Abstract
Labor market presence of cancer survivors has been significantly improved as medical technology revolutionized cancer-specific diagnoses and treatments. However, less understood are post-cancer variations in job market outcomes of racial and ethnic minorities in the US. Using a theoretical framework derived from family labor supply decision models and taking advantage of the rich data in the 2008–2014 Medical Expenditure Panel Survey (MEPS), this study employs a double-hurdle empirical model of labor force participation and hours worked to evaluate the employment decisions of Black and Hispanic cancer survivors. Hispanic and Black breast cancer survivors were less likely to be employed by 4% and 7.5%, respectively, when compared with Whites. Black prostate cancer survivors were 8% less likely to work than Whites, with nonsignificant differences between Hispanic and White prostate cancer survivors. Once employed, Black and Hispanic breast cancer survivors worked an extra 4 and 6 h than Whites, while Hispanic prostate cancer survivors worked 5 fewer weekly hours than Whites. In addition, our estimates indicate the significance of job types in labor market outcomes post-cancer. Employment of minorities in blue collar or service occupations decreased employment hours of survivors. Labor market disparities for minorities amplifies the socio-economic and familial burden of cancers. This timely work motivates informed public policy to reduce unexamined consequences of chronic conditions among minorities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction and Literature Review
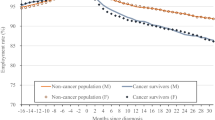
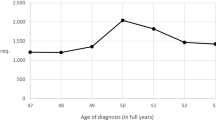
Breast and prostate cancers have been the most prevalent types of cancers for working age women and men in the US (Siegel et al. 2018). Between 1999 and 2013, the incidence rates for breast cancer increased, while the incidence rates for prostate cancer decreased (Melaku et al. 2018). How these cancers impacted socio-economic activities have differed by gender and ethnicity/race (Ward et al. 2004). Breast cancer in women, compared to prostate cancer in men, has been diagnosed at younger ages than other common types of cancers (Bradley et al. 2005) with a median age at diagnosis of 61 years (Miller et al. 2016). The average age for diagnoses of prostate cancer has been age 66 (Heinesen et al. 2018). Increasing retirement age has enhanced the likelihood of job market presence of cancer survivors (Bradley and Bednarek 2002). While some cancer survivors left the labor force post-diagnosis and treatment, others reduced their work hours. Bradley et al. (2005) reported that breast cancer survivors were 9% less likely to work after diagnosis and Bradley et al. (2007) described that prostate cancer survivors were 10% less likely to work than their non-cancer counterparts. Short et al. (2008) noted that the average reduction in work hours for cancer survivors of both genders has been 3 to 5 h. Race was also associated with the employment decisions of breast cancer survivors, with the negative effect of breast cancer on employment being twice as strong for Black women compared to White women (Bradley et al. 2007).
Central to the decision about remaining employed after experiencing breast or prostate cancer has been the ability to meet the needs of the family (Ashenfelter and Heckman 1974; Killingsworth and Heckman 1986). Not only has cancer as a chronic medical condition affected the physical and mental health of survivors, it also has increased the likelihood of financial hardships for survivors and their families as a result of catastrophic medical expenditures (Banegas et al. 2016). Employment decisions have varied between households where survivors live with spouses or other working adults, compared with households where the survivor is the only working adult in the household; family composition and alternative sources of household income were key factors influencing employment decisions and the resulting financial security of the household (Swanberg et al. 2017). The need to care for children and elderly residing in the household also has impacted employment decisions of persons with chronic health conditions (Artazcoz et al. 2004). Depending on the number of young children present in the home, higher child care cost have led to lower labor force participation (Connelly 1992).
What has been the connection between the experience of breast and prostate cancer and employment? Breast and prostate cancer have been associated with physical and mental disabilities that limit labor market attachments (Kiasuwa Mbengia et al. 2018). Arm morbidity, including movement limitations, swelling and lymph drainage were identified among 5-year breast cancer survivors (Engel et al. 2003). Breast cancer survivors also have experienced high levels of depressive and anxiety-related symptoms, as well as high levels of self-reported cognitive limitations (Hansen et al. 2008). Challenges with mental rotation and recall of spatial information have been reported for post-treatment prostate cancer survivors (Cherrier et al. 2010). Another challenge with post-treatment prostate cancer was urinary leakage (Grunfeld et al. 2013). After radical prostectomy, Dahl et al. (2016) reported that prostate cancer survivors with urinary leakage (about 30% of their sample) were twice as likely to report moderate or poor work ability. Clinically relevant fatigue (i.e., fatigue that is so severe that it interferes with function) has been reported as a significant post-treatment concern for prostate cancer survivors (Storey et al. 2012). Furthermore, it was documented that the type of jobs held post-cancer has mattered for the labor market outcomes of cancer survivors. Bradley et al. (2007), for instance, found that among breast cancer and prostate cancer patients whose jobs required heavy lifting, 62% of breast cancer patients and 30% of prostate cancer patients indicated that their cancer interfered with their ability to perform the task. Other challenges for breast and prostate cancer patients were jobs requiring that they keep pace with others, concentration, and stooping (Hansen et al. 2008). However, there has been sparse evidence on how female breast and male prostate cancers affect the labor market outcomes for racial and ethnic minorities in the US. Also, in contrast to the literature on employment outcomes for breast cancer patients, a very sparse literature investigated work patterns among prostate cancer survivors, especially in the United States (Grunfeld et al. 2013).
The current study explored the post-breast and prostate cancer labor market decisions of non-Hispanic Blacks and Hispanics by taking into consideration a standard labor supply model and using Medical Expenditure Panel Surveys (MEPS) data. Dealing with the problems of heterogeneity associated with cancer survivorship and the right skewedness of data, we implemented a double hurdle decision making econometric modelling technique to detect robust estimates of labor supply models of breast and prostate cancer survivors.
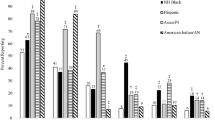
The key contributions of this work were threefold. First, we augmented the past literature that reports non-Hispanic Black were more likely than non-Hispanic White women to leave their jobs post-breast cancer. Bradley et al. (2007) indicated that African American women were twice as likely as White women to move from employment to unemployment but noted that the reason for this racial difference was unclear. We hypothesized that perhaps the difference in employment decisions of breast and prostate cancer survivors was due to racial differences in the types of jobs held. When chronic health conditions resulted in fatigue and physical weakness, those in physically demanding jobs were more likely to leave their jobs (Currie and Madrian 1999). Racial and ethnic minorities were more likely to work in physically demanding jobs (US Bureau of Labor Statistics 2015). Black and Hispanic men were more likely than White men to work in natural resources, construction, and material moving occupations. While 27% of Hispanic men were employed in natural resources, construction, and maintenance jobs, only 18% of White men and 12% of Black men held these types of jobs. Similar ethnic/racial diversity in occupations existed for women. White women were more likely than Black or Hispanic women to work in management or professional jobs (44% vs. 35% and 27%, respectively). Hispanic and Black women were more likely to work in service occupations, sales and office positions (62% and 57%, compared to 50%). Given this ethnic/racial stratification in occupations held, we asked whether the differential impact of race on breast cancer survivors’ employment decisions was primarily explained by racial differences in the types of jobs held, or other factors. Within this context, we revisited the work decisions of prostate cancer survivors. A second contribution of this study was to expand this work by also including Hispanics in our analysis sample. By performing our analysis using a sizable number of Hispanic respondents, we were able to contrast racial and ethnic differences in employment outcomes for breast and prostate cancer survivors.
Finally, this study employed a double hurdle regression specification to explore employment decisions of breast and prostate cancer survivors at the extensive and intensive margins by including individual, familial, and economic factors. In previous analysis exploring employment decisions of breast and prostate cancer survivors, conditional ordinary least square (OLS) methods have been used (Bradley et al. 2002, 2007). Given the nature of labor market data, with dependent variables including many zeros, a double hurdle model provided better estimates (Blundell and Meghir 1987). Besides addressing the dominance of zeros and right skewedness of the data, the double hurdle model considered the forward sloping and backward bending labor supply behavior of a cancer survivor in the estimates (Chiappori et al. 2002). Additionally, the double hurdle model recognized, in contrast to the traditional OLS perspective, that a value of zero for hours of labor market work may indicate that the person was unemployed and unable to find work, rather than not participating in the labor market (Blundell et al. 1989).
