Abstract
Exposure to domestic violence in the preschool years is consistently associated with children’s heightened risk for developing behavior problems. Maternal meta-emotion philosophy (awareness, acceptance, and coaching of children’s emotions) has been identified as an important protective factor in children’s development of internalizing and externalizing behaviors following exposure to domestic violence. However, mothers who are victims of domestic violence often experience symptoms of depression, anxiety, and post-traumatic stress, which may undermine their capacity to respond to their children’s negative emotions. The present study examines the protective role of maternal meta-emotion philosophy among mothers and preschool-aged children exposed to domestic violence. Participants were 95 mothers (mean age = 31.78) and their preschool-aged children (mean age = 4.11) who had witnessed domestic violence involving their mothers. Multiple regression analyses, controlling for family socioeconomic status and child exposure to interpersonal violence in the family, indicated that maternal symptomatology was positively associated with children’s internalizing problems. In addition, maternal awareness and coaching of children’s negative emotions was found to moderate relations between maternal symptomatology and children’s internalizing behaviors, and maternal awareness of children’s negative emotions was found to moderate relations between maternal symptomatology and children’s externalizing behaviors. These findings expand our understanding of maternal meta-emotion philosophy as a protective factor for preschoolers who have witnessed domestic violence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children under the age of five are disproportionately represented in households with domestic violence, with an estimated 7.1% of children witnessing domestic violence in the before age five (Cochran 1995; Fantuzzo et al. 1997; Finkelhor et al. 2009). Preschoolers exposed to domestic violence are at higher risk for developing externalizing behavior problems such as aggressive behavior and conduct problems (Fantuzzo et al. 1991; Shipman et al. 2004) and internalizing behavior problems such as depressive symptoms, anxiety, worry, and PTSD (e.g. Graham-Bermann 1996; Sternberg et al. 1993; Sturge-Apple et al. 2012).
Previous research has revealed that parental meta-emotion philosophy may be a protective factor for children exposed to domestic violence during the preschool years. Parental meta-emotion philosophy (Gottman et al. 1996, 1997; Katz et al. 2012, 1999) is comprised of parents’ awareness, acceptance, and coaching of their children’s emotions (Gottman et al. 1996, 1997, 2012; Katz et al. 1999). Awareness is defined as parents’ ability to recognize, describe, and report interest in their children’s experience of emotion. Acceptance pertains to parents’ comfort with their children’s expression of a given emotion. Coaching refers to parents’ assisting of their children in identifying the emotions they are experiencing, respect for their children’s emotional expression, and active involvement in situations that trigger a particular emotion for their children.
Generally, parents who are highly aware, accepting, and coaching of their children’s emotions view their children’s experiences of negative emotions as opportunities to scaffold their children’s development of effective emotion regulation strategies, build intimacy with their children, and help their children think of strategies to cope with emotions. In contrast, parents who have a dismissive meta-emotion philosophy generally believe that their children’s experiences of negative emotions are best ignored or denied, that these experiences are harmful, and that it is important to emphasize the transience of these experiences when comforting their children. Dismissing parents are typically not able to provide insight into a child’s experience of a negative emotion and cannot help their children to think about how this experience may affect them (Gottman et al. 1996).
In preschool-aged children without a history of trauma exposure, parents’ awareness, acceptance, and coaching of their children’s negative emotions, specifically anger and sadness, have been linked to children’s better self-regulatory capacities (e.g., more adaptive physiological reactivity to stress, employment of successful emotion regulatory skills, effortful control), lower levels of externalizing and internalizing problems, as well as better academic performance and higher IQ (Brajša-Žganec 2014; Chen et al. 2011; Cohodes et al. 2015; Gottman et al. 1996; Katz and Hunter 2007). For example, in a longitudinal study of children from preschool to middle childhood, Gottman et al. (1996) found that high levels of parental awareness, acceptance, and coaching of children’s anger and sadness was associated with greater levels of inhibitory control, better academic achievement, and better physical health.
Related to peer social interactions, Denham et al. (1997) found that preschool-aged children whose parents were more emotion coaching of their children’s general emotional experience had better peer relationships and social competence, compared to children whose parents were more emotion dismissing. This pattern of results is in line with Hooven et al.’s (1995) finding that 5-year-old children of parents who were more emotion coaching of their children’s anger and sadness had more positive social interactions with their best friend. In addition, in a sample of preschool-aged children who met criteria for Oppositional Defiant Disorder (ODD), Katz and Windecker-Nelson (2004) found that mothers’ awareness and emotion coaching of their children’s sadness, fear, and anger was positively related to the quality of children’s peer interactions. Although previous research has examined both mothers’ and fathers’ parental meta-emotion philosophy (e.g., Hooven et al. 1995), the present study specifically examines how maternal meta-emotion philosophy may moderate the relationship between maternal trauma symptomatology and children’s behavioral problems in a sample of mother–child dyads co-exposed to domestic violence.
Consistent with findings documenting the potential protective effect of maternal meta-emotion philosophy on children’s outcomes in samples without a history of trauma exposure, maternal meta-emotion philosophy of children’s negative emotions has been identified as a protective factor in preschool-aged children’s development of internalizing and externalizing problems, as well as emotion regulatory capacities, following exposure to domestic violence (Johnson and Lieberman 2007; Katz and Windecker-Nelson 2006). Katz and Windecker-Nelson (2006) found that maternal emotion coaching of children’s sadness, anger, and fear moderated the link between four- to 5-year-old children’s witnessing domestic violence in early childhood and their development of aggression, withdrawal, and anxious-depressed symptoms.
More recently, Ellis and Alisic (2014) coded maternal emotion coaching in recordings of fifteen mothers discussing a negative event with their preschool-aged children who were exhibiting trauma symptoms, and found a positive correlation between mothers’ emotion coaching of their children’s emotional experience during a dyadic conversation about a conflict and children’s utilization of adaptive emotion regulation skills. A study by Johnson and Lieberman (2007) examined effects of maternal attunement (Stern 1985), a closely related but distinct construct measured by both clinician ratings of the parent–child relationship and items from the maternal emotion coaching subscale of Gottman’s Meta-Emotion Interview (specifically with regard to children’s sadness and anger), on children’s externalizing problems following domestic violence. Controlling for the severity of children’s domestic violence exposure, maternal attunement to their preschool-aged children’s sadness and anger was significantly associated with lower externalizing behavior among children exposed to domestic violence (Johnson and Lieberman 2007).
