Abstract
Purpose
To assess the effects of letrozole or tamoxifen coadministration on fertility preservation treatment outcomes.
Methods
Retrospective cohort study of 118 breast cancer patients undergoing fertility preservation treatment between 2008 and 2018. Patients who received letrozole (n = 36) or tamoxifen (n = 30) were compared to controls (n = 52) who underwent standard ovarian stimulation protocols. The primary outcome measures included the number of retrieved oocytes, mature oocytes (MII), fertilization, and top-quality embryo rates. The secondary outcome measures included duration of stimulation, gonadotropin dose and peak estradiol level.
Results
The number of oocytes retrieved, MII oocytes, fertilization rate, duration of stimulation, or gonadotropin dose were similar in the letrozole and tamoxifen groups, compared to controls. Top-quality embryo rate was lower in the tamoxifen group compared to controls (25% vs 39.4%, respectively, P = 0.034). The abnormal fertilization rate was higher in the letrozole group compared to controls (7.8% vs 3.60%, respectively, P = 0.015). A stepwise logistic regression analysis revealed that letrozole and peak estradiol were significantly associated with abnormal fertilization (OR 11.94; 95% CI 2.35–60.4, P = 0.003 for letrozole and OR 1.075; 95% CI 1.024–1.12, P = 0.004 per 100 unit change in estradiol).
Conclusions
There may be a negative effect of letrozole or tamoxifen on fertilization and embryo quality, in fertility preservation cycles. Further studies are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignancy in women of reproductive age [1]. Mortality rates have declined since 1990, more prominently in the younger age group, and primarily due to early detection and widespread application of adjuvant chemotherapy and endocrine therapies [2, 3]. Nevertheless, the gonadotoxic damage of chemotherapeutic agents and their detrimental effect on the ovarian reserve persists as a major concern, resulting in a large proportion of breast cancer patients of reproductive age facing future infertility [4, 5]. The most notorious and commonly used chemotherapies are the cyclophosphamide-based regimens, taxane-based regimens, and anthracycline/epirubicin-based regimens, were all shown to cause the highest rate of chemotherapy induced amenorrhea (CIA) [6, 7].
Ovarian stimulation for oocyte or embryo cryopreservation is currently the preferred and most established method for fertility preservation in breast cancer patients [8,9,10,11]. The main concern with controlled ovarian hyperstimulation (COH) in these patients is the secretion of supraphysiologic serum estrogen levels that might be as high as 10-fold greater than that of a natural cycle [12, 13]. The association between breast cancer cells proliferation and accelerated cancer aggressiveness in women with estrogen receptor positive tumors, is not clear [14,15,16]. In aim of reducing exposure to potentially harmful estradiol (E2) levels, modifications to COH protocols were developed, incorporating either selective estrogen receptor modulators (SERMS, most commonly, tamoxifen) or an aromatase inhibitor (letrozole) [17, 18].
Tamoxifen, a nonsteroidal triphenylethylene antiestrogen, competes with estrogen for binding sites in the estrogen receptor (ER) in target tissues, such as breast cancer cells. Tamoxifen was first used as an ovulation-induction agent [19] and later for breast cancer treatment and prophylaxis [20,21,22]. Given as adjuvant therapy, it effectively reduces breast cancer recurrence and improves long-term survival in premenopausal patients with an ER-positive tumor [23]. Oktay et al. [17] were the first to describe a protocol for breast cancer patients which combines its two properties as an ovarian stimulator and an antineoplastic agent; they also showed the feasibility of using tamoxifen in combination with FSH to cryopreserve more oocytes or embryos [18].
Letrozole is a third-generation aromatase inhibitor. It is potent and highly selective, and competitively binds to the active site of the enzyme. Letrozole significantly reduces plasma estrogen levels [24, 25]. Given as first-line endocrine therapy, it is superior to tamoxifen for advanced-stage postmenopausal breast cancer [26, 27]. It is also used off-label as an ovulation-induction agent in the treatment of patients with anovulatory infertility [28, 29]. It reduces peak E2 serum levels when used in COH cycles, levels of 381–829 pg/ml were reportedly attained when letrozole was initiated on days 2–3 of cycle, compared to 1464–1744 pg/ml in cycles without letrozole [9, 30,31,32].
To date, only a few studies examined the effect of these agents on fertility preservation treatment. The objective of this study is to explore the effect of the coadministration of letrozole or tamoxifen with a standard stimulation protocol on treatment outcomes, specifically, the number and quality of oocytes and embryos.