Theoretical Model
Previous studies of health shock consequences on labor market attachments have concentrated mostly on a framework of an individual’s health capital (Bradley et al. 2002; Halpern and Hausman 1986; Cain and Dooley 1976; Podor and Halliday 2012). Built upon pioneering work of Becker (1964) and Grossman’s (1972) classic formulation, an individual adopted his or her investment in behaviors that affect health based on the investment’s effects on discounted expected utility. Cancer, as an unpredicted health shock, was a negative investment in health and it affected labor market outcomes through different pathways. First, it may affect an individual’s work productivity as a result of changes in the stock of health capital. Decrement in health-related productivity has been demonstrated as either absenteeism or lower presenteeism (Koopman et al. 2002). Second, it altered the level of utility received from consumption of different goods and services. Given the difference between utility in healthy and sick states, if cancer increased this difference with consumption, we concluded that the marginal utility of consumption declined as health deteriorated, a situation called negative state dependence. On the other hand, if the difference in utility decreased with consumption, we concluded that marginal utility increased as health deteriorated and it was called positive state dependence (Finkelstein et al. 2013). Third, cancer impacted the availability of time for a survivor. For instance, a cancer survivor needed to spend more time on self-care or to see health care providers. This discussion suggested that changes in health due to cancer may have substantial consequences for the labor market behavior of a survivor. To formalize these ideas, we incorporated a family labor supply decision model (Ransom 1987). In this context, we assumed that a family (e.g., a single decision-making unit) with at least one cancer survivor maximized the following utility function:
subject to family budget constraintFootnote 1:
in Eqs. 1 and 2, \(\text{C}\) represented the family’s composite consumption good, \({\text{L}}_{\text{i}}\) was the leisure time of family member \(\text{i}\) (\(\text{i}=\text{maleorfemale})\), \(\text{P}\) was the price of consumption good, \(\text{I}\) was the non-wage income of the family, and wi and hi were the market hourly wage and weekly hours of work, respectively. Given strict equality, it was more convenient to re-write the family utility function in terms of hours of market work as follows:
For a cancer survivor, marginal utility of decreasing and increasing labor supply based on any combination of weekly hours of work was:
In the absence of any quantity constraints and usual circumstances, \({\text{m}}_{\text{i}}=0\), was a requirement for the first order condition of the utility maximization problem. This motivated estimation of reduced form labor supply models in the empirical analysis. However, if one of the spouses in the household quit work with an intention to achieve higher household utility, the strict equality of Eq. (4) does not hold for one of the spouses. As a result, it created two reduced form labor supply equations and the labor market decision was endogenously determined by the family constraints. Assuming that the working spouse was a cancer survivor in the household, the labor supply decision followed a standard labor supply model (Blundell et al. 1989). Conditional on employment, the survivor worked certain hours in the labor market, given the financial assets and observable factors and random noise \({{\upepsilon }}_{\text{i}}\). Then, the decided work hours for a utility maximizing cancer survivor assumed the function:
In Eq. 5, \({\upgamma }\) shows the vector of preference parameters and observables including racial/ethnic differences. Considering a specific distribution for the error term \({{\upepsilon }}_{\text{i}}\) and an explicit form for the hours of work \({\text{h}}_{\text{i}}\) yielded a normal linear equation of work hours indicated as:
Assuming \({{\upepsilon }}_{\text{i}}~\text{N} (0,{{\upsigma }}^{2})\), it was possible to estimate Eq. (6) by reduced form equations. However, it ignored the fact that some potential types of labor supply response were excluded. Specifically, the linear model ignored the occurrence of forward sloping and backward bending labor supply behavior of a cancer survivor (Blundell et al. 1989). Unlike restricted traditional limited dependent variable models, the empirical specification of this paper dealt with these limitations in the next section.
Methods
Data Source and Sample Selection
We utilized the 2008–2014 waves of the Medical Expenditure Panel Survey (MEPS). This rich survey has been administered by the Agency for Healthcare Research and Quality (AHRQ) since 1996. The survey included comprehensive information about American families and individuals which is linked to their medical providers (e.g., doctors, hospitals, pharmacies) as well as their employers. MEPS has collected a wide range of health-specific variables on health care utilization, cost, source of financing using household component (HC), and insurance component. The HC collected data from persons living within households and was linked to data from their medical providers. HC participants were randomly drawn from a nationally representative subsample of households that engaged in the previous year’s National Center for Health Statistics’ National Health Interview Survey. In short, MEPS provided detailed data for each person in the household on socioeconomic status, demographic characteristics, health condition and health care utilization, charges and source of payments.
Cancer status was self-reported in MEPS. The survey asked respondents whether a physician or other healthcare professional had ever told them that they had any type of cancer or a malignancy. We included all those responding “yes” to the above question and then specified that they have breast or prostate cancer. MEPS began collecting data on cancer in 2008. Therefore, we identify unique observations from 2008 to 2014 data. Figure 1 provided a detailed explanation of how we reached the final study sample.
Econometric Model
The choice of statistical method for modeling labor force participation and labor supply depended on the assumptions related to cancer survivors’ job market behavior and the data structure. MEPS data included the hours of work over the past week. Naturally, a linear regression model was restrictive in analyzing supply of labor given the dominance of zeros and a skewed data structure. While the Tobit model (1958) was an alternative, as it adjusts the zeros (Grogan and Sadanand 2013), it fails to appropriately deal with the zero observations. In the Tobit model, a zero value indicates a corner solution when solving a utility maximization problem of the agent. However, zero observations in the data generating process may have occurred for certain reasons beside a corner solution (Wooldridge 2005). When analyzing labor market attachments on both extensive and intensive margins, apparently, data generating processes (DGP) were the same in both margins. However, decisions to enter the job market and then allocate certain hours of work were not necessarily determined by the same factors. As a result of two different DGPs, an endogenity problem occurred if not properly dealt with (Salmon and Tanguy 2016). A two-stage modeling specification was substantial to solve the endogenous participation problem. Apparently, the Heckman (1977) correction model was appropriate in dealing with such circumstances, but its dependence on a strong assumption that none of the zero data points was generated by a corner solution was less favorable.
Integer values that arose from counting and non-negativity of hours worked made it tempting to rely on count data empirical models. The Poisson model (Cameron and Trivedi 1990) was the simplest count model to be considered, but its unrealistic assumption of equal conditional mean and variance restricted its application in most empirical studies. Generally speaking, the presence of overdispersion (the conditional variance greater than the conditional mean) has been a prominent characteristic of count data in economic studies. This characteristic of the data was associated with the heterogeneity and positivity in the datasets (McCullagh and Nelder 1989). Furthermore, another equally important peculiarity of labor market data was the dominance of zero especially in survey settings (Gurmu 1997; Gurmu and Trivedi 1996).
The econometric specification of this paper was based on a count data hurdle negative binomial model, to deal with possible unobserved heterogeneity as well as dominance of zeros in the data. It is well documented that the hurdle model specification was appropriate in estimating models with a presence of “excess zeros” in the data (Hellström 2002). This model was first developed by Portney and Mullahy (1986) and their work was inspired by ideas from Cragg (1971), who first thought about double hurdle models. With a versatile functional form, the hurdle model allowed estimation of both under- and over-dispersion. Also, it had an intuitively sound interpretation that mirrors a two-stage decision process. The first stage governed individuals who reported zero work hours, while the second part dealt with strictly positive work hours. Statistically, the equality of DGPs in the first and second stages, as well as their distributions could be tested. In the zero truncated negative hurdle models, the independence property was relaxed and instead a truncated distribution was applied in the second stage. For our study, this shows that if a survivor is assumed to be employed prior to cancer, the probability for that person to work as a cancer survivor in the market was associated with the past history of work hours before cancer. The hurdle decision model specified the first part as a binary outcome model and the second part as a zero-truncated model. To fix ideas, \({{\uppsi }}_{1}=\left({{\upgamma }}_{1}^{{\prime }}{{\upsigma }}_{2}^{{\prime }}\right)\) and \({{\uppsi }}_{2}=\left({{\upgamma }}_{1}^{{\prime }}{{\upgamma }}_{2}^{2}\right)\) indicated the parameters of stage 1 and 2, respectively. Then, the likelihood function for the hurdle specification was shown by:
The first product in Eq. (7) showed the probability of zero counts while the second product indicated the process once the first hurdle was passed and was estimated using the zero-truncated negative hurdle model. \({\text{S}}_{1},{\text{S}}_{2}\) illustrated the subsamples of cancer survivors unemployed and employed, respectively. The joint likelihood was maximized separately by the maximization of each hurdle, assuming the functional independence between each step of decision-making. Given that the first stage only included binary information on the dependent variable, the dispersion parameter and the constant term were not separately identifiable. Therefore, the constant term in the first stage was a non-linear combination of the true constant and the dispersion parameter as follows:
However, we explicitly estimated and tested the dispersion parameter in the second stage of the analysis. In a hurdle model, positive hours of work were associated with a two-stage process: (1) the cancer survivor had to decide to participate in the labor market, and (2) the cancer survivor had to allocate time to work. The determinants of the labor participation and number of hours worked decisions were not the same. First, if an individual was not participating in the labor market, any value of the independent variables was irrelevant due to abstentions. Second, the individual could be a potential job market participant, but may decide not to work for some economically justified reasons. In the second case we have a corner solution. Thus, we assumed that exogenous factors that affected the individual’s decision to participate were different from those determining the number of hours worked.