It is critical to test each unique subscale of Gottman’s meta-emotion philosophy (i.e. awareness, acceptance, and coaching) in a sample of mother–child dyads exposed to domestic violence because evidence suggests that maternal trauma symptomatology may differentially affect each of the three components of maternal meta-emotion philosophy. With regard to awareness, mothers’ poorer adaptation following trauma exposure has been found to be associated with a lack of attunement and empathy in interactions with her children, suggesting that exposure to domestic violence may compromise mothers’ awareness of their children’s experience of sadness and anger (Koren-Karie et al. 2004, 2008). Also, related to maternal awareness of children’s sadness and anger, parents exposed to domestic violence and experiencing psychological distress have been found to be less available and involved in their children’s lives (e.g., Lyons-Ruth et al. 2002; Pianta and Egeland 1990) and therefore may have fewer opportunities to observe their children’s experiences of anger and sadness.
Other research indicates unique effects of domestic violence on mothers’ emotional acceptance. Related to maternal acceptance of children’s sadness and anger, Lieberman (2004) suggests that, for mothers exposed to domestic violence, children’s emotions may represent a reminder of their own trauma, which may lead to maternal avoidance. Avoidance surrounding children’s experience of negative emotions, such as sadness and anger, as a result of trauma may translate into lower levels of acceptance and coaching of children’s negative emotions. Finally, with regard to specific deficits in maternal coaching, trauma-related symptomatology (e.g., depression, hyperarousal, avoidance, intrusions, anxiety) may also make it more difficult for parents to offer sustained, empathic structuring around their children’s emotional experiences as these symptoms are known to affect executive function (Fossati et al. 2001; Leskin and White 2007), which may impact parents’ planning abilities, narrative coherence, and ability to successfully assist their children in processing emotional events.
In summary, the present study investigates whether maternal meta-emotion philosophy—as measured by maternal awareness, acceptance, and coaching of preschool-aged children’s sadness and anger—moderates the relationship between maternal symptomatology and child behavioral outcomes (internalizing and externalizing behaviors) in a sample of dyads exposed to domestic violence. It was hypothesized that, among mothers and children exposed to domestic violence, maternal meta-emotion philosophy (maternal awareness, assistance, and acceptance of children’s sadness and anger) would moderate the relationship between maternal symptomatology and children’s externalizing and internalizing problems. Specifically, it was hypothesized that there would be a significant positive association between maternal symptomatology and children’s behavioral problems for mothers with low levels of awareness, acceptance, and coaching of their children’s negative emotions (sadness and anger). It was also hypothesized that high levels of maternal awareness, acceptance, and coaching of children’s negative emotions would buffer the negative effects of maternal symptomatology on children’s behavioral problems.
Method
Participants
The current study included 95 children (48 male; M age = 4.11 years, SD = .95) and mothers (M age = 31.78 years, SD = 6.90) who were referred to [blinded for review]. Mother–child dyads were referred due to concern about the child’s behavior and/or the mother’s parenting following the dyad’s exposure to domestic violence. Referral sources included family court (40%), domestic violence service providers (12%), medical providers (9%), preschools (6%), other agencies (12%), child protective services (3%), former clients (6%), and self-referrals (3%). Dyads met the following inclusion criteria: the child was between the ages of 3 and 5 years at time of intake; the child witnessed domestic violence involving the mother in the dyad; and the perpetrator of marital violence was no longer living in the home with the dyad. In order to assess dyadic exposure to domestic violence, mothers completed the Revised Conflict Tactics Scales, a measure of the occurrence of conflict-related behaviors between romantic partners in the previous year of their relationship (Straus et al. 1996).
Exclusionary criteria consisted of the following: mother or child mental intellectual disability or autism spectrum disorders; substance abuse; or a life-threatening medical condition. In addition, mothers and children had to speak either English or Spanish and there could be no confirmed case of physical or sexual abuse perpetrated by the mother against the child.
Children in the study were 38.9% (n = 37) mixed ethnicity, 21.1% Latino/a (n = 20), 20.0% African American (n = 19), 13.7% Caucasian (n = 13), 4.2% Asian (n = 4), and 2.1% “other” (n = 2). Children were 52.6% monolingual English speakers (n = 50), 13.7% monolingual Spanish speakers (n = 13), and 5.3% bilingual English and Spanish speakers (n = 5); language data was missing for 27 children. Mothers were 30.5% Caucasian (n = 29), 29.5% Latina (n = 28), 22.1% African American (n = 21), 7.4% Asian (n = 7), 6.3% mixed ethnicity (n = 6); and 4.3% “other” (n = 4). Mothers were 55.8% English-speaking (n = 53) and 15.8% (n = 15) Spanish-speaking; language data was missing for 27 mothers. Mothers had completed an average of 12.99 years of education (SD = 3.41) and had mean family incomes of $22,945 per year (SD = $17,310), with 37.2% of families having incomes below the federal poverty line per the Department of Health and Human Services Guidelines (Department of Health and Human Services 2004). Seventy-one percent of mothers in the sample had scores on the Symptoms Checklist-90-R (SCL-90-R) that were above the clinical cut-off for psychological distress.
Procedure
The Committee for Human Research at [blinded for review] and the Institutional Review Board of [blinded for review] approved all research procedures, and all participants gave informed consent to participate in all research procedures prior to participating in the study. Mother–child dyads that met study criteria and who were willing to participate were scheduled for an initial clinic appointment. Mothers were scheduled for a clinic visit in which they were administered a semi-structured interview that asked about demographic information, maternal meta-emotion philosophy, the prevalence of domestic violence in their relationships, and mental health symptoms. Parents also completed a questionnaire about their children’s behaviors. At the end of the intake assessment phase, mothers were paid $30 for their participation.
Mothers were assessed by postdoctoral fellows, pre-doctoral interns, and master’s-level trainees in clinical psychology and social work who were supervised by licensed clinical psychologists. Interviews were conducted in an interview room at a hospital-based clinic specializing in early childhood trauma treatment and clinical research.
