Abstract
Purpose
The purpose of our study was to determine if progesterone (P4) values on day of trigger affect certain cycle outcome parameters, ploidy status of embryos, as well as pregnancy outcomes in the subsequent first frozen embryo transfer cycle.
Methods
Two hundred thirty-eight patients undergoing pre-gestational screening and freeze all protocol at our fertility center from 2013 to 2014 were included. Excluded patients were those whom had cancelled cycles prior to egg retrieval as well as cycles utilizing donor eggs. Once patients were identified as eligible for this study, frozen serum from the day of trigger was identified and analyzed using the Siemens Immulite 2000. Number of eggs retrieved, number of available embryos for biopsy, and number of euploid/aneuploid embryos were analyzed. The first frozen embryo transfer cycle was linked to the initial egg retrieval and outcomes including pregnancy rates, and live birth/ongoing pregnancy rates were calculated and analyzed. A discriminatory P4 value of 1.5 ng/ml was set. Group A had P4 values of less than 1.5 ng/ml and group B had P4 values greater than or equal to 1.5 ng/ml. T tests and chi-squared tests were used for statistical analysis.
Results
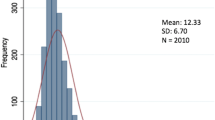
Group A had an average trigger P4 value of 0.87 +/− 0.3 and group B had an average trigger P4 of 2.1 +/− 0.8. Table 1 shows the baseline characteristics of both group A and group B. The only significant difference between the two groups was total gonadotropin dosage (IU) with a p value of 0.02 and estradiol (pg/ml) at trigger, also with a p value of 0.02 (Table 1). Number of eggs retrieved, number of embryos biopsied, number euploid/aneuploid, and non-diagnosis embryos were all non-significant. Chi-square analysis was used to compare pregnancy rates between the two groups after the first frozen embryo transfer cycle. Group A had a pregnancy rate of 72 % and Group B had a pregnancy rate of 66.7 %, which was not significant. Ongoing pregnancy/live birth rates were 65.6 % in group A and 66.67 % in group B, also not significant (Table 2).
Conclusions
P4 values on day of trigger do not affect number of eggs retrieved and number of chromosomally normal embryos available for transfer in a subsequent embryo transfer cycle. Elevated P4 values (≥1.5 ng/ml) also do not affect pregnancy rates or live birth/ongoing pregnancy rates in the first subsequent frozen embryo transfer cycle.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During controlled ovarian hyperstimulation (COH), premature luteinization (and resultant elevation in serum progesterone (P4) levels is associated with elevated estrogen levels and premature luteinizing hormone (LH) surge [1]. Premature luteinization and eventual ovulation is prevented by suppression of LH secretion with a gonadotropin releasing hormone (GnRH) analogue or antagonist. Despite the use of GnRH analogues/antagonists, a subtle rise in serum P4 levels is observed in a subgroup of women at the end of the stimulation cycle. This phenomenon has been reported with an incidence ranging from 12.3 to 46.7 % of cycles [2]. In many instances, the increase of P4 levels leads to cancellation of the in vitro fertilization (IVF) cycle [3, 4].
Since the introduction of GnRH analogues/antagonists into ART cycles, the phenomenon of elevated day-of-trigger P4 levels has been controversial [5]. Both the significance and the etiology of this phenomenon remain under debate. Many investigators have found that elevated P4 on day of human chorionic gonadotropin (HCG) trigger adversely affects pregnancy rates [2–4, 6–15]. Others have not found a correlation between P4 and pregnancy rates [16–21]. Still others have found a mixed [21, 22] or favorable effect [23, 24] on ART outcome for specific populations. Nonetheless, a recent meta-analysis of 63 studies involving over 60,000 cycles concluded that elevated P4 on day of HCG trigger lowers the pregnancy rate in fresh, but not frozen embryo transfers (FET) [2].
The current literature states that mildly elevated P4 on day of HCG trigger is likely due to embryo-uterine asynchrony. We agree that this is the likely cause of the decrease in fresh IVF success rates we are observing in these instances. However, there is controversy in the literature that premature luteinization affects the quality of the egg. For example, P4 level has also been associated with poor meiosis in animal studies [25]. Studies before the use of GnRH analogues linked elevated P4 to poor oocyte maturation, lower oocyte recovery, fertilization, and reduced embryo quality [26–28]. However, the more recent studies have linked the phenomenon to endometrial receptivity or endometrial asynchrony, and this manuscript will attempt to prove this theory [21, 22, 29–31].
