Abstract
Purpose
To determine whether concomitant tamoxifen 20 mg with gonadotropins (tamoxifen-gonadotropin) versus letrozole 5 mg with gonadotropins (letrozole-gonadotropin) affects mature oocyte yield.
Methods
Open-label, single-institution, randomized trial. Inclusion criteria included the following: females, ages 18–44 years old, with new diagnosis of non-metastatic breast cancer, who were undergoing fertility preservation with either oocyte or embryo cryopreservation. Those with estrogen-receptor-positive (ER+) breast cancer were randomized to tamoxifen-gonadotropin or letrozole-gonadotropin. Another group with estrogen-receptor-negative (ER−) breast cancer was recruited, as a prospectively collected comparison arm who took neither letrozole nor tamoxifen (gonadotropin only). The primary outcome was the number of mature oocytes obtained from the cycle. The randomized groups were powered to detect a difference of three or more mature oocytes.
Results
Forty-five patients were randomized to tamoxifen-gonadotropin and fifty-one to letrozole-gonadotropin. Thirty-eight patients completed gonadotropin only. Age, antral follicle count, and body mass index were similar between the randomized groups. Our primary outcome of mature oocyte yield was similar between the tamoxifen-gonadotropin and letrozole-gonadotropin groups (12±8.6 vs. 11.6±7.5, p=0.81, 95%CI of difference =−2.9 to 3.7). In a pre-specified secondary comparison, mature oocyte yield was also similar with tamoxifen-gonadotropin or letrozole-gonadotropin versus gonadotropin only (12±8.6 vs. 11.6±7.5 vs. 12.4±7.2). There were no serious adverse events in any of the groups.
Conclusions
Tamoxifen-gonadotropin and letrozole-gonadotropin produced a similar number of mature oocytes. Women who received either tamoxifen-gonadotropin or letrozole-gonadotropin had a similar number of oocytes to the gonadotropin-only group.
Trial registration
NCT03011684 (retrospectively registered 1/5/2017, after 9% enrolled)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oocyte and embryo cryopreservation are accepted standard treatments for fertility preservation prior to breast cancer treatment [1]. However, the use of injectable gonadotropins in ovarian stimulation can induce estradiol levels up to ten times higher than physiologic levels [2,3,4]. While there have never been data to demonstrate a decrease in disease-free survival from estrogen-receptor-positive (ER+) breast cancer after ovarian stimulation, this elevation in estrogen levels has caused concern for oncology providers and patients diagnosed with ER+ breast cancer [5]. Over two decades ago, natural cycle in vitro fertilization (IVF) cycle was initially proposed as the safest approach to fertility preservation with ER+ breast cancer. While estradiol is not artificially elevated in natural cycle IVF, such cycles only yield a maximum of one oocyte.
Increasing the number of oocytes or embryos in storage can meaningfully boost the patients’ chance of future pregnancy after cryopreservation [6]. Novel approaches to safely obtaining more than one oocyte for cryopreservation in patients diagnosed with ER+ breast cancer have been introduced, over time. For example, ovarian stimulation with tamoxifen alone was shown to obtain twice as many mature eggs and embryos as natural cycle IVF [6]. Oktay and colleagues subsequently demonstrated that letrozole-gonadotropins might produce more oocytes or embryos than tamoxifen-gonadotropins and proposed that letrozole theoretically may be safer, due to lower estrogen levels [7, 8]. Meirow and colleagues then showed that tamoxifen-gonadotropins is also a safe and effective means of ovarian hyperstimulation in the setting of breast cancer.[3] These prior studies with letrozole and tamoxifen were often small, non-randomized, and employed concomitant use of lower injectable gonadotropin regimens than are commonly used today.[3, 8] The choice to use letrozole-gonadotropins or tamoxifen-gonadotropins during ovarian stimulation for breast cancer is presently largely guided by regional practice patterns.