Measures
Maternal measures
Socio-economic status
A composite of family socio–economic status was created from maternal years of education and the family’s average yearly income by standardizing and summing both variables.
Meta-emotion interview
Gottman’s Meta-Emotion Interview is a semi-structured interview that is used to assess parents’ acceptance, awareness, and coaching of their child’s negative emotions, specifically sadness and anger (Gottman et al. 1996). Trained raters used verbatim transcripts of audio-taped interviews and an adapted version of Meta-Emotion Coding System (Gottman et al. 1997) to rate mothers on each of the meta-emotion categories. Each item was scored separately for children’s sadness and anger.
Maternal awareness of her child’s emotion consisted of the following items (for sadness and anger, respectively): mother notices child has emotion, mother has no problem distinguishing emotion, mother is descriptive of child’s experience of emotion, mother has insight into child’s experience of emotion, mother is descriptive of some remediation process with regard to emotion, mother knows cause of child’s emotion, mother talks at length about child’s experience of emotion, mother answers questions about emotion quickly and easily, mother shows interest with regard to child’s emotion.
Maternal acceptance of her child’s emotion consisted of the following items (for sadness and anger, respectively): mother seems comfortable with child’s emotion, child expresses this emotion, mother emphasizes child’s emotion, mother wants child to know it is okay to have emotion, mother wants child to talk to them about emotion, mother judges how and when child could express emotion, child is isolated when expressing emotion, child is punished when expressing emotion, child is restrained when expressing emotion, mother prefers child to be soothed before parent is involved in experience of emotion, mother distracts child from emotion, mother offers treat to distract child from emotion, mother uses mental/analytic approach to child’s emotion, mother says it is important to talk about the emotion, mother dislikes the way others express emotion, mother confides in interviewer, and mother digressed with question being asked.
Maternal coaching of her child’s emotion consisted of the following items (for sadness and anger, respectively): mother shows respect for child’s experience of the emotion, when child is upset, mother talks about situation and emotion, mother intervenes in situations causing emotion, mother comforts child during emotion, mother teaches child rules for appropriate expression of emotion, mother educates child with regard to the nature of emotion, mother teaches child strategies to self-soothe during experience of emotion, mother seems unsure of how to deal with emotion, mother seems to have given thought and energy to emotion, and mother’s strategies seem age and situation appropriate.
Each item in each of the three dimensions of parental meta-emotion philosophy was coded on a Likert Scale of 1–5 (1 = low and 5 = high) using the meta-emotion coding system to assess maternal awareness, acceptance, and coaching of sadness and ager (Katz et al. 1994). Raters were blind to study hypotheses and clinician ratings of child behavior problems and other indicators of the parent–child relationship. Interrater reliability, computed as correlations between independent coders for 30% of the sample, was established on each emotion (anger and sadness) and each meta-emotion construct (awareness, acceptance, and coaching). Interrater reliability for awareness of sadness and anger was r = .56 and r = .66, respectively. Interrater reliability for maternal acceptance of sadness and anger was r = .75 and r = .71, respectively. Interrater reliability for maternal coaching of sadness and anger was r = .70 and r = .66, respectively. The master coder’s codes were used when there were discrepancies between the master coder and reliability coders’ scores.
Composite scores were calculated for maternal awareness, coaching, and acceptance of both sadness and anger, respectively, by calculating total scores for component items on each subscale of maternal awareness, maternal acceptance, and maternal coaching. Next, a composite score for each meta-emotion dimension (awareness, coaching, and acceptance) was created by standardizing and summing the subscales for sadness and anger. For example, maternal acceptance of children’s sadness and maternal acceptance of children’s anger were both z-scored and then summed to create the maternal acceptance of children’s negative emotions composite. Maternal meta-emotion philosophy composites consisted of the following: (1) maternal awareness of negative emotions (composite of maternal awareness of sadness and maternal awareness of anger); (2) maternal acceptance of negative emotions (composite of maternal acceptance of sadness and maternal acceptance of anger); and (3) maternal coaching of negative emotions (composite of maternal coaching of sadness and maternal coaching of anger).
Symptoms checklist-90 revised (SCL-90-R)
The SCL-90-R is a 90-item checklist that assesses for psychiatric symptoms, and has been demonstrated to have a strong test–retest reliability (Derogatis 1996). The global severity index t-score, which is considered the most sensitive single indicator of psychological distress and calculated by taking the mean of all 90 items in the questionnaire, was used as a measure of total maternal symptomatology.
Child measures
Child behavioral checklist (CBCL 2/3 and 4/18)
The CBCL, a widely-used, reliable measure of children’s behavioral patterns that has been validated cross-culturally in clinical and non-clinical populations, was administered to mothers in an interview form (Achenbach 1991; Achenbach and Edelbrock 1993). The present study focused on two scales: (1) internalizing behavior problems, a composite of the withdrawn and anxious depressed subscales in the 2/3 version of the measure and a composite of the withdrawn, somatic complaints, and anxious depressed subscales in the 4/18 version of the measure, and (2) externalizing behavior problems, a composite of the delinquent behavior and aggressive behavior subscales in both versions of the measure. Since two age versions of the measure were used (2/3 and 4/18), t-scores from both age versions of the measure were used in order to compare across the two different versions. Cronbach’s alphas for internalizing problems were .83 (YCBCL) and .87 (CBCL), and .88 (YCBCL) and .88 (CBCL) for externalizing problems.
Children’s exposure to community violence, parent report version
The Children’s Exposure to Community Violence, Parent Report Version was completed by mothers to assess the level of the child’s exposure to violence (Richters and Martinez 1993). For purposes of this study, items related to community violence and to violence directed against the child were not considered. A composite score of child exposure to marital violence was constructed by adding the total number of items endorsed by the mother about the child’s exposure to violence against a family member or a person known to the child. This score was used to measure the child’s exposure to domestic violence in all analyses. On average, children in the present study had been exposed to an average of 3.43 instances of domestic violence (SD = 1.84).
Data Analyses
Hierarchical multiple regression analyses were performed to test the hypothesis that maternal symptomatology would be associated with children’s behavioral functioning in a sample of children exposed to domestic violence, as measured by the internalizing and externalizing subscales of the CBCL. In addition, we tested whether composites of maternal meta-emotion philosophy moderated effects of maternal symptomatology on children’s internalizing and externalizing disorders in a sample of children exposed to domestic violence.
