Abstract
Purpose
Although catheter ablation targeting the pulmonary vein (PV) is a well-known therapy for patients with paroxysmal atrial fibrillation (PAF), ectopic firings from the superior vena cava (SVC) can initiate PAF. The purpose of this study was to investigate predictors of SVC firing.
Methods
The subjects included 336 consecutive PAF patients (278 males, age 56.1 ± 10.8 years) undergoing atrial fibrillation (AF) ablation. The appearance of SVC firing was monitored throughout the procedure using a decapolar catheter with multiple electrodes to record electrograms of the coronary sinus and SVC. In addition to PV isolation, SVC isolation was performed only in patients with documented SVC firing.
Results
SVC firing was observed in 43/336 (12.8 %) of the patients, among whom complete isolation of the SVC was achieved in 40/43 (93 %) patients. A lower body mass index (BMI) (22.8 ± 2.8 vs 24.1 ± 3.1 kg/m2, p = 0.007) and higher prevalence of prior ablation procedures (58 vs 18 %, p = 0.0001) were related to the presence of SVC firing. In a multivariate analysis, a lower BMI (p = 0.012; odds ratio 0.83, 95 % CI 0.72 to 0.96) and history of prior ablation procedures (p < 0.0001; odds ratio 5.37, 95 % CI 2.71 to 10.63) were found to be independent predictors of the occurrence of SVC firing. Among 96 patients undergoing repeat ablation procedures, less PV-left atrial re-conduction was observed in patients with SVC firing than in those without (2.7 ± 1.2 vs 3.2 ± 0.8, p = 0.02).
Conclusions
The presence of SVC firing in patients with PAF is associated with a history of repeat ablation procedures and lower BMI values.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
As ectopic beats from the pulmonary vein (PV) have been demonstrated to be a major source of atrial fibrillation (AF), radiofrequency catheter ablation (RFCA) targeting the PV has been shown to be a therapy for paroxysmal AF (PAF) [1–3]. Ectopic firing from the superior vena cava (SVC) has been reported to initiate AF in some patients [4–7]. One study demonstrated that a female gender was associated with the presence of SVC ectopic beats [7]. However, the clinical predictors of the presence of ectopic firing from the SVC remain to be determined. In the present study, we retrospectively investigated predictors of firing from the SVC.
2 Methods
2.1 Study subjects
A total of 336 consecutive patients (278 males, age 56.1 ± 10.8 years) with PAF undergoing initial or repeat RFCA for AF was included in the present study. PAF was defined as AF lasting fewer than 7 days without treatment with antiarrhythmic drugs. The patients were divided into two groups according to the presence/absence of ectopic beats from the SVC.
2.2 Electrophysiological study
The ethics committee of our institution approved this study, and all patients provided their written informed consent to participate in this study. All antiarrhythmic drugs were discontinued for at least five half-lives before the procedure was performed. The electrophysiological study was performed under mild intravenous sedation. A steerable 16-polar (five poles for the SVC, one pole for the anode, and 10 poles for the coronary sinus) mapping catheter (InquiryTM Luma–CathTM, St. Jude Medical, St. Paul, MN, USA) was positioned within the coronary sinus via the right subclavian vein. A 7-F non-irrigated 8-mm-tip quadripolar ablation catheter (Fantasista, Japan Lifeline, Tokyo, Japan, or Blazer II, Boston Scientific, CA, USA) or an irrigated 3.5-mm-tip ablation catheter (Cool Path™ Duo™, St. Jude Medical, or ThermoCool Navistar, Biosense Webster) and a 20-polar circumferential mapping catheter (Lasso, Biosense Webster, Diamond Bar, CA, USA) were placed transseptally at the antrum of the targeted PVs. Selective PV angiography was performed in biplane views and displayed during the procedure to show the venous anatomy and the location of the left atrium (LA)-PV junction. PV mapping was performed with a 20-polar circumferential mapping catheter measuring 20, 25, or 30 mm in diameter. A dose of 100 U/kg body weight of heparin was administered intravenously following a transseptal puncture, followed by the continuous infusion of 1000 U/h of heparin to maintain an activated clotting time of 300–400 s as measured every 20 min [8]. A surface electrocardiogram and bipolar endocardial electrogram were continuously monitored and recorded for an off-line analysis (Bard Electrophysiology, Lowell, MA, USA, or EP Med System, Inc, West Berlin, NJ, USA). The intracardiac electrograms were filtered from 30 to 500 Hz.