Letrozole, an aromatase inhibitor, and tamoxifen, a selective estrogen receptor modulator (SERM), have different mechanisms of action. These differing mechanisms of action, at the level of the hypothalamus and pituitary or the ovarian follicle, have the potential to differentially affect fertility preservation outcomes. Within the follicle, aromatase inhibitors would be expected to lower estrogen and create a large accumulation of intra-follicular androgens, whereas SERMS like tamoxifen would not. Intra-follicular estrogen could be instrumental to follicular growth and oocyte development in animals [9]. Increased intra-follicular androgens can enhance early follicular growth but may also lead to increased follicular atresia [2, 10]. Clinically, a 2014 randomized trial of letrozole versus a SERM (clomiphene) for ovulation induction demonstrated that letrozole led to increased rates of both ovulation and live birth in women with polycystic ovary syndrome [10]. Conversely, the AMIGOS Trial of letrozole versus clomiphene for ovulation induction in the treatment of unexplained infertility showed similar rates of clinical pregnancy and live between the letrozole and clomiphene [11].
While tamoxifen and letrozole are both commonly used in ovarian stimulation in the setting of breast cancer, it is not clear if either helps to optimize oocyte yield, particularly in the setting of random-start ovarian stimulation [2]. We undertook the TAmoxifen or Letrozole in Estrogen Sensitive tumors (TALES) Trial to assess the impact of tamoxifen-gonadotropin and tamoxifen-gonadotropin on mature oocyte yield.
Materials and methods
We performed a randomized clinical trial. All study procedures were approved by the University of California, San Francisco (UCSF) Committee on Human Research.
Study overview and design
We conducted a randomized controlled trial of concomitant administration of tamoxifen-gonadotropins versus letrozole-gonadotropins during our standard ovarian stimulation protocol for patients undergoing oocyte or embryo cryopreservation. We also included an additional comparison arm of patients with ER− breast cancer who were undergoing gonadotropin-only stimulation. Our primary outcome was mature oocyte yield within a single cycle of ovarian stimulation.
The consulting physician identified patients eligible for the study at the initial fertility preservation consult visit. The prospect of their future fertility, following 2–5 years of refraining from conceiving owing to adjuvant endocrine treatment (if applicable), was discussed with the patient. A proposed ovarian stimulation protocol with gonadotropins was discussed with the patient in the consultation office. If ER+, we then invited them to participate in our randomized study to take either tamoxifen-gonadotropin or letrozole-gonadotropin. Written, informed consent for study participation was obtained by the recruiting physician after the patient chose to undergo oocyte or embryo cryopreservation.
The doses of medication to which patients with ER+ tumors were randomized were as follows: the standard dose of gonadotropin plus tamoxifen (20 mg per day) or standard dose of gonadotropin plus letrozole (starting dose 5 mg per day). The doses of tamoxifen and letrozole were chosen based on a review of common doses reported in the literature and based on discussion with our breast cancer research review board [3, 8]. Patients with ER− tumors were consented to study participation prior to ovarian stimulation, but took neither tamoxifen nor letrozole during their stimulation.
Ovarian stimulation protocol
In both the ER+ and ER− groups, ovarian stimulation was performed with a random-start GnRH antagonist protocol [2]. The starting dose and adjustment of gonadotropins were based on the clinic’s standard of care. The initial dosage of gonadotropins (Follistim, Merck; Gonal-F, EMD-Serono; and/or Menopur, Ferring) was determined by the patient’s age, body mass index (BMI), and ovarian reserve, as estimated by antral follicle count (AFC) (which was measured on the day of initial consultation). During the cycle, gonadotropin dosages were adjusted as needed, based on follicle count/size and estradiol levels (in the tamoxifen-gonadotropin and gonadotropin-only groups), to maximize response and minimizing the risk of ovarian hyperstimulation syndrome (OHSS). GnRH antagonist (0.25mg ganirelix acetate, Organon; or 0.25 mg cetrotide, EMD-Serono) was administered daily to prevent premature ovulation when the lead follicle measured ≥12-mm mean diameter.
Estradiol level was assessed at every clinic visit during ovarian stimulation. For patients with estrogen-sensitive breast cancer, 5 mg letrozole was administered daily beginning with the start of ovarian stimulation and letrozole was titrated up to as much as 10 mg per day with the goal of maintaining estradiol levels close to that observed during mono-follicular development in natural cycles ( <500 pg/mL). At the time of design of the TALES Trial, the titration of letrozole above 5 mg daily dose was believed to be likely to be able to keep estradiol levels below the typical physiologic peak of 500 pg/mL. The final dose of letrozole and tamoxifen was taken the evening of trigger injection [12]. Doses of tamoxifen were kept at 20 mg daily and were not titrated, as per the breast protection protocol previously used by Meirow and colleagues [3].