Results
Table 1 presents descriptive statistics for all major study variables. Preliminary analyses were conducted to examine associations between demographic and main study variables. Study variables did not differ significantly based on child gender (all p-values greater than .5). Family SES was negatively associated with child internalizing problems (r = −.18 and p = .00). Zero-order correlations were examined for main study variables (Table 2). There was a significant positive correlation between the global severity index t-score on the SCL-90 and internalizing scores on the CBCL (r = .40, p = .00) and externalizing scores on the CBCL (r = .22, p = .03).
SES was entered as a covariate in all models. Children’s frequency of exposure to domestic violence was also entered into all models as a covariate. Predictor and product terms (created by multiplying each maternal meta-emotion philosophy subscale by maternal symptomatology) were centered-standardized (Aiken and West 1991). For each regression, the covariates (SES and children’s frequency of exposure to domestic violence) were entered in the first block, the centered predictor variables (meta-emotion philosophy composites, maternal symptomatology) were entered in the second block, and the centered moderator term was entered in the third block.
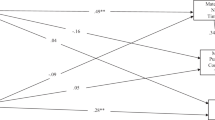
Six regression models were run to test interaction terms (created by multiplying each of the three meta-emotion philosophy composites by maternal symptomatology) as predictors of children’s internalizing and externalizing problems. Consistent with hypotheses, controlling for SES and frequency of children’s exposure to domestic violence, maternal symptomatology was positively associated with children’s internalizing problems (B = .34 t(94) = 3.75, p = .00) (Table 3). The interaction between maternal awareness of children’s negative emotions and maternal symptomatology was significantly associated with children’s internalizing problems (B = −.24, t(94) = −2.14, p = .04). In addition, the interaction between maternal coaching of children’s negative emotions and maternal symptomatology was also significantly associated with children’s internalizing problems (B = −.21, t(94) = −2.15, p = .03) (Table 4).
Contrary to hypotheses, controlling for SES and frequency of children’s exposure to domestic violence, maternal symptomatology was not associated with children’s externalizing problems. However, there was a significant interaction between maternal awareness of children’s negative emotions and maternal symptomatology in predicting children’s externalizing problems (B = −.30, t(94) = −2.55, p = .01) (Table 3). Neither the interaction between maternal acceptance of children’s negative emotions and maternal symptomatology nor the interaction between maternal coaching of children’s negative emotions and maternal symptomatology were significant associated with children’s externalizing problems (Table 5).
Simple slopes analyses were used to probe the three significant interaction effects (Aiken and West 1991). As shown in Fig. 1, among mothers with low and mid-levels of awareness of their children’s negative emotions, higher maternal symptomatology was significantly associated with higher levels of internalizing behaviors in their children (ts = 4.25, 3.59), suggesting that lower awareness of children’s negative emotions exacerbates the effect of maternal symptomatology on children’s internalizing problems. In contrast, for mothers with high levels of awareness of their children’s negative emotions, associations between maternal symptomatology and child’s internalizing problems were non-significant, suggesting that maternal awareness of negative emotions may buffer the negative effect of maternal symptomatology on children’s presentation of internalizing disorders. In line with this finding, among mothers with low and mid-levels of coaching of their children’s negative emotions, higher levels of maternal symptomatology were associated with higher levels of internalizing behaviors in children (ts = 4.01, 4.04). For mothers with high levels of coaching of their children’s negative emotions, there was no association between maternal symptomatology and child internalizing problems, suggesting that coaching may buffer children from the effects of maternal symptomatology on children’s internalizing behavior (Figs. 2, 3).
Simple slopes analyses were also used to probe the interaction between maternal awareness of children’s negative emotions and maternal symptomatology in predicting children’s externalizing behavior (Aiken and West 1991). Among mothers with low levels of awareness of their children’s negative emotions, higher maternal symptomatology was significantly associated with higher levels of externalizing behaviors in their children (t = 2.87), suggesting that lower awareness of children’s emotions exacerbates the effect of maternal symptomatology on children’s externalizing problems. In contrast, for mothers with mid- to high levels of awareness of their children’s negative emotions, the associations between maternal symptomatology and child’s externalizing problems were non-significant, suggesting that maternal awareness of negative emotions may buffer the negative effect of maternal symptomatology on children’s presentation of externalizing disorders.
Discussion
Previous research has documented links between maternal psychopathology and children’s development of behavioral problems following dyadic exposure to domestic violence, as well as the protective role of maternal coaching of children’s negative emotions for preschool-aged witnesses to domestic violence. The present study makes two novel contributions to the existing literature—(1) examining the role of a broader array of maternal meta-emotion scales (i.e. awareness, acceptance, and coaching of children’s negative emotions) in the relationship between maternal trauma symptomatology and children’s behavioral problems and (2) examining the interactive relations between maternal symptomatology, meta-emotion philosophy, and children’s behavioral problems in a sample of mothers and children exposed to domestic violence.
Consistent with previous research documenting associations between maternal psychopathology and children’s behavioral problems (Luoma et al. 2001; Silk et al. 2006), findings from the present study indicate that maternal symptomatology is associated with children’s internalizing and externalizing problems. We hypothesize that this association is due to the fact that mothers may be compromised in their ability to scaffold their children’s development of emotion regulatory capacities due to their own trauma exposure. In their seminal paper, Goodman and Gotlib (1999) delineate potential pathways between maternal and child risk for developing psychopathology, including child exposure to negative maternal cognitions, behaviors, and affect, as well as the stressful nature of children’s lives in the context of parental psychopathology. Additionally, stressing the importance of parents’ involvement in the emotional life of a trauma-exposed toddler, Levendosky et al. (2013) posited that, for preschool-aged children exposed to domestic violence, the severity of maternal psychopathology may be a more accurate indicator of a child’s behavioral reaction to trauma than a child’s own exposure to domestic violence.