To model the labor force participation and hours of worked decisions, we empirically estimated Eq. (4) to provide robust estimates of hours worked by survivors who were in the labor market and seek employment opportunities. Note that our empirical model did not include a wage rate. This was because: (1) we could not explicitly distinguish between those who were not seeking jobs and those who were actively in the labor market seeking jobs, yet have not found them; both report zero hours of work, and (2) job seekers who reported zero hours of work do not have a wage rate. Since all potential workers had a reservation wage (i.e., the lowest wage that they would consider in order to accept a job option), we included a measure of the reservation wage instead of a measure of the market wage in our analysis. Our proxy measures of the reservation wage were work experience and non-wage income (Hofler and Murphy 1994). An increase in non-wage income was associated with an increase in the reservation wage, and thus should decrease entry into the labor market. Similarly, the greater work experience, the greater the reservation wage and the lower hours of work. Unlike a healthy person, a cancer survivor might place more value on leisure time and any increment in the wage rate may lead to a desire to purchase more leisure time and less work time. Consequently, this was an indication of backward bending labor supply behavior of utility maximizing persons, which cannot be captured by OLS regression models (Hanoch 1965).
Cancer Survivor’s Demographics Variables
Built upon the theoretical and econometric models of this analysis, this study included several dimensions of demographic, family, and health status variables besides the categorical variable of interest, race/ethnicity (non-Hispanic White, non-Hispanic Black and Hispanic), in the first and second stages of empirical modelling specification as independent controls. These included the cancer survivor’s age (18–64); educational attainment (no high school diploma, diploma, college and graduate); marital status (married, widowed/divorced/separated, and never married); geographic region (Northeast, Midwest, South and West); perceived health status (excellent/very good, good/fair, and poor); number of co-morbidities; and family size. The individual’s age, here associated with diminishing work ability and job tenure (Schneider et al. 2013), has been widely used in labor and health economics (Jeon 2017; Kirschenbaum and Weisberg 2002; Ng and Feldman 2009; Van Breukelen et al. 2004). The utility gains from being in the job market have increased due to accumulation of job-related human capital as the person’s age increased (Burdett 1978). Further, certain types of cancers have been directly associated with a person’s age (Miller et al. 2016). We included all age groups that were eligible for labor market attachment. Our sample excluded all retired and disabled cancer survivors on social security income.
A large body of evidence confirmed that educational attainment plays a key role in labor market attachment (Card 1999). We included educational attainment as a proxy for “movement human capital” as it may be associated with reduced cost of job searches and increased benefits of employment (Trevor 2001). In our analysis, the hypothesis was that well-educated cancer survivors have a higher likelihood of employment but diminishing utility of hours worked. Marital status of individuals has been correlated with job market decisions (Blundell and Meghir 1987). Compared to those who never married, a cancer surviving married woman might have financial support from a spouse who was eligible to work, adjust employment hours, or provide access to employment based health insurance, thus possibly leading her to choose not to work or to work less (Chen et al. 2016). Marital status was assumed to affect the cancer survivor’s job market participation as well as hours worked.
Culture, social norms, and lived experience vary by unchanged individual characteristics, such as geographical residence, and influence preferences for employment. Geographic differences capture the heterogeneous effects of multiple factors (Acs and Armington 2004) correlated with cancer occurrence. For example, unemployment rates have varied greatly across the US cities and regions (Kline and Moretti 2013). Additionally, costs of child care vary by region of residence and higher costs have been associated with a lower likelihood of labor force participation (Anderson and Levine 1999).These factors altogether were likely influences on a cancer survivor’s decision to participate in the job market and the number of hours worked.
Health status and work ability of an individual were widely discussed in the health economics literature (Cai and Kalb 2006; Lloyd and Auld 2002; Podor and Halliday 2012). Poor health status was likely to reduce work ability and hours of work through negative impacts on tastes for work and increases in the marginal value of leisure time (Grossman 1972). Our study incorporated a cancer survivor’s perceived health status in the three different categories discussed above, and also a continuous variable measure of the number of co-morbidities, including hypertension, diabetes, and heart diseases. Finally, family size was included as a crucial factor for determining job market entry and hours worked decisions (Cotton and Tuttle 1986). We assumed family size was associated with the number of dependents in the household and influenced the opportunity cost of unemployment and hours worked (Schneider et al. 2013).
Labor Market Related Variables
Besides the cancer survivor’s demographics, work related measures and economic variables were included as determinants of employment decisions. Job market participation and hours worked were sequential decisions in our econometric model specification. There was no clear-cut theoretical guidance on the choice of variables for inclusion in the first and second hurdles of the model (Pudney 1989). However, including the same array of factors in each decision stage made it difficult to identify the model parameters correctly and therefore an exclusion restriction was favorable. An essential assumption of the double-hurdle model was that the second hurdle equation was determined by both non-economic and economic factors determining the cancer survivor’s decisions (Jones 1992; Okunade et al. 2010; Yen et al. 1996). Type of occupation and actual work experience were only included in the second hurdle of the model because there has been a large body of theoretical and empirical evidence on the effects of these economic variables on an individual’s hours worked decision (Grossbard 2015; Mincer 1962; Strauss and Thomas 1998).
Intuitively, a cancer survivor with diminished marginal utility of work may prefer to work in less physically demanding jobs. To determine the impact of certain occupations on cancer survivors’ hours worked, we distinguished between blue collar and service jobs in this analysis. Investigating the labor/leisure behavior of an individual, considering family income as the unit of analysis, was theoretically consistent with standard labor supply in household decision-making models.
As income was assumed to be pooled over family members, increases in family income increased consumption, and might affect the employment decision in the market (Mincer 1962). Additionally, we considered that after experiencing breast cancer, the share of family income that went to cancer treatment and health maintenance increased, and fewer resources were available for other consumption goods. Thus, demand for leisure declined and demand for labor force participation increased.
To quantify this effect, we included three categories of family income (low income = 125% of poverty to less than 200%, middle income = 200% of poverty to less than 400%, and high income = above 400%) in the participation equation. Household income as a percentage of the federal poverty line indicated the socio-economic status of the household. Non-wage income was also included in the first stage because it came from private sources other than labor market wages and includes rent, interest payments, dividends, royalties and other private transfers such as child support payments and other intra-family transfers. This type of wage has been important in alleviating financial stress while an individual was out of a job. At the same time, it affected the labor force participation decision (Hoynes et al. 2016; Cai and Liu 2011). Non-wage income in some ways was an indicator of permanent income (assets) for cancer survivors. Employment-based health insurance was crucial in the labor market, especially for people with chronic health conditions (Gruber 2000). Health insurance has influenced both labor force participation and hours worked for a cancer survivor (Bradley et al. 2002). Within the context of family decision-making, spousal health insurance has protected the cancer survivor from catastrophic health expenses associated with long-term treatment and follow-up. Health insurance status (privately insured, publicly insured and uninsured) was included in both stages of this analysis.
Empirical Results
Descriptive Statistics
Table 1 provided descriptive statistics for both categorical and continuous variables, and the results of Chi square tests for categorical variables and t-tests for continuous variables. Most breast and prostate cancer survivors were employed, with non-Hispanic White women having the highest percentage of employment among breast cancer survivors (63.68%) and Hispanic men having the highest percentage of employment among prostate cancer survivors (69.7%). In contrast, non-Hispanic Black women reported the highest number of hours worked among breast cancer survivors (39.18) and Hispanic men reported the highest number of hours worked among prostate cancer survivors (27.09). Interesting to note was that breast cancer survivors were more likely to work full-time and prostate cancer survivors reported hours similar to part-time employment. Types of jobs held among breast cancer survivors varied by race and ethnicity. Non-Hispanic White women were significantly more likely than non-Hispanic Black or Hispanic women to work in professional jobs. Non-Hispanic Black women were more likely to work in service jobs than non-Hispanic White or Hispanic women. Hispanic women were more likely to work in blue collar jobs than non-Hispanic White or Black women. The same racial/ethnic pattern of employment across job sectors existed for prostate cancer survivors, with non-Hispanic White men more likely to work in professional jobs, non-Hispanic Black men more likely to work in service jobs, and Hispanic men more likely to work in blue-collar jobs. Work experience was highest among non-Hispanic Black women, compared to other female breast cancer survivors, and non-Hispanic Black men, compared to other prostate cancer survivors.
There were racial/ethnic differences in other characteristics of breast and prostate cancer survivors. Non-wage income was significantly lower for non-Hispanic Black and Hispanic women, compared to non-Hispanic White women. Similarly, non-wage income was significantly lower for non-Hispanic Black and Hispanic prostate cancer survivors, compared to non-Hispanic Whites; indeed, non-wage income for non-Hispanic White men was almost four times that for Hispanic men. Southern residents were more likely to be non-Hispanic Black, while Northeastern and Western residents were more likely to be Hispanic. Education varied by race/ethnicity; Hispanics were least likely to have completed high school and non-Hispanic Whites were most likely to hold graduate degrees. Over 60% of non-Hispanic White breast and prostate cancer survivors and Hispanic prostate cancer survivors were married. Non-Hispanic Blacks were more likely than other ethnic/racial groups to be widowed/separated/divorced. Non-Hispanic Black breast cancer survivors and Hispanic prostate cancer survivors were most likely to be never married. Hispanic breast cancer survivors have larger families (2.83 persons, compared with 2.34 and 2.27 persons in non-Hispanic White and Black families). Hispanic prostate cancer survivors had larger families (3.09 persons, compared with 2.25 and 2.30 persons in non-Hispanic White and Black families). Health and health insurance coverage also vary by race/ethnicity. Non-Hispanic White breast and prostate cancer survivors were more likely to report excellent/very good health. Non-Hispanic White breast and prostate cancer survivors also were more likely to have private health insurance coverage.
