Abstract
Background
Benefit from cardiac resynchronization therapy (CRT) is likely influenced by the location of the left ventricular (LV) lead.
Purpose
To evaluate the association of LV lead position with outcome after CRT.
Methods
Two-hundred and fifty patients with LV dysfunction, New York Heart Association (NYHA) class III (68%) or IV (32%) symptoms, and QRS durations ≥120 ms were followed for a median of 30 months post-CRT. LV lead position was categorized as anterior (n = 20, 8%), lateral (n = 128, 51%), or posterior (n = 102; 41%) using postero-anterior and lateral postoperative chest radiographs.
Results
Median age was 69 years and most (68%) had ischemic LV dysfunction. Clinical response, defined by a ≥1 NYHA class reduction, was lower in patients with an anterior (30%) versus lateral (76%) or posterior (73%) lead position (p = 0.001). An anterior versus nonanterior position was independently associated with a two to three-fold higher risk for nonresponse to CRT, cardiovascular death, death from worsening heart failure or cardiac transplantation, and death from any cause. Repositioning of the LV lead from an anterior to a nonanterior position in seven patients who had not clinically responded to CRT after ≥6 months resulted in clinical improvement in all cases.
Conclusions
An anterior versus nonanterior LV lead position is independently associated with an increased likelihood of nonresponse to CRT and a higher risk of serious outcomes. Repositioning of an anteriorly placed LV lead to a nonanterior position should be considered in CRT nonresponders.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Cardiac resynchronization therapy (CRT) reduces heart failure symptoms and improves survival in patients with left ventricular (LV) ejection fraction values ≤0.35, conduction delay, and highly symptomatic heart failure [1–8]. Thus, it is recommended for routine use in these patients [9, 10]. Despite the demonstrated efficacy of CRT, a significant proportion of patients fail to derive sustained benefit from (i.e., respond to) this therapy. The proportion of patients responding to CRT is frequently estimated to exceed 75% based on improvement in symptoms [11]. However, these estimates do not take into account the effect of surgery itself, as most studies did not mask treatment allocation. When CRT response is restricted to symptomatic improvement plus favorable LV remodeling, fewer than 60% of patients are categorized as responders [12].
The LV pacing site appears to be important with respect to the benefit from CRT. The site of latest LV activation in most CRT candidates is typically lateral or posterior [13]. Pacing from an anterior site is generally associated with less acute hemodynamic benefit [14, 15] and reduced clinical benefit over time [14, 16–18]. Whether an anterior LV pacing site is associated with a higher risk of serious clinical outcomes is unclear. The purpose of this study was to evaluate the relationship of LV lead pacing site, defined using postoperative chest radiographs, with the risks of death from any cause, cardiovascular death and heart failure progression (composite of death from heart failure or need for cardiac transplant), and with the rate of clinical response to CRT.
2 Materials and methods
The study population included 250 consecutive patients with LV ejection fraction values of 0.35 or less, QRS durations of at least 120 ms, and New York Heart Association (NYHA) III or IV symptoms despite optimal medical therapy who received transvenous CRT systems between January 2002 and September 2006. All surviving patients were followed for at least 12 months. The protocol was reviewed and approved by the Conjoint Ethics Committee at the University of Calgary. Patients in whom an LV lead could not be successfully placed transvenously (n = 5) were excluded. Patients were included irrespective of the etiology of heart failure, or whether they had conventional indications for bradycardia pacing or an implantable cardioverter defibrillator.
2.1 Follow-up
Follow-up visits occurred at 2, 6 and 12 months postoperatively and then every 6 months. At each visit, functional status was recorded and device interrogation was performed.
2.2 Outcome assessment
All deaths occurring in follow-up were recorded, and the cause was categorized after review of all available clinical and pathologic data. Death from any cause was the principle study outcome. Cardiovascular death was defined as death due to myocardial infarction, stroke, arrhythmia, heart failure progression, or resulting from complications of treatment of these conditions [19]. The composite measure of heart failure progression (death attributable to worsening heart failure or need for cardiac transplant) was also chosen to provide a sensitive indicator of disease progression. Patients were censored after a first event. The vital status of all patients as of November 30, 2007 was verified, with no patient lost to follow-up. Clinical response to CRT was also assessed to correlate change in the aforementioned outcomes with functional status. Patients who survived for at least 6 months and had an improvement of at least one NYHA functional class over the initial 6 months of follow-up were categorized as having responded to CRT. While clinical data at six months was available for all patients, complete data on adjudicated causes of hospitalization during long term follow-up was not.