Mothers exposed to domestic violence are at a heightened risk for developing symptoms of depression, anxiety disorders, and PTSD (Gorde et al. 2004; Kemp et al. 1991; Levendosky and Graham-Bermann 1998) and abuse and related symptomatology has been associated with decreased parenting warmth (Levendosky and Graham-Bermann 2000, 2001), poorer attachment quality (Cleaver et al. 2011), as well as increased hostility and disengagement during interactions with their children (Levendosky et al. 2006). Since preschoolers rely on their parents for effective external emotion regulation and guidance in developing their own self-regulatory strategies (Grolnick et al. 2006; Levendosky et al. 2003), the effects of abuse and related symptomatology on the parent–child relationship, attachment, and parenting may be especially salient for parents of preschool-aged children.
In addition, the present study found that maternal meta-emotion philosophy plays a significant role in the association between maternal and child psychopathology among preschool-aged children exposed to domestic violence. To summarize, maternal trauma-related symptomatology was positively associated with children’s internalizing problems, but not externalizing problems. Maternal awareness of children’s negative emotions moderated the effect of maternal symptomatology on children’s development of both externalizing and internalizing problems and maternal coaching moderated the relationship between maternal trauma-related symptomatology and children’s internalizing problems following domestic violence exposure. There was not a significant interaction between maternal acceptance or maternal coaching of children’s negative emotions and children’s externalizing problems.
Specifically, for mothers who were less aware of their children’s negative emotions, there was a significant positive association between maternal symptomatology and their children’s higher internalizing and externalizing problems, and for mothers who were less coaching of their children’s negative emotions, there was a significant positive association between maternal symptomatology and their children’s internalizing problems. These findings suggest that maternal awareness and coaching of children’s sadness and anger may be an important factor in the relationship between maternal symptomatology and children’s behavioral problems among children exposed to domestic violence.
One potential explanation for this pattern of results is that mothers who are less aware of and coaching of their children’s emotions may overlook opportunities to scaffold their child’s development of effective emotion regulation strategies to deal with their expressions of negative emotions. Given the wide range of emotions children may experience following exposure to domestic violence (Fantuzzo et al. 1997; Holt et al. 2008; Levendosky et al. 2003), this deficit of maternal emotion socialization may be particularly pernicious for preschool-aged children who are learning to cope with their experience of emotions. Parents play a key role in children’s development of self-regulation (Eisenberg et al. 1998), and children’s deficits in their abilities to regulate their emotions have been linked to elevated levels of internalizing and externalizing problems, underscoring the idea that a lack of maternal scaffolding in children’s development of adaptive emotion regulation skills may be linked to children’s development of behavior problems post-exposure to domestic violence (Cole et al. 1996).
As previously discussed, a mother’s abuse-related psychopathology and stress may cause her to be emotionally distant or unavailable to her children (e.g., Holden 2003) but, in the present sample, among mothers with high levels of awareness and coaching of their children’s emotions, there was no significant link between maternal symptomatology and children’s development of behavioral problems, suggesting that these mothers were able to overcome the predicted course of emotional disengagement in the parent–child relationship among children and parents exposed to domestic violence. We propose that domestic violence-exposed mothers with high levels of symptomatology who were able to be aware of and coaching of their children’s emotions may represent a uniquely resilient group of caregivers who were able to overcome the negative effects of symptomatology in order to be attuned to their children’s expressions of emotions. It is possible that these mothers demonstrated higher levels of awareness and coaching prior to their recent exposure to domestic violence or that they had a stronger relationship with their child at the outset of the occurrence of violence in the home.
Alternatively, in contrast, these mothers may have had a heightened awareness of their children’s displays of negative emotions due to the fact that they were experiencing high levels of symptomatology and may have, themselves, been feeling higher levels of both sadness and anger in response to recent traumatic exposure, making it easier to recognize and respond to displays of these emotions in their offspring. In line with findings that individuals with depression display an attentional bias for negative interpersonal stimuli as compared to neutral and positive stimuli (e.g., Gotlib et al. 2004; Joormann and Gotlib 2006), mothers experiencing psychopathology may be more likely to become aware of, and report, negative emotional states of their children, leading to higher scores on emotional awareness, as captured by the Meta-Emotion Interview.
To contribute to our understanding of this phenomenon, future research should directly compare these two theoretical models (i.e. that maternal meta-emotion philosophy prior to domestic violence exposure may enable mothers to maintain these high levels of awareness, acceptance, and coaching following the incident, as compared to the theory that mothers experiencing high levels of symptomatology may be more aware of their children’s negative affect, and therefore more likely to respond). More generally, future studies should explore what factors contribute to a mother’s ability to be attuned to her child’s emotions despite violent disruptions in the family context and her own psychopathology.
Inconsistent with our hypotheses, interactions between acceptance and maternal symptomatology did not significantly predict children’s behavioral problems. While null findings should be interpreted with caution, these findings suggest that, in contrast to maternal awareness and coaching, variations in maternal acceptance of children’s sadness and anger neither buffers nor exacerbates effects of maternal symptomatology on children’s behavioral problems. It is possible that with a trauma-exposed, preschool-age population, more direct means of emotional scaffolding, such as emotion coaching, are required to buffer effects of maternal symptomatology.
With regard to the fact that a significant interaction effect was found between maternal coaching of children’s negative emotions and maternal psychopathology in predicting children’s internalizing behaviors, but not externalizing behaviors, we hypothesize that this may have been due to the fact that preschool-aged children’s externalizing behaviors may be more difficult for mothers to address via coaching methods. By nature, externalizing behaviors represent more outward expressions of emotion and likely often involve aggression that may be more difficult to manage through verbal means. In contrast, the nature of children’s internalizing problems may be much easier for a parent to address through verbal instructions and conversation and therefore may have been more effective targets of maternal coaching. Although testing a different moderation model (exposure to domestic violence, as compared to maternal symptomatology as the independent variable), Katz and Windecker-Nelson (2006) found that maternal coaching of children’s sadness, anger, and fear moderated the relationship between child exposure to domestic violence and aggression (externalizing problems) to a greater degree than children’s anxiety and depression (internalizing problems).
Katz and Windecker Nelson’s (2006) pattern of results pertaining to externalizing problems is directly opposed to the findings of the present study and suggests a specific interaction between maternal symptomatology and maternal meta-emotion philosophy in predicting symptom outcomes, such that internalizing problems are more successfully buffered by maternal emotion socialization. Given the relatively small sample size of the present study, future studies should investigate differences between parental socialization of negative emotions in children with internalizing, as compared to externalizing problems, in the context of exposure to domestic violence.