Double Hurdle Model Results
Table 2 presented the results of first- and second-hurdles of the models for breast cancer and prostate cancer, separately. The first stage exclusively included family income status and non-wage income and the second stage model exclusively included work experience and types of jobs held. All estimations were performed by maximum likelihood with bootstrapped robust standard errors, and thus estimates were interpreted within the pseudo-maximum likelihood method. We performed Wald and Hausman tests to confirm the robustness of the negative binomial specification over the Poisson model. The over-dispersion in the data was modeled with a mean dispersion method. Alpha and log-alpha were dispersion parameters of the zero-truncated negative binomial model. The likelihood-ratio Chi square test of the dispersion parameter was highly significant at 0.00, and implies that the data were over-dispersed. The high value and significance of \({\tilde {\chi }^2}\) was an indication that two separate data generating processes produce employment and weekly hours worked.
Furthermore, to confirm the contribution of excess zeros and unobserved heterogeneity in the modelling of labor market decisions, we relied on the Vuong (1989) test. This statistical test compares single count models (Poisson and Poisson zero-inflated) with zero altered models. A significant test result implies excess zeros and unobserved heterogeneity are the contributing sources for overdispersion. Therefore, zero-altered models are preferred. As a final step in model comparison and selection, we compared the values of the Bayesian Information Criterion (BIC) and the Akaika Information Criterion (AIC) among zero-altered models. We obtained the lowest value of AIC and BIC in the Zero-truncated negative hurdle models.
The results in Table 2 indicated that race and ethnicity influenced the employment and weekly hours worked decisions of both female breast cancer survivors and prostate cancer survivors. Non-Hispanic Black and Hispanic breast cancer survivors were significantly less likely to work than non-Hispanic White breast cancer survivors. However, if survivors were working, non-Hispanic Black and Hispanic women worked more hours than non-Hispanic White women. This race/ethnicity effect on employment existed even though we account for differences in types of jobs held. As predicted, employment in service jobs decreased weekly hours worked. Other factors that influenced the decision to work among breast cancer survivors were: region of residence, marital status, education, health status, health insurance, and income. Breast cancer survivors were more likely to work if they lived in the Midwest, were not married, held graduate degrees, were not in poor health, did not have public health insurance, had middle or high family income, and had greater non-wage income.
In comparison to private health insurance holders, breast and prostate cancer survivors who were covered by public insurance were less likely to be attached to the job market. This might be due to the fact that income eligibility for certain types of health insurance coverage (e.g., Medicaid) might have discouraged job market activities and therefore public coverage reduced the incentive to work (Baicker et al. 2014). On the other hand, uninsured breast and prostate cancer survivors were not significantly different from those with private health insurance in regard to remaining in the labor market. Uninsured, employed breast cancer survivors worked more hours in the labor market than those otherwise insured. Lacking health insurance increased the price of health care, an essential purchase item for all family members. Extra work hours may thus be needed in order to cover out-of-pocket health care charges.
Hours of work among breast cancer survivors were higher for those who lived in the South and lower for those who lived in the West. Work hours were higher for widowed/separated/divorced breast cancer survivors who held graduate degrees, had health that was not poor, and were uninsured. Similar to decisions regarding employment, breast cancer survivors’ weekly hours of work were negatively associated with having public insurance. However, conditional on employment, uninsured breast cancer survivors indicated more weekly hours of work. Increased out-of-pocket health expenditures in the absence of any risk pooling mechanism might have caused an obligation to increase hours of work.
Work hours were lower for breast cancer survivors who had more work experience. Non-Hispanic Black prostate cancer survivors were less likely to work than non-Hispanic White survivors. Employed Hispanic prostate cancer survivors worked fewer hours than non-Hispanic White prostate cancer survivors. This race/ethnicity effect on employment existed even though we accounted for differences in types of jobs held. As predicted, employment in professional jobs was associated with greater weekly hours worked. Other factors that influenced the decision to work among prostate cancer survivors were: education, health status, health insurance, and income. Prostate cancer survivors were more likely to work if they held a baccalaureate degree, were not in poor health, were not publicly insured, and had middle or high income. Hours of work among prostate cancer survivors were higher for those who lived in the Midwest, were widowed/separate/divorced, and had health that was not poor.
Race/Ethnicity and Employment Decisions of Breast and Prostate Cancer Survivors
Why were race and ethnicity significant in influencing employment decisions of breast and prostate cancer survivors, even after we controlled for the influence of personal, family, and job characteristics? Let us explore the race/ethnicity effect further. Table 3 reports the employment rates of non-Hispanic White, non-Hispanic Black, and Hispanic breast cancer survivors and prostate cancer survivors (Columns 1–3 and 6–8), based on the raw descriptive data reported in Table 1. In Columns 4 and 5 and 9 and 10, racial and ethnic differences in employment were reported. Among breast cancer survivors, non-Hispanic Black women worked 8.7 percentage points less than non-Hispanic White women, and Hispanic women worked 13 percentage points less. Among prostate cancer survivors, non-Hispanic Black men worked 7.5 percentage points less than non-Hispanic White men, and Hispanic men work 11.4 percentage points more. The regression results reported in Table 2, indicate the adjusted differences in the percentage employment by race/ethnicity after controlling for age, age-squared, education, marital status, census region, perceived health status, health insurance coverage, family income, family size, and non-wage income.
A substantial portion of the racial/ethnic difference in the employment decision of breast cancer survivors was due to racial/ethnic differences in characteristics. But after adjusting for characteristics, a substantial disparity in the likelihood of employment continued to exist. The unadjusted employment gap declined from 8.7 percentage points to 4 for non-Hispanic Black breast cancer survivors, and the 13-percentage point gap of Hispanic women declined to 7.5. For non-Hispanic Black prostate cancer survivors, the 7.5 percentage point gap in employment grew to an 8.7 percentage point gap, after adjusting for characteristics. A nonsignificant coefficient for Hispanics in the employment status regression suggested that the greater labor force participation of Hispanics compared to non-Hispanic Whites (11-point difference) was explained solely by differences in characteristics. What explains the remaining racial/ethnic gap in labor force participation of Hispanic and non-Hispanic Black women breast cancer survivors and non-Hispanic Black prostate cancer survivors?
The lower portion of Table 3 explores unadjusted and adjusted weekly hours worked for breast cancer and prostate cancer survivors. For breast cancer survivors, non-Hispanic Black women worked 3.43 more hours per week than non-Hispanic White women, and Hispanic women worked 2.63 fewer hours. However, after adjusting for differences in characteristics, race accounted for more hours worked by non-Hispanic Black and Hispanic women than the unadjusted hours. Why did race and ethnicity lead non-Hispanic Black and Hispanic breast cancer survivors to work more hours than non-Hispanic White breast cancer survivors?
There were also disparities in the decisions regarding hours worked for non-Hispanic Black and Hispanic prostate cancer survivors. The results indicated that after adjusting for job type and other characteristics, the hours gap is fully explained for non-Hispanic Black men prostate cancer survivors (since the coefficient was not statistically significant) and the adjusted hours gap for Hispanics changed from an advantage of 1.78 h to a disadvantage of 5.2 h. Quite surprisingly, Hispanic breast cancer survivors and prostate cancer survivors, adjusting for differences in characteristics reversed the sign of the disparity with non-Hispanic White respondents.
Interactive Effects of Race/Ethnicity on Hours Worked by Type of Job Held
To provide further insights regarding the roles of race/ethnicity in influencing weekly hours worked, Table 4 examines interactive effects of race/ethnicity and job type. It presents the second stage of the hurdle model, adding interaction variables. The previously significant race/ethnicity variables for breast cancer survivors were no longer significant. The interaction terms were significant. The data indicated that holding a professional job (rather than a blue collar or service job) increased weekly hours worked. However, if a breast cancer survivor was non-Hispanic Black or Hispanic and working in a professional job, their work hours were lower than those of a non-Hispanic White breast cancer survivor who worked in a professional job. The professional work hours reduction was largest for non-Hispanic Blacks. For prostate cancer survivors, the significant race/ethnicity effect was now significant for both non-Hispanic Blacks and Hispanics, who worked fewer hours than non-Hispanic Whites. The occupation type variable (professional) was also significant, with those who worked in professional jobs working more hours than those employed in blue collar or service jobs. Only one interaction term was significant. It suggested that non-Hispanic Blacks who were in service jobs work more hours than non-Hispanic Blacks in blue collar jobs or non-Hispanic Whites in service jobs.
Discussion and Conclusions
Utilizing the Medical Expenditure Panel Survey data for 2008–2014 and applying a double hurdle regression technique, we explored the roles of race/ethnicity in influencing the labor market decisions of breast and prostate cancer survivors. Similar to previous work by Bradley et al. (2005a) we found that non-Hispanic Black women breast cancer survivors were less likely to work than were non-Hispanic White women breast cancer survivors. While Bradley et al. (2005b) reported no differences by race in the employment decisions of prostate cancer survivors, we found that non-Hispanic Black prostate cancer survivors were less likely to work than non-Hispanic White prostate cancer survivors.
