Abstract
Purpose
The objective of our study was to determine if trophectoderm biopsy, vitrification, array-comparative genomic hybridization and single thawed euploid embryo transfer (STEET) can reduce multiple gestations and yield high pregnancy and low miscarriage rates.
Methods
We performed a retrospective observational study comparing single thawed euploid embryo to routine age matched in vitro fertilization (IVF) patients that underwent blastocyst transfer from 2008 to 2011 and to our best prognosis group donor oocyte recipients (Donor). Our main outcome measures were implantation rate, clinical pregnancy rate, spontaneous abortion rate and multiple gestation rate.
Results
The STEET group had a significantly higher implantation rate (58 %, 53/91) than the routine IVF group (39 %, 237/613) while the Donor group (57 %, 387/684) had a similar implantation rate. The clinical pregnancy rates were not statistically different between the STEET and IVF groups. However, the multiple gestation rate was significantly lower in the STEET group (STEET 2 % versus IVF 34 %, Donor 47 %).
Conclusions
STEET results in a high pregnancy rate, low multiple gestation rate and miscarriage rates. Despite the older age of STEET patients and transfer of twice as many embryos, the implantation rate for STEET was indistinguishable from that for egg donation. STEET offers an improvement to IVF, lowering risks without compromising pregnancy rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
While in vitro fertilization (IVF) has provided thousands of people with success, IVF outcomes are still not ideal. The ultimate goal is to provide patients with one healthy child in a cost effective manner while avoiding the heartache of pregnancy loss. This is quite a tremendous and difficult goal for all age groups. Firstly, despite many advances in IVF in the past thirty years such as intracytoplasmic injection (ICSI) [26], extended embryo culture [8, 9], embryo biopsy and preimplantation genetic diagnosis (PGD) [10, 12], the pregnancy rate in fresh IVF cycles nationally in 2010 was only 42 % in those under 35 years of age (often referred to as a good prognosis group). In addition, while a miscarriage is devastating for all women, having a loss after IVF is even more upsetting and time consuming. On the other end of the spectrum is the complication of multiple gestations. Multiple gestations are associated with costs to society [4] and couples via neonatal intensive care unit hospitalizations, increased risks of cerebral palsy [15], preterm delivery and death [27, 38]. Even though the multiple gestation rate and high order multiple rates are declining nationally they still pose a serious threat. Although elective single embryo transfer (SET) has been shown to have equivalent pregnancy outcomes to cycles where more than one embryo is transferred [22, 33], a majority of providers still fail to perform SET [16, 36]. The obvious answer to reduce the multiple gestation rate (MGR) is to transfer one embryo at a time but this puts tremendous pressure on the embryologists and physician to choose the best embryo for transfer.
Much of our failures in IVF such as pregnancy loss and decreased implantation rates can be explained by aneuploidy [2, 3, 40]. In addition, embryo morphology cannot be used exclusively to reliably choose the best embryos for transfer as aneuploid embryos are capable of achieving high morphologic scores, and poor morphology does not exclude euploidy [1, 20, 23, 24]. While it makes logical sense that directly identifying the ploidy status of an embryo would improve pregnancy rates and decrease miscarriage rates, initial studies for PGD using fluorescence in situ hybridization (FISH) did not demonstrate a benefit to screening the embryos before transfer [6]. FISH was limited in its ability to screen more than 12 chromosomes and later found to be inconsistent with a poor negative predictive value [25, 34].
Recent technologies are showing significantly more promise [13, 29, 32]. Comprehensive chromosomal screening (CCS) provides a benefit of examining all 23 pairs of chromosomes using comparative genomic hybridization. [5, 11, 14, 28, 30, 31, 35, 39] In addition, trophectoderm (TE) biopsy allows for more cells to be analyzed at a time when less mosaicism exists and the embryo sustains less irreparable damage [21, 25, 37]. So far, one randomized controlled trial and many other observational studies have demonstrated an increase in implantation rates, clinical pregnancy rates and decreased spontaneous abortion rates [28, 31, 41].
The objective of our study was to compare outcomes of our single thawed euploid embryo transfer population (STEET group) to an age-matched routine IVF population (IVF) and to our best prognosis group, donor recipient population (Donor).