Lastly, it should be noted that the present study examined composite scores of maternal meta-emotion philosophy with regard to sadness and anger, rather than analyzing these two emotions separately, due to the fact that they were strongly correlated for each subscale of the Meta-Emotion Interview (awareness subscale: r = .435, p < .001, acceptance subscale: r = .458, p < .001, coaching: r = .435, p < .001). For example, although children’s internalizing symptoms are typically associated with their dysregulation of sadness (Eisenberg et al. 2001), maternal coaching of both sadness and anger buffered the effect of maternal psychopathology on children’s internalizing symptoms. Similarly, although children’s externalizing problems are typically associated with their dysregulation of anger (Zeman et al. 2002), maternal awareness of both sadness and anger buffered the effect of maternal psychopathology on children’s externalizing symptoms. We posit that, although mothers may differ in their awareness, acceptance, and coaching of specific emotions (e.g., anger and sadness), a mother’s overall style of interaction with her children in dealing with negative emotions may be representative of her capacity to engage in external regulation of her child’s emotions and of the overall emotional climate of the parent–child relationship. However, future research is needed to examine the specific effects of maternal awareness, acceptance, and coaching of sadness and anger, as distinct emotions, on children’s presentation of behavioral problems following exposure to violence.
Limitations and Future Directions
Our finding that maternal symptomatology was positively associated with children’s internalizing behaviors among dyads exposed to domestic violence, and that maternal meta-emotion philosophy buffered children from these negative effects, adds to an existing body of literature that explores young children’s compounded risk of witnessing domestic violence and receiving care from caregivers experiencing psychopathology (Ybarra et al. 2007) and offers hopeful new avenues for future research. One limitation of the present study is its reliance on maternal report of both her mental health symptoms as well as her children’s externalizing and internalizing symptoms. Future studies should include third-party objective ratings of mother and child functioning following exposure to domestic violence. Another limitation of the present study is its reliance on cross-sectional data. Although previous literature suggests that children’s behavioral problems and maternal symptomatology consistently result from exposure to domestic violence, baseline data that predates domestic violence exposure is needed to support the directionality of these relations, and to provide stronger evidence that maternal meta emotion philosophy can buffer against the development of children’s behavior problems. Given that missing data prevented further examination of language differences among meta-emotion variables in the present study, and given language-based differences in acceptance scores in the present sample, future research should test differences in maternal awareness, acceptance, and coaching based on parent and child language.
In addition, as analyses did not meet Bonferroni-corrected thresholds (p < .0083) for significance, it is possible that the number of regressions conducted in the analyses may have increased the likelihood of Type 1 error. Future studies should also examine the longitudinal impact of maternal symptomatology on child outcomes post-clinical intervention to determine how maternal symptomatology relates to children’s development of internalizing and externalizing problems after more time has passed since children’s exposure to violence.
In this vein, in a sample of preschool-aged children exposed to domestic violence, maternal awareness of children’s emotions may be a critical marker of mothers’ ability to be involved in their children’s emotional lives. Although the present study did not test the sequential development of maternal meta-emotion constructs, in mother–child dyads exposed to domestic violence in which mothers are experiencing trauma-related symptomatology, maternal awareness of children’s emotions may be a precursor of mothers’ more advanced scaffolding of children’s emotion that encompasses all three meta-emotion philosophy subscales. Mothers who are better able to identify children’s expressions of negative emotions following dyadic exposure to domestic violence may be able to build on these foundational observational skills in time in order to develop more in depth skills around emotional acceptance and coaching, especially in light of recent research which suggests that parental meta-emotion philosophies are susceptible to change over time (Stettler and Katz 2014). Future studies should test a sequential model of maternal development of meta-emotion philosophies following dyadic exposure to domestic violence to assess the potential for change in mother’s awareness, acceptance, and coaching of their children’s negative emotions.
References
Achenbach, T. (1991). Manual for the child behavior checklist 4-18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry.
Achenbach, T., & Edelbrock, C. (1993). Manual for child behavior checklist and revised child behavioral profile. Burlington, VT: University of Vermont, Department of Psychiatry.
Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Newbury Park: Sage.
BrajšaŽganec, A. (2014). Emotional life of the family: Parental metaemotions, children’s temperament and internalising and externalising problems. Social Research: Journal for General Social Issues, 1, 25–45. doi:10.5559/di.23.1.02.
Chen, F., Lin, H., & Li, C. (2011). The role of emotion in parent-child relationships: Children’s emotionality, maternal meta-emotion, and children’s attachment security. Journal of Child and Family Studies, 21(3), 403–410. doi:10.1007/s10826-011-9491-y.
Cleaver, H., Unell, I., & Aldgate, J. (2011). Child abuse: Parental mental illness, learning disability, substance misuse, and domestic violence. 2nd edn. London: TSO.
Cochran, D. (1995). The tragedies of domestic violence: A qualitative analysis of civil restraining orders in Massachusetts. Boston, MA: Office of the Commissioner of Probation, Massachusetts Trial Court.
Cohodes, E., Hagan, M., Lieberman, A., & Dimmler, M. H. (2015). Maternal meta emotion philosophy and cognitive functioning in children exposed to violence. Journal of Child & Adolescent Trauma, 9(3), 191–199. doi:10.1007/s40653-015-0072-x.
Cole, P., Zahn-Waxler, C., Fox, N., Usher, B., & Welsh, J. D. (1996). Individual differences in emotion regulation and behavior problems in preschool children. Journal of Abnormal Psychology, 105(4), 518–529. doi:10.1037/0021-843X.105.4.518.
Denham, S. A., Mitchell-Copeland, J., Strandberg, K., Auerbach, S., & Blair, K. (1997). Parental contributions to preschoolers’ emotional competence: Direct and indirect effects. Motivation and Emotion, 21, 65–86. doi:10.1023/A:1024426431247.
Department of Health and Human Services (2004). Department of Health and Human Services Guidelines, Annual update of the HHS poverty guidelines. Retrieved from http://aspe.hhs.gov/poverty/01poverty.htm.
Derogatis, L. R. (1996). SCL-90-R: Symptom checklist-90-R: Administration, scoring, and procedures manual. Towson, MD: NCS Pearson.