Our work also fills the literature gap on job market outcomes of Hispanic survivors. Hispanic cancer survivors represent a rapidly growing population in the country. They are widely present in the labor market (Campesino et al. 2009). According to the Bureau of Labor Statistics, Hispanics comprise approximately 16.8% of the total labor force in the US. However, the current economics literature is mute about the employment prospects of Hispanic cancer survivors. Unlike our study, past literature did not provide any suggestive significant effect of cancers on the employment outcomes of Hispanic survivors (Bradley et al. 2005b). Another distinguishing feature of the current study from previous work is the analysis of occupation type and the labor market decisions of Hispanic survivors.
We note that there are unique racial and ethnic differences in the labor market decisions of non-Hispanic Black, Hispanic, and non-Hispanic White breast and prostate cancer survivors. Non-Hispanic Black and Hispanic breast cancer survivors make similar decisions on whether to work and the number of hours; both are less likely to work and if employed, work more hours when compared with non-Hispanic White survivors. Similarly, non-Hispanic Black and Hispanic breast cancer survivors who work in professional jobs work fewer hours than their non-Hispanic White counterparts who hold professional jobs. More dissimilarity exists among non-Hispanic Black and Hispanic prostate cancer survivors. Hispanic prostate cancer survivors are not dissimilar from non-Hispanic White survivors in their decision to work, with both more likely to work than non-Hispanic Black prostate cancer survivors. Given employment, both non-Hispanic Black and Hispanic prostate cancer survivors work fewer hours than non-Hispanic White survivors. However, Hispanic and non-Hispanic White prostate cancer survivors who are employed in service jobs work fewer hours than non-Hispanic Black survivors. These contrasts and similarities illustrate the importance of reporting and analyzing data by both race and ethnicity in order to better understand unique decision patterns.
These reported racial/ethnic differences reflect regression-adjusted differences in labor market participation, i.e., the role of race/ethnicity after adjusting for racial/ethnic differences in characteristics. Thus, we learn that some, but not all, of the reason for the observed differences in labor market participation of non-Hispanic Black and Hispanic breast and prostate cancer survivors is because of the lower likelihood that non-Hispanic Black and Hispanic breast cancer survivors hold graduate degrees, and their greater likelihood of reporting poor health and low income. Part of the reason that non-Hispanic Black prostate cancer survivors are less likely to participate in the labor market is their greater likelihood of not having a high school diploma, greater likelihood of having poor health, as well as greater likelihood of public health insurance coverage and low income.
What explains the remaining racial/ethnic gap in labor force participation of Hispanic and non-Hispanic Black women breast cancer survivors and non-Hispanic Black prostate cancer survivors? We know that workers with disabilities experience discrimination and implicit bias in the workplace, particularly those with mental disabilities (Acemoglu and Angrist 2001; Baldwin and Johnson 2000). What is unclear is whether employers respond differently to White cancer survivors compared to Black and Hispanic cancer survivors when they return to work with disabilities. Thus we ask: Are the unexplained racial/ethnic gaps in labor force participation due to racial/ethnic differences in actual or perceived discrimination (Darity 1998) or implicit bias when women present to work after experiencing a major health event that is associated with a long term treatment process, and a non-zero probability of reoccurrence within a 5 year time period?
Alternatively, the unexplained race/ethnicity gap may capture racial and ethnic differences in the response to and treatment of breast and prostate cancer. Non-Hispanic Black women tend to present for breast cancer treatment at later disease stages. In addition to the role of lacking health insurance on causing treatment delays, racial/ethnic differences in patient trust, belief that providers will take their health care concerns seriously, fear, confidence in their concern to get needed information from providers, and concerns about potential impact on family and significant others have all been identified as associated with delays (White-Means et al. 2015). Thus, resulting from delays, treatment and recovery from it differs by race, with more extreme outcomes, including higher mortality, experienced by non-Hispanic Black women (Ashing-Giwa et al. 2004). Although mortality rates for Hispanic women are not as high as those for non-Hispanic White women, Hispanic women also are less likely to receive timely treatment (Freedman et al. 2011). Early detection may involve less invasive, painful and debilitating treatment and lead to fewer limitations in activities or less severe disability (Ashing-Giwa et al. 2010).
Perhaps race and ethnicity are capturing racial/ethnic differences in the impact of breast cancer on physical abilities post treatment. With greater morbidity post-treatment, non-Hispanic Black and Hispanic women have lower labor force participation (Bound et al. 1996). Non-Hispanic Black men have been found to receive different treatment for prostate cancer than non-Hispanic White men (Moses et al. 2010); non-Hispanic Black men are more likely to receive androgen deprivation therapy (ADT) and less likely to receive surgery. ADT is associated with osteoporosis, fatigue, impotence and lower quality of life (Holzbeierlein et al. 2004). Perhaps racial/ethnic differences in the morbidity impacts of prostate cancer treatment are associated with non-Hispanic Black men having lower labor force participation. Availability, affordability and continuity of health care services are important correlates of employment and return to work for cancer survivors (Mehnert 2011).
A next step in analysis of the race/ethnicity gap in labor force participation among cancer survivors would be an assessment that distinguishes how much of the racial/ethnic gap in labor force participation of breast and prostate cancer survivors is associated with racial/ethnic differences in survivors’ experiences of discrimination and implicit bias in the workplace and how much is due to racial/ethnic differences in disability status resulting from late stage treatment. The second stage of the double hurdle model indicated that non-Hispanic Black and Hispanic breast cancer survivors work 4.3 and 6 h more than non-Hispanic White breast cancer survivors. In contrast, Hispanic prostate cancer survivors work 5 fewer hours per week than non-Hispanic White prostate cancer survivors. However, when we introduced race/ethnicity and job type interaction terms, the race/ethnicity variable was not statistically significant in the weekly hours regression for breast cancer survivors. In contrast, for prostate cancer survivors, the race/ethnicity interaction term and the race/ethnicity variable were statistically significant, with the race/ethnicity coefficient indicating reduced hours of work for both non-Hispanic Black and Hispanic prostate cancer survivors compared with non-Hispanic White prostate cancer survivors.
Our work confirms that job type, specifically holding a professional job, decreases the likelihood of reduced weekly hours of work. An interesting and unexplained result is that among breast cancer survivors who work in professional jobs, non-Hispanic Black and Hispanic survivors work fewer hours than non-Hispanic White survivors. These findings confirm our hypothesis that racial/ethnic differences in job type explain differences in weekly work hours of breast cancer survivors. In addition, our results suggest that there is a race/ethnicity effect within job type (professional workers) that also accounts for lower hours of work among non-Hispanic Black and Hispanic survivors.
For prostate cancer survivors, our results confirm our hypothesis that racial/ethnic differences in job type explain differences in weekly work hours of prostate cancer survivors. And within the category of service workers non-Hispanic Black prostate cancer survivors work more hours. However, there remains an unexplained racial and ethnic difference in weekly hours worked for prostate cancer survivors, with non-Hispanic White men working more hours weekly. What does this racial/ethnic effect measure? Understanding how differences in cultural perceptions of masculinity influence workplace decisions may provide clues about this unexplained racial/ethnic effect (Pedersen et al. 2012).
The current study provides important insights about the possible effects of cancer diagnosis on post-diagnosis and treatment labor force participation and supply of labor, using a novel econometric specification. Nonetheless, there are additional considerations for future research. First, while a rich source of longitudinal health care data, the dataset utilized in this study does not incorporate measures of the duration of cancer survivorship, stage at which it was diagnosed, and treatment dose and intensity. Such data would provide further insight on racial/ethnic differences in disability and its impact on labor market outcomes of prostate and breast cancer survivors. Second, the dataset lacks pre-cancer labor market information. Ideally, research insights would benefit from access to longitudinal data that allowed assessment of labor market work status change as cancer status changed. Currently, we assess labor market status, given a known diagnosis of breast or prostate cancer. Thus, we note for the reader that our analysis provides robust estimates of labor market states post-cancer, i.e., the decision of survivors to work or not work post-cancer. Finally, while MEPS provides a wealth of national data on health and medical care utilization, data on workplace experiences are more limited. Having such data would enable future researchers to assess the roles of disability-related discrimination and implicit bias on labor market outcomes.
This study has important research, practice, and policy implications. To our knowledge, this work is one of the first to investigate the labor market consequences of cancer survivorship for racial and ethnic minorities in the US. We augment the past literature that found Black and White differentials in labor market outcomes by analyzing the types of jobs held. Moreover, our estimates provide evidence on the job market attachments of Hispanic breast and prostate cancer survivors.
From a practice point of view, our findings motivate potential employers and employees to understand the labor market consequences of cancers among racial and ethnic minorities that require long-term treatment and adjustment of labor market schedules. Similarly, understanding the association between types of jobs held and cancer survivorship, not only helps employers but it informs survivors of the need to restructure their work regime and type of work performed. Furthermore, awareness about the labor market burden of leading types of cancers among racial and ethnic minorities encourages families and professional support groups to provide necessary assistance for unemployed male and female survivors who may have challenges in transitioning from the labor market.