2.3 Ablation procedure
In each case, all four PVs were targeted to be electrically disconnected individually from the LA at their antrum as previously described [9]. RFCA was performed with a non-irrigated 8-mm-tip or irrigated 3.5-mm-tip ablation catheter during either sinus rhythm or AF. The radiofrequency energy was applied at a target temperature of 50 °C with a power limit of 30 to 35 W for the non-irrigated catheter or 42 °C with 30 W for the irrigated catheter for 30 to 60 s at each site. Following the elimination of all PVPs, the absence of conduction from the PV to the LA was confirmed using circumferential pacing with a Lasso catheter. The end point was the establishment of a bidirectional conduction block between the LA and PV with the elimination of dormant PV conduction, as revealed by the administration of adenosine triphosphate. Cavotricuspid isthmus ablation was performed in all patients. In patients with non-PV AF, additional RFCA was performed to eliminate the arrhythmia.
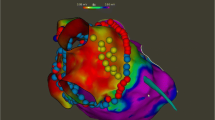
2.4 Detection of SVC firing and SVC isolation
In this study, SVC firing was defined as the presence of premature atrial beats from the SVC or the initiation of AF from ectopic beats of the SVC with/without the infusion of isoproterenol and/or adenosine triphosphate. For the detection of SVC firing, as well as PV re-conduction, isoproterenol (4–8 μg) was administered after the isolation of all four PVs in all procedures. Twenty milligrams of adenosine triphosphate injection was added after the isoproterenol injection. The induction protocol was the same in the initial and repeat procedures. The reproducibility of the presence of SVC firing was confirmed at least three times during the procedure. The presence of SVC firing was continuously monitored throughout the ablation procedure with a steerable 16-polar tow site (five poles for the SVC, one pole for the anode, and 10 poles for the coronary sinus) mapping catheter (Fig. 1a, b). In patients with suspected SVC firing, a 20-polar circumferential mapping catheter was placed within the SVC to confirm that the origin of the atrial arrhythmia was the SVC.
a Demonstration of simultaneous recordings of both surface and intracardiac electrograms when a short-coupled premature atrial beat induced the occurrence of atrial fibrillation. Leads II and V1 as well as the coronary sinus, right superior/right inferior pulmonary vein, and superior vena cava are shown. Note that the earliest activity of the premature atrial beat was identified as a sharp potential in the superior vena cava (asterisk). b Two Lasso catheters with a diameter of 25 and 20 mm were positioned at the antrum of the right superior pulmonary vein and right inferior pulmonary vein, respectively. Note that extra electrodes for the superior vena cava are shown
Patients with SVC firing underwent SVC isolation. SVC angiography was performed in the biplane views in order to visualize the SVC-right atrial (RA) junction. SVC mapping was then performed with a 20-polar circumferential mapping catheter measuring 20 mm in diameter. Segmental isolation was performed using a 7-F non-irrigated 8-mm-tip quadripolar ablation catheter (Fantasista, Japan Lifeline, Tokyo, Japan, or Blazer II, Boston Scientific, CA, USA) with a maximum power of 30 W and a maximum temperature of 50 °C for 30 to 60 s at each lesion. The end point was the establishment of a bidirectional conduction block between the RA and SVC [10]. To avoid phrenic nerve injury, radiofrequency application was withheld in cases of diaphragmatic stimulation.
2.5 Patient follow-up
After the ablation procedure, all patients received periodic follow-up examinations in an outpatient clinic at our institution. A recurrence of AF was diagnosed based on the patient symptoms, electrocardiogram recordings, and the results of 24-h ambulatory monitoring (at 1, 3, and 6 months, then every year, after the procedure). In this study, recurrence was defined as episodes of atrial tachyarrhythmia lasting more than 30 s after a 90-day-blanking period. Repeat ablation procedures were recommended for patients with recurrence.