Materials and methods
Study population
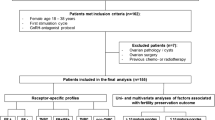
This is a retrospective cohort study. All patients were recruited from the reproductive center of a university-affiliated medical center. We searched the medical records of women undergoing medical fertility preservation treatment in the IVF Unit of Lis Maternity Hospital between 2008 and 2018. The inclusion criteria were a histologically confirmed diagnosis of breast cancer or being a carrier of the BRCA1 or the BRCA 2 gene. The exclusion criteria were age younger than 18 years or older than 42 years, having undergone chemotherapy or pelvic radiation, or a history of ovarian surgery with a possible effect on the ovarian reserve.
Patient data cycle parameters
Patient demographics, baseline hormonal profile, cycle parameters, and embryo status were retrieved from our electronic database. Treatment outcomes (the number of retrieved oocytes, the number of mature oocytes [MII], and the fertilization and top-quality embryo rates) were compared between the patients that received standard protocol for controlled ovarian stimulations (controls) and those of the two study groups, one comprised of women who received letrozole 5 mg (letrozole group) and those who received 20 mg of tamoxifen (tamoxifen group), each in addition to a standard stimulation protocol. The choice of fertility preservation protocol was based on the receptor status of the tumor and treating physician choice in accordance with patient preference. Letrozole has been administered in fertility preservation cycles in our IVF unit since 2012.
Controlled ovarian hyperstimulation and oocyte or embryo cryopreservation
COH was performed by means of one of the three standard protocols: (i) short gonadotropin-releasing hormone (GnRH) agonist, (ii) fixed GnRH antagonist, and (iii) midluteal long GnRH agonist. Patients were treated with 5 mg of an aromatase inhibitor daily (Letrozole, Femara, Novartis, NJ, USA) [16] or tamoxifen 20 mg/day starting on day one of stimulation [33, 34]. As per our center’s protocol for women with breast cancer, FSH was administered at a starting dose of 225 IU/D and a maximal dose of 450 IU/D. Ovulation was triggered by 250 mg of human recombinant chorionic gonadotropin (hCG) 250 mg (Choriogonadotropin alfa, Ovitrelle, Merck Serono Italy) or 0.2 mg of a GnRH agonist (Triptorelin, Ferring Pharmaceuticals Switzerland) when at least two follicles reached a mean diameter of 17 mm. Oocyte retrieval by an ultrasound-guided transvaginal approach was scheduled to take place 36–38 h later, and the patients were offered oocyte or embryo cryopreservation according to the couple’s status and preferences. Carriers of BRCA 1/2 were offered intracytoplasmic sperm injection (ICSI) to allow future pregestational diagnosis (PGD). It has been common practice in our IVF unit since 2012 to perform ICSI for all fertility preservation cancer patients in order to allow the possibility for future PGD [35]. For ICSI cycles, cumulus stripping was performed 2–3 h after oocyte retrieval in order to examine oocyte maturation. Metaphase II (MII) oocytes were vitrified or inseminated by ICSI. Oocyte–cumulus complexes of women undergoing IVF cycles were inseminated with 100,000/ml motile spermatozoa per insemination dish that contained 3–5 oocytes. Fertilization was confirmed 16–18 h after insemination by the appearance of two distinct pronuclei (2PN) and two polar bodies. Oocytes were cryopreserved by vitrification; embryos were cryopreserved by slow freezing on day 2 or 3 until 2013 and by vitrification after that. Embryos were graded according to the Society for Assisted Reproductive Technology (SART) classification. Top-quality embryos were defined as having four symmetrical cells at day 2 or 8 symmetrical cells at day three, and fragmentation of 0–10% [36, 37].
Statistical analysis
We used the Shapiro–Wilk test to evaluate data distribution. A parametric test was used for normally distributed data and a nonparametric test (Wilcoxon test) for skewed data. Categorical variables were compared using Fisher’s exact test when appropriate. Descriptive statistics were given as median (interquartile range, IQR) for skewed data or mean ± standard deviation (SD). Due to the small sample size, cycles with coadministration of letrozole or tamoxifen were compared to the controls. However, since the data on the effects of tamoxifen versus letrozole is very limited, the differences in cycle outcomes between these cycles were also analyzed and are presented in the supplementary material. Based on the results of the univariate analysis, we searched for parameters that were independently associated with abnormal fertilization for which we applied a stepwise multiple logistic regression model adjusted for age, IVF/ICSI, duration of stimulation, administration of letrozole or tamoxifen, and total gonadotropins dose. A P value < 0.05 was considered significant. All statistical analyses were performed with JMP 14 for Macintosh.