2.3 CRT implant details
The LV lead was positioned in a branch of the coronary sinus with the aid of contrast venography and intra-operative fluoroscopy (left anterior oblique of 30° to 60° and right anterior oblique of 30° to 45°). A posterior or lateral coronary sinus branch was most often targeted, though the final position was guided by the coronary sinus anatomy and the ability to obtain satisfactory pacing thresholds without phrenic nerve stimulation. Most patients with ischemic heart disease had suffered multiple prior infarctions. In these patients, care was taken to place the LV lead in a viable segment. This was facilitated by use of preoperative cardiac magnetic resonance imaging [20, 21] and echocardiographic tissue Doppler strain analyses [22].
2.4 Categorization of LV lead position
The final LV lead position was categorized using postero-anterior (PA) and lateral chest radiographs performed the day after CRT implantation (Fig. 1). Three individuals (SBW, MAS, and RS) unaware of the patient’s vital status or clinical response to CRT independently interpreted each pair of radiographs. On the lateral film, the LV lead tip was classified as “anterior”, “middle”, or “posterior” using anatomic landmarks (see legend of Fig. 1 for description and Fig. 2 for examples). On the PA film, the LV lead tip was classified as “basal”, “mid”, or “apical” by dividing the ventricular silhouette into basal, middle, and apical thirds (Fig. 1). Rotation of the heart was considered to be present when the tip of an apically placed right ventricular lead was directed posteriorly on the lateral film. Disagreement occurred in only seven of 250 cases and was resolved by consensus. This classification system was chosen over a fluoroscopic approach [23] because the standard orthogonal views provide comparable lead tip localization and can easily be used serially to assess changes in position over time.
Categorization of left ventricular lead position from chest radiographs. On the postero-anterior film (upper panel), left ventricular lead tip position was localized to the base, mid, or apical third of the LV silhouette. On the lateral film (lower panel), the LV lead tip position was categorized as anterior (Ant), lateral (Lat), or posterior (Post) based on the position of the LV lead tip with relative to the aortic arch (anterior to its posterior junction with the heart, below it, or posterior to the left subclavian artery origin, respectively)
Sample chest radiographs illustrating an anterior versus posterior lead position. Note the similar appearance on the postero-anterior films (left panels) but the marked differences in left ventricular lead position on the lateral films (right panels). On the top panel, the left ventricular lead is in a basal to mid anterior position, while in the bottom panel the LV lead is in a basal to mid posterior position. Image contrast has been modified to enhance lead visibility
2.5 Statistical analysis
Continuous variables were expressed as median (interquartile range) and compared among the lead position groups using the Kruskal–Wallis test. Pairwise comparisons were evaluated with the Wilcoxon rank sum test. Categorical variables were compared using a Fisher’s exact test. The proportional hazards assumption was verified using log–log plots. Cox models were used to assess the association between lead position and outcome. Variables known or suspected to be associated with outcome were included in the models. They included age, gender, baseline LV ejection fraction, NYHA class, QRS duration, etiology of LV dysfunction, and medications. Two-sided p-values of <0.05 were deemed significant. All analyses were performed using Stata 9.2 MP software (Stata Corp., TX, USA).
3 Results
The distribution of final LV lead tip positions is shown in Table 1. Twenty patients had an anterior position and 26 patients had leads placed in apical segments of posterior or lateral branches, but no patient had an anterior lead placed in an apical segment. The baseline characteristics of patients with anterior, lateral, and posterior lead positions are shown in Table 2. The three groups were well matched in most respects, but differences in age (p = 0.04), the proportion of males (p = 0.04), use of angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocker (ARB) therapy (p = 0.008), and median QRS width (p = 0.02) were apparent. Only median QRS duration significantly differed among patients with an anterior versus nonanterior lead position (p = 0.02). Most patients received a defibrillator, two thirds had an ischemic etiology of LV dysfunction, and one third had NYHA class IV symptoms at baseline. Use of evidence-based medications for heart failure was similarly high in all three groups.