Final oocyte maturation was induced with sliding-scale hCG (1500 to 10,000 IU subcutaneously) or GnRH agonist (4 mg leuprolide acetate subcutaneously) trigger injection depending upon size of the follicular cohort and perceived risk of OHSS. The trigger injection in the tamoxifen-gonadotropin (ER+) and gonadotropin-alone (ER−) groups was administered when the largest follicle attained a mean two-dimensional diameter of 18 mm with the general cohort of follicles >13 mm. If letrozole was used, the criterion for trigger was a follicle reaching a mean diameter of 20 mm with a general cohort of follicles >13 mm, based on prior work by Oktay et al. that supported larger follicle size at trigger with letrozole [7].
Oocyte retrieval was performed under transvaginal ultrasound guidance, 36 h after trigger shot administration. Cumulus cells were stripped 2–3 h after retrieval and oocyte cryopreservation was performed by vitrification, according to the laboratory standard at the time. For patients desiring embryo cryopreservation, ICSI was performed with ejaculated sperm in meiosis II oocytes in a similar time frame. Embryos were cryopreserved on either day 3 or day 5, depending upon the quality and quantity of embryos in a given cohort.
Study population and eligibility requirements
From June 2016 to September 2020, women 18 to 44 years of age with a new diagnosis of non-metastatic breast cancer who had not yet undergone chemotherapy and who planned to undergo ovarian stimulation for fertility preservation with either oocyte or embryo cryopreservation were approached about joining the study during their initial fertility preservation consult. Eligibility criteria included the following: new breast cancer diagnosis; had not yet begun chemotherapy; planned to undergo ovarian stimulation and oocyte retrieval prior to cancer treatment. Exclusions included the following: chemotherapy had already commenced or been completed; history of recurrent breast cancer; stage IV breast cancer at diagnosis; if patient’s oncologist advised against the trial; any significant concurrent disease, illness, or psychiatric disorder that would have compromised patient safety or compliance and interfere with consent, study participation, follow-up, or interpretation of study results. We did not make any modifications to the enrollment criteria, once the study began.
Outcome measures
The primary outcome to be compared was mature oocyte yield in the tamoxifen-gonadotropin versus letrozole-gonadotropin group. Mature oocyte yield was defined as the number of meiosis II oocytes seen 2 to 3 h after oocyte retrieval during cumulus stripping. Some patients underwent more than one cycle of ovarian stimulation, so outcomes were only measured in the first cycle after informed consent was obtained. A secondary comparison of this primary outcome was mature oocyte yield in the groups receiving tamoxifen-gonadotropin (ER+) versus letrozole-gonadotropin (ER+) versus gonadotropins alone (ER−). Our other a priori secondary outcomes in the TALES Trial included the following: comparison of follicular fluid hormone levels, assessment of embryo quality (if applicable), and comparison of clinical pregnancy rates when cryopreserved tissue is eventually utilized among patients from the assigned stimulation regimens. These latter outcomes are either outside the focus of this manuscript, or remote from the present time, and so were not included in this analysis. Adverse events were defined as any side effects that resulted in discontinuation of study medication. Serious adverse events (SAEs) were defined as events that were fatal/immediately life-threatening or required inpatient hospitalization.
Sample size
Forty-four subjects in each group in our primary comparison (tamoxifen-gonadotropin versus letrozole-gonadotropin) were required to obtain 80% statistical power to demonstrate a clinically meaningful absolute difference of three mature oocytes, assuming a standard deviation of five mature oocytes per cycle with the use of an unpaired t-test with a two-sided significance level of 0.05. A difference of three mature oocytes was chosen as this number of oocytes could commonly lead to an additional embryo transfer in the future. For our power calculation, we used ten for the expected mean number of oocytes in the tamoxifen group, with the desired effect size of three [3]. The sample size was increased to 48 per arm for an expected dropout of 10%. We also planned to also enroll an additional approximately 44 patients with ER− breast cancer, to be used for our secondary comparison.
Randomization and allocation concealment
Randomization occurred in an unrestricted 1:1 ratio to receive either standard dose of gonadotropin plus tamoxifen (20 mg per day) or standard dose of gonadotropin plus letrozole (starting dose 5 mg per day). A computer-generated randomizer was used to determine study drug exposure after patients agreed to undergo ovarian stimulation and after informed written consent to participate in the study was obtained by the recruiting physician.