Materials and methods
This retrospective study reviewed all patients that underwent STEET from November 2010 to June 2012. These patients chose to undergo TE biopsy due to various reasons such as aneuploidy screening (due to a history of recurrent pregnancy loss or infertility or advanced maternal age), single gene defects, family balancing, or known parental translocation. Oocyte recipients (5 during this time period) were excluded from the analysis. The STEET group was compared to age matched controls (3:1) who had a blastocyst fresh transfer during routine IVF cycles from 2008 to 2010. In addition, the STEET group was then compared to donor recipients that underwent a fresh blastocyst transfer from 2008 to 2010.
Each patient’s ovarian stimulation protocol was individualized to achieve adequate numbers of mature oocytes at retrieval and at times the providers were more aggressive than patients undergoing conventional IVF. When lead follicles reached a mean diameter of 17–18 mm, 10,000 IU of hCG was administered intramuscularly and ∼35 h later, oocytes were collected by ultrasound guided, transvaginal aspiration. Oocytes were isolated from follicular fluid and immediately placed in 75-uL droplets of human tubal fluid (HTF Irvine, Ca) supplemented with 6 % Plasmanate (Pittsburgh, PA) overlaid with Sage mineral oil. Partner’s sperm was collected on day of retrieval and washed. Oocytes were inseminated at 4-6 hours post retrieval or intracytoplasmic sperm injection was performed when indicated by severe male factor, history of poor fertilization, or for single gene defects PGD. Fertilization was assessed 18 h post insemination or ICSI by visualization of two pronuclei (2pn). Embryos were incubated and monitored on day 3 for blastomere number, symmetry, degree of fragmentation, and overall quality. The decision to culture to day 5 was based on the quantity and quality of embryos on day 3 for the Donor group and the IVF group. [9] All of the patients in the IVF and Donor group had an excess number of good quality embryos available for transfer (generally > 3 embryos), so embryo culture was continued until day 5 and blastocyst transfer performed. Embryos were graded on day 5 using the Gardner criteria [7].
For both the IVF and Donor group, the best-quality embryos based on morphology were chosen for embryo transfer regardless of fertilization method used, and the number of blastocysts for transfer was decided collaboratively with the embryologist, physician and patient in accordance with American Society of Reproductive Medicine guidelines. The remaining good-quality blastocysts were cryopreserved on day 5 or 6 according to protocol. [18]
STEET protocol
For patients that had elected to have TE biopsy, a hole was made in the zona pellucida on day 3 of embryo development using a Cronus laser (Research Instruments, Falmouth, United Kingdom) to allow hatching. Resultant embryos were cultured to day 5 and any embryos not suitable on day 5 for biopsy were cultured to day 6. On the day of biopsy (day 5 or 6), TE biopsy was performed and a piece of the extruded trophectoderm was isolated and cut using laser. The biopsied cells were placed in Eppendorf tubes, frozen in dry ice, and then transported to Reprogenetics for PGS analysis once all of the biopsies were performed. This analysis was performed using the method described in Gutierrez, Mateo et al. without modification. [11] Embryos were then cryopreserved using vitrification. Embryos were then cryopreserved using vitrification. Embryos were first equilibrated in media containing the lowest concentration of cryoprotectants (7.5 % ethylene glycol [EG] and 7.5 % dimethyl sulfoxide [DMSO]) to achieve the first level of dehydration. They were then placed in vitrification solution with cryoprotectants (15 % EG and 15 % DMSO). Embryos were then loaded onto Cryolock (Cummings, GA) and immediately plunged directly into liquid nitrogen.
The STEET group then underwent a thaw cycle utilizing sequential oral estradiol supplemented by intramuscular progesterone after the endometrial stripe achieved a ring pattern and was greater than 7 mm. An appropriately timed thaw and ultrasound guided embryo transfer was performed with a single euploid blastocyst.
Statistical analyses
The main outcome measures included implantation (IR), clinical pregnancy (CPR) and live birth or ongoing pregnancy (LBR/OPR) rates per transfer. The IR was calculated as the number of intrauterine gestational sacs visualized on ultrasound per total number of embryos transferred. A clinical pregnancy was defined as the presence of an intrauterine gestational sac(s) with fetal cardiac activity as documented by ultrasound. A spontaneous abortion (SAB) was considered as a loss less than 20 week and the SAB rate (SABR) was calculated as the number of SABs per pregnancies with at least one intrauterine sac on ultrasound. The multiple gestation rate (MGR) was calculated per clinical pregnancy. The LBR per transfer was calculated for the IVF and Donor groups but an ongoing pregnancy rate (OPR, pregnancies into the second trimester per transfer) was used for the STEET group. For statistical analysis, t-test was used to compare baseline characteristics and Chi-square to compare outcomes between the groups. Our retrospective study was approved for exemption by the New York University School of Medicine Institutional Review Board, and no investigators declared a conflict of interest.