Pre-implantation genetic screening (PGS) cycles offer a unique opportunity to investigate this mechanism. PGS was developed to assess the chromosomal status of embryos created through in vitro fertilization. It has been shown to be a sensitive analysis for ploidy, [32] and a mechanism to improve live births and decrease spontaneous abortions in IVF cycles [33, 34]. In nearly all cases, it is followed by cryopreservation of the embryo and transfer of a single euploid embryo in a subsequent programmed cycle [35]. The ultimate goal of an IVF cycle is the live birth of a singleton. If it is true that elevated P4 (premature luteinization) during a stimulation cycle affects egg quality, then we should see a drop in the amount of euploid embryos available for transfer in this subgroup of patients. We intend to prove this is not the case.
Methods
A retrospective chart review was conducted on all embryo transfers derived from PGS in the calendar years 2013 to 2014. Inclusion criteria included patients that underwent egg retrieval with subsequent day 5/6 embryo biopsy (at least a stage 3 blastocyst), cryopreservation, and transfer in a FET cycle. Only the first subsequent frozen embryo transfer cycle was considered. Positive outcomes that were considered include clinical pregnancy rate and ongoing/live birth rate. Clinical pregnancy was defined as the presence of a gestational sac on transvaginal sonogram. Patients were excluded if they received a fresh transfer in that specific COH cycle or if the cycle involved donor eggs. Only single embryo transfer FET cycles were included in the analysis. A total of 520 patients that had undergone PGD/PGS were initially identified for the time period in question. Two hundred thirty-eight patients where frozen serum was available for analysis were ultimately included.
All patients were offered PGS screening, as is the protocol of our center. At our center, 50 % of patients have failed in vitro fertilization (IVF) in other centers and seek PGS specifically when they come for consultation. Thirty-seven percent of the patients underwent intracytoplasmic sperm injection (ICSI) and 63 % underwent standard insemination. We have shown in the past that the rates of aneuploidy achieved with both insemination technologies are similar (unpublished data).
As per our center’s practice, stimulation protocols were chosen based on patient characteristics and baseline ovarian reserve lab values. The average age of our study population and the average starting follicle stimulating hormone (FSH) levels are listed in Table 1. The majority of ovarian stimulation cycles were the standard gonadotropin/antagonist cycles. Thirty-one cycles utilized micro dose Lupron flare, four were estrogen prime cycles, and three were Lupron “long protocol” cycles. As per our center protocol (in the antagonist cycles), when a lead follicle reached 13 mm or if estradiol was > 1000 pg/ml, the GnRH antagonist was initiated. When at least two lead follicles reached 18–19 mm in size, an ovulation trigger utilizing 250 mcg of recombinant HCG ×2 doses was given. Thirty-five to thirty-six hours after the trigger shot was administered, the oocytes were collected via ultrasound-guided transvaginal aspiration. Trigger, at our center, is achieved with 250 mcg of Ovidrel ×2 injections or if there is a concern for hyperstimulation, leuprolide acetate 40 units and 1000 units of human chorionic gonadotropin.
As has been described in other publications from our center, incubator conditions are set at 37 °C, 6 % CO2, and 5 % O2. We use single step Lifeglobal(R) (Guilford, CT) culture media and insemination was performed the same day as oocyte retrieval. If sperm appeared compromised, ICSI was performed for standard indications. Fertilization was assessed on culture day 1 via the presence of two pronuclei. On day 3 of culture, embryos were removed from the incubator and assessed for development. At this time, a small hole in the zona pellucida was created via laser assistance using a Cronus laser (Research instruments, Falmouth, UK).
Days 5/6 of culture embryos were graded via our center’s standard grading criteria, adapted from Gardner and Lane 1997 [36]. When embryos reached the expanded blastocyst stage, they underwent tropho-ectoderm biopsy (TE). Immediately following biopsy, embryos were cryopreserved. TE biopsy material was analyzed via array comparative hybridization technology (CGH).