The treating physician and the patient could not be blinded to the study drug, for the following reasons: the suppressive effect of letrozole on estradiol; the absence of such an effect with tamoxifen; the standard need to counsel patients in our stimulation protocol about the progress of their stimulation cycle (based on their estradiol response). The embryologists who were counting mature oocytes were, importantly, blinded to the study drug.
Given the possibility of differential allocation to the study groups with our unrestricted (non-block randomized) approach, our recruitment for the study was to be considered complete once 44 patients completed ovarian stimulation in each of the randomization arms. Due to resource limitations, we planned to continue to recruit ER− patients in the comparison arm until the randomization arms of the study completed enrollment, and then stop the recruitment in the ER− group, at that point. With an approximate 2:1 ratio of patients with ER+:ER− breast cancer having presented to our clinic in the past, we estimated we would have approximately 44 patients in the ER− group, at the end of the study.
Statistical analysis
Statistical analysis was performed using Stata version 15 (Stata Corp., College Station, TX). To compare cycle and background characteristics between the two randomized patient groups in our primary aim, univariate analyses were performed. Characteristics of interest included the following: patient age, antral follicle count, body mass index (BMI), total gonadotropin dose, number of stimulation days, maximal estradiol level, trigger shot type, number of retrieved oocytes, number of mature oocytes, and plan for oocyte versus embryo cryopreservation. Continuous data are reported as means ± standard deviation (SD) and dichotomous or categorical outcome data are reported as percentages, as appropriate. In order to best understand the effects of tamoxifen and letrozole on ovarian stimulation outcomes, we performed a per-protocol data analysis. For continuous data, the two-sample t-test was used when data were normally distributed and the Wilcoxon two-sample test when distribution was skewed. For continuous data involving comparison of three groups, one-way ANOVA was used and the Kruskal-Wallis test was used when distribution was skewed. For variables in the ANOVA with p <0.05, a post hoc Bonferroni test was performed to provide estimates of the difference between each predictor variable, with adjustment for multiple comparisons. For categorical data, the chi-square test was used. A post hoc linear regression was performed to assess the impact of age on oocyte yield, once it was discovered that the average age of patients in our ER− comparison arm was significantly lower than the tamoxifen-gonadotropin group. All tests were two-tailed, and p-values <0.05 were considered statistically significant. For the primary outcome of mature oocyte yield, the 95% confidence interval of the observed difference between groups was also reported.
Trial registration, approval, and safety monitoring
This study was reviewed and approved by our institutional review board (15-17818). Since the study was performed on patients with cancer, the study was also approved by our institution’s cancer center review board and cancer disease-specific site (breast) review board. The cancer review board provided active oversight of the study, including at least an annual assessment of recruitment and adverse events. The trial was registered at ClinicalTrials.gov (NCT03011684). An independent safety monitoring board was assembled and a priori study stoppage criteria had been if mature oocyte yield was 50% higher in one of the groups at half-way point of attainment of recruitment goal.
The first patient was enrolled on July 21, 2016. By omission, this study was registered after the study start date on ClinicalTrials.gov on January 5, 2017. The trial was approved by three local review boards at our university and was not changed from the time of first enrollment to study completion. Between the beginning of enrollment and ClinicalTrials.gov registration, there were six patients enrolled in the letrozole group and six patients in the tamoxifen group. During this time period, there were no patients enrolled in the ER-negative group, though this group was included a priori from the outset of the study.
Results
Characteristics of the participants
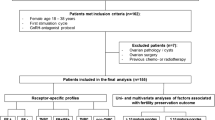
A total of 137 patients (ages 21 to 43 years old) were initially enrolled in the study (ER+, n=98; ER−, n=39) and study completion and attrition is detailed in Figure 1. After randomization, two patients (one in the tamoxifen arm and one in the letrozole arm) decided to not pursue ovarian stimulation due to financial or logistical reasons related to their cancer care. These patients were not included in the analysis. One patient in the tamoxifen group experienced cycle cancelation on day 5 of ovarian stimulation, at which time she had a single lead follicle of 17 mm. Her cycle was canceled due to unifollicular development. She was counted in the study as having had zero oocytes retrieved and zero mature oocytes and her outcome data were included in the primary and secondary comparisons.