Eisenberg, N., Cumberland, A., & Spinrad, T. (1998). Parental socialization of emotion. Psychological Inquiry, 9(4), 241–273. doi:10.1207/s15327965pli0904_1.
Eisenberg, N., Cumberland, A., Spinrad, T. L., Fabes, R. A., Shepard, S. A., Reiser, M., et al. (2001). The relations of regulation and emotionality to children’s externalizing and internalizing problem behavior. Child Development, 72(4), 1112–1134. doi:10.1111/1467-8624.00337.
Ellis, H., & Alisic, E. (2014). Maternal emotion coaching: A protective factor for traumatized children’s emotion regulation? Journal of Child and Adolescent Trauma, 6(2), 118–125. doi:10.1080/19361521.2013.755651.
Fantuzzo, J., Boruch, R., Beriama, A., Atkins, M., & Marcus, S. (1997). Domestic violence and children: Prevalence and risk in five major U.S. cities. Journal of the American Academy of Child and Adolescent Psychiatry, 36(1), 116–122. doi:10.1097/00004583199701000-00025.
Fantuzzo, J., DePaola, L., Lambert, L., Martino, T., Anderson, G., & Sutton, S. (1991). Effects of interparental violence on the psychological adjustment and competencies of young children. Journal of Consulting and Clinical Psychology, 58, 258–265. doi:10.1037/0022-006X.59.2.258.
Finkelhor, D., Turner, H., Ormrod, R., Hamby, S., & Kracke, K. (2009). Children’s exposure to violence: A comprehensive national survey. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention.
Fossati, P., Ergis, A. M., & Allilaire, J. F. (2001). Executive functioning in unipolar depression: A review. L’Encephale, 28(2), 97–107.
Goodman, S. H., & Gotlib, I. H. (1999). Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490. doi:10.1037/0033-295X.106.3.458.
Gorde, M., Helfrich, C., & Finlayson, M. (2004). Trauma symptoms and life skill needs of domestic violence victims. Journal of Interpersonal Violence, 19(6), 691–708. doi:10.1177/0886260504263871.
Gotlib, I. H., Krasnoperova, E., Yue, D. N., & Joormann, J. (2004). Attentional biases for negative interpersonal stimuli in clinical depression. Journal of Abnormal Psychology, 113(1), 127. doi:10.1037/0021-843X.113.1.121.
Gottman, J., Katz, L., & Hooven, C. (1996). Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. Journal of Family Psychology, 10(3), 243–268. doi:10.1037/0893-3200.10.3.243.
Gottman, J. M., Katz, L. F., & Hooven, C. (1997). Meta-emotion: How families communicate emotionally. Mahwah, NJ: Psychology press.
Graham-Bermann, S. (1996). Family worries: The assessment of interpersonal anxiety in children from violent and nonviolent families. Journal of Clinical Child Psychology, 25(3), 280–287. doi:10.1207/s15374424jccp2503_4.
Grolnick, W. S., McMenamy, J. M., & Kurowski, C. O. (2006). Emotional self-regulation ininfancy and toddlerhood. In L. Balter, & C. S. Tamis-LeMonda (Eds.), Child psychology: A handbook of contemporary issues. 2nd edn. (pp. 3–25). New York, NY: Psychology.
Holden, G. (2003). Children exposed to domestic violence and child abuse: Terminology and taxonomy. Clinical Child and Family Psychological Review, 6(3), 151–160. doi:10.1023/A:1024906315255.
Holt, S., Buckley, H., & Whelan, S. (2008). The impact of exposure to domestic violence on children and young people: A review of the literature. Child Abuse & Neglect, 32(8), 797–810. doi:10.1016/j.chiabu.2008.02.004.
Hooven, C., Gottman, J. M., & Katz, L. F. (1995). Parental meta-emotion structure predicts family and child outcomes. Cognitions and Emotion, 9, 229–264. doi:10.1080/02699939508409010.
Johnson, V., & Lieberman, A. (2007). Variations in behavior problems of preschoolers exposed to domestic violence: The role of mother’s attunement to children’s emotional experiences. Journal of Family Violence, 22(5), 297–308. doi:10.1007/s10896-007-9083-1.
Joormann, J., & Gotlib, I. H. (2006). Is this happiness I see? Biases in the identification of emotional facial expressions in depression and social phobia. Journal of Abnormal Psychology, 115(4), 705 doi:10.1037/0021-843X.115.4.705.
Katz, L., & Hunter, E. (2007). Maternal meta-emotion philosophy and adolescent depressive symptomatology. Social Development, 2, 343–360. doi:10.1111/j.14679507.2007.00388.x.
Katz, L., Maliken, A., & Stettler, N. (2012). Parental meta-emotion philosophy: A review of research and theoretical framework. Child Development Perspectives, 6(4), 417–422. doi:10.1111/j.1750-8606.2012.00244.x.
Katz, L.F., Mittmann, A., & Hooven, C. (1994). The meta-emotion coding system. Unpublished manuscript, University of Washington.
Katz, L. F., Wilson, B., & Gottman, J. M. (1999). Meta-emotion philosophy and family adjustment: Making an emotional connection. In M. J. Cox, & J. Brooks-Gunn (Eds.), Conflict and cohesion in families: Causes and consequences (pp. 131–165). Mahwah, NJ: Lawrence Erlbaum Associates.
Katz, L., & Windecker-Nelson, B. (2004). Parental meta-emotion philosophy in families with conduct-problem children: Links with peer relations. Journal of Abnormal Child Psychology, 32, 385–398. doi:10.1023/B:JACP.0000030292.36168.30.
Katz, L., & Windecker-Nelson, B. (2006). Domestic violence, emotion coaching, and child adjustment. Journal of Family Psychology, 20(1), 56–67. doi:10.1037/0893-3200.20.1.56.
Kemp, A., Rawlings, E., & Green, B. (1991). Post-traumatic stress disorder (PTSD) in batteredwomen: A shelter sample. Journal of Traumatic Stress, 4(1), 137–148. doi:10.1007/BF00976014.
Koren-Karie, N., Oppenheim, D., & Getzler-Yosef, R. (2004). Mothers who were severely abused during childhood and their children talk about emotions: Co-construction of narratives in light of maternal trauma. Infant Mental Health Journal, 25(4), 300–317. doi:10.1002/imhj.20007.