Single embryo transfer was performed in the subsequent FET cycle. The protocol is described in great detail in a previous publication by our center [37]. It is not the standard of our center to obtain P4 values on the day of HCG trigger. As such, frozen serum was used that is stored for a maximum of 2 years at our center in a −80 °C freezer. The samples were de-identified, and ascension numbers were used to match the sample to the patient and also to the correct day. In our case, this involved ensuring that the current sample for the trigger day of the corresponding cycle was identified. After thawing the sample, an Immulite 2000 (Siemens Healthcare Global) was used to measure the progesterone value (ng/ml) that corresponded to that patient’s trigger day. The sample was then refrozen at −80 °C for future use. Our intra-assay variation is 5.9–6.8 % and inter-assay variation is 5.4–12.3 % for our Immulite system.
The patients were divided into two groups based on the serum P4 value on day of trigger. Group A included those patients with a P4 value of <1.5 ng/ml on day of trigger. Group B included those patients with a P4 value of ≥1.5 ng/ml. A threshold P4 value of 1.5 ng/ml was chosen based on the published literature, and one of the largest series to date that reported decreased ongoing pregnancy rates if this threshold was exceeded [4].
Statistical analysis was performed using a free online epidemiologic calculator (http://www.openepi.com/v37/Menu/OE_Menu.htm). T tests of means where completed where appropriate. Chi-square tests were used to evaluate pregnancy outcomes between the two patient groups.
Results
Patients were initially identified via searching our database for FET cycles performed between 2013 and 2014. Retrieval cycles that involved embryo biopsy and subsequent FET were identified. Only the first FET after index retrieval was considered in our results. As stated in the “Methods,” 238 patients total were included in the analysis.
Average age for group A was 38.4 years which is identical to the average age for Group B. For each FET cycle included in the analysis, baseline characteristics of the patients were collected and analyzed; these are listed in Table 1. Group A had an average trigger P4 value of 0.87 +/− 0.3 and group B had an average trigger P4 of 2.1 +/− 0.8. Significantly, estradiol in group B was 3034.2 pg/ml, which was significantly greater than group A, 2483.8 pg/ml. Total gonadotropin dosage was also found to be significantly different between the two groups (group A 3795.3 IU and group B 4395.2 IU).
The number of eggs retrieved and number of embryos biopsied (i.e., number of blastocysts that reached the stage that could be biopsied) were not different between the two groups. Number of euploid embryos available for transfer after the index retrieval cycle was not significantly different between the two groups (group A 1.87 embryos and group B 1.6 embryos). Number of aneuploid and non-diagnosis embryos was also not found to be significantly different; 32.1 % of patients in group A had no normal embryos available after the index retrieval. This is in comparison to 25.5 % of patients in group B that had no embryos available after the index retrieval, and this was not statistically significant. Group A had a pregnancy rate of 72 % and group B had a pregnancy rate of 66.7 %, which was not statistically significant (Table 2). Ongoing pregnancy/live birth rates were 65.6 % in group A and 66.67 % in group B, also not significant.
Discussion
Our study found that elevated P4 was associated with increased gonadotropin use and increased estradiol level on day of HCG trigger. We also found that elevated P4 had no measurable effect on the number of oocytes retrieved or the number of embryos available for biopsy. Further, there was no measurable effect on the pregnancy rate in subsequent FET cycles. Most notably, we found no correlation between P4 and the number of euploid embryos derived from the index retrieval. We can infer that elevated P4 on day of HCG trigger does not affect egg quality; instead, it likely affects the endometrium. Many researchers have hypothesized the same and have investigated the question from different perspectives, but this is the first study we are aware of that has shown that ploidy status of the embryo is not affected by serum P4 values on day of HCG trigger.
Our data revealed no difference in number of oocytes retrieved between group A and group B in our study. Other authors have found a correlation between elevated P4 and increased oocytes retrieved [12–14, 31, 38]. However, given the similarity in patient characteristics between the two groups, and the generally standard stimulation protocols our center follows, it is within reason that egg number would not vary between the two groups.
The idea that the uterine window of implantation is the main factor is supported significantly in the literature. Studies performed in oocyte donation programs suggested that pregnancy rates of recipients were not negatively influenced by progesterone levels of the donors on day of HCG trigger [17, 20, 23, 39]. Thus, we can infer that elevated P4 on day of HCG trigger is not reflecting poor egg and subsequently embryo quality, but is instead influencing the endometrium. Many other researchers have hypothesized the same and have investigated the endometrium from different perspectives. Several studies have investigated the association of P4 on the day of HCG administration during a stimulation cycle with pregnancy rates after a subsequent FET of those embryos obtained from the previous cycle [30, 31, 40–42]. In a meta-analysis, there was no difference in pregnancy rates [2]. While this finding suggests the endometrium is responsible for the drop in pregnancy seen in fresh cycles, many of these studies are not ideal. Specifically, the idea of the embryo factor cannot be discounted. The gold standard at this time is to transfer a single embryo with a normal chromosomal complement. To the best of our ability, we know that this embryo is genetically capable of producing an intrauterine gestation, and we know the accuracy of our genetic testing approaches 98 % [43].