3.1 Clinical outcomes
During a median follow-up of 30 months, 64 patients (26%) died. Most (48 of 64; 75%) deaths were categorized as cardiovascular and the majority of cardiovascular deaths (38 of 48; 79%) were attributed to worsening heart failure. Another ten patients underwent cardiac transplantation for worsening heart failure. Of the 20 patients with an anterior pacing site, 11 deaths (55%) were observed over a median of 19.0 (13.6, 23.0) months. Nine of the 11 deaths (81%) were categorized as cardiovascular. All nine of these deaths (81% of all deaths) were attributed to worsening heart failure. Of the 128 patients with a lateral pacing site, 31 deaths (24%) were observed over a median of 9.2 (4.7, 32.6) months. Of these, 22 (71%) were categorized as cardiovascular deaths and 18 (58%) were attributed to worsening heart failure. Five other patients with a lateral pacing site underwent cardiac transplantation. Of the 102 patients with a posterior pacing site, 22 deaths (22%) were observed over a median of 13.7 (7.2, 24.2) months. Of these, 17 (77%) were categorized as cardiovascular. Thirteen deaths (59%) were attributed to worsening heart failure. Five patients with a posterior pacing site underwent a cardiac transplant for worsening heart failure. Kaplan–Meier curves for cardiovascular death and heart failure progression are shown in Fig. 3.
Risk of outcomes over time, by lead position. Time to death (upper panel), cardiovascular death (middle panel), and death from heart failure or the need for cardiac transplantation (lower panel). Patients with an anterior site were at higher risk for each outcome. Log-rank p-values for the comparison among all three groups are shown in the upper left of each graph. The number of patients at risk of death in each of the time periods is shown below
3.1.1 Unadjusted models
An anterior versus nonanterior LV lead position was associated with a higher risk of death from any cause, a higher risk of cardiovascular death, and a higher risk of heart failure progression (Table 3). The risk of death from any cause (hazard ratio (HR) 1.2, 95% confidence interval (CI) 0.7 to 2.0), cardiovascular death (HR 1.2, 95% CI 0.6 to 2.4), and the risk of heart failure progression (HR 1.3, 95% CI 0.6 to 2.7) were similar for patients with a lateral versus a posterior lead position. An apical versus a nonapical position was associated with a similar risk of death from any cause (HR 1.1, 95% CI 0.5 to 2.5), cardiovascular death (HR 0.8, 95% CI 0.3 to 2.3), and heart failure progression (HR 0.7, 95% CI 0.2 to 2.3).
The presence of NYHA class IV symptoms at baseline was associated with an increased risk of death (HR 3.0, 95% CI 1.8 to 4.9), cardiovascular death (HR 4.5, 95% CI 2.4 to 8.4), and heart failure progression (HR 5.8, 95% CI 2.8 to 11.7). Male gender was also associated with an increased risk of death (HR 5.2, 95% CI 1.6 to 16.5), cardiovascular death (HR 5.3, 95% CI 1.3 to 21.9), and heart failure progression (HR 4.6, 95% CI 1.1 to 19.2). An ischemic versus nonischemic etiology of LV dysfunction tended to be associated with a higher risk of death (HR 1.9, 95% CI 1.0 to 3.5) and heart failure progression (HR 2.3, 95% CI 1.0 to 5.2), while increasing baseline QRS duration tended to be associated with an increased risk of cardiovascular death (HR 1.1, 95% CI 1.0 to 1.2 per 10 ms increase in QRS duration).
3.1.2 Multivariate models
An anterior versus nonanterior LV lead position remained independently associated with a higher risk of death from any cause, cardiovascular death, and heart failure progression after adjustment (Table 3). Baseline NYHA functional class IV versus III status was associated with an increased risk of death (HR 2.9, 95% CI 1.7 to 4.9), cardiovascular death (HR 3.9, 95% CI 2.0 to 7.7), and heart failure progression (HR 5.4, 95% CI 2.6 to 11.5) in the fully adjusted model. Male gender was associated with an increased risk of death (HR 4.0, 95% CI 1.2 to 13.3) and cardiovascular death (HR 4.8, 95% CI 1.1 to 20.7). An ischemic versus nonischemic etiology of LV dysfunction tended to be associated with a higher risk of heart failure progression (HR 2.5, 95% CI 1.0 to 6.3).