2.6 Statistical analysis
Continuous variables are expressed as the mean ± SD. Comparisons between groups were made using Student’s t test (unpaired). Proportions were compared using a chi-square analysis. A multivariate analysis was performed with a logistic regression model to determine independent predictors of ectopic beats from the SVC. Differences with a p value of <0.05 were considered to be statistically significant. Receiver-operating characteristic curves were used to determine the BMI cutoffs for optimal sensitivity and specificity for the prediction of SVC firing.
3 Results
3.1 Prevalence of SVC firing
SVC firing was detected in 43 (12.8 %) patients, 25 (58.1 %) cases of which were found only during the repeat ablation procedures. SVC firing without AF initiation was observed in 21 (48.8 %) patients, while the initiation of AF from SVC ectopy was detected in 22 (51.2 %) patients. The infusion of isoproterenol was required to reveal SVC firing in 10 (23.3 %) patients, whereas spontaneous SVC firing was noted in the remaining 33 (76.7 %) patients. During the repeat procedure, isoproterenol was required in only 4 (16.0 %) patients. With respect to PV isolation, 6 (33.3 %) and 13 (52.0 %) cases of SVC firing were detected before completion of the PV isolation during the initial and repeat procedures, respectively.
3.2 Patient characteristics and predictors of SVC firing
The clinical characteristics of the patients with and without SVC firing are shown in Table 1. According to a univariate analysis, patients with SVC firing had significantly lower body mass index (BMI) values, a higher number of prior AF ablation procedures, and higher brain natriuretic peptide values. A multivariate analysis revealed that a lower BMI value (p = 0.01) and history of prior ablation procedures (p < 0.001) independently predicted the presence of SVC firing (Table 2). Among the total study population, the distribution of gender did not differ between the patients with and without SVC firing (p = 0.84). The BMI values were similar between the male patients with and without SVC firing (23.6 ± 2.3 vs 24.1 ± 2.8, p = 0.30) and significantly lower in the patients with SVC firing than in those without among the female patients (19.6 ± 2.4 vs 24.2 ± 4.4, p = 0.004, Fig. 2). The receiver-operating characteristic curve identified a BMI 21 as the optimal cut point, with 77.8 % sensitivity and 77.6 % specificity for the detection of SVC firing in female patients.
Distribution of the patients with SVC firing according to the BMI value. The black and white bars indicate male and female patients with SVC firing, respectively. The bars express the percentage of patients with SVC firing. In nine female patients with SVC firing, the prevalence of SVC firing at BMI values of 16, 17, 18, 19, 20, 21, 22, 23, and 24 were 100 (1/1), 67 (2/3), 0 (0/1), 40 (2/5), 25 (1/4), 17 (1/6), 11 (1/9), 0 (0/5), and 17 % (1/6), respectively. In contrast, in 34 male patients, the prevalence of SVC firing at BMI values of 20, 21, 22, 23, 24, 25, 26, 27,28, 29, 30, and 31 were 13 (1/8), 22 (4/18), 18 (8/45), 13 (4/31), 15 (7/47), 14 (6/45), 4 (1/24), 4 (1/24), 11 (1/9), 0 (0/8), 0 (0/1), and 20 % (1/5), respectively. The data showed that a lower BMI value was more frequently observed in female patients with SVC firing. In contrast, a lower BMI value was equally distributed in male patients with/without SVC firing
3.3 Ablation results
All targeted PVs were electrically isolated from the LA. Sixty-nine (23.5 %) of the patients without SVC firing required repeat ablation procedures (two and three procedures in 65 and four patients, respectively), whereas 34 (79.1 %) of those with SVC firing underwent repeat procedures (two, three, and four procedures in 28, four, and two patients, respectively, p < 0.001). In 18 patients with SVC firing detected during the initial procedure, 11 (61.1 %) patients continued to be in sinus rhythm following the initial procedure. During the repeat procedures, PV-LA re-conduction was less frequently observed in the patients with SVC firing than in those without (2.7 ± 1.2 vs 3.2 ± 0.8 PVs, respectively, p = 0.02); all such cases were successfully re-isolated.