Therefore, the mechanism by which P4 influences pregnancy rates is likely to be asynchrony between the embryo and the endometrium, whereby the implantation window is missed in patients with elevated P4. Franasiak et al. (2013) demonstrated that slower developing blastocysts have a decreased implantation rate in fresh, but not frozen, transfer cycles [44]. Due to the fact that the day of transfer is controlled in FET cycles, his finding suggests that a dyssynchronous endometrium decreases implantation rate.
Indeed, several authors have found that patients with a P4 serum concentration above 1.5 ng/ml on the day of HCG administration demonstrate a distinct difference in endometrial gene expression profile during the traditional window of implantation when compared to women with a normal P4 profile [29, 45, 46]. Our study was unique in that it conveniently assessed the influence of P4 on both the endometrium and egg quality. By combining PGS with FET, we were able to investigate embryo quality and control for the influence of P4 on the endometrium by transferring frozen-thawed embryos in subsequent cycles. Weaknesses of our study include the retrospective nature of the study, the relatively small sample size, and the older age of the PGS population, which may not be reflective of the general IVF population.
In conclusion, elevated P4 values on day of trigger have been shown to not affect egg number and ultimate number of available euploid embryos for transfer. The “freeze-all” strategy [40] in situations where the P4 value is found to be elevated can be employed safely, and patients can be reassured that the quality of these embryos is similar to those obtained in non-elevated P4 COH cycles. Rather than canceling a cycle for women with elevated P4 on day of HCG trigger, freezing embryos for transfer in subsequent cycles is a logical alternative that will be just as likely to result in a healthy pregnancy.
References
Messinis IE, Templeton A, Baird DT. Endogenous luteinizing hormone surge during superovulation induction with sequential use of clomiphene citrate and pulsatile human menopausal gonadotropin. J Clin Endocrinol Metab. 1985;61(6):1076–80.
Venetis, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60000 cycles. Hum Reprod Update. 2013;19(5):433–57.
Bosch E, Valencia W, Escudero E, Crespo J, Simon C, Remohi J, et al. Premature luteinization during gonadotropin-releasing hormone antagonist cycles and its relationship with in vitro fertilization outcome. Fertil Steril. 2003;80(6):1444–9.
Bosch E, Labarta E, Crespo J, Simon C, Remohi J, Jenkins J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod. 2010;25(8):2092–100.
Fleming R. Progesterone elevation on the day of hCG: methodological issues. Hum Reprod Update. 2008;14(4):391–2.
Schoolcraft W, Sinton E, Schlenker T, Huynh D, Hamilton F, Meldrum DR. Lower pregnancy rate with premature luteinization during pituitary suppression with leuprolide acetate. Fertil Steril. 1991;55(3):563–6.
Check JH, Lurie D, Askari HA, Hoover L, Lauer C. The range of subtle rise in serum progesterone levels following controlled ovarian hyperstimulation associated with lower in vitro fertilization pregnancy rates is determined by the source of manufacturer. Eur J Obstet Gynecol Reprod Biol. 1993;52(3):205–9.
Fanchin R, de Ziegler D, Taieb J, Hazout A, Frydman R. Premature elevation of plasma progesterone alters pregnancy rates of in vitro fertilization and embryo transfer. Fertil Steril. 1993;59(5):1090–4.
Shulman A, Ghetler Y, Beyth Y, Ben-Nun I. The significance of an early (premature) rise of plasma progesterone in in vitro fertilization cycles induced by a ‘long protocol’ of gonadotropin releasing hormone analogue and human menopausal gonadotropins. J Assist Reprod Genet. 1996;13(3):207–11.
Fanchin R, Hourvitz A, Olivennes F, Taieb J, Hazout A, Frydman. Premature progesterone elevation spares blastulation but not pregnancy rates in in vitro fertilization with coculture. Fertil Steril. 1997;68(4):648–52.