Results
STEET group
During that time period, there were 91 single embryo transfers from 78 patients that underwent an oocyte retrieval followed by TE biopsy, vitrification, array-comparative genomic hybridization analysis, and embryo thaw. Most patients (69) had a single transfer but seven patients had two transfers and two patients had three transfers (all from the single egg retrieval) during this time period. There were also two patients that had 2 retrievals during this time period. The average age of the patients was 37.2 ± 4.0 (range 22–43). The reasons the patients elected TE biopsy included aneuploidy screening (n = 58), family balancing (n = 16), single gene defect (n = 13) and parental translocation (n = 4). The pregnancy rates for each group were as follows: aneuploidy screening 50 %, family balancing 62 %, single gene defect 62 % and parental translocation 75 %.
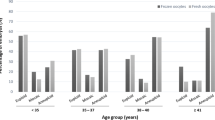
From the 80 retrievals there were 545 blastocysts that underwent biopsy (range of number of embryos for biopsy was 1–26, avg. 6.8 ± 4.8) and 242 were normal (44.4 %). The percent of euploid embryos decreased with age (<35–56 %, 35–37 yo −56 %, 38–40 yo −40 %, 41–42 yo −34 %, 43yo −43 %). There were 37 STEETs performed where there were no other euploid embryos for transfer and 54 STEETs where there were other euploid embryos for transfer. There was no difference in pregnancy rate between the two groups (57 % in those with remaining euploid embryos versus 51 %). Pregnancy was achieved in those with anywhere from 1 to 26 embryos for biopsy. There were 4 SABs in the STEET group. Two of the SABs underwent dilation and curettage with chromosome analysis and euploidy and gender were confirmed (46, XY in both cases).
IVF group comparison
In the IVF group there were 273 age-matched controls and Table 1 describes the cycle characteristics between the groups and cycle outcomes. While there were significantly more oocytes retrieved and 2pns on average in the STEET group, the ovarian reserve did not differ between the two groups. In addition, the range of oocytes retrieved and 2pns in the STEET group (6–42 oocytes, 3–34 2 pns) was similar to the IVF group (4–49 oocytes, 3–29 2 pns). Also of note, significantly more embryos were transferred in the routine IVF group (range 1–6). The IR per transfer is significantly higher in STEET than routine IVF while the SABR and MGR were significantly lower. There was one monozygotic twin pregnancy in the STEET group, 43 twin pregnancies and 3 triplet pregnancies in the IVF group.
Outcomes were stratified by age in Table 2. STEET improved the IR for both those under and over 35. For those under the age of 35, STEET offers the same CPR, SABR, and LBR per transfer without the increased risk of a multiple gestation (56 % of clinical pregnancies in this group). For those over 35, STEET provides not only the benefit of a decreased MGR but also of a decreased SABR.
Donor group comparison
There were 355 donor recipients that underwent blastocyst transfers from 2008 to 2010. The characteristics and outcomes can be found in Table 3. Yet again, there were significantly more embryos transferred in the Donor group (range 1–3) while the donor oocyte age was significantly younger than the STEET group. There was no difference in IR per transfer when comparing STEET to the Donor group and the CPR per transfer was higher in the Donor group but the MGR was also significantly higher. There were 108 twin pregnancies and 4 triplet pregnancies in this group.
Discussion
STEET clearly has many advantages. The same IVF CPR can be achieved with one euploid embryo. We believe that the IR is a better outcome measure as the main goal is for a single embryo to implant. While the CPR and LBR appear comparable to routine IVF and Donor, it comes at a price with increased multiple gestations and higher miscarriage rate in some. With STEET, triplets will be virtually eliminated. It is important to note that these are pregnancies per transfer and not retrieval. The STEET CPR per retrieval is approximately 66 % in those that had at least one euploid embryo. Performing SET will possibly lead to more transfer cycles but again less twins and triplets.