Study flow diagram. Patients in the estrogen-receptor-positive group (ER+) were randomized to letrozole or tamoxifen and were analyzed according to completion of the protocol. Patients in the estrogen-receptor-negative group (ER−) did not receive a study intervention and were included as a secondary comparison group (without letrozole or tamoxifen)
The randomized groups in our study were similar for baseline antral follicle count, body mass index, and race/ethnicity (Table 1). However, there was a statistically significant difference in age between the three groups, as determined by one-way ANOVA (F(2,130=4.61, p=0.01). A Bonferroni post hoc test revealed that age was significantly higher in the tamoxifen-gonadotropin group than the gonadotropin-only group (35.4±0.8 vs. 32.5±0.6, p=0.01). The mean age for the tamoxifen-gonadotropin was 1.7 years less than the letrozole-gonadotropin group, though this difference was not statistically significant (35.4±0.8 vs. 33.7±0.6, p=0.18). Lastly, age was not statistically significantly different for letrozole-gonadotropin versus gonadotropin alone (33.7±0.6 vs. 32.5±0.6, p=0.64).
In vitro fertilization cycle characteristics
In vitro fertilization (IVF) cycle parameters, including total doses of gonadotropins, duration of stimulation, and trigger shot type, were similar between the three groups (Table 2). While the letrozole-gonadotropin protocol required trigger at larger lead follicle sizes, the letrozole follicles may have developed at a faster rate, as the average length of stimulation was similar across the treatment groups. The one significant difference in IVF parameters was peak estradiol levels, which were much lower in the letrozole group, by design. However, despite titrating doses of letrozole above 5 mg, peak estradiol levels did exceed 500 pg/mL.
Primary and secondary comparisons
Tamoxifen-gonadotropin and letrozole-gonadotropin yielded similar mean numbers of mature oocytes (12±8.6 vs. 11.6±7.5, p=0.81, 95%CI of difference =−2.9 to 3.7; Table 2). In the secondary comparison, letrozole-gonadotropin (ER+) or tamoxifen-gonadotropin (ER+) versus gonadotropin only (ER−) also yielded similar mean mature oocyte yields: tamoxifen-gonadotropin versus gonadotropin only appeared similar for mature oocyte yield (12±8.6 vs. 12.4±7.2, p=0.81, 95%CI of difference =−3.9 to 3.1); letrozole-gonadotropin versus gonadotropin only also appeared similar for mature oocyte yield (11.6±7.5 vs. 12.4±7.2, p=0.61, 95%CI of difference =−4 to 2.3). Total numbers of oocytes retrieved, oocyte maturity rates, and proportion of cycles with poor ovarian response were also similar between the three groups (Table 2).
Since age was discovered to be different between the tamoxifen-gonadotropin and gonadotropin-only groups, a post hoc sensitivity analysis was performed by including study group (tamoxifen-gonadotropin, letrozole-gonadotropin, and gonadotropin alone) and age in a general linear model to predict mature oocyte yield. Overall, the three arms of the study continued to appear clinically similar for mature oocyte yield, after adjustment for age: tamoxifen-gonadotropin versus letrozole-gonadotropin (estimated difference: 1.8 mature oocytes, p=0.22, 95%CI−1.1 to 4.8); tamoxifen-gonadotropin versus gonadotropin alone (estimated difference: 1.9 mature oocytes, p=0.24, 95%CI−1.3 to 4.8); letrozole-gonadotropin versus gonadotropin only (estimated difference: 0.1 mature oocytes, p=0.96, 95%CI−2.9 to 3.1).
Adverse events
No serious adverse events related to the treatments occurred during the study, including no unplanned hospitalizations during the study for any of the three groups. Though we did not collect a specific a priori list of side effects during treatment, our patients did undergo very close monitoring during the 2 weeks of the study, with frequent (every 1 to 3 days) visits for ultrasounds. No one stopped their medications due to self-report of concerns about side effects.
Discussion
When performing ovarian stimulation for fertility preservation for newly diagnosed ER+ breast cancer, tamoxifen-gonadotropin and letrozole-gonadotropin produce similar mature oocyte yields. Additionally, tamoxifen-gonadotropin and letrozole-gonadotropin also appear to produce similar mature oocyte yields to gonadotropin alone.