From a policy perspective, this study provides further insight for effective implementation of the Americans with Disabilities Act (ACA). Promoting the adoption of flexible work schedules, paid time-off from work, and provision of equal employment opportunities for all racial and ethnic cancer survivors might reduce the familial, social, and economic burden associated with cancers (Osmani and Okunade 2018). Increased labor market flexibility not only enhances the likelihood of labor market presence, but it also increases labor productivity (Gehrke and Weber 2018). However, the value-added distribution of job flexibility could be heterogeneous among different types of jobs and genders (Golden 2008). Therefore, any public policy reform needs to be carefully formulated to target flexible work schedules toward workers with families or those in desperate need of such opportunities. Past studies have indicated the positive effect of family-friendly workplace policies that do not harm a firm’s profitability (Berg et al. 2004; Schmidt and Duenas 2002).
Health related complications of cancer such as functional limitations, pain, muscle weakness, and mental rotation, particularly in work settings, require specific medical interventions. For instance, availability of multiple treatment options with the lowest side-effect could reduce some of these work-related limitations. Offering occupational, physical and mental therapy could minimize work-impeding side-effects of cancer and its treatment. Individualized consultations and tailored treatment strategies have been found effective in lowering cancer related fatigue. Short- and long-term interventions are only justifiable if they have a significant effect on workplace and economic productivity and on the quality of life of the cancer survivor (Steiner et al. 2004).
Our analysis indicates that part of the racial/ethnic difference in employment decisions of survivors was due to racial/ethnic differences in characteristics, including education, family size, perceived health status, marital status, and health insurance coverage. Table 1 reports these differences in characteristics for both breast and prostate cancer survivors. Multiple factors could account for racial/ethnic differences in characteristics. These include disparities in economic opportunities (e.g., labor market attachment), lower educational attainment, lifestyle, physical surroundings, social norms, social networks, and community social capital. An extensive body of literature has found that racial and ethnic barriers could potentially affect socioeconomic status, including health and income of minority populations in the United States (Bertrand and Mullainathan 2004; Welch 1967). For instance, variation in income by persons with equivalent education is evidence that workers with comparable abilities do not fare similarly (Bayer and Charles 2018). We also know that ethnicity and race influence the type of job sector in which workers are employed, and thus impacts the likelihood of working for an employer who offers health insurance coverage (White-Means and Hersch 2005). Residential built environments also are associated with differences in self-perceived health. Hazardous polluted and crime infested neighborhoods limit choices and resources available in communities, including access to nutritious food, safe places for walking and medical facilities (Cubbin et al. 2008). Thus, where racial and ethnic groups live impacts their health, education, health care, and health options. An inclusive set of public policies that could provide multi-dimensional and multi-level interventions such as culturally tailored approaches, neighborhood, institution and system-based reforms, instead of simple interventions that address disparities by modifying within workplace barriers only, will also address disparities in employment outcomes for survivors.
Cancer survivors’ labor market responses based on the type of health insurance held provide strong evidence on the substantial role of health insurance in reducing excessive labor force efforts that could be damaging to recovery from breast cancer and mitigating health disparities among labor market employees. This is because being uninsured resulted in greater hours of work among employed breast cancer survivors. Thus, an interesting public policy question is: How do breast cancer survivors’ labor market participation and hours worked in countries that provide universal health insurance coverage compare to patterns observed in the United States?
Our analysis would predict significantly lower labor market work hours among cancer survivors covered by universal health insurance compared to a comparable uninsured population in the United States.
Notes
In this circumstance, the decisions are made based on intrahousehold agreements that could include two or more individuals (e.g., the patient and their spouse, extended family member, and/or informal caregiver). As a result of basic collective decision-making, this process generates Pareto-efficient outcomes for the family (Chiappori 1997) .
References
Acemoglu, D., & Angrist, J. D. (2001). Consequences of employment protection? The case of the Americans with Disabilities Act. Journal of Political Economy, 109(5), 915–957. https://doi.org/10.1086/322836.
Acs, Z. J., & Armington, C. (2004). The impact of geographic differences in human capital on service firm formation rates. Journal of Urban Economics, 56(2), 244–278. https://doi.org/10.1016/j.jue.2004.03.008.
Anderson, P. M., & Levine, P. B. (1999). Child care and mothers’ employment decisions. New York: National Bureau of Economic Research. https://doi.org/10.3386/w7058.
Artazcoz, L. a., Borrell, C., Benach, J., Cortès, I., & Rohlfs, I. (2004). Women, family demands and health: the importance of employment status and socio-economic position. Social Science and Medicine, 59(2), 263–274. https://doi.org/10.1016/j.socscimed.2003.10.029.
Ashenfelter, O., & Heckman, J. (1974). The estimation of income and substitution effects in a model of family labor supply. Econometrica: Journal of the Econometric Society, 42, 73–85. https://doi.org/10.2307/1913686.
Ashing-Giwa, K. T., Gonzalez, P., Lim, J. W., Chung, C., Paz, B., Somlo, G., et al. (2010). Diagnostic and therapeutic delays among a multiethnic sample of breast and cervical cancer survivors. Cancer, 116(13), 3195–3204. https://doi.org/10.1002/cncr.25060.
Ashing-Giwa, K. T., Padilla, G., Tejero, J., Kraemer, J., Wright, K., Coscarelli, A., et al. (2004). Understanding the breast cancer experience of women: A qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology, 13(6), 408–428. https://doi.org/10.1002/pon.750.
Baicker, K., Finkelstein, A., Song, J., & Taubman, S. (2014). The impact of Medicaid on labor market activity and program participation: Evidence from the Oregon Health Insurance Experiment. American Economic Review, 104(5), 322–328. https://doi.org/10.1257/aer.104.5.322.
Baldwin, M. L., & Johnson, W. G. (2000). Labor market discrimination against men with disabilities in the year of the ADA. Southern Economic Journal, 66, 548–566, https://doi.org/10.2307/1061425.
Banegas, M. P., Guy, G. P. Jr., de Moor, J. S., Ekwueme, D. U., Virgo, K. S., Kent, E. E., et al. (2016). For working-age cancer survivors, medical debt and bankruptcy create financial hardships. Health Affairs, 35(1), 54–61. https://doi.org/10.1377/hlthaff.2015.0830.
Bayer, P., & Charles, K. K. (2018). Divergent paths: A new perspective on earnings differences between Black and White men since 1940. The Quarterly Journal of Economics, 133(3), 1459–1501. https://doi.org/10.1093/qje/qjy003.
Becker, G. S. (1964). Human capital: A theoretical and empirical analysis, with special reference to education. New York: National Bureau of Economic Research. https://doi.org/10.2307/2229541.
Berg, P., Appelbaum, E., Bailey, T., & Kalleberg, A. L. (2004). Contesting time: International comparisons of employee control of working time. ILR Review, 57(3), 331–349. https://doi.org/10.1177/001979390405700301.
Bertrand, M., & Mullainathan, S. (2004). Are Emily and Greg more employable than Lakisha and Jamal? A field experiment on labor market discrimination. American Economic Review, 94(4), 991–1013. https://doi.org/10.1257/0002828042002561.
Blundell, R., Ham, J., & Meghir, C. (1989). Unemployment and female labour supply. In Unemployment in Europe (pp. 9–36). http://www.jstor.org/stable/3038229.
Blundell, R., & Meghir, C. (1987). Bivariate alternatives to the Tobit model. Journal of Econometrics, 34(1–2), 179–200.
Bound, J., Schoenbaum, M., & Waidmann, T. (1996). Race differences in labor force attachment and disability status. Gerontologist, 36(3), 311–321. https://doi.org/10.1093/geront/36.3.311.
Bradley, C. J., & Bednarek, H. L. (2002). Employment patterns of long-term cancer survivors. Psycho-Oncology, 11(3), 188–198. https://doi.org/10.1002/pon.544.
Bradley, C. J., Bednarek, H. L., & Neumark, D. (2002). Breast cancer survival, work, and earnings. Journal of Health Economics, 21(5), 757–779. https://doi.org/10.1016/S0167-6296(02)00059-0.
Bradley, C. J., Given, C. W., & Roberts, C. (2002). Race, socioeconomic status, and breast cancer treatment and survival. Journal of the National Cancer Institute, 94(7), 490–496. https://doi.org/10.1093/jnci/94.7.490.
Bradley, C. J., Neumark, D., Bednarek, H. L., & Schenk, M. (2005a). Short-term effects of breast cancer on labor market attachment: Results from a longitudinal study. Journal of Health Economics, 24(1), 137–160. https://doi.org/10.1016/j.jhealeco.2004.07.003.
Bradley, C. J., Neumark, D., Luo, Z., Bednarek, H., & Schenk, M. (2005b). Employment outcomes of men treated for prostate cancer. Journal of the National Cancer Institute, 97(13), 958–965. https://doi.org/10.1093/jnci/dji171.
Bradley, C. J., Neumark, D., Luo, Z., & Schenk, M. (2007). Employment and cancer: Findings from a longitudinal study of breast and prostate cancer survivors. Cancer Investigation, 25(1), 47–54. https://doi.org/10.1080/07357900601130664.
Burdett, K. (1978). A theory of employee job search and quit rates. The American Economic Review, 68(1), 212–220. http://www.jstor.org/stable/180970.
Cai, L., & Kalb, G. (2006). Health status and labour force participation: Evidence from Australia. Health Economics, 15(3), 241–261. https://doi.org/10.1002/hec.1053.