We were able to demonstrate a SABR in women over 35 similar to the SABR in those under 35 or donor recipients. Replacing known euploid embryos will help to avoid the cost, time and heartache of a miscarriage. Larger numbers may be needed to reveal this benefit in the younger patients if it exists. The pregnancy rate was the same whether the patient had more euploid embryos available or not, a characteristic typically used to predict a better prognosis. Knowing ploidy status before transfer may be more beneficial than having more embryos available and will avoid storage of aneuploid embryos. In addition, recent literature suggests that there may be neonatal benefits to embryo transfer into an unstimulated uterus. [17]
SET are also offered typically in young, good prognosis patients but clearly those 35 and over are still at risk of multiple gestations. More embryos are typically transferred in this age group in an effort to make sure a euploid embryo is replaced as aneuploidy is known to increase with age. [3, 19] However, without a biopsy before transfer how many euploid embryos are actually transferred is not known thus increasing chances of more than one implantation. There is no compromise in LBR by transferring one euploid embryo in this population not typically characterized as good prognosis patients. When comparing STEET to all IVF cycles at our center with a mean age of 37 from 2003 to 2009, STEET has a statistically significant CPR (50/91 vs. 641/1520, p = 0.03, unpublished data).
STEET is not for all patients. Patients that are eligible for STEET need to have embryos for biopsy and at least one euploid embryo for transfer. During the same time period we had 22 cycles where there was no euploid embryos available for transfer. While this may seem disappointing at first, it does save time, cost, patient progesterone injections, and heartache that would otherwise be involved if no biopsy had been done and the patient ended up with a negative pregnancy test or pregnancy loss. A more frustrating situation involves cancellation as we had 13 patients that had nothing for biopsy on day 5 or 6. In these patients it is not known if any of their embryos were euploid or not. It should be noted that if we calculated the CPR including patients that did not have embryos for biopsy and embryos for transfer it would 36 % per retrieval. Patients need to be aware, as they would with routine IVF, that there is the possibility that they would have nothing available for transfer.
The study has several limitations. Its retrospective nature allows for inherent selection bias. In fact, many of the STEET patients had previous IVF failures or repeated miscarriage with IVF. While these results may be extrapolated to a large population of patients undergoing TE biopsy for a variety of reason, there is the potential for confounders in patients that elect to undergo TE biopsy.
Comprehensive chromosome screening of blastocysts may finally alleviate some of the negative outcomes associated with IVF such as SABs and multiple gestations. This study confirms that knowing the ploidy status of an embryo leads to the same CPR and LBR as routine IVF patients while decreasing the MGR and SABR. Chromosomal status is a better predictor of success than morphology assessment and thus a better method for single embryo selection. More prospective and randomized studies are needed to verify these findings but STEET may be the best tool providers have so far to help meet the ultimate goal of one healthy infant at a time.
References
Alfarawati S, Fragouli E, Colls P, Stevens J, Gutierrez-Mateo C, Schoolcraft WB, Katz-Jaffe MG, Wells D. The relationship between blastocyst morphology, chromosomal abnormality, and embryo gender. Fertil Steril. 2011;95:520–4.
Bettio D, Venci A, Levi Setti PE. Chromosomal abnormalities in miscarriages after different assisted reproduction procedures. Placenta. 2008;29(Suppl B):126–8.
Bielanska M, Tan SL, Ao A. Chromosomal mosaicism throughout human preimplantation development in vitro: incidence, type, and relevance to embryo outcome. Hum Reprod. 2002;17:413–9.
Bromer JG, Ata B, Seli M, Lockwood CJ, Seli E. Preterm deliveries that result from multiple pregnancies associated with assisted reproductive technologies in the USA: a cost analysis. Curr Opin Obstet Gynecol. 2011;23:168–73.
Fragouli E, Lenzi M, Ross R, Katz-Jaffe M, Schoolcraft WB, Wells D. Comprehensive molecular cytogenetic analysis of the human blastocyst stage. Hum Reprod. 2008;23:2596–608.
Fritz MA. Perspectives on the efficacy and indications for preimplantation genetic screening: where are we now? Hum Reprod. 2008;23:2617–21.
Gardner DWA, Howles C, Shoham Z. Textbook of assisted reproductive techniques laboratory and clinical perspectives. Malden: Blackwell Science Inc; 2001.
Gardner DK, Schoolcraft WB, Wagley L, Schlenker T, Stevens J, Hesla J. A prospective randomized trial of blastocyst culture and transfer in in-vitro fertilization. Hum Reprod. 1998;13:3434–40.