Results
The final analysis included the records of 118 breast cancer patients undergoing COH for fertility preservation between 2008 and 2018. Thirty-six patients received letrozole (letrozole group), and 30 received tamoxifen (tamoxifen group) in addition to the stimulation protocol. The remaining 52 patients undergoing COH without coadministration of letrozole or tamoxifen comprised the control group. Amongst the control group, 4 patients were healthy BRCA carrier patients undergoing fertility preservation treatment. For most cancer patients, BRCA carrier status was unknown since they were referred for an urgent fertility preservation cycle. The mean ages of the patients in the study and control groups were similar, and the other patient demographics and stimulation protocol parameters are presented in Table 1.
A subgroup analysis for 2012–2018 (when letrozole and PGD were routinely implemented in our IVF unit) revealed that the ICSI rate was comparable for the letrozole and control groups (96% and 95%, respectively, P = 1). A GnRH agonist trigger was more commonly used in the letrozole group (86%) compared to the control and tamoxifen groups (33%) (P < 0.001) (Table 1).
GnRH antagonist protocol was most frequently used in all 3 study groups, due to the very small number of cycles with GnRH agonist downregulation a statistical analysis could not be applied. Nevertheless, cycle parameters including the number of oocytes retrieved and mature oocyte rate were calculated and were found to be within the range of the group. There were no differences in the number of retrieved oocytes, the number of mature oocytes (MII), and the fertilization rates between the letrozole and tamoxifen groups compared to the controls (Table 2). However, the rate of top-quality embryos was lower in the tamoxifen group compared to the controls (25% vs 39.4%, respectively, P = 0.034), but not in the letrozole group compared to the controls (37.9% vs 39.4%, respectively, P = 0.808).
The duration of stimulation and the total amount of gonadotropin were comparable between the groups (Table 2). The rate of abnormal fertilization (1PN/3PN) was significantly higher in the letrozole group (7.8% vs 3.60% for the letrozole vs controls, P = 0.015). These results were further supported by a subgroup analysis of ICSI cycles, which yielded similar high rates of abnormal fertilization (1PN/3PN) in the letrozole group compared to the controls (7.7% vs 2.5%, respectively, P = 0.009). Additionally, the rates of abnormal fertilization were higher in the letrozole group compared to the controls when cycles with GnRH analog triggering were analyzed separately (8.4% vs 2.3%, respectively, P = 0.003). Cycles with coadministration of tamoxifen had a significantly lower rate of top-quality embryos with similar abnormal fertilization rate when compared to the letrozole group (Supplemental table I).
A stepwise logistic regression analysis adjusted for cycle parameters (i.e., letrozole, tamoxifen, maximal E2, duration of stimulation, maximal gonadotropin dose, IVF, ICSI, GnRH agonist trigger) revealed that letrozole and maximal E2 were the only parameters significantly associated with abnormal fertilization (Table 3).
Discussion
Our study aimed to explore the possible adverse effects of coadministration of tamoxifen or letrozole with a standard stimulation protocol on the outcomes of fertility preservation treatment among women who had a histologically confirmed diagnosis of breast cancer or were carriers of the BRCA1 or the BRCA2 gene. No differences were found in oocyte yield, fertilization rate, or the number of cryopreserved oocytes and embryos when either the aromatase inhibitor or the selective estrogen receptor modulator was added. However, the rate of top-quality embryos was lower in cycles that included the coadministration of tamoxifen, and the rate of abnormal fertilization was higher in cycles that included the coadministration of letrozole.
In this study, the numbers of oocytes retrieved and frozen embryos in cycles with coadministration of letrozole, tamoxifen, or controls are comparable to previous reports in breast cancer patients (on average 8–16 oocytes collected and 5–6 cryopreserved embryos) [9, 16, 18, 32, 33, 38, 39]. Furthermore, cycle outcomes in the controls, who had undergone conventional COH cycle, were similar to the control group in other studies who underwent IVF for noncancer indication [30]. Whether or not letrozole negatively effects oocyte yield remains a matter of controversy in the literature, with some in agreement with those of the current study by not detecting any differences in total or mature oocyte yield [31, 40], and others showing a small but statistically significant decrease in mature oocyte yield [30, 32, 41]. A recent metaanalysis by Bonardi et al. [42] showed that the addition of letrozole does not have a negative effect on the number of mature oocytes collected nor on other cycle parameters including maturation and fertilization rates, total gonadotropin dose, and the length of the stimulation. A secondary analysis including breast cancer patients only reached similar results [42].