3.2 Clinical response to CRT
A reduction in NYHA symptoms and survival for ≥6 months was observed in 30%, 76%, and 73% of in the anterior, lateral, and posterior groups, respectively (p < 0.001). The risk of nonresponse to CRT was similar for patients with a lateral versus posterior (HR 0.9, 95% CI 0.6 to 1.5; p = 0.7) and for patients with an apical versus nonapical lead position (HR 1.7, 95% CI 0.9 to 3.2). In contrast, an anterior versus nonanterior lead position was associated with significantly higher risk of nonresponse (Table 3). In addition to an anterior versus nonanterior lead position, an ischemic versus nonischemic etiology of LV dysfunction (HR 2.6, 95% CI 1.4 to 4.8) and class IV versus III functional impairment (HR 1.9 95% CI 1.2 to 3.0) individually predicted a higher risk of nonresponse. Similar findings were observed after adjustment for disease severity and medication use (Table 3). In the fully adjusted models, an ischemic versus nonischemic etiology of LV dysfunction (HR 2.8, 95% CI 1.4 to 5.4) and class IV versus III functional impairment (HR 1.8 95% CI 1.1 to 3.0) remained independent predictors of a higher risk of nonresponse to CRT.
3.3 Stratified analyses
3.3.1 Etiology of heart failure
Since etiology of LV dysfunction was an independently associated with outcome, a stratified analysis was performed. The association between an anterior lead position and the risk of death, cardiovascular death, heart failure progression, and clinical response to CRT was similar, regardless of etiology of LV dysfunction.
3.3.2 QRS duration
Since baseline differences in QRS duration were observed in the anterior versus nonanterior groups, the 181 patients (72%) with baseline QRS durations of at least 150 ms were assessed separately. In these patients, an anterior lead position was strongly associated with an increased risk of death (HR 3.2, 95% CI 1.5 to 6.7), cardiovascular death (HR 3.7, 95% CI 1.6 to 8.2), heart failure progression (HR 4.4, 95% CI 1.9 to 10.0), and nonresponse to CRT (HR 3.4, 95% CI 1.8 to 6.4).
3.3.3 Heart rotation
Due to potential misclassification of lead position related to heart rotation, analyses were restricted to the 196 patients (78%) with a nonrotated heart, as assessed by the position of the RV lead on the lateral film. The associations between anterior versus nonanterior LV lead position remained statistically associated with a higher risk of death (2.5, 95% CI 1.2 to 5.0), cardiovascular death (HR 3.0, 95% CI 1.4 to 6.5), heart failure progression (HR 3.5, 95% CI 1.6 to 7.7), and lack of clinical response to CRT (HR 3.1, 95% CI 1.7 to 5.5).
4 Discussion
This analysis demonstrates that on average, LV pacing from an anterior versus nonanterior site is independently associated with a greater than two fold higher risk of death, cardiovascular death, heart failure progression and nonresponse to CRT. In contrast, pacing from a lateral or posterior LV site and from a basal or mid versus apical segment is associated with similar outcomes in CRT recipients.
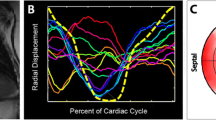
4.1 Late electromechanical activation and response to CRT
The posterior or lateral LV is typically the latest region of electrical and mechanical activation in patients referred for CRT [24, 25]. Pacing near the latest site of electrical or mechanical activation has been linked to greater mechanical remodeling and higher rates of clinical response with CRT [26–28]. Further, pacing from an early activating site has been shown to acutely worsen hemodynamic parameters [29].
4.2 Clinical outcomes
Previous studies have demonstrated that an anterior LV pacing site is typically associated with a lesser degree of hemodynamic improvement at the time of implant [14, 26, 30] and with reduced clinical benefit over time [14, 16–18]. We have extended these observations by demonstrating that pacing from an anterior site is associated with a higher risk of serious clinical outcomes. These results complement the findings of Rossillo and colleagues, who found a lower rate of functional improvement with pacing from an anterior or anterolateral versus other pacing site. In that analysis, patients with either an anterior or anterolateral (n = 66; 28%) were less likely to exhibit structural remodeling compared to patients with other LV pacing sites (n = 167; 72%) [17]. However, unlike Rossillo et al., who found no difference in survival between these patient groups, we were able to demonstrate alterations in these hard clinical outcomes. Despite having similar numbers of patients, there are important differences between the present study and that analysis. In that analysis, anterior and anterolateral lead positions were combined, while in the present study, only an anterior position was used. An animal study using three-dimensional mapping to determine the optimal pacing sites for resynchronization therapy found that all lateral sites, including anterolateral ones, were equally efficacious [31]. Differences in prescription of heart failure medications may also be relevant due to the time frame in which the cohort of Rossillo and colleagues versus ours was enrolled. Our study population also contained a higher proportion of patients with NYHA class IV symptoms (32%) as compared to that cohort (11%). Thus, a difference in mortality, cardiovascular death, and heart failure progression would be more likely to be detected in the present analysis.