Cai, L., & Liu, A. Y. (2011). Public–private sector wage gap in Australia: Variation along the distribution. British Journal of Industrial Relations, 49(2), 362–390. https://doi.org/10.1111/j.1467-8543.2009.00773.x.
Cain, G. G., & Dooley, M. D. (1976). Estimation of a model of labor supply, fertility, and wages of married women. Journal of Political Economy, 84(4), S179–S199. https://doi.org/10.1086/260538.
Cameron, A. C., & Trivedi, P. K. (1990). Regression-based tests for overdispersion in the Poisson model. Journal of Econometrics, 46(3), 347–364. https://doi.org/10.1016/0304-4076(90)90014-K.
Campesino, M., Ruiz, E., Glover, J. U., & Koithan, M. (2009). Counternarratives of Mexican-origin women with breast cancer. Advances in Nursing Science, 32(2), E57. https://doi.org/10.1097/ANS.0b013e3181a3b47c.
Card, D. (1999). The causal effect of education on earnings. Handbook of Labor Economics, 3, 1801–1863. https://doi.org/10.1016/S1573-4463(99)03011-4.
Chen, W., Zheng, R., Baade, P. D., Zhang, S., Zeng, H., Bray, F., et al. (2016). Cancer statistics in China, 2015. CA: A Cancer Journal for Clinicians, 66(2), 115–132. https://doi.org/10.3322/caac.21338.
Cherrier, M. M., Borghesani, P. R., Shelton, A. L., & Higano, C. S. (2010). Changes in neuronal activation patterns in response to androgen deprivation therapy: A pilot study. BMC Cancer, 10(1), 1. https://doi.org/10.1186/1471-2407-10-1.
Chiappori, P.-A. (1997). Introducing household production in collective models of labor supply. Journal of Political Economy, 105(1), 191–209. https://doi.org/10.1086/262071.
Chiappori, P.-A., Fortin, B., & Lacroix, G. (2002). Marriage market, divorce legislation, and household labor supply. Journal of Political Economy, 110(1), 37–72. https://doi.org/10.1086/324385.
Connelly, R. (1992). The effect of child care costs on married women’s labor force participation. The Review of Economics and Statistics, 74, 83–90. https://doi.org/10.2307/2109545.
Cotton, J. L., & Tuttle, J. M. (1986). Employee turnover: A meta-analysis and review with implications for research. Academy of Management Review, 11(1), 55–70. https://doi.org/10.5465/amr.1986.4282625.
Cragg, J. G. (1971). Some statistical models for limited dependent variables with application to the demand for durable goods. Econometrica: Journal of the Econometric Society, 39, 829–844, https://doi.org/10.2307/1909582.
Cubbin, C., Pedregon, V., Egerter, S., & Braveman, P. (2008). Where we live matters for our health: Neighborhoods and health. Princeton, NJ: Robert Wood Johnson Foundation Commission to Build a Healthier America.
Currie, J., & Madrian, B. C. (1999). Health, health insurance and the labor market. Handbook of Labor Economics, 3, 3309–3416. https://doi.org/10.1016/S1573-4463(99)30041-9.
Dahl, S., Cvancarova, M., Dahl, A. A., & Fossa, S. D. (2016). Work ability in prostate cancer survivors after radical prostatectomy. Scandinavian Journal of Urology, 50(2), 116–122. https://doi.org/10.3109/21681805.2015.1100674.
Darity, W. a. M., Patrick (1998). Evidence on Discrimination in Employment: Codes of color, codes of gender. Journal of Economic Perspectives, 12(2), 63–90. https://doi.org/10.1257/jep.12.2.63.
Engel, J., Kerr, J., Schlesinger-Raab, A., Sauer, H., & Holzel, D. (2003). Axilla surgery severely affects quality of life: Results of a 5-year prospective study in breast cancer patients. Breast Cancer Research and Treatment, 79(1), 47–57.
Finkelstein, A., Luttmer, E. F., & Notowidigdo, M. J. (2013). What good is wealth without health? The effect of health on the marginal utility of consumption. Journal of the European Economic Association, 11(s1), 221–258. https://doi.org/10.1111/j.1542-4774.2012.01101.x.
Freedman, R. A., Virgo, K. S., He, Y., Pavluck, A. L., Winer, E. P., Ward, E. M., et al. (2011). The association of race/ethnicity, insurance status, and socioeconomic factors with breast cancer care. Cancer, 117(1), 180–189. https://doi.org/10.1002/cncr.25542.
Gehrke, B., & Weber, E. (2018). Identifying asymmetric effects of labor market reforms. European Economic Review, 110, 18–40. https://doi.org/10.1016/j.euroecorev.2018.07.006.
Golden, L. (2008). Limited access: Disparities in flexible work schedules and work-at-home. Journal of Family and Economic Issues, 29(1), 86–109. https://doi.org/10.1007/s10834-007-9090-7.
Grogan, L., & Sadanand, A. (2013). Rural electrification and employment in poor countries: Evidence from Nicaragua. World Development, 43, 252–265. https://doi.org/10.1016/j.worlddev.2012.09.002.
Grossbard, S. (2015). A theory of allocation of time in markets for labor and marriage: Macromodel. In Grossbard S. (Ed.), The marriage motive: A price theory of marriage (pp. 21–32). New York: Springer. https://doi.org/10.1007/978-1-4614-1623-4_3.
Grossman, M. (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80(2), 223–255. https://doi.org/10.1086/259880.
Gruber, J. (2000). Health insurance and the labor market. Handbook of Health Economics, 1, 645–706. https://doi.org/10.1016/S1574-0064(00)80171-7.
Grunfeld, E. A., Drudge-Coates, L., Rixon, L., Eaton, E., & Cooper, A. F. (2013). The only way I know how to live is to work”: A qualitative study of work following treatment for prostate cancer. Health Psychology, 32(1), 75.
Gurmu, S. (1997). Semi-parametric estimation of hurdle regression models with an application to medicaid utilization. Journal of Applied Econometrics. https://doi.org/10.1002/(SICI)1099-1255(199705)12:3%3C225::AID-JAE445%3E3.0.CO;2-Y.
Gurmu, S., & Trivedi, P. K. (1996). Excess zeros in count models for recreational trips. Journal of Business & Economic Statistics, 14(4), 469–477. https://doi.org/10.1080/07350015.1.
Halpern, J., & Hausman, J. A. (1986). Choice under uncertainty: A model of applications for the social security disability insurance program. Journal of Public Economics, 31(2), 131–161. https://doi.org/10.1016/0047-2727(86)90015-0.
Hanoch, G. (1965). The “backward-bending” supply of labor. Journal of Political Economy, 73(6), 636–642. https://doi.org/10.1086/259089.
Hansen, J. A., Feuerstein, M., Calvio, L. C., & Olsen, C. H. (2008). Breast cancer survivors at work. Journal of Occupational and Environmental Medicine, 50(7), 777–784. https://doi.org/10.1097/JOM.0b013e318165159e.
Heckman, J. J. (1977). Sample selection bias as a specification error (with an application to the estimation of labor supply functions). Cambridge, MA: National Bureau of Economic Research. https://doi.org/10.3386/w0172.
Heinesen, E., Imai, S., & Maruyama, S. (2018). Employment, job skills and occupational mobility of cancer survivors. Journal of Health Economics, 58, 151–175. https://doi.org/10.1016/j.jhealeco.2018.01.006.
Hellström, J. (2002). Count data modelling and tourism demand. Umeå: Umeå Economic Studies.
Hofler, R. A., & Murphy, K. J. (1994). Estimating reservation wages of employed workers using a stochastic frontier. Southern Economic Journal, 60, 961–976.
Holzbeierlein, J. M., McLaughlin, M. D., & Thrasher, J. B. (2004). Complications of androgen deprivation therapy for prostate cancer. Current Opinion in Urology, 14(3), 177–183. https://doi.org/10.3816/CGC.2003.n.022.
Hoynes, H., Simeonova, E., & Simonsen, M. (2016). Health and the labor market–New developments in the literature. Labour Economics, 43, 1–5. https://doi.org/10.1016/j.labeco.2016.07.002.
Jeon, S. H. (2017). The long-term effects of cancer on employment and earnings. Health Economics, 26(5), 671–684. https://doi.org/10.1002/hec.3342.
Jones, A. M. (1992). A note on computation of the double-hurdle model with dependence with an application to tobacco expenditure. Bulletin of Economic Research, 44(1), 67–74. https://doi.org/10.1111/j.1467-8586.1992.tb00507.x.
Kiasuwa Mbengia, R., Tiraboschi, M., Bouland, C., & de Brouwer, C. (2018). How do social security schemes and labor market policies support the return-to-work of cancer survivors? A review article on challenges and opportunities in the European Union. Journal of Cancer Policy. https://doi.org/10.1016/j.jcpo.2018.02.008.
Killingsworth, M. R., & Heckman, J. J. (1986). Female labor supply: A survey. Handbook of Labor Economics, 1, 103–204. https://doi.org/10.1016/S1573-4463(86)01005-2.