Our primary finding was that tamoxifen-gonadotropin and letrozole-gonadotropin produce similar mature oocyte yields. This observation is concordant with prior, non-randomized studies. Oktay and colleagues performed one of the only published trials to date that compared letrozole and tamoxifen in fertility preservation cycles [8]. In this smaller, prospective trial (n=60), with doses of gonadotropins that were lower than are generally used today, tamoxifen 60 mg daily plus FSH 150 international units (IU) and letrozole 5 mg daily plus FSH 150 IU did not show a significant difference in oocyte yield. However, the tamoxifen-gonadotropin group had a higher baseline FSH—suggesting lower starting ovarian reserve. In our study, baseline age and antral follicle count were similar between the tamoxifen and letrozole groups, supporting the interpretation that neither medicine, in a well-powered study, appears to substantially alter mature oocyte yield. The conclusion that mature oocyte yields are similar is further supported by another recent trial of tamoxifen-gonadotropin versus letrozole-gonadotropin from Europe (reported at the 2019 American Society of Reproductive Medicine Conference, not yet published) [13].
Despite differing mechanisms of action, we also observed that tamoxifen-gonadotropin and letrozole-gonadotropin likely produce similar mature oocyte yields to gonadotropin alone. This observation is also consistent with prior studies. Meirow and colleagues previously demonstrated similar oocyte yields with tamoxifen-gonadotropin versus gonadotropin alone [3]. Several non-randomized studies have compared letrozole-gonadotropin in ER+ breast cancer patients to gonadotropin alone and reported results similar to our study [14]. Oktay et al. compared ER+ patients using letrozole-gonadotropin to patients with tubal factor infertility (without cancer) using gonadotropin alone [7]. Similar mature oocyte yield was observed in both groups. In Revelli’s retrospective study of 50 patients with ER+ disease exposed to letrozole-gonadotropin versus 25 ER− disease exposed to gonadotropin alone, letrozole-gonadotropin was associated with one to two fewer oocytes per cycle [14]. Our data did not show a difference in letrozole-gonadotropin or tamoxifen-gonadotropin versus gonadotropin alone, though we may have been underpowered to detect such a difference.
While we highlighted the potential cancer safety benefit of concomitant use of tamoxifen and letrozole in the setting of ER+ disease, our current study is not powered to investigate the long-term impact of their use on cancer outcomes. Prior observational studies have suggested that fertility preservation with concomitant use of letrozole and gonadotropins does not increase the risk of cancer recurrence [5, 15]. It is worth noting that, after the conclusion of this trial, there remains a lack of evidence to support doses of letrozole above 5 mg being able to reliably keep estradiol levels below 500 pg/mL, particularly among women with higher numbers of follicles developing [16, 17].
Well-powered, randomized studies that assess whether tamoxifen or letrozole is associated with differences in long-term cancer or obstetrical outcomes are still needed. Mature oocytes are a proxy measure for the desired outcome of a healthy baby. Outcomes like implantation rate and live birth rate were not a focus of this report but would be of interest to study in the future. Patients undergoing fertility preservation for breast cancer take a median of 5 years to utilize their cryopreserved oocytes and embryos, so such outcomes are unlikely to be available from a randomized trial for some time [18]. In the interim, the choice of tamoxifen-gonadotropin or letrozole-gonadotropin could reasonably be dictated by the following: patient preference regarding side effect profiles, regional practice patterns, simplicity of stimulation protocol, and/or ease or cost of obtaining either medication. In our study, we did not give letrozole or tamoxifen to women with ER− breast cancer, though it is reasonable to do so, as many tumors diagnosed as clinically ER− may still express a small number of estrogen receptors [19].
Increasingly, fertility centers are becoming interested in whether letrozole-gonadotropin might perform better than gonadotropins alone, in the infertility setting [20]. Based on our data, it appears that letrozole-gonadotropin and tamoxifen-gonadotropin are unlikely to have a clinically significant difference in oocyte yield versus gonadotropins alone, at least among patients with breast cancer. There is an ongoing randomized trial of letrozole-gonadotropins versus gonadotropin alone during ovarian stimulation for infertility (NCT02912988), which is expected to provide more robust data about the use of concomitant letrozole (or not) during ovarian stimulation for infertility. Lastly, there may be non-oncologic circumstances in which one might infer a possible clinical benefit of lower estrogen levels, such as in the setting of endometriosis or a history of provoked thromboembolism [21].