4.3 Is pacing from an anterior site detrimental?
This study was not designed to address whether pacing at an anterior position is worse than withholding CRT. This question can only be addressed in a properly designed randomized trial. However, the observed rate of clinical response to CRT in the present analysis among patients with an LV lead in an anterior position (30%) is similar to that observed in control patients enrolled in the Multicenter InSync Randomized Clinical Evaluation (MIRACLE) trial (38%), patients who received a CRT device but in whom the CRT device was left inactive [3]. Furthermore, the mortality rate in the placebo arm in the Cardiac Resynchronization Heart Failure (CARE HF) trial (39% at 29 months) [6] is the same as the rate observed among patients with a lead in an anterior position in this analysis (39% at 29 months). These data suggest that while an anterior LV lead position is clearly inferior to a lateral or posterior location, an anterior position does not likely result in clinical deterioration, given that the present study population had a high proportion of patients with NYHA class IV symptoms (32%) as compared to MIRACLE (9%) and CARE HF (7%).
4.4 Limitations
This was a retrospective observational analysis and is subject to bias. Several steps were taken to minimize bias. Enrollment of consecutive patients minimized selection bias. Standardized and complete follow-up was achieved, minimizing follow-up bias. Blinded categorization of lead position minimized misclassification bias. Furthermore, unambiguous clinical events (mortality, cardiovascular death, heart failure progression) were used as the principle outcome measures. While heart failure hospitalization is another means to measure benefit from CRT, these data were not available. Furthermore, our definition of clinical response to CRT, change in NYHA class, is subjective. This data was provided as ancillary data on CRT response rather than a definitive measure of benefit. Detailed information on disease severity and medications were available for all subjects, allowing appropriate statistical adjustment. Statistical adjustment for potential confounding variables did not significantly alter the observed association between an anterior versus nonanterior lead position with a higher risk of serious clinical outcomes.
4.5 Lead delivery
Advances in lead delivery methods have enhanced the ability to target LV lead position. Based on a preliminary analysis of our data [32], seven of the surviving patients with an anterior LV lead position who had not responded to CRT underwent a repeat procedure to reposition the LV lead in a posterolateral location. Using subselective guiding catheters, a nonanterior lead position was obtained in all seven cases. All seven patients have shown evidence of clinical response to CRT. Three patients have subsequently improved by two NYHA classes and four by one NYHA class at 6 months following LV lead revision. Furthermore, all seven patients demonstrated an improvement in LV function as assessed by radionuclide angiography, with a mean absolute improvement in LV ejection fraction of 0.16 (range 0.09 to 0.34). These observations, while not definitive, imply that the associations observed in this study represent a true effect of lead position rather than confounding by other patient characteristics.
5 Conclusion
An anterior versus nonanterior LV pacing site, identified using standard PA and lateral chest radiographs, has prognostic importance. An anterior versus nonanterior lead position is independently associated with significantly worse clinical outcomes. This appears related to the lead position itself rather than other factors. Repositioning of the LV lead in patients with an anterior lead position and who have not clinically responded to CRT is feasible and would be anticipated to increase the likelihood of subsequent benefit from CRT.
References
Auricchio, A., Stellbrink, C., Sack, S., Block, M., Vogt, J., Bakker, P., et al. (2002). Long-term clinical effect of hemodynamically optimized cardiac resynchronization therapy in patients with heart failure and ventricular conduction delay. Journal of the American College of Cardiology, 39(12), 2026–2033.
Cazeau, S., Leclercq, C., Lavergne, T., Walker, S., Varma, C., Linde, C., et al. (2001). Effects of multisite biventricular pacing in patients with heart failure and intraventricular conduction delay. The New England Journal of Medicine, 344(12), 873–880.
Abraham, W. T., Fisher, W. G., Smith, A. L., Delurgio, B. D., Leon, A., Loh, E., et al. (2002). Multicenter InSync Randomized Clinical Evaluation. Cardiac resynchronization in chronic heart failure. The New England Journal of Medicine, 346(24), 1845–1853.
Young, J. B., Abraham, W. T., Smith, A. L., Leon, A. R., Lieberman, R., Wilkoff, B., et al. (2003). Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD trial. Journal of the American Medical Association, 289(20), 2685–2694.
