composition might not be the most important factor affecting bacterial adhesion. In previous studies, the performance of titanium and zirconia abutments in bacterial adhesion has been evaluated and the results showed diverse results [14,15,16,17,18]. Some of the studies concluded that the surface chemical composition of abutment does not affect the bacterial adhesion significantly [15,16,17], as the findings in present study. Some of the other studies favor the use of zirconia abutment (vs. titanium abutment) because of less bacterial adhesion [14, 18]. The conflict results might be related to the different surface physical characteristics of the test sample used. Although all of the abovementioned studies included both titanium and zirconia samples, the surface characteristics conditions in each study were either disregarded or very different.
However, in Scarano and his colleagues’ study, the Ra value of test titanium and zirconia is both about 0.7 µm [14]. This Ra value is clearly higher than that of clinically used abutments and other studies [16, 17]. Since bacteria tend to adhere on rougher surfaces, the higher amount of adhered bacteria is expected in Scarano’s study. Therefore, the effect of surface chemical composition on the adhered bacteria amount might be magnified to reach statistically significant level.
Clinically, both titanium and zirconia abutments are covered by bio-inert oxides (Fig. 1, TiO2 on titanium and ZrO2 on zirconia), instead of active pure titanium and zirconium elements. Even if bacteria might have different affinity toward these two oxides, the difference might be too small to reach significant level. Therefore, in this study, the PT and PZ samples with similar low Ra (~ 0.02 µm) had no statistically significant difference in bacterial adhesion amount (Tables 4, 5) even though both samples had different chemical compositions.
Some other researchers have emphasized the positive correlation of other surface characteristics, such as surface hydrophilicity and surface free energy, on bacterial adhesion [11, 27, 28]. In the present study, significant differences in surface hydrophilicity (Table 2) and surface free energy (Table 3) existed between all test groups. However, there was no significant difference in the amounts of adhered bacteria between PZ and PT groups (Fig. 3, Tables 4, 5). This disagreement might be a result from the difference in materials, experimental designs and methods used to detect bacteria. In the present study, the contact angles of PZ and PT groups both indicated hydrophobic surfaces, which were supposedly unfavorable to the initial bacterial adhesion. In the 6-h incubation test, the samples were immersed in plenty culture medium. This study setting attenuated the influence of hydrophilicity on bacterial adhesion.
Counting CFU on plates is regarded as a straightforward method for microbial quantification. This approach eliminates interference from dead bacteria; however, the complexity of the procedure can lead to technical errors. The measurement of turbidity according to OD value is relatively simple. However, unable to exclude dead microbes from living ones is its major limitation. In the present study, we adopted CFU counting as well as turbidity test to compensate for the shortcomings of both methods. As expected, CFU counting resulted in greater standard deviations, despite the fact that the statistical results coincided with those obtained through the turbidity test.
As for the influence of incubation time, significant difference existed in CFU of adhered bacteria between the GT group and the other two groups following incubation for 6 h; however, no difference was observed after just 1-h incubation (Fig. 3, Tables 4, 5). There were some possible explanations. First, we sought to simulate the oral environment of patients with good oral hygiene, which was clinically acceptable to start implant therapy, by using a relatively low concentration of loaded bacteria solution. It would be expected to take some time for bacteria to grow to a noticeable level. Second, in our experiment design, the bacteria incubation solution was added on the sample and left to stand still instead of shaking during the first hour of incubation to facilitate bacterial adhesion firmly. The dispersion of the solution would be influenced by hydrophilicity of samples initially. Since the samples were generally hydrophobic (Table 2), the dispersion of bacteria on test materials in 1-h incubation test might thus be limited. This partially explained that fact that there was no significant difference in bacterial adhesion after 1-h incubation on test samples (Tables 4, 5), regardless of surface chemical composition and roughness of samples.
In this study, both bacteria evaluation methods, turbidity measurement and CFU counting, revealed a significantly greater number of bacterial adhesions after 6-h incubation in GT group, which presented the highest roughness, hydrophilicity, and surface free energy. Unfortunately, interactions between roughness, hydrophilicity and surface free energy made it difficult to determine the impact of each characteristic independently. For example, the most common approach to measuring the surface free energy is by calculating the contact angle of polar and non-polar liquids using specific equations, i.e., hydrophilicity and surface free energy are mathematically related. Recent studies also pointed out that changes in roughness affect the hydrophilicity of a material [29, 30]. Thus, any attempt to explain the adhesion of bacteria based on a single factor must be done with caution.
5 Conclusion
In summary, the polished zirconia, polished titanium and ground titanium samples were prepared to simulate the clinically used dental implant abutments in present study. The number of initial adhered bacteria was more related to the physical characteristics of the surface than to the surface chemical composition. Among the surface physical characteristics studied, the hydrophilicity and surface free energy were less prone to influence the bacterial adhesion than the surface roughness. We would conclude that when considering the resistance to bacterial adhesion, dental clinicians should focus more on abutments’ surface roughness instead of surface chemical composition.
References
Doornewaard R, Christiaens V, De Bruyn H, Jacobsson M, Cosyn J, Vervaeke S, Jacquet W. Long-term effect of surface roughness and patients’ factors on crestal bone loss at dental implants. A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2017;19(2):372.
Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29(S):308.
Marcantonio C, Nicoli LG, Marcantonio Junior E, Zandim-Barcelos DL. Prevalence and possible risk factors of peri-implantitis: a concept review. J Contemp Dent Pract. 2015;16(9):750.
Link-Bindo EE, Soltys J, Donatelli D, Cavanaugh R. Common prosthetic implant complications in fixed restorations. Compend Contin Educ Dent. 2016;37(7):431.
Derks J, Tomasi C. Peri-implant health and disease. A systematic review of current epidemiology. J Clin Periodontol. 2015;42(S16):S158.