According to our knowledge, this is the first report showing negative effect of letrozole and tamoxifen on fertilization and top-quality embryo rate.
The median total FSH dose in this cohort was higher than previously reported [30, 32, 43]; this can result from a higher FSH starting dose and longer stimulation. It was previously reported that the ovarian stimulation phase lasts 9 to 12 days; the median duration found in this study is within the upper limits of this range [9, 30, 32, 43]. Estradiol level as expected in women who received tamoxifen was comparable to controls and higher than in women with letrozole. Estradiol levels in the tamoxifen group was in accordance with the study of Meirow et al. [33]; however, others reported lower mean E2 that can be explained by a different stimulation protocol [17, 18].
It has been suggested that BRCA mutation may reduce the reproductive performance in women carriers. Animal models showed accelerated follicle loss and reduced ovarian reserve [44]; these findings were supported by lower AMH levels in carriers of BRCA1 mutation and earlier age of menopause [45,46,47,48,49]. Though differences in the outcomes of fertility preservation cycles may be affected by the BRCA carrier status, the negative effects of BRCA mutation on ovarian aging are still debatable [50, 51]. It was first reported by Shapira et al. [52] that BRCA carriers had comparable ovarian reserve and response to stimulation, compared to noncarriers [52, 53]. Comparable results were demonstrated not only for healthy carriers but for cancer patients as well [46].
ICSI and GnRH agonist triggering were used more frequently in our letrozole group. Both the routine implementation of letrozole in our IVF unit for fertility preservation cycles in breast cancer patients and the routine practice of ICSI to allow future PGD for women found to be carriers of a mutation causing familial cancer were initiated in 2012. Nevertheless, the results were similar when ICSI cycles and GnRH agonist trigger were analyzed separately. Furthermore, a stepwise logistic regression analysis adjusted for cycle parameters, including ICSI and trigger used, found that letrozole and higher maximal E2 were the only significant parameters that negatively affected fertilization.
We hypothesized that the lower rate of top-quality embryos associated with tamoxifen and the high rate of abnormal fertilization rate associated with letrozole in our study may be explained by interference in follicular hormonal balance caused by these agents. This theory has some basis in the results of animal model studies. Moor et al. (1980) altered follicular steroid secretion in bovine oocytes by using enzyme inhibitors and exogenous steroid supplementation and found these alterations were associated with fertilization abnormalities [54]. They observed that inhibiting steroidogenesis by adding the aromatase inhibitor, aminoglutethimide, hindered normal pronuclear development. Moreover, higher percentages of oocytes were penetrated by more than one spermatozoon, and the development of the male pronuclei was abnormal as well. In a study on rats, tamoxifen enhanced follicle-stimulating hormone (FSH)–stimulated aromatase activity in granulosa cells, causing increased follicular estrogen levels. It also inhibited FSH-stimulated production of progesterone and 20α-hydroxy-4-pregnen-3-one [55]. Tamoxifen also prevented the induction of luteinizing hormone receptors in granulosa cells [56]. Letrozole caused a significant increase in testosterone and androstenedione and also increased luteinizing hormone plasma levels and the expression of Cyp17a1 mRNA, a key enzyme in the regulation of androgen biosynthesis [57]. The effects of letrozole on embryo quality were described in a number of studies by Lossl et al. [5859]. In the first report from this group, the short-term use of an aromatase inhibitor and hCG prior to COH increased local and intraovarian levels of androgens with higher numbers of good-quality embryos [58]. In a later work, the same group failed to demonstrate that the administration of an aromatase inhibitor and hCG before controlled ovarian stimulation for IVF/ICSI improved the number of top-quality embryos [59]. To the best of our knowledge, no studies have examined either embryo quality or the rate of abnormal fertilization associated with the coadministration of tamoxifen with a standard stimulation protocol.