Kirschenbaum, A., & Weisberg, J. (2002). Employee’s turnover intentions and job destination choices. Journal of Organizational Behavior, 23(1), 109–125. https://doi.org/10.1002/job.124.
Kline, P., & Moretti, E. (2013). Place based policies with unemployment. The American Economic Review, 103(3), 238–243. https://doi.org/10.1257/aer.103.3.238.
Koopman, C., Pelletier, K. R., Murray, J. F., Sharda, C. E., Berger, M. L., Turpin, R. S., et al. (2002). Stanford presenteeism scale: Health status and employee productivity. Journal of Occupational and Environmental Medicine, 44(1), 14–20.
Lloyd, K. M., & Auld, C. J. (2002). The role of leisure in determining quality of life: Issues of content and measurement. Social Indicators Research, 57(1), 43–71. https://doi.org/10.1023/A:1013879518210.
McCullagh, P., & Nelder, J. A. (1989). Generalized linear models (Vol. 37). Boca Raton: CRC Press. https://doi.org/10.1016/0377-2217(84)90282-0.
Mehnert, A. (2011). Employment and work-related issues in cancer survivors. Critical Reviews in Oncology/Hematology, 77(2), 109–130. https://doi.org/10.1016/j.critrevonc.2010.01.004.
Melaku, Y. A., Appleton, S. L., Gill, T. K., Ogbo, F. A., Buckley, E., Shi, Z., et al. (2018). Incidence, prevalence, mortality, disability-adjusted life years and risk factors of cancer in Australia and comparison with OECD countries, 1990–2015: Findings from the Global Burden of Disease Study 2015. Cancer Epidemiology, 52, 43–54. https://doi.org/10.1016/j.canep.2017.11.007.
Miller, K. D., Siegel, R. L., Lin, C. C., Mariotto, A. B., Kramer, J. L., Rowland, J. H., et al. (2016). Cancer treatment and survivorship statistics, 2016. CA: A Cancer Journal for Clinicians, 66(4), 271–289. https://doi.org/10.3322/caac.21349.
Mincer, J. (1962). Labor force participation of married women: A study of labor supply. In Mincer, J. (Ed.), Aspects of labor economics (pp. 63–105). Princeton, NJ: Princeton University Press.
Moses, K. A., Paciorek, A. T., Penson, D. F., Carroll, P. R., & Master, V. A. (2010). Impact of ethnicity on primary treatment choice and mortality in men with prostate cancer: Data from CaPSURE. Journal of Clinical Oncology, 28(6), 1069–1074. https://doi.org/10.1200/JCO.2009.26.2469.
Ng, T. W., & Feldman, D. C. (2009). Age, work experience, and the psychological contract. Journal of Organizational Behavior, 30(8), 1053–1075. https://doi.org/10.1002/job.599.
Okunade, A. A., Suraratdecha, C., & Benson, D. A. (2010). Determinants of Thailand household healthcare expenditure: The relevance of permanent resources and other correlates. Health Economics, 19(3), 365–376. https://doi.org/10.1002/hec.1471.
Osmani, A. R., & Okunade, A. A. (2018). Cancer survivors in the labor market: Evidence from recent US micro-panel data. Economic Modelling. https://doi.org/10.1016/j.econmod.2018.11.008.
Pedersen, V. H., Armes, J., & Ream, E. (2012). Perceptions of prostate cancer in Black African and Black Caribbean men: A systematic review of the literature. Psycho-Oncology, 21(5), 457–468. https://doi.org/10.1002/pon.2043.
Podor, M., & Halliday, T. J. (2012). Health status and the allocation of time. Health Economics, 21(5), 514–527. https://doi.org/10.1002/hec.1725.
Portney, P. R., & Mullahy, J. (1986). Urban air quality and acute respiratory illness. Journal of Urban Economics, 20(1), 21–38. https://doi.org/10.1016/0094-1190(86)90013-6.
Pudney, S. (1989). Modelling individual choice. The econometrics of corners, kinks and holes. Oxford: Basil Blackwell.
Ransom, M. R. (1987). An empirical model of discrete and continuous choice in family labor supply. The Review of Economics and Statistics, 69, 465–472. https://doi.org/10.2307/1925534.
Salmon, C., & Tanguy, J. (2016). Rural electrification and household labor supply: Evidence from Nigeria. World Development, 82, 48–68. https://doi.org/10.1016/j.worlddev.2016.01.016.
Schmidt, D. E., & Duenas, G. (2002). Incentives to encourage worker-friendly organizations. Public Personnel Management, 31(3), 293–308. https://doi.org/10.1177/009102600203100303.
Schneider, U., Trukeschitz, B., Mühlmann, R., & Ponocny, I. (2013). Do I stay or do I go?”—Job change and labor market exit intentions of employees providing informal care to older adults. Health Economics, 22(10), 1230–1249. https://doi.org/10.1002/hec.2880.
Short, P. F., Vasey, J. J., & Moran, J. R. (2008). Long-term effects of cancer survivorship on the employment of older workers. Health Services Research, 43(1p1), 193–210. https://doi.org/10.1111/j.1475-6773.2007.00752.x.
Siegel, R. L., Miller, K. D., & Jemal, A. (2018). Cancer statistics, 2018. CA: A Cancer Journal for Clinicians, 68(1), 7–30. https://doi.org/10.3322/caac.21442.
Steiner, J. F., Cavender, T. A., Main, D. S., & Bradley, C. J. (2004). Assessing the impact of cancer on work outcomes: what are the research needs? Cancer: Interdisciplinary International Journal of the American Cancer Society, 101(8), 1703–1711. https://doi.org/10.1002/cncr.20564.
Storey, D. J., McLaren, D. B., Atkinson, M. A., Butcher, I., Liggatt, S., O’Dea, R., et al. (2012). Clinically relevant fatigue in recurrence-free prostate cancer survivors. Annals of Oncology, 23(1), 65–72. https://doi.org/10.1093/annonc/mdr034.
Strauss, J., & Thomas, D. (1998). Health, nutrition, and economic development. Journal of Economic Literature, 36(2), 766–817.
Swanberg, J. E., Nichols, H. M., Ko, J., Tracy, J. K., & Vanderpool, R. C. (2017). Managing cancer and employment: Decisions and strategies used by breast cancer survivors employed in low-wage jobs. Journal of Psychosocial Oncology, 35(2), 180–201. https://doi.org/10.1080/07347332.2016.1276503.
Tobin, J. (1958). Estimation of relationships for limited dependent variables. Econometrica: Journal of the Econometric Society, 26, 24–36. https://doi.org/10.2307/1907382.
Trevor, C. O. (2001). Interactions among actual ease-of-movement determinants and job satisfaction in the prediction of voluntary turnover. Academy of Management Journal, 44(4), 621–638. https://doi.org/10.5465/3069407.
US Bureau of Labor Statistics. (2015). Labor force characteristics by race and ethnicity, 2014. Washington, DC: US Bureau of Labor Statistics.
Van Breukelen, W., Van der Vlist, R., & Steensma, H. (2004). Voluntary employee turnover: Combining variables from the ‘traditional’ turnover literature with the theory of planned behavior. Journal of Organizational Behavior, 25(7), 893–914. https://doi.org/10.1002/job.281.
Vuong, Q. H. (1989). Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica: Journal of the Econometric Society, 307–333, https://doi.org/10.2307/1912557.
Ward, E., Jemal, A., Cokkinides, V., Singh, G. K., Cardinez, C., Ghafoor, A., et al. (2004). Cancer disparities by race/ethnicity and socioeconomic status. CA: A Cancer Journal for Clinicians, 54(2), 78–93. https://doi.org/10.3322/canjclin.54.2.78.
Welch, F. (1967). Labor-market discrimination: An interpretation of income differences in the rural South. Journal of Political Economy, 75(3), 225–240. https://doi.org/10.1086/259274.
White-Means, S., & Hersch, J. (2005). Health insurance disparities in traditional and contingent/alternative employment. International Journal of Health Care Finance and Economics, 5, 351–368. https://doi.org/10.1007/s10754-005-5559-9.
White-Means, S., Rice, M., Dapremont, J., Davis, B., & Martin, J. (2015). African American women: surviving breast cancer mortality against the highest odds. International Journal of Environmental Research and Public Health, 13(1), 6. https://doi.org/10.3390/ijerph13010006.
Wooldridge, J. M. (2005). Simple solutions to the initial conditions problem in dynamic, nonlinear panel data models with unobserved heterogeneity. Journal of Applied Econometrics, 20(1), 39–54. https://doi.org/10.1002/jae.770.
Yen, S. T., Jensen, H. H., & WANG, O. (1996). Cholesterol information and egg consumption in the US: A nonnormal and heteroscedastic double-hurdle model. European Review of Agricultural Economics, 23(3), 343–356. https://doi.org/10.1093/erae/23.3.343.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
White-Means, S.I., Osmani, A.R. Job Market Prospects of Breast vs. Prostate Cancer Survivors in the US: A Double Hurdle Model of Ethnic Disparities. J Fam Econ Iss 40, 282–304 (2019). https://doi.org/10.1007/s10834-018-09607-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10834-018-09607-x
Keywords
- Breast cancer
- Prostate cancer
- Double hurdle model
- Medical expenditure panel survey
- Employment disparities