The SVC was successfully isolated in 93 % (40/43, 18 in the initial, 22 in the repeat procedure) of the patients who underwent SVC isolation for SVC firing; SVC isolation was not achieved in the remaining three patients in the second procedure due to the possibility of phrenic nerve damage. Eight patients had AF recurrence (four with SVC triggered AF and four with SVC triggered ectopy), and SVC-RA re-conduction was detected in all five patients undergoing repeat procedures following SVC isolation, all cases of which were successfully re-isolated. SVC firing was detected in 40 % (2/5) of these patients. Complications related to SVC isolation were observed in three patients (phrenic nerve injury two patients and sinus node injury in one). Two patients with phrenic nerve injury showed decreased phrenic movement during the procedure and right diaphragm paresis on chest X-rays the day after the procedure. Both patients were asymptomatic, and their diaphragm movement recovered 1 month after the procedure. One patient with sinus node injury showed significant sinus bradycardia during the RF application to the SVC, which recovered 2 months after the procedure.
Other non-PV foci were more frequently observed in patients with SVC firing than in those without (13/43 (30.2 %) vs 17/293 (5.8 %), p < 0.0001). In patients with SVC firing, 8/13 (61.5 %) of non-PV foci were from the right atrium, including 5 (38.5 %) from the crista terminalis, while 9/17 (52.9 %) of those without SVC firing were from the right atrium, including 2 (11.8 %) from the crista terminalis.
PV foci were equally distributed in patients with and without SVC firing (20/43 (46.5 %) vs 158/293 (53.9 %), p = 0.46).
4 Discussion
In this study, we showed that a lower BMI, particularly in females, and history of prior AF ablation can be used to predict the presence of SVC firing. The unique mapping catheters used in both the coronary sinus and SVC easily detected the presence of SVC firing by providing continuous monitoring throughout the ablation procedure. In the repeat procedures, the patients with SVC firing exhibited less frequent PV-LA re-conduction.
4.1 Prevalence and mapping of SVC firing
Previous studies have demonstrated that the prevalence of SVC foci initiating AF ranges from 11 to 13 % among PAF patients [6, 7]. Our finding that 13 % of PAF patients had SVC firing is consistent with previous results. Mapping for SVC foci has been performed in previous studies following mapping and ablation of the LA, which may result in the missed detection of transient SVC firing. The mapping catheter in the coronary sinus with “extra” electrodes for the SVC and high RA used in our study is a simple tool for detecting arrhythmias originating from the RA, including the SVC throughout the procedure.
4.2 Predictors of SVC firing
Lee et al. [7] showed that a female gender predicts the presence of SVC ectopic beats. The authors suggested that female hormones and a higher parasympathetic tone in females may explain the higher incidence of SVC firing, without definitive evidence. On the other hand, a female gender was almost equally distributed among the patients with/without SVC firing in our patient population. Instead, SVC firing was more frequently observed in patients with a lower BMI. While the BMI values were similar in the patients with and without SVC firing among males, they were significantly lower in the patients with SVC firing among females in our data. This discrepancy between previous and the present findings may be due to differences in the study populations. One study demonstrated that patients with a higher BMI had an increased LA volume and shortened effective refractory period in the LA and PV, possibly contributing to the facilitation and perpetuation of AF [11]. In the present study, we first demonstrated that, among female AF patients, a lower BMI is likely associated with SVC firing.
4.3 PV-LA re-conduction in the repeat procedures
In the present study, PV-LA re-conduction was less frequently observed among the patients with SVC firing during the repeat procedures, suggesting that both PV and non-PV foci should be carefully mapped in patients with fewer PV-LA re-conductions. Ouyang et al. [12] showed that recovered PV-LA conduction is the dominant factor for AF recurrence. In their patients without recovered PV-LA conduction, non-PV foci were responsible for the recurrence of AF consistent with our findings.
4.4 Limitations
The present study is associated with several limitations. First, since a small number of patients were evaluated retrospectively in this study, prospective studies with a larger number of patients should be performed to provide a more detailed analysis including the association between a lower BMI and the presence of SVC firing. Second, since late recurrence of AF from the SVC can occur in patients without SVC firing, a longer follow-up period should be considered. Third, the occurrence of catheter-induced ectopy from the SVC cannot be ruled out. However, isoproterenol, which can increase cardiac and catheter movement, was not required to reveal SVC firing in most cases. Thus, catheter-induced ectopy should be rare due to the stable catheter location. Fourth, since the relation between the SVC firing detected during the procedure and clinical atrial arrhythmia cannot be determined, the contributions of additional SVC isolation remained to be unclear.