Study strengths and limitations
This study has several strengths. The most apparent strength is the randomization between the tamoxifen-gonadotropin and letrozole-gonadotropin groups. We also had a high number of eligible patients enroll in the study, so the results are likely representative of the breadth of patients who would typically undergo ovarian stimulation prior to breast cancer at a fertility clinic. While this study was performed at a university referral center, many of the patients in our study were initially referred from community oncology clinics. We did also have a very low rate of dropout or loss to follow-up in our study. This likely reflects the motivation of patients to complete their fertility preservation cycle prior to cancer treatment, as has been seen in other fertility preservation trials [22].
Our study has some limitations worth noting. As discussed above, we did not study the important outcomes of healthy childbirth or cancer recurrence, though they would be interesting areas of future research. Another limitation is that participants and study physicians were not blinded to the treatment allocation. Given that study physicians are making active decisions about ovarian stimulation dosing adjustments and triggering decisions after allocation is revealed to them, this could be a source of bias. We did use a standard protocol for medication dosing and trigger shot criteria, to help minimize performance bias. In addition, physicians performing the oocyte retrieval reviewed the patient’s chart beforehand (including the estradiol levels), so they could not be adequately blinded. However, we were able to blind our embryologists to study allocation. Another potential limitation is that we did not collect information about cancer predisposition genes, which may affect ovarian reserve [23]. However, our chosen ovarian reserve marker (antral follicle count) was similar between all of the groups in our study. Lastly, we used a dose of tamoxifen (20 mg) that has been used in prior studies to protect the breast from excess estrogen [3]. However, the ovarian stimulation dose of tamoxifen could be considered to be as high as 40 to 60 mg daily, as has been used by Oktay and colleagues [8]. It is possible that a higher dose of concomitant tamoxifen may have led to a higher response with the tamoxifen group.
Conclusion
Letrozole and tamoxifen, the most commonly used additions to attempt to maintain safety in ovarian stimulation for ER+ breast cancer, appear to produce similar mature oocyte yields during ovarian stimulation. Also, though their mechanisms of action would suggest that tamoxifen-gonadotropin and letrozole-gonadotropin may result in differing mature oocyte yields from gonadotropins alone, we saw similar mature oocyte yields in all three approaches in this study.
Data availability
The data from our manuscript have not been deposited in a data repository.
References
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36:1994–2001.
Cakmak H, Katz A, Cedars MI, Rosen MP. Effective method for emergency fertility preservation: random-start controlled ovarian stimulation. Fertil Steril. Elsevier Inc. 2013;100:1673–80.
Meirow D, Raanani H, Maman E, Paluch-Shimon S, Shapira M, Cohen Y, et al. Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril. Elsevier Inc. 2014;102:488–495.e3.
Werner M, Reh A, Labella PA, Noyes N. Laboratory evaluation in oocyte cryopreservation suggests retrieved oocytes are comparable whether frozen for medical indications, deferred reproduction or oocyte donation. J Assist Reprod Genet. 2010;27:613–7.
Letourneau JM, Wald K, Sinha N, Juarez-Hernandez F, Harris E, Cedars MI, et al. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. 2020;126:487–95.
Oktay K, Buyuk E, Davis O, Yermakova I, Veeck L, Rosenwaks Z. Fertility preservation in breast cancer patients: IVF and embryo cryopreservation after ovarian stimulation with tamoxifen. Hum Reprod. 2003;18:90–5.
Oktay K, Hourvitz A, Sahin G, Oktem O, Safro B, Cil A, et al. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006;91:3885–90.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23:4347–53.
Zelinski-Wooten MB, Hess DL, Baughman WL, Molskness TA, Wolf DP, Stouffer RL. Administration of an aromatase inhibitor during the late follicular phase of gonadotropin-treated cycles in rhesus monkeys: effects on follicle development, oocyte maturation, and subsequent luteal function. The Journal of Clinical Endocrinology& Metabolism. 1993;76:988–95.
Legro RS, Brzyski RG, Diamond MP, Coutifaris C, Schlaff WD, Casson P, et al. Letrozole versus clomiphene for infertility in the polycystic ovary syndrome. N Engl J Med. 2014;371:119–29.
Diamond MP, Legro RS, Coutifaris C, Alvero R, Robinson RD, Casson P, et al. Letrozole, gonadotropin, or clomiphene for unexplained infertility. N Engl J Med. 2015;373:1230–40.