The main limitation of our study is in its retrospective nature, small numbers and heterogeneity of the stimulation protocols. There is very limited data comparing coadministration of letrozole to tamoxifen in fertility preservation cycles; however, a model analyzing the differences among the 3 groups would lack statistical power to determine such a difference. These results are presented in the supplementary material and future studies are required to confirm these findings. Furthermore, we did not have baseline parameters of ovarian reserve, such as day 3 follicle-stimulating hormone, since most of the study patients were referred for emergency fertility preservation. In addition, antiMüllerian hormone values could not be analyzed since they are not part of the routine tests covered by our national healthcare. The strengths of this study are that our control group included exclusively breast cancer patients, unlike other studies in which the controls included women with noncancer-related indication for IVF or other cancer types, thus eliminating a possible bias of the systemic effects of different cancer types [41]. Finally, previous studies did not examine embryo quality or abnormal fertilization rates.
In conclusion, coadministration of tamoxifen or letrozole with a standard stimulation protocol did not affect oocyte and embryo yield. However, tamoxifen was associated with lower rates of top-quality embryos, and letrozole was associated with higher rates of abnormal fertilization. These findings should be viewed cautiously when implicated in clinical practice, due to the relatively small study groups. Further studies are needed in order to clarify these effects on treatment outcomes.
Data availability
Not applicable.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. https://doi.org/10.3322/caac.21551.
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353(17):1784–92. https://doi.org/10.1056/NEJMoa050518.
DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64(1):52–62. https://doi.org/10.3322/caac.21203.
Bines J, Oleske DM, Cobleigh MA. Ovarian function in premenopausal women treated with adjuvant chemotherapy for breast cancer. J Clin Oncol. 1996;14(5):1718–29. https://doi.org/10.1200/JCO.1996.14.5.1718.
Byrne J, Fears TR, Gail MH, Pee D, Connelly RR, Austin DF, et al. Early menopause in long-term survivors of cancer during adolescence. Am J Obstet Gynecol. 1992;166(3):788–93. https://doi.org/10.1016/0002-9378(92)91335-8.
Zhao J, Liu J, Chen K, Li S, Wang Y, Yang Y, et al. What lies behind chemotherapy-induced amenorrhea for breast cancer patients: a meta-analysis. Breast Cancer Res Treat. 2014;145(1):113–28. https://doi.org/10.1007/s10549-014-2914-x.
Lambertini M, Campbell C, Bines J, Korde LA, Izquierdo M, Fumagalli D, et al. Adjuvant anti-HER2 therapy, treatment-related amenorrhea, and survival in premenopausal HER2-positive early breast cancer patients. J Natl Cancer Inst. 2019;111(1):86–94. https://doi.org/10.1093/jnci/djy094.
Kasum M, von Wolff M, Franulic D, Cehic E, Klepac-Pulanic T, Oreskovic S, et al. Fertility preservation options in breast cancer patients. Gynecol Endocrinol : the official journal of the International Society of Gynecological Endocrinology. 2015;31(11):846–51. https://doi.org/10.3109/09513590.2015.1081684.
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, et al. Fertility preservation in patients with cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol. 2018 Jul 1;36(19):1994–2001. https://doi.org/10.1200/JCO.2018.78.1914.
Paluch-Shimon S, Cardoso F, Partridge AH, Abulkhair O, Azim HA Jr, Bianchi-Micheli G, et al. ESO-ESMO 4th international consensus guidelines for breast cancer in young women (BCY4). Ann Oncol. 2020;31:674–96. https://doi.org/10.1016/j.annonc.2020.03.284.
Lambertini M, Peccatori FA, Demeestere I, Amant F, Wyns C, Stukenborg JB, et al. Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2020;31:1664–78. https://doi.org/10.1016/j.annonc.2020.09.006.
Pena JE, Chang PL, Chan LK, Zeitoun K, Thornton MH 2nd, Sauer MV. Supraphysiological estradiol levels do not affect oocyte and embryo quality in oocyte donation cycles. Hum Reprod. 2002;17(1):83–7. https://doi.org/10.1093/humrep/17.1.83.
Pittaway DE, Wentz AC. Evaluation of the exponential rise of serum estradiol concentrations in human menopausal gonadotropin-induced cycles. Fertil Steril. 1983;40(6):763–7. https://doi.org/10.1016/s0015-0282(16)47476-5.
Endogenous H, Breast Cancer Collaborative G, Key TJ, Appleby PN, Reeves GK, Travis RC, et al. Sex hormones and risk of breast cancer in premenopausal women: a collaborative reanalysis of individual participant data from seven prospective studies. Lancet Oncol. 2013;14(10):1009–19. https://doi.org/10.1016/S1470-2045(13)70301-2.
Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354(3):270–82. https://doi.org/10.1056/NEJMra050776.
Kim J, Turan V, Oktay K. Long-term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab. 2016;101(4):1364–71. https://doi.org/10.1210/jc.2015-3878.
Oktay K, Buyuk E, Davis O, Yermakova I, Veeck L, Rosenwaks Z. Fertility preservation in breast cancer patients: IVF and embryo cryopreservation after ovarian stimulation with tamoxifen. Hum Reprod. 2003;18(1):90–5. https://doi.org/10.1093/humrep/deg045.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–53. https://doi.org/10.1200/JCO.2005.05.037.
Klopper A, Hall M. New synthetic agent for the induction of ovulation: preliminary trials in women. Br Med J. 1971;1(5741):152–4. https://doi.org/10.1136/bmj.1.5741.152.
Early Breast Cancer Trialists’ Collaborative Group. Systemic treatment of early breast cancer by hormonal, cytotoxic, or immune therapy. 133 randomised trials involving 31,000 recurrences and 24,000 deaths among 75,000 women. Early Breast Cancer Trialists' Collaborative Group. Lancet. 1992;339(8784):1–15.
Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90(18):1371–88. https://doi.org/10.1093/jnci/90.18.1371.
Prichard RS, Hill AD, Dijkstra B, McDermott EW, O'Higgins NJ. The prevention of breast cancer. Br J Surg. 2003;90(7):772–83. https://doi.org/10.1002/bjs.4218.
Ekholm M, Bendahl PO, Ferno M, Nordenskjold B, Stal O, Ryden L. Two years of adjuvant tamoxifen provides a survival benefit compared with no systemic treatment in premenopausal patients with primary breast cancer: long-term follow-up (> 25 years) of the phase III SBII:2pre trial. J Clin Oncol. 2016;34(19):2232–8. https://doi.org/10.1200/JCO.2015.65.6272.
Santen RJ. Recent progress in development of aromatase inhibitors. J Steroid Biochem Mol Biol. 1990;37(6):1029–35.
Pfister CU, Martoni A, Zamagni C, Lelli G, De Braud F, Souppart C, et al. Effect of age and single versus multiple dose pharmacokinetics of letrozole (Femara) in breast cancer patients. Biopharm Drug Dispos. 2001;22(5):191–7.
Mouridsen H, Gershanovich M, Sun Y, Perez-Carrion R, Boni C, Monnier A, et al. Phase III study of letrozole versus tamoxifen as first-line therapy of advanced breast cancer in postmenopausal women: analysis of survival and update of efficacy from the International Letrozole Breast Cancer Group. J Clin Oncol. 2003;21(11):2101–9. https://doi.org/10.1200/JCO.2003.04.194.
Breast International Group 1-98 Collaborative G, Thurlimann B, Keshaviah A, Coates AS, Mouridsen H, Mauriac L, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med. 2005;353(26):2747–57. https://doi.org/10.1056/NEJMoa052258.
Casper RF, Mitwally MF. A historical perspective of aromatase inhibitors for ovulation induction. Fertil Steril. 2012;98(6):1352–5. https://doi.org/10.1016/j.fertnstert.2012.10.008.
Mitwally MF, Casper RF. Use of an aromatase inhibitor for induction of ovulation in patients with an inadequate response to clomiphene citrate. Fertil Steril. 2001;75(2):305–9. https://doi.org/10.1016/s0015-0282(00)01705-2.
Domingo J, Guillen V, Ayllon Y, Martinez M, Munoz E, Pellicer A, et al. Ovarian response to controlled ovarian hyperstimulation in cancer patients is diminished even before oncological treatment. Fertil Steril. 2012;97(4):930–4. https://doi.org/10.1016/j.fertnstert.2012.01.093.
Checa Vizcaino MA, Corchado AR, Cuadri ME, Comadran MG, Brassesco M, Carreras R. The effects of letrozole on ovarian stimulation for fertility preservation in cancer-affected women. Reprod BioMed Online. 2012;24(6):606–10. https://doi.org/10.1016/j.rbmo.2012.02.020.