Grifo JA, Flisser E, Adler A, McCaffrey C, Krey LC, Licciardi F, Noyes N, Kump LM, Berkeley AS. Programmatic implementation of blastocyst transfer in a university-based in vitro fertilization clinic: maximizing pregnancy rates and minimizing triplet rates. Fertil Steril. 2007;88:294–300.
Grifo JA, Tang YX, Cohen J, Gilbert F, Sanyal MK, Rosenwaks Z. Pregnancy after embryo biopsy and coamplification of DNA from X and Y chromosomes. JAMA. 1992;268:727–9.
Gutierrez-Mateo C, Colls P, Sanchez-Garcia J, Escudero T, Prates R, Ketterson K, Wells D, Munne S. Validation of microarray comparative genomic hybridization for comprehensive chromosome analysis of embryos. Fertil Steril. 2011;95:953–8.
Handyside AH, Kontogianni EH, Hardy K, Winston RM. Pregnancies from biopsied human preimplantation embryos sexed by Y-specific DNA amplification. Nature. 1990;344:768–70.
Hardarson T, Hanson C, Lundin K, Hillensjö T, Nilsson L, Stevic J, Reismer E, Borg K, Wikland M, Bergh C. Preimplantation genetic screening in women of advanced maternal age caused a decrease in clinical pregnancy rate: a randomized controlled trial. Hum Reprod. 2008;23:2806–12.
Hellani A, Abu-Amero K, Azouri J, El-Akoum S. Successful pregnancies after application of array-comparative genomic hybridization in PGS-aneuploidy screening. Reprod Biomed Online. 2008;17:841–7.
Hvidtjørn D, Grove J, Schendel D, Svaerke C, Schieve LA, Uldall P, Ernst E, Jacobsson B, Thorsen P. Multiplicity and early gestational age contribute to an increased risk of cerebral palsy from assisted conception: a population-based cohort study. Hum Reprod. 2010;25:2115–23.
Jungheim ES, Ryan GL, Levens ED, Cunningham AF, Macones GA, Carson KR, Beltsos AN, Odem RR. Embryo transfer practices in the United States: a survey of clinics registered with the Society for Assisted Reproductive Technology. Fertil Steril. 2010;94:1432–6.
Kalra SK, Ratcliffe SJ, Coutifaris C, Molinaro T, Barnhart KT. Ovarian stimulation and low birth weight in newborns conceived through in vitro fertilization. Obstet Gynecol. 2011;118:863–71.
Kaufmann RA, Menezo Y, Hazout A, Nicollet B, Dumont M, Servy EJ. Cocultured Blastocyst cryopreservation - experience of more than 500 transfer cycles. Fertil Steril. 1995;64:1125–9.
Kuliev A, Cieslak J, Verlinsky Y. Frequency and distribution of chromosome abnormalities in human oocytes. Cytogenet Genome Res. 2005;111:193–8.
Magli MC, Gianaroli L, Ferraretti AP, Lappi M, Ruberti A, Farfalli V. Embryo morphology and development are dependent on the chromosomal complement. Fertil Steril. 2007;87:534–41.
Mottla GL, Adelman MR, Hall JL, Gindoff PR, Stillman RJ, Johnson KE. Lineage tracing demonstrates that blastomeres of early cleavage-stage human pre-embryos contribute to both trophectoderm and inner cell mass. Hum Reprod. 1995;10:384–91.
Mullin CM, Fino ME, Talebian S, Krey LC, Licciardi F, Grifo JA. Comparison of pregnancy outcomes in elective single blastocyst transfer versus double blastocyst transfer stratified by age. Fertil Steril. 2010;93:1837–43.
Munne S, Alikani M, Tomkin G, Grifo J, Cohen J. Embryo morphology, developmental rates, and maternal age are correlated with chromosome abnormalities. Fertil Steril. 1995;64:382–91.
Munné S, Chen S, Colls P, Garrisi J, Zheng X, Cekleniak N, Lenzi M, Hughes P, Fischer J, Garrisi M, Tomkin G, Cohen J. Maternal age, morphology, development and chromosome abnormalities in over 6000 cleavage-stage embryos. Reprod Biomed Online. 2007;14:628–34.
Northrop LE, Treff NR, Levy B, Scott RT. SNP microarray-based 24 chromosome aneuploidy screening demonstrates that cleavage-stage FISH poorly predicts aneuploidy in embryos that develop to morphologically normal blastocysts. Mol Hum Reprod. 2010;16:590–600.