Koren-Karie, N., Oppenheim, D., & Getzler-Yosef, R. (2008). Shaping children’s internal working models through mother-child dialogues: The importance of resolving past maternal trauma. Attachment & Human Development, 10(4), 465–483. doi:10.1080/14616730802461482.
Leskin, L. P., & White, P. M. (2007). Attentional networks reveal executive function deficits in posttraumatic stress disorder. Neuropsychology, 21(3), 275. doi:10.1037/08944105.21.3.275.
Levendosky, A., Bogat, G., & Martinez-Torteya, C. (2013). PTSD symptoms in young children exposed to intimate partner violence. Violence Against Women, 19(2), 187–201. doi:10.1177/1077801213476458.
Levendosky, A., & Graham-Bermann, S. (1998). The moderating effect of parenting stress on children’s adjustment in women-abusing families. Journal of Interpersonal Violence, 13(3), 383–397. doi:10.1177/088626098013003005.
Levendosky, A. A., & Graham-Bermann, S. A. (2000). Behavioral observations of parenting in battered women. Journal of Family Psychology, 14(1), 80. doi:10.1037/08933200.14.1.80.
Levendosky, A. A., & Graham-Bermann, S. A. (2001). Parenting in battered women: The effects of domestic violence on women and their children. Journal of Family Violence, 16(2), 171–192. doi:10.1023/A:1011111003373.
Levendosky, A. A., Leahy, K. L., Bogat, G. A., Davidson, W. S., & von Eye, A. (2006). Domestic violence, maternal parenting, maternal mental health, and infant externalizing behavior. Journal of Family Psychology, 20(4), 544. doi:10.1037/0893-3200.20.4.544.
Levendosky, A., Huth-Bocks, A., Shapiro, D., & Semel, M. (2003). The impact of domestic violence on the maternal- child relationship and preschool-age children’s functioning. Journal of Family Psychology, 17(13), 275–287. doi:10.1177/088626098013003005.
Lieberman, A. F. (2004). Traumatic stress and quality of attachment: Reality and internalization in disorders of infant mental health. Infant Mental Health Journal, 25(4), 336–351. doi:10.1002/imhj.20009.
Luoma, I., Tamminen, T., Kaukonen, P., Laippala, P., Puura, K., Salmelin, R., & Almqvist, F. (2001). Longitudinal study of maternal depressive symptoms and child well-being. Journal of the American Academy of Child & Adolescent Psychiatry, 40(12), 1367–1374.
Lyons-Ruth, K., Wolfe, R., Lyubchik, A., & Steingard, R. (2002). Depressive symptoms in parents of children under age 3: Sociodemographic predictors, current correlates, and associated parenting behaviors. In N. Halfon, K. Taaffe McLearn, & M. A. Schuster (Eds.), Child rearing in America: Challenges facing parents with young children (pp. 217–259). Cambridge: Cambridge University Press.
Pianta, R. C., & Egeland, B. (1990). Life stress and parenting outcomes in a disadvantaged sample: Results of the mother-child interaction project. Journal of Clinical Child Psychology, 19(4), 329–336. doi:10.1207/s15374424jccp1904_4.
Richters, J. E., & Martinez, P. E. (1993). The NIMH community violence project: Children as victims of and witnesses to violence. In D. Reiss, J. E. Richters, M. Radke–Yarrow, & D. Scharf (Eds.), Children and violence (pp. 7–21). New York, NY: Guilford.
Shipman, K., Schneider, R., & Brown, A. (2004). Emotion dysregulation and psychopathology. In M. Beauregard (Ed.), Consciousness, emotional self-regulation and the brain 85, (61. Philadelphia, PA: John Benjamins.
Silk, J. S., Shaw, D. S., Forbes, E. E., Lane, T. L., & Kovacs, M. (2006). Maternal depression and child internalizing: The moderating role of child emotion regulation. Journal of Clinical Child and Adolescent Psychology, 35(1), 116–126. doi:10.1207/s15374424jccp3501_10.
Stern, D. N. (1985). The interpersonal world of the infant a view from psychoanalysis and developmental psychology: A view from psychoanalysis and developmental psychology. New York, NY: Basic books.
Sternberg, K., Lamb, M., Greenbaum, C., Cicchetti, D., Dawud, S., & Cortes, R. (1993). Effects of domestic violence on children’s behavior problems and depression. Developmental Psychology, 29(1), 44–52. doi:10.1037/0012-1649.29.1.44.
Stettler, N., & Katz, L. (2014). Changes in parents’ meta-emotion philosophy from preschool to early adolescence. Parenting, 14(3–4), 162–174. doi:10.1080/15295192.2014.945584.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The revised conflict tactics scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17(3), 283–316. doi:10.1177/019251396017003001.
Sturge-Apple, M., Davies, P., Cicchetti, D., & Manning, L. (2012). Interparental violence, maternal emotional unavailability and children’s cortisol functioning in family contexts. Developmental Psychology, 48(1), 237–249. doi:10.1037/a0025419.
Ybarra, G., Wilkens, S., & Lieberman, A. (2007). The influence of domestic violence on preschooler behavior and functioning. Journal of Family Violence, 22, 33–42. doi:10.1007/s10896-006-9054-y.
Zeman, J., Shipman, K., & Suveg, C. (2002). Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology, 31(3), 393–398. doi:10.1207/S15374424JCCP3103_11.
Acknowledgements
This research was supported by the National Institute of Mental Health Grant R21 MH59, 661 and by the Irving Harris Foundation. The authors also wish to thank Griselda Oliver Bucio, LMFT, Dr. Chandra Ghosh Ippen, Dr. Christine Zalecki, and Dr. Michelle Robbins-Broth.
Author Contributions
E.M.C. and S.C. designed the study, analyzed the data, and wrote the paper. A.F.L. collected the data, collaborated with the design of the study, and provided edits on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Cohodes, E., Chen, S. & Lieberman, A. Maternal Meta-Emotion Philosophy Moderates Effect of Maternal Symptomatology on Preschoolers Exposed to Domestic Violence. J Child Fam Stud 26, 1831–1843 (2017). https://doi.org/10.1007/s10826-017-0699-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10826-017-0699-3