Revelli A, Porcu E, Levi Setti PE, Delle Piane L, Merlo DF, Anserini P. Is letrozole needed for controlled ovarian stimulation in patients with estrogen receptor-positive breast cancer? Gynecol Endocrinol : the official journal of the International Society of Gynecological Endocrinology. 2013;29(11):993–6. https://doi.org/10.3109/09513590.2013.819083.
Meirow D, Raanani H, Maman E, Paluch-Shimon S, Shapira M, Cohen Y, et al. Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril. 2014;102(2):488–95 e3. https://doi.org/10.1016/j.fertnstert.2014.05.017.
Practice Committee of the American Society for Reproductive Medicine. Electronic address aao. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112(6):1022–33. https://doi.org/10.1016/j.fertnstert.2019.09.013.
Practice Committees of the American Society for Reproductive M, Society for Assisted Reproductive T. Intracytoplasmic sperm injection (ICSI) for non-male factor infertility: a committee opinion. Fertil Steril. 2012;98(6):1395–9. https://doi.org/10.1016/j.fertnstert.2012.08.026.
Racowsky C, Vernon M, Mayer J, Ball GD, Behr B, Pomeroy KO, et al. Standardization of grading embryo morphology. Fertil Steril. 2010;94(3):1152–3. https://doi.org/10.1016/j.fertnstert.2010.05.042.
Racowsky C, Ohno-Machado L, Kim J, Biggers JD. Is there an advantage in scoring early embryos on more than one day? Hum Reprod. 2009;24(9):2104–13. https://doi.org/10.1093/humrep/dep198.
Rodgers RJ, Reid GD, Koch J, Deans R, Ledger WL, Friedlander M, et al. The safety and efficacy of controlled ovarian hyperstimulation for fertility preservation in women with early breast cancer: a systematic review. Hum Reprod. 2017;32(5):1033–45. https://doi.org/10.1093/humrep/dex027.
Oktay K, Turkcuoglu I, Rodriguez-Wallberg KA. GnRH agonist trigger for women with breast cancer undergoing fertility preservation by aromatase inhibitor/FSH stimulation. Reprod BioMed Online. 2010;20(6):783–8. https://doi.org/10.1016/j.rbmo.2010.03.004.
Ben-Haroush A, Wertheimer A, Klochendler E, Sapir O, Shufaro Y, Oron G. Effect of letrozole added to gonadotropins in controlled ovarian stimulation protocols on the yield and maturity of retrieved oocytes. Gynecol Endocrinol: the official journal of the International Society of Gynecological Endocrinology. 2019;35(4):324–7. https://doi.org/10.1080/09513590.2018.1534950.
Cobo A, Garcia-Velasco J, Domingo J, Pellicer A, Remohi J. Elective and Onco-fertility preservation: factors related to IVF outcomes. Hum Reprod. 2018;33(12):2222–31. https://doi.org/10.1093/humrep/dey321.
Bonardi B, Massarotti C, Bruzzone M, Goldrat O, Mangili G, Anserini P, et al. Efficacy and safety of controlled ovarian stimulation with or without letrozole co-administration for fertility preservation: a systematic review and meta-analysis. Front Oncol. 2020;10:574669. https://doi.org/10.3389/fonc.2020.574669.
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100(6):1681–5 e1. https://doi.org/10.1016/j.fertnstert.2013.08.030.
Titus S, Li F, Stobezki R, Akula K, Unsal E, Jeong K, et al. Impairment of BRCA1-related DNA double-strand break repair leads to ovarian aging in mice and humans. Sci Transl Med. 2013;5(172):172ra21. https://doi.org/10.1126/scitranslmed.3004925.
Phillips KA, Collins IM, Milne RL, McLachlan SA, Friedlander M, Hickey M, et al. Anti-Mullerian hormone serum concentrations of women with germline BRCA1 or BRCA2 mutations. Hum Reprod. 2016;31(5):1126–32. https://doi.org/10.1093/humrep/dew044.
Lin WT, Beattie M, Chen LM, Oktay K, Crawford SL, Gold EB, et al. Comparison of age at natural menopause in BRCA1/2 mutation carriers with a non-clinic-based sample of women in northern California. Cancer. 2013;119(9):1652–9. https://doi.org/10.1002/cncr.27952.
Finch A, Valentini A, Greenblatt E, Lynch HT, Ghadirian P, Armel S, et al. Frequency of premature menopause in women who carry a BRCA1 or BRCA2 mutation. Fertil Steril. 2013;99(6):1724–8. https://doi.org/10.1016/j.fertnstert.2013.01.109.