Bristow, M. R., Saxon, L. A., Boehmer, J., Krueger, S., Kass, D. A., De Marco, T., et al. (2004). Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. The New England Journal of Medicine, 350(21), 2140–2150.
Cleland, J. G. F., Daubert, J. C., Erdmann, E., Freemantle, N., Gras, D., Kappenberger, L., et al. (2005). The effect of cardiac resynchronization on morbidity and mortality in heart failure. The New England Journal of Medicine, 352, 1539–1549.
Auricchio, A., Stellbrink, C., Butter, C., Sack, S., Vogt, J., Misier, A. R., et al. (2003). Clinical efficacy of cardiac resynchronization therapy using left ventricular pacing in heart failure patients stratified by severity of ventricular conduction delay. Journal of the American College of Cardiology, 42, 2109–2116.
Lozano, I., Bocchiardo, M., Achtelik, M., Gaita, F., Trappe, H. J., Daoud, E., et al. (2000). Impact of biventricular pacing on mortality in a randomized crossover study of patients with heart failure and ventricular arrhythmias. Pacing and Clinical Electrophysiology, 23(11 Pt 2), 1711–1712.
Arnold, J. M. O., Liu, P., Demers, C., Dorian, P., Giannetti, N., Haddad, H., et al. (2006). Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. The Canadian Journal of Cardiology, 22(1), 23–45.
Hunt, S. A., Abraham, W. T., Chin, M. H., Feldman, A. M., Francis, G. S., Ganiats, T. G., et al. (2005). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult. Circulation, 112(12), e154–e235.
Diaz-Infante, E., Mont, L., Leal, J., Garcia-Bolao, I., Fernandez-Lozano, I., Hernandez-Madrid, A., et al. (2005). Predictors of lack of response to resynchronization therapy. The American Journal of Cardiology, 95(12), 1436–1440.
Bleeker, G. B., Bax, J. J., Fung, J. W. -H., van der Wall, E. E., Zhang, Q., Schalij, M. J., et al. (2006). Clinical versus echocardiographic parameters to assess response to cardiac resynchronization therapy. The American Journal of Cardiology, 97(2), 260–263.
Ansalone, G., Giannantoni, P., Ricci, R., Trambaiolo, P., Fedele, F., & Santini, M. (2002). Doppler myocardial imaging to evaluate the effectiveness of pacing sites in patients receiving biventricular pacing. Journal of the American College of Cardiology, 39(3), 489–499.
Butter, C., Auricchio, A., Stellbrink, C., Fleck, E., Ding, J., Yu, Y., et al. (2001). Effect of resynchronization therapy stimulation site on the systolic function of heart failure patients. Circulation, 104(25), 3026–3029.
Verbeek, X. A., Vernooy, K., Peschar, M., Cornelussen, R. N., & Prinzen, F. W. (2003). Intra-ventricular resynchronization for optimal left ventricular function during pacing in experimental left bundle branch block. Journal of the American College of Cardiology, 42, 558–567.
Macias, A., Gavira, J. J., Alegria, E., Azcarate, P. M., Barba, J., & Garcia-Bolao, I. (2004). Effect of the left ventricular pacing site on echocardiographic parameters of ventricular dyssynchrony in patients receiving cardiac resynchronization therapy. Revista Espanola de Cardiologia, 57(2), 138–145.
Rossillo, A., Verma, A., Saad, E. B., Corrado, A., Gasparini, G., Marrouche, N. F., et al. (2004). Impact of coronary sinus lead position on biventricular pacing: mortality and echocardiographic evaluation during long-term follow-up. Journal of Cardiovascular Electrophysiology, 15(10), 1120–1125.
Nagele, H., Hashagen, S., Azizi, M., Behrens, S., & Castel, M. A. (2006). Long-term hemodynamic benefit of biventricular pacing depending on coronary sinus lead position. Herzschrittmachertherapie & Elektrophysiologie, 17(4), 185–190.
Hinkle Jr, L. E., & Thaler, H. T. (1982). Clinical classification of cardiac deaths. Circulation, 65(3), 457–464.
White, J. A., Yee, R., Yuan, X., Krahn, A., Skanes, A., Parker, M., et al. (2006). Delayed Enhancement magnetic resonance imaging predicts response to cardiac resynchronization therapy in patients with intraventricular dyssynchrony. Journal of the American College of Cardiology, 48(10), 1953–1960.