Palermo G, Joris H, Derde MP, Camus M, Devroey P, van Steirteghem A. Sperm characteristics and outcome of human assisted fertilization by subzonal insemination and intracytoplasmic sperm injection. Fertil Steril. 1993;59:826–35.
Reddy UM, Wapner RJ, Rebar RW, Tasca RJ. Infertility, assisted reproductive technology, and adverse pregnancy outcomes: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2007;109:967–77.
Schoolcraft WB, Fragouli E, Stevens J, Munné S, Katz-Jaffe MG, Wells D. Clinical application of comprehensive chromosomal screening at the blastocyst stage. Fertil Steril. 2010;94:1700–6.
Schoolcraft WB, Katz-Jaffe MG, Stevens J, Rawlins M, Munne S. Preimplantation aneuploidy testing for infertile patients of advanced maternal age: a randomized prospective trial. Fertil Steril. 2009;92:157–62.
Schoolcraft WB, Treff NR, Stevens JM, Ferry K, Katz-Jaffe M, Scott RT. Live birth outcome with trophectoderm biopsy, blastocyst vitrification, and single-nucleotide polymorphism microarray-based comprehensive chromosome screening in infertile patients. Fertil Steril. 2011;96:638–40.
Scott RT, Ferry K, Su J, Tao X, Scott K, Treff NR. Comprehensive chromosome screening is highly predictive of the reproductive potential of human embryos: a prospective, blinded, nonselection study. Fertil Steril. 2012;97:870–5.
Staessen C, Platteau P, van Assche E, Michiels A, Tournaye H, Camus M, Devroey P, Liebaers I, van Steirteghem A. Comparison of blastocyst transfer with or without preimplantation genetic diagnosis for aneuploidy screening in couples with advanced maternal age: a prospective randomized controlled trial. Hum Reprod. 2004;19:2849–58.
Styer AK, Wright DL, Wolkovich AM, Veiga C, Toth TL. Single-blastocyst transfer decreases twin gestation without affecting pregnancy outcome. Fertil Steril. 2008;89:1702–8.
Treff NR, Levy B, Su J, Northrop LE, Tao X, Scott RT. SNP microarray-based 24 chromosome aneuploidy screening is significantly more consistent than FISH. Mol Hum Reprod. 2010;16:583–9.
Treff NR, Su J, Tao X, Levy B, Scott RT. Accurate single cell 24 chromosome aneuploidy screening using whole genome amplification and single nucleotide polymorphism microarrays. Fertil Steril. 2010;94:2017–21.
van Peperstraten AM, Nelen WL, Hermens RP, Jansen L, Scheenjes E, Braat DD, Grol RP, Kremer JA. Why don't we perform elective single embryo transfer? A qualitative study among IVF patients and professionals. Hum Reprod. 2008;23:2036–42.
Vanneste E, Voet T, le Caignec C, Ampe M, Konings P, Melotte C, Debrock S, Amyere M, Vikkula M, Schuit F, Fryns JP, Verbeke G, D'Hooghe T, Moreau Y, Vermeesch JR. Chromosome instability is common in human cleavage-stage embryos. Nat Med. 2009;15:577–83.
Voelker R. Researchers in Canada call for policy to mandate single-embryo transfer in IVF. JAMA. 2011;305:1848.
Wells D, Delhanty JD. Comprehensive chromosomal analysis of human preimplantation embryos using whole genome amplification and single cell comparative genomic hybridization. Mol Hum Reprod. 2000;6:1055–62.
Werner M, Reh A, Grifo J, Perle MA. Characteristics of chromosomal abnormalities diagnosed after spontaneous abortions in an infertile population. J Assist Reprod Genet; 2012.
Yang Z, Liu J, Collins GS, Salem SA, Liu X, Lyle SS, Peck AC, Sills ES, Salem RD. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5:24.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule
Single thawed euploid embryo transfer results in a high pregnancy rate, low multiple gestation rate and miscarriage rates.
Rights and permissions
About this article
Cite this article
Grifo, J.A., Hodes-Wertz, B., Lee, HL. et al. Single thawed euploid embryo transfer improves IVF pregnancy, miscarriage, and multiple gestation outcomes and has similar implantation rates as egg donation. J Assist Reprod Genet 30, 259–264 (2013). https://doi.org/10.1007/s10815-012-9929-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-012-9929-1