Kiliçdag E, Haydardedeoglu B, Cok T, Hacivelioglu S, Bagis T. Premature progesterone elevation impairs implantation and live birth rates in GnRH-agonist IVF/ICSI cycles. Arch Gynecol Obstet. 2010;281(4):747–52.
Ochsenkuhn R, Arzberger A, von Schönfeldt V, Gallwas J, Rogenhofer N, Crispin A, et al. Subtle progesterone rise on the day of human chorionic gonadotropin administration is associated with lower live birth rates in women undergoing assisted reproductive technology: a retrospective study with 2,555 fresh embryo transfers. Fertil Steril. 2012;98(2):347–54.
Kyrou D, Al-Azemi M, Papanikolaou EG, Donoso P, Tziomalos K, Devroey P, et al. The relationship of premature progesterone rise with serum estradiol levels and number of follicles in GnRH antagonist/recombinant FSH-stimulated cycles. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):165–8.
Park J, Lee B, Kim S. Factors influencing serum progesterone level on triggering day in stimulated in vitro fertilization cycles. Clin Exp Reprod Med. 2015;42(2):67–71.
Hill MJ, Royster IV GD, Healy MW, Richter KS, Levy G, DeCherney AH, et al. Are good patient and embryo characteristics protective against the negative effect of elevated progesterone level on the day of oocyte maturation? Fertil Steril. 2015;103(6):1477–84.
Edelstein MC, Seltman HJ, Cox BJ, Robinson SM, Shaw RA, Muasher SJ. Progesterone levels on the day of human chorionic gonadotropin administration in cycles with gonadotropin-releasing hormone agonist suppression are not predictive of pregnancy outcome. Fertil Steril. 1990;54(5):853–7.
Check JH, Hourani C, Choe JK, Callan C, Adelson HG. Pregnancy rates in donors versus recipients according to the serum progesterone level at the time of human chorionic gonadotropin in a shared oocyte program. Fertil Steril. 1994;61(2):262–4.
Givens CR, Schriock ED, Dandekar PV, Martin MC. Elevated serum progesterone levels on the day of human chorionic gonadotropin administration do not predict outcome in assisted reproduction cycles. Fertil Steril. 1994;62(5):1011–7.
Venetis CA, Kolibianakis EM, Papanikolaou E, Bontis J, Devroey P, Tarlatzis BC. Is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. Hum Reprod Update. 2007;13(4):343–55.
Check JH, Wilson C, Choe JK, Amui J, Brasile D. Evidence that high serum progesterone (P) levels on day of human chorionic gonadotropin (hCG) injection have no adverse effect on the embryo itself as determined by pregnancy outcome following embryo transfer using donated eggs. Clin Exp Obstet Gynecol. 2010;37(3):179–80.
Elgindy EA. Progesterone level and progesterone/estradiol ratio on the day of hCG administration: detrimental cutoff levels and new treatment strategy. Fertil Steril. 2011;95(5):1639–44.
Papanikolaou EG, Kolibianakis EM, Pozzobon C, Tank P, Tournaye H, Bourgain C, et al. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril. 2009;91(3):949–52.
Legro RS, Ary BA, Paulson RJ, Stanczyk FZ, Sauer M. Premature luteinization as detected by elevated serum progesterone is associated with a higher pregnancy rate in donor oocyte in-vitro fertilization. Hum Reprod. 1993;8(9):1506–11.
Doldi N, Marsiglio E, Destefani A, Gessi A, Merati G, Ferrari A. Elevated serum progesterone on the day of HCG administration in IVF is associated with a higher pregnancy rate in polycystic ovary syndrome. Hum Reprod. 1999;14(3):601–5.
Nagai T, Ding J, Moor RM. Effect of follicle cells and steroidogenesis on maturation and fertilization in vitro of pig oocytes. J Exp Zool. 1993;266(2):146–51.
Stanger JD, Yovich JL. Reduced in-vitro fertilization of human oocytes from patients with raised basal luteinizing hormone levels during the follicular phase. Br J Obstet Gynaecol. 1985;92(4):85–93.
Eibschitz I, Belaisch-Allart JC, Frydman R. In vitro fertilization management and results in stimulated cycles with a spontaneous luteinizing hormone discharge. Fertil Steril. 1986;45(2):231–6.
Lujueune B, Degueldre M, Camus M, Vekemans M, Opsomer L, Leroy F. In vitro fertilization and embryo transfer as related to endogenous luteinizing hormone rise or human chorionic gonadotropin administration. Fertil Steril. 1986;45(3):377–83.