5 Conclusion
A lower BMI and history of prior AF ablation can be used to predict the presence of SVC firing. Mapping catheters for the coronary sinus with extra electrodes for the SVC are useful for detecting SVC firing. In this study, patients with less PV-LA conduction exhibited SVC firing more frequently; thus, careful mapping of the SVC should be considered in this population.
References
Haissaguerre, M., Jais, P., Shah, D. C., Takahashi, A., Hocini, M., Quiniou, G., et al. (1998). Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. The New England Journal of Medicine, 339(10), 659–666.
Jais, P., Cauchemez, B., Macle, L., Daoud, E., Khairy, P., Subbiah, R., et al. (2008). Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation, 118(24), 2498–2505.
Sawhney, N., Anousheh, R., Chen, W. C., Narayan, S., & Feld, G. K. (2009). Five-year outcomes after segmental pulmonary vein isolation for paroxysmal atrial fibrillation. The American Journal of Cardiology, 104(3), 366–372.
Chen, S. A., Tai, C. T., Yu, W. C., Chen, Y. J., Tsai, C. F., Hsieh, M. H., et al. (1999). Right atrial focal atrial fibrillation: electrophysiologic characteristics and radiofrequency catheter ablation. Journal of Cardiovascular Electrophysiology, 10(3), 328–335.
Tsai, C. F., Tai, C. T., Hsieh, M. H., Lin, W. S., Yu, W. C., Ueng, K. C., et al. (2000). Initiation of atrial fibrillation by ectopic beats originating from the superior vena cava: electrophysiological characteristics and results of radiofrequency ablation. Circulation, 102(1), 67–74.
Lin, W. S., Tai, C. T., Hsieh, M. H., Tsai, C. F., Lin, Y. K., Tsao, H. M., et al. (2003). Catheter ablation of paroxysmal atrial fibrillation initiated by non-pulmonary vein ectopy. Circulation, 107(25), 3176–3183.
Lee, S. H., Tai, C. T., Hsieh, M. H., Tsao, H. M., Lin, Y. J., Chang, S. L., et al. (2005). Predictors of non-pulmonary vein ectopic beats initiating paroxysmal atrial fibrillation: implication for catheter ablation. Journal of the American College of Cardiology, 46(6), 1054–1059.
Calkins, H., Kuck, K. H., Cappato, R., Brugada, J., Camm, A. J., Chen, S. A., et al. (2012). 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Journal of Interventional Cardiac Electrophysiology, 33, 171–257.
Yamane, T., Date, T., Kanzaki, Y., Inada, K., Matsuo, S., Shibayama, K., et al. (2007). Segmental pulmonary vein antrum isolation using the “large-size” Lasso catheter in patients with atrial fibrillation. Circulation Journal, 71(5), 753–760.
Tada, H., Naito, S., Meguro, K., Nogami, A., & Taniguchi, K. (2004). Persistent tachycardia originating from the superior vena cava as a driver for atrial fibrillation. Pacing and Clinical Electrophysiology, 27(2), 252–255.
Munger, T. M., Dong, Y. X., Masaki, M., Oh, J. K., Mankad, S. V., Borlaug, B. A., et al. (2012). Electrophysiological and hemodynamic characteristics associated with obesity in patients with atrial fibrillation. Journal of the American College of Cardiology, 60(9), 851–860.
Ouyang, F., Antz, M., Ernst, S., Hachiya, H., Mavrakis, H., Deger, F. T., et al. (2005). Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation, 111(2), 127–135.
Acknowledgments
We are grateful to Brain Quinn (Editor-in-Chief, Japan Medical Communication) for providing linguistic comments on the manuscript.
Conflict of interest
None of the authors has any relevant conflicts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inada, K., Matsuo, S., Tokutake, Ki. et al. Predictors of ectopic firing from the superior vena cava in patients with paroxysmal atrial fibrillation. J Interv Card Electrophysiol 42, 27–32 (2015). https://doi.org/10.1007/s10840-014-9954-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-014-9954-3