Son KA, Lee DY, Choi D. Association of BRCA mutations and anti-Mullerian hormone level in young breast cancer patients. Front Endocrinol (Lausanne). 2019;10:235. https://doi.org/10.3389/fendo.2019.00235.
Porcu E, Cillo GM, Cipriani L, Sacilotto F, Notarangelo L, Damiano G, et al. Impact of BRCA1 and BRCA2 mutations on ovarian reserve and fertility preservation outcomes in young women with breast cancer. J Assist Reprod Genet. 2020;37(3):709–15. https://doi.org/10.1007/s10815-019-01658-9.
Lambertini M, Goldrat O, Toss A, Azim HA Jr, Peccatori FA, Ignatiadis M, et al. Fertility and pregnancy issues in BRCA-mutated breast cancer patients. Cancer Treat Rev. 2017;59:61–70. https://doi.org/10.1016/j.ctrv.2017.07.001.
Peccatori FA, Mangili G, Bergamini A, Filippi F, Martinelli F, Ferrari F, et al. Fertility preservation in women harboring deleterious BRCA mutations: ready for prime time? Hum Reprod. 2018;33(2):181–7. https://doi.org/10.1093/humrep/dex356.
Shapira M, Raanani H, Feldman B, Srebnik N, Dereck-Haim S, Manela D, et al. BRCA mutation carriers show normal ovarian response in in vitro fertilization cycles. Fertil Steril. 2015;104(5):1162–7. https://doi.org/10.1016/j.fertnstert.2015.07.1162.
Gunnala V, Fields J, Irani M, D’Angelo D, Xu K, Schattman G, et al. BRCA carriers have similar reproductive potential at baseline to noncarriers: comparisons in cancer and cancer-free cohorts undergoing fertility preservation. Fertil Steril. 2019;111(2):363–71. https://doi.org/10.1016/j.fertnstert.2018.10.014.
Moor RM, Polge C, Willadsen SM. Effect of follicular steroids on the maturation and fertilization of mammalian oocytes. J Embryol Exp Morphol. 1980;56:319-335.
Welsh TH Jr, Jia XC, Jones PB, Zhuang LZ, Hsueh AJ. Disparate effects of triphenylethylene antiestrogens on estrogen and progestin biosyntheses by cultured rat granulosa cells. Endocrinology. 1984;115(4):1275–82. https://doi.org/10.1210/endo-115-4-1275.
Knecht M, Tsai-Morris CH, Catt KJ. Estrogen dependence of luteinizing hormone receptor expression in cultured rat granulosa cells. Inhibition of granulosa cell development by the antiestrogens tamoxifen and keoxifene. Endocrinology. 1985;116(5):1771–7. https://doi.org/10.1210/endo-116-5-1771.
Ortega I, Sokalska A, Villanueva JA, Cress AB, Wong DH, Stener-Victorin E, et al. Letrozole increases ovarian growth and Cyp17a1 gene expression in the rat ovary. Fertil Steril. 2013;99(3):889–96. https://doi.org/10.1016/j.fertnstert.2012.11.006.
Lossl K, Andersen AN, Loft A, Freiesleben NL, Bangsboll S, Andersen CY. Androgen priming using aromatase inhibitor and hCG during early-follicular-phase GnRH antagonist down-regulation in modified antagonist protocols. Hum Reprod. 2006;21(10):2593–600. https://doi.org/10.1093/humrep/del221.
Lossl K, Andersen CY, Loft A, Freiesleben NL, Bangsboll S, Andersen AN. Short-term androgen priming by use of aromatase inhibitor and hCG before controlled ovarian stimulation for IVF. A randomized controlled trial. Hum Reprod. 2008;23(8):1820–9. https://doi.org/10.1093/humrep/den131.
Acknowledgments
The authors thank the staff members of the IVF Laboratory at the Tel Aviv Sourasky Medical center for their guidance and assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
(IRB) 0695-17TLV of the Tel Aviv Medical Center.
Consent to participate
Not applicable
Consent for publication
Not applicable
Code availability (software application or custom code)
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Shulman, Y., Almog, B., Kalma, Y. et al. Effects of letrozole or tamoxifen coadministered with a standard stimulation protocol on fertility preservation among breast cancer patients. J Assist Reprod Genet 38, 743–750 (2021). https://doi.org/10.1007/s10815-020-02030-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-02030-y