Van Vaerenbergh, Fatemi HM, Blockeel C, Van Lommel L, In’t Veld P, Schuit F. Progesterone rise on HCG day in GnRH antagonist/rFSH stimulated cycles affects endometrial gene expression. Reprod Biomed Online. 2011;22(3):263–71.
Wu Z, Li R, Ma Y, Deng B, Zhang X, Meng Y, et al. Effect of HCG-day serum progesterone and oestradiol concentrations on pregnancy outcomes in GnRH agonist cycles. Reprod Biomed Online. 2012;24(5):511–20.
Lahoud R, Kwik M, Ryan J, Al-Jefout M, Foley J, Illingworth. Elevated progesterone in GnRH agonist down regulated in vitro fertilisation (IVFICSI) cycles reduces live birth rates but not embryo quality. Arch Gynecol Obstet. 2012;285(2):535–40.
Gutierrez-Mateo C, Colls P, Sanchez-Garcia J, Escudero T, Prates R, Ketterson K, et al. Validation of microarray comparative genomic hybridization for comprehensive chromosome analysis of embryos. Fertil Steril. 2011;95(3):953–8.
Grifo J, Hodes-Wertz B, Hsiao-Ling L, Amperloquio E, Clarke-Williams M, Adler A. Single thawed euploid embryo transfer improves IVF pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J Assist Reprod Genet. 2013;30(2):259–64.
Scott Jr RT, Upham KM, Forman EJ, Hong KH, Scott KL, Taylor D, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100(3):697–703.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100(1):100–7.
Gardner DK, Lane M. Culture and selection of viable blastocysts: a feasible proposition for human IVF? Hum Reprod Update. 1997;3(4):367–82.
Kofinas J, Blakemore J, McCulloh D, Grifo J. Serum progesterone levels greater than 20 ng/dl on day of embryo transfer are associated with lower live birth and higher pregnancy loss rates. J Assist Reprod Genet. 2015;32(9):1395–9.
Azem F, Tal G, Lessing, Malcov M, Ben-Yosef D, Almog B, et al. Does high serum progesterone level on the day of human chorionic gonadotropin administration affect pregnancy rate after intracytoplasmic sperm injection and embryo transfer? Gynecol Endocrinol. 2008;24(7):368–72.
Melo, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohi J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21(6):1503–7.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C, Thomas S. Embryo cryopreservation rescues cycles with premature luteinization. Fertil Steril. 2010;93(2):636–41.
Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro. Fertil Steril. 2012;97(6):1321–7.
Huang R, Fang C, Xu S, Yi Y, Liang X. Premature progesterone rise negatively correlated with live birth rate in IVF cycles with GnRH agonist: an analysis of 2,566 cycles. Fertil Steril. 2012;98(3):664–70.
Colls P, Escudero T, Fischer J, Cekleniak NA, Ben-Ozer S, Meyer B, et al. Validation of array comparative genome hybridization for diagnosis of translocations in preimplantation human embryos. Reprod BioMed Online. 2012;24(6):621–9.
Franasiak J, Forman E, Hong K, Werner M, Upham K, Scott RT. Investigating the impact of the timing of blastulation on implantation: active management of embryo-endometrial synchrony increases implantation rates. Fertil Steril. 2013;100(3):S97.
Labarta E, Martinez-Conejero JA, Alama P, Horcajadas JA, Pellicer A, Simon C, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011;26(7):1813–25.
Li R, Qiao J, Wang L, Li L, Zhen X, Liu P, et al. MicroRNA array and microarray evaluation of endometrial receptivity in patients with high serum progesterone levels on the day of hCG administration. Reprod Biol Endocrinol. 2011;9:29.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Our findings indicate that elevated progesterone on trigger day (greater than 1.5 ng/ml) is not associated with poor embryo quality or successful live births in subsequent frozen embryo transfer cycles.
Rights and permissions
About this article
Cite this article
Kofinas, J.D., Mehr, H., Ganguly, N. et al. Is it the egg or the endometrium? Elevated progesterone on day of trigger is not associated with embryo ploidy nor decreased success rates in subsequent embryo transfer cycles. J Assist Reprod Genet 33, 1169–1174 (2016). https://doi.org/10.1007/s10815-016-0752-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0752-y