Bleeker, G. B., Kaandorp, T. A. M., Lamb, H. J., Boersma, E. P., Steendijk, P. P., de Roos, A. M. D. P., et al. (2006). Effect of posterolateral scar tissue on clinical and echocardiographic improvement after cardiac resynchronization therapy. Circulation, 113(7), 969–976.
Zhang, Y., Chan, A. K., Yu, C. M., Yip, G. W., Fung, J. W., Lam, W. W., et al. (2005). Strain rate imaging differentiates transmural from non-transmural myocardial infarction: a validation study using delayed-enhancement magnetic resonance imaging. Journal of the American College of Cardiology, 46(5), 864–871.
Becker, M., Kramann, R., Franke, A., Breithardt, O. A., Heussen, N., Knackstedt, C., et al. (2007). Impact of left ventricular lead position in cardiac resynchronization therapy on left ventricular remodelling. A circumferential strain analysis based on 2D echocardiography. European Heart Journal, 28(10), 1211–1220.
Alonso, C., Leclercq, C., Victor, F., Mansour, H., de Place, C., Pavin, D., et al. (1999). Electrocardiographic predictive factors of long-term clinical improvement with multisite biventricular pacing in advanced heart failure. The American Journal of Cardiology, 84(12), 1417–1421.
Auricchio, A., Fantoni, C., Regoli, F., Carbucicchio, C., Goette, A., Geller, C., et al. (2004). Characterization of left ventricular activation in patients with heart failure and left bundle-branch block. Circulation, 109(9), 1133–1139.
Arzola-Castaner, D., Taub, C., Heist, E. K., Fan, D., Haelewyn, K., Mela, T., et al. (2006). Left ventricular lead proximity to an akinetic segment and impact on outcome of cardiac resynchronization therapy. Journal of Cardiovascular Electrophysiology, 17(6), 623–627.
Murphy, S., Mulamalla, A., Popovic, S., et al. (2006). Tissue synchronization imaging and optimal left ventricular pacing site in cardiac resynchronization therapy. The American Journal of Cardiology, 97(11), 1615–1621.
Becker, M., Franke, A., Breithardt, O. A., Ocklenburg, C., Kaminski, T., Kramann, R., et al. (2007). Impact of left ventricular lead position on the efficacy of cardiac resynchronisation therapy: a two-dimensional strain echocardiography study. Heart (British Cardiac Society), 93(10), 1197–1203.
Dekker, A. L., Phelps, B., Dijkman, B., van Der Nagel, T., van Der Veen, F. H., Geskes, G. G., et al. (2004). Epicardial left ventricular lead placement for cardiac resynchronization therapy: optimal pace site selection with pressure–volume loops. The Journal of Thoracic and Cardiovascular Surgery, 127(6), 1641–1647.
Peschar, M., de Swart, H., Michels, K. J., Reneman, R. S., & Prinzen, F. W. (2003). Left ventricular septal and apex pacing for optimal pump function in canine hearts. Journal of the American College of Cardiology, 41(7), 1218–1226.
Helm, R. H., Byrne, M., Helm, P. A., Daya, S. K., Osman, N. F., Tunin, R., et al. (2007). Three-dimensional mapping of optimal left ventricular pacing site for cardiac resynchronization. Circulation, 115(8), 953–961.
Wilton, S. M., Sondergaard, R., Shah, S., Cowan, K., Semeniuk, L., & Exner, D. V. (2006). Location matters: LV lead position and outcome with CRT. Heart Rhythm, 3(5), s41.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Wilton is a Canadian Institutes of Health Research (CIHR) Strategic Training Fellow in Tomorrow’s Research Cardiovascular Health Professionals (TORCH). Dr. Exner is a CIHR Clinical Investigator and Scholar of the Alberta Heritage Foundation for Medical Research.
Dr. Exner has received research grants and consulting fees from Medtronic Inc., Boston Scientific and St. Jude Medical. Dr. Semeniuk is now employed by Johnson & Johnson.
Rights and permissions
About this article
Cite this article
Wilton, S.B., Shibata, M.A., Sondergaard, R. et al. Relationship between left ventricular lead position using a simple radiographic classification scheme and long-term outcome with resynchronization therapy. J Interv Card Electrophysiol 23, 219–227 (2008). https://doi.org/10.1007/s10840-008-9287-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-008-9287-1