Quinn MM, Cakmak H, Letourneau JM, Cedars MI, Rosen MP. Response to ovarian stimulation is not impacted by a breast cancer diagnosis. Hum Reprod. 2017;127:474–7.
Balkenende EME, Dahhan T, Beerendonk CCM, Linn SC, Van W M , Goddijn M Stimulation of the ovaries in women with breast cancer undergoing fertility preservation: alternative versus standard stimulation protocols. American Society of Reproductive Medicine Annual Conference (2019). Philadelphia, PA. Available from: https://www.fertstert.org/article/S0015-0282(19)30797-6/pdf
Revelli A, Porcu E, Setti PEL, Piane LD, Merlo DF, Anserini P. Is letrozole needed for controlled ovarian stimulation in patients with estrogen receptor-positive breast cancer? Gynecol Endocrinol. 2013;29:993–6.
Kim J, Turan V, Oktay K. Long-term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. The Journal of Clinical Endocrinology& Metabolism. 2016;101:1364–71.
Rauch ER, Stubbs R, Christos P, Costantini-Ferrando M, Schattman G. A randomized open label clinical trial of fixed vs. titrated dose letrozole for ovarian stimulation in breast cancer patients: an interim analysis. Fertil Steril. 2012;98:S117.
Quinn M, et al. Titration of letrozole to maintain low estradiol (e2) levels during fertility preservation cycles for estrogen receptor positive (ER+) breast cancer patients does not impact ovarian response or mature oocyte yield. American Society of Reproductive Medicine Annual Conference (2016). Salt Lake City, UT. Available from: https://www.fertstert.org/article/S0015-0282(16)61793-4/pdf
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F. Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. J Clin Oncol. 2015;33:2424–9.
Yi M, Huo L, Koenig KB, Mittendorf EA, Meric-Bernstam F, Kuerer HM, et al. Which threshold for ER positivity? a retrospective study based on 9639 patients. Ann Oncol. 2014;25:1004–11.
Haas J, Bassil R, Meriano J, Samara N, Barzilay E, Gonen N, et al. Does daily co-administration of letrozole and gonadotropins during ovarian stimulation improve IVF outcome? Reprod Biol Endocrinol. 2017;15:70.
Kim SJ, Choo CW, Kim SK, Lee JR, Jee BC, Suh CS, et al. The effects of letrozole on women with endometriosis undergoing ovarian stimulation for in vitro fertilization. Gynecological endocrinology : the official journal of the International Society of Gynecological Endocrinology. 2020;36:257–60.
Moore HCF, Unger JM, Phillips K-A, Boyle F, Hitre E, Porter D, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. New Engl J Medicine. 2015;372:923–32.
Turan V, Bedoschi G, Emirdar V, Moy F, Oktay K. Ovarian stimulation in patients with cancer: impact of Letrozole and BRCA mutations on fertility preservation cycle outcomes. Reprod Sci. 2018;25:26–32.
Acknowledgements
This study was supported by internal departmental research funds.
Code availability
N/A
Funding
This study was supported by departmental research funding within the University of California, San Francisco Department of Obstetrics, Gynecology, and Reproductive Sciences.
Author information
Authors and Affiliations
Contributions
JL’s roles included study design, recruitment, data collection, data analysis, and manuscript writing. F J-H and KW’s roles included recruitment, data collection, and manuscript writing. SR and AW’s roles included data collection and manuscript writing. CM’s roles included data analysis and manuscript writing. EML’s roles included recruitment and manuscript writing. MD’s roles included study design and manuscript writing. AJC’s roles included study design and manuscript writing. MIC’s roles included study design and manuscript writing. MR’s roles included study design, recruitment, data analysis, and manuscript writing.
Corresponding author
Ethics declarations
Ethics approval
All study procedures were approved by the University of California, San Francisco Committee on Human Research. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Letourneau, J., Juarez-Hernandez, F., Wald, K. et al. Concomitant tamoxifen or letrozole for optimal oocyte yield during fertility preservation for breast cancer: the TAmoxifen or Letrozole in Estrogen Sensitive tumors (TALES) randomized clinical trial. J Assist Reprod Genet 38, 2455–2463 (2021). https://doi.org/10.1007/s10815-021-02273-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02273-3