Rakic M, Grusovin MG, Canullo L. The microbiologic profile associated with peri-implantitis in humans: a systematic review. Int J Oral Maxillofac Implants. 2016;31(2):359.
Stokman MA, van Winkelhoff AJ, Vissink A, Spijkervet FK, Raghoebar GM. Bacterial colonization of the peri-implant sulcus in dentate patients: a prospective observational study. Clin Oral Investig. 2017;21(2):717.
Teughels W, Van Assche N, Sliepen I, Quirynen M. Effect of material characteristics and/or surface topography on biofilm development. Clin Oral Implants Res. 2006;17(S2):68.
Subramani K, Jung RE, Molenberg A, Hammerle CH. Biofilm on dental implants: a review of the literature. Int J Oral Maxillofac Implants. 2009;24(4):616.
Lee A, Wang HL. Biofilm related to dental implants. Implant Dent. 2010;19(5):387.
Elter C, Heuer W, Demling A, Hannig M, Heidenblut T, Bach FW, Stiesch-Scholz M. Supra- and subgingival biofilm formation on implant abutments with different surface characteristics. Int J Oral Maxillofac Implants. 2008;23(2):327.
Yamane K, Ayukawa Y, Takeshita T, Furuhashi A, Yamashita Y, Koyano K. Bacterial adhesion affinities of various implant abutment materials. Clin Oral Implants Res. 2013;24(12):1310.
De Bruyn H, Christiaens V, Doornewaard R, Jacobsson M, Cosyn J, Jacquet W, Vervaeke S. Implant surface roughness and patient factors on long-term peri-implant bone loss. Periodontol 2000. 2017;73(1):218.
Scarano A, Piattelli M, Caputi S, Favero GA, Piattelli A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: an in vivo human study. J Periodontol. 2004;75(2):292.
Salihoglu U, Boynuegri D, Engin D, Duman AN, Gokalp P, Balos K. Bacterial adhesion and colonization differences between zirconium oxide and titanium alloys: an in vivo human study. Int J Oral Maxillofac Implants. 2011;26(1):101.
van Brakel R, Cune MS, van Winkelhoff AJ, de Putter C, Verhoeven JW, van der Reijden W. Early bacterial colonization and soft tissue health around zirconia and titanium abutments: an in vivo study in man. Clin Oral Implants Res. 2011;22(6):571.
Egawa M, Miura T, Kato T, Saito A, Yoshinari M. In vitro adherence of periodontopathic bacteria to zirconia and titanium surfaces. Dent Mater J. 2013;32(1):101.
Nascimento C, Pita MS, Fernandes FH, Pedrazzi V, de Albuquerque Junior RF, Ribeiro RF. Bacterial adhesion on the titanium and zirconia abutment surfaces. Clin Oral Implants Res. 2014;25(3):337.
Bollen CM, Lambrechts P, Quirynen M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: a review of the literature. Dent Mater. 1997;13(4):258.
Owens DK, Wendt RC. Estimation of the surface free energy of polymers. J Appl Polym Sci. 1969;13(8):1741.
Kwok DY, Neumann AW. Contact angle measurement and contact angle interpretation. Adv Colloid Interface Sci. 1999;81(3):167.
Yeo IS, Kim HY, Lim KS, Han JS. Implant surface factors and bacterial adhesion: a review of the literature. Int J Artif Organs. 2012;35(10):762.
Tanner J, Robinson C, Soderling E, Vallittu P. Early plaque formation on fibre-reinforced composites in vivo. Clin Oral Investig. 2005;9(3):154.
Al-Ahmad A, Wiedmann-Al-Ahmad M, Fackler A, Follo M, Hellwig E, Bachle M, Hannig C, Han JS, Wolkewitz M, Kohal R. In vivo study of the initial bacterial adhesion on different implant materials. Arch Oral Biol. 2013;58(9):1139.
Badihi HL, Sela MN, Steinberg D, Rosen G, Kohavi D. The adhesion of oral bacteria to modified titanium surfaces: role of plasma proteins and electrostatic forces. Clin Oral Implants Res. 2013;24(SA100):49.
Quirynen M, Bollen CM, Papaioannou W, Van Eldere J, van Steenberghe D. The influence of titanium abutment surface roughness on plaque accumulation and gingivitis: short-term observations. Int J Oral Maxillofac Implants. 1996;11(2):169.
Al-Radha AS, Dymock D, Younes C, O’Sullivan D. Surface properties of titanium and zirconia dental implant materials and their effect on bacterial adhesion. J Dent. 2012;40(2):146.
Etxeberria M, Lopez-Jimenez L, Merlos A, Escuin T, Vinas M. Bacterial adhesion efficiency on implant abutments: a comparative study. Int Microbiol. 2013;16(4):235.
Saidi W, Hfayedh N, Megriche A, Girtan M, El Maaoui M. Hydrophilic/hydrophobic and optical properties of B2O3 doped TiO2 sol–gel thin films: effect of B2O3 content, film thickness and surface roughness. Mater Chem Phys. 2018;215(15):31.
Mozammel M, Khajeh M, Ilkhechi NN. Effect of surface roughness of 316L stainless steel substrate on the morphological and super-hydrophobic property of TiO2 thin films coatings. Silicon. 2018;10(6):2603.
Acknowledgements
This study was financially supported by the National Yang-Ming University Hospital (Nos. RD 2011-009, RD 2012-021 and RD 2013-013), Taiwan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, YS., Huang, HH. Effects of clinical dental implant abutment materials and their surface characteristics on initial bacterial adhesion. Rare Met. 38, 512–519 (2019). https://doi.org/10.1007/s12598-019-01219-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12